Abstract
Background
Children who experience more than one urinary tract infection (UTI) are at increased risk of kidney scarring due to their UTIs. Girls are at especially high risk for developing kidney scarring as a result of recurrent UTIs. Prior work suggested that neutrophil gelatinase-associated lipocalin (NGAL) may be lower in children with recurrent UTI compared with those without. The objective of this work was to compare urine NGAL concentrations in matched urine samples in girls with single and recurrent UTIs.
Methods
Girls less than 6 years of age who presented with signs and symptoms of a UTI were eligible for enrollment. Both acute, obtained from residual urine collected as part of their clinical evaluation, and follow-up urine samples, obtained after the completion of antibiotics when the patient was in their usual state of health, were collected from patients. Acute and follow-up urine NGAL concentrations were compared between girls with single and recurrent UTIs, as well as those with negative cultures who served as controls.
Results
Seventy girls were included in this study, 6 controls, 43 single UTIs, and 20 girls with recurrent UTIs. Patients in the control group had lower median acute NGAL concentrations than either those with single or recurrent UTI. There were no differences in either acute or follow-up urine NGAL concentrations between those with single and recurrent UTIs.
Conclusion
In this cohort of girls less than 6 years of age, there is no difference in urine NGAL concentrations between those with single and recurrent UTIs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary tract infections (UTIs) are one of the most common bacterial infections in children. Approximately 8% of children with an initial UTI will go on to develop recurrent infections [1], placing these children at increased risk for kidney scarring [2]. However, despite the identification factors that increase the risk of recurrent UTIs, such as vesicoureteral reflux (VUR) [3] and bowel and bladder dysfunction (BBD) [4], accurately predicting which children will experience a recurrent infection at the time of the initial UTI is difficult. Indeed, one study examined the rate of recurrent UTI in children with BBD and found that in several subsets of patients (those without VUR and not on prophylaxis and those with VUR and on prophylaxis), BBD was not associated with risk of UTI or febrile UTI, while in children with VUR and not on prophylaxis, BBD was associated with recurrent UTIs, but not febrile UTIs [4]. The authors concluded that their data highlighted the poorly understood relationships between BBD, VUR, recurrent UTIs, and antibiotic prophylaxis [4]. A further complicating factor to preventing recurrent UTIs is that continuous antibiotic prophylaxis, frequently used to decrease the risk of recurrent UTI in children despite a meta-analysis that suggests a lack of efficacy in preventing scarring [5], is associated with increased risk of both colonization and infection with an antibiotic-resistant organism [6]. The ability to identify which children are at increased risk of recurrent UTI at the time of the initial infection would allow for targeted initiation of interventions, such as continuous antibiotic prophylaxis, in those children who may disproportionately benefit from their use.
There are several areas of gender differences with regard to UTI. After the first few months of life [7], girls have a higher rate of UTIs than boys: the prevalence of UTIs in girls less than 6 years of age is 3–7%, compared with 1–2% for boys of the same age [8,9,10]. Additionally, girls are more likely to develop postnatal scarring compared with boys, who have a higher rate of prenatal scars [11,12,13]. Further, in children with prior UTIs, the only identified risk factor for progression of kidney damage (as defined by further reduction in differential kidney function) in boys is the presence of high-grade VUR, while recurrent febrile UTIs are also significantly associated with risk of progression of kidney damage in girls [14]. Taken together, these data suggest that girls are at higher risk of kidney scarring and continued decline in kidney function as a result of febrile UTIs compared with boys.
Urine neutrophil gelatinase-associated lipocalin (NGAL) is a protein that exerts a bacteriostatic effect in the urinary tract through chelation of environmental iron [15]. As such, urine NGAL is a part of the local innate immune system in the bladder. Given the role that urine NGAL plays in the local innate immune system, children who are deficient for urine NGAL would theoretically be at risk for UTIs. Indeed, NGAL knock-out mice have longer bacteriuria following induction of UTI compared with controls, providing support for this hypothesis. Further, a previous proof-of-concept study demonstrated a relative decrease in urine NGAL in children with history of recurrent UTI compared with controls [16]. The objective of this work was to confirm this previously reported finding of decreased urine NGAL levels in children with recurrent UTI using paired samples from girls with UTI, rather than a convenience sample of controls used in the prior study. Given the increased risk of acquired kidney scarring and decreased kidney function associated with recurrent febrile UTIs in girls, as well as gender-based differences in normal urine NGAL values [17], we chose to focus exclusively on girls in this study.
Methods
Patients
Girls less than 4 years of age who were diagnosed with either a febrile or non-febrile UTI in the emergency department or general pediatrics clinic at a single free-standing children’s hospital from March of 2016 to March of 2018 were eligible for inclusion in this study. Patients were excluded if they were already taking antibiotics prescribed to treat the active infections (patients who developed a UTI despite being on prophylactic antibiotics were still enrolled); had evidence of acute kidney injury on presentation to the emergency department; had a known immunodeficiency; had a known abnormality of the genitourinary tract such as hydronephrosis, posterior urethral valves, or high-grade vesicoureteral reflux (grade III or higher); or required clean intermittent catheterization. Patients with uncomplicated vesicoureteral reflux (grades II or less) were eligible for inclusion in this study. Patients were identified through use of VigiLanz™ (Minneapolis, MN), a real-time lab monitoring system. Patients who had a urinalysis with any of the following parameters triggered the alert: more than 1+ leukocyte esterase, positive nitrites, or more than 10 white blood cells. When a patient met these criteria, an email was sent to a member of the research team. These patients were then screened to determine if they met inclusion criteria and residual urine sent to the lab for urine culture. Urine cultures were followed, and if the culture was positive for at least 50,000 colony-forming units per milliliter of a uropathogen, the parent/guardian caregiver was contacted for consent.
Definitions
UTI was defined as per the American Academy of Pediatrics definition: growth of ≥ 50,000 colony-forming units per milliliter of a known uropathogen in urine culture in combination with pyuria [18]. Children with a history of UTI, as reported in the electronic health record or by parental report, were in the recurrent UTI group. Children enrolled during their first UTI were in the single UTI group. Each patient was followed for a period of 6 months to identify UTI recurrence. If a UTI recurred in a patient in the single UTI group, they were moved to the recurrent UTI group. Control patients were those who presented to the emergency department with signs and symptoms of a UTI but had a negative urine culture.
Urine samples
Acute samples were obtained from residual urine initially collected for routine clinical purposes. Residual urine for this study was collected from the clinical laboratory after the patient was screened and determined to have met inclusion criteria. Samples were centrifuged and the supernatant aliquoted and frozen at − 80 °C within 12 hours of collection. If consent was not obtained, the samples were discarded. The follow-up urine sample was collected at least 2 weeks following the completion of the antibiotic course prescribed to treat the UTI, when the participants had returned to their baseline state of health. Follow-up urine samples were either collected by clean catch or placement of cotton balls within the diaper on the same day the urine sample was delivered to the research team. Families were instructed to place the sample in the refrigerator if there was a delay between sample collection and delivery. Once the follow-up samples were received, the urine was centrifuged and the supernatant aliquoted and frozen as described above. Samples did not undergo any freeze-thaw cycles prior to biomarker analysis.
Biomarker measurement
Urine NGAL was measured by the Center for Acute Care Nephrology at Cincinnati Children’s Hospital Medical Center. Urine NGAL was measured by ELISA (Bioporto, Grusbakken, Denmark) and urine creatinine by assay (Siemens Dimension RXL Max Clinical Analyzer, Munich, Germany).
Statistical analysis
Normally distributed continuous variables were compared using ANOVA and post hoc Tukey, while Kruskal-Wallis with a post hoc Dunn was used for non-normally distributed variables. Categorical variables were compared with chi-square or Fisher’s exact, as appropriate. As we initially enrolled several children diagnosed and treated for a UTI who ultimately had negative urine cultures (thus comprising our control group), we used a receiver operating curve (ROC) to determine the accuracy of urine NGAL in predicting positive urine cultures in children with signs and symptoms of a UTI. A p value of less than 0.05 was considered statistically significant. All statistical analyses were completed with R [19], with package pROC to generate ROC curves [20]. This work was approved by the Cincinnati Children’s Hospital Institutional Review Board. Written informed consent was obtained from parents or guardians for participation in this study. All data is available from the corresponding author upon reasonable request.
Results
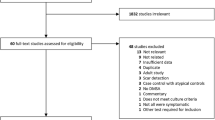
Seven hundred thirty-seven unique patients were screened, of whom 255 were eligible for inclusion and had a urine sample that was collected within the required time period. Of these 255 patients, 163 families could not be reached for consent, 21 declined, and 70 consented (Fig. 1). The 70 girls enrolled included 6 controls, 44 with single UTIs, and 20 children with recurrent UTIs. Fifty-three percent of the 70 participants provided a follow-up sample (3 in the control group, 24 in the single UTI group, and 10 children in the recurrent UTI group). There was no difference in demographics, presence of fever on presentation, or history of constipation between groups, for both the entire cohort (Table 1) and the subgroup of patients who returned the follow-up sample (Table 2). Most (94%) patients with UTIs had Escherichia coli as the causative pathogen.
Twenty-nine patients in this study had a kidney ultrasound completed, including 15 of the patients in the recurrent UTI group, 13 in the single UTI group, and one in the control group. Twenty-three ultrasounds were normal, 4 showed duplex collecting systems, and one showed bilateral pelviectasis. Fourteen patients underwent a vesicoureteral cystogram (VCUG), five in the single UTI group and nine in the recurrent UTI group. Of these, five patients did not have vesicoureteral reflux (VUR), four had unilateral grade 1 VUR, one had bilateral grade 1 VUR, three had unilateral grade 2 VUR, and one had bilateral grade 2 VUR. Of the five patients in the single UTI group who had VCUGs, three had no VUR, one was found to have bilateral grade 1 VUR, and one had unilateral grade 2 VUR.
Patients in the control group had lower median acute urine NGAL concentrations (64 μg/g creatinine; 95% confidence interval (CI), 14–255; interquartile range (IQR), 20–125) compared with those in the single (820 μg/g creatinine; 95% CI, 499–1070; IQR, 391–1561; p < 0.01) and recurrent UTI group (899 μg/g creatinine; 95% CI, 382–2009; IQR, 368–2066; p < 0.01). In patients for whom both acute and follow-up samples were collected, acute NGAL concentrations were higher in those with single UTIs (825 μg/g creatinine; 95% CI, 348–1070; IQR, 342–1133) compared with controls (133 μg/g creatinine; IQR, 115, 194; p < 0.05), although there was no difference between those with recurrent UTIs (729 μg/g creatinine; 95% CI, 220–2009; IQR, 307–1429) and controls. There was no difference in the follow-up urine NGAL concentration between groups. Patients in the single UTI group (282 ng/mL; 95% CI, 92–662; IQR, 88, 670) had a greater difference in the non-normalized NGAL as compare with controls (− 14 ng/mL; IQR, − 45, 14; p = 0.03), but this difference did not persist when NGAL was normalized to urine creatinine. No other differences between acute and follow-up NGAL concentrations between the groups were present (Table 3). There was no correlation between follow-up urine NGAL concentrations and the number of days between the acute and follow-up measurements (standardized by urine creatinine, R2 = 0.01, non-standardized by urine creatinine R2 = 0.07).
There was no difference between median non-standardized NGAL concentrations between patients with non-febrile and febrile UTIs (non-febrile 395 ng/mL; 95% CI, 200–45; IQR, 128, 507; febrile 454 ng/ml; 95% CI, 349–650; IQR, 227, 833; p = 0.12). However, there was a difference in the median standardized NGAL concentrations between non-febrile and febrile UTIs (standardized 461 μg/g creatinine; 95% CI, 325–817; IQR, 268, 841; 1036 μg/g creatinine; 95% CI, 767–1580; IQR, 613, 2945; p < 0.01). There was also a difference in the median urine creatinine levels between those with non-febrile versus febrile UTIs (non-febrile 66 mg/dL; 95% CI, 51–92; IQR, 36, 96; febrile 43 mg/dL; 95% CI, 37–56; IQR, 24, 77; p = 0.04).
We performed an area under the receiver operating curve (AUC) for the outcome of positive urine culture in this group of children with both signs and symptoms of UTI. The AUC was 0.95 (0.89–1.0) for urine NGAL not standardized by urine creatinine and 0.96 (0.91–1.0) for urine NGAL standardized by urine creatinine. At a cut-off of 269 μg/g creatinine, NGAL has a sensitivity of 1.0 and specificity of 0.84 for a positive urine culture. We repeated the AUC for the outcome of positive urine culture in the subset of patients who presented with fever. In this subset, the AUC for urine NGAL not standardized by urine creatinine was 0.96 (0.89–1.0) and 0.98 (0.94–1.0) for urine NGAL standardized by urine creatinine. At a cut-off of 272 μg/g creatinine, NGAL has a sensitivity of 0.90 and specificity of 1.0 for a positive urine culture in the subset of febrile patients. Among the subset of febrile patients, none of the urine NGAL measurements (acute, baseline, delta, standardized, non-standardized) had an AUC that suggested the marker had utility for the prediction of recurrent UTI. This was confirmed by logistic regression, in which urine NGAL was not a significant predictor of recurrent UTI.
Discussion
We sought to determine if there were differences in urine NGAL concentrations between girls with single and recurrent UTIs. We did not find a difference in either the acute or follow-up NGAL concentrations between patients with single and recurrent UTIs. We did find that patients who presented to the emergency department with symptoms and urinalysis results suggestive of UTI, but with negative cultures, had urine NGAL concentrations that were lower than those with a validated UTI. Accordingly, we report that urine NGAL can be a sensitive marker of positive urine culture among girls who present to the emergency department with signs and symptoms of a UTI. This suggests that comparing urine NGAL to age- and gender-based normal levels [17] may have a role in determining when to prescribe or, more importantly, to avoid prescribing antibiotics for girls who present for evaluation of UTI.
NGAL has multiple functions within the urinary tract, one of which includes chelating urinary iron [15]. By competing with gram-negative bacteria for this urinary iron, NGAL exerts a local bacteriostatic effect. During an acute UTI, NGAL is produced by the alpha-intercalated cells in the kidney in response to lipopolysaccharide [21], supporting its use as a marker of UTI. Further, NGAL levels decrease rapidly after resolution of infection, further supporting its utility as an acute marker [21, 22]. Urine NGAL has demonstrated utility as a marker of UTI in several clinical studies, including adults, children, and children with neuropathic bladders [23,24,25]. Given the role of NGAL in the innate immune system of the urinary tract, we hypothesized that a localized deficiency of NGAL would manifest as a phenotype of recurrent UTIs. This has been demonstrated in mice, in which NGAL knock-out mice demonstrate decreased clearance of bacteriuria following transurethral inoculation compared with controls [21, 22]. A small pilot study of children with recurrent UTI supported the hypothesis that some children with UTI may have a relative deficiency of uNGAL [16]. However, the data we present here do not support this prior study, as we do not report any data to suggest patients with recurrent UTI have different NGAL concentrations compared with patients without recurrent UTI. Indeed, in our cohort, 40% of the children in the recurrent UTI groups had values that were below the median of 15 ng/ml reported in the prior work, compared with 42% of children in the single UTI group. Further, there was only one patient who had an acute NGAL below 15 ng/ml, which was from a control patient.
There are several reasons that may partially explain the lack of concordance between our results and those previously reported. First, the patients with recurrent UTI in the prior study were recruited from a subspecialty clinic in which patients did not have factors such as bowel and bladder dysfunction that contribute to an increased risk of UTI [26]. Conversely, we recruited a broader population of children with recurrent UTI and may not have been able to identify the various reasons for recurrent UTI. However, a more likely reason for these discordant results is the choice of controls used in each study. In the prior work, controls were children without history of UTI who had a urine sample sent in the emergency department, but did not have a UTI. In this work, our comparators were children presenting with a single UTI and those who had signs and symptoms of UTI, but did not have positive urine cultures. Finally, we limited the ages of patients in this work, while the prior work had a wider range of ages. Given that urine NGAL changes with age, the larger range of ages in the prior work may partially account for these differences [17].
The intended comparator group in this work was patients with single UTIs. However, we discovered that some patients who had signs and symptoms of UTI, and were diagnosed and treated as such, ultimately had negative urine cultures. Such antibiotic prescribing is consistent with previous data demonstrating that up to 40% of children given antibiotics for UTI during an acute visit ultimately have negative urine cultures [27]. Therefore, we consented and collected urine samples from several patients who ultimately had negative urine cultures. We changed our consent process after this discovery so that we only contacted families once the urine culture became positive. The altered consent process, which required the research team to contact patients by phone, limited our ability to consent a large portion of eligible patients, as many families did not answer the phone when contacted. However, these initial samples allowed an unplanned opportunity to determine the utility of NGAL to identify children with signs and symptoms of UTI who ultimately have negative urine cultures. We found that NGAL is a highly sensitive marker of UTI in this cohort of children with signs and symptoms of UTI. However, we had a low number of patients in this unexpected control group, and these results need to be confirmed in a larger cohort of patients.
We did not differentiate between cystitis and pyelonephritis in this work as not all patients received the imaging necessary to accurately make this distinction. We were, however, able to compare patients in our cohort who had febrile versus non-febrile UTI and did not find a difference in the non-standardized NGAL concentrations. While there was a difference in the standardized NGAL, this is likely driven by the lower levels of urine creatinine in the febrile children, which would then cause an increase in the NGAL concentrations. Prior work in a small number of children suggests that urine NGAL can differentiate cystitis from pyelonephritis [28]. Although we were not able to directly compare our results given our inability to differentiate pyelonephritis from cystitis, our data does not suggest a difference in urine NGAL between non-febrile and febrile UTIs.
Limitations of this work include a low rate of return of follow-up samples, which limit the power of the analysis of the follow-up urine NGAL concentrations, the small number of patients in the control group, inability to differentiate cystitis from pyelonephritis, and the single-center design of this study. Further, we only included girls in this study, which may limit the generalizability of these results. Additionally, only a subset of the patients included in this study had imaging of the urinary tract, and therefore the urological status of each child is not known. There is also the possibility that patients in the single UTI group had prior UTIs that were not reported by the parents or discerned from the EHR or had future UTIs that did not occur within the follow-up period. Finally, we included a small number of control patients. However, despite these limitations, we believe these results provide data suggesting that in a general population of children with recurrent UTI, urine NGAL cannot identify those who may have a deficiency of NGAL as a contributor in the pathogenesis of their recurrent infections.
Conclusion
We did not show a difference in either acute or follow-up urine NGAL concentrations between girls with single and recurrent UTIs. We do show that urine NGAL is a sensitive marker of positive urine cultures in a cohort of girls presenting with signs and symptoms of UTI. While a deficiency in NGAL may exist and contribute to an individual’s risk of UTI, our data does not support this in a more generalized population of girls with recurrent UTI.
References
Conway PH, Cnaan A, Zaoutis T, Henry BV, Grundmeier RW, Keren R (2007) Recurrent urinary tract infections in children: risk factors and association with prophylactic antimicrobials. JAMA 298:179–186. https://doi.org/10.1001/jama.298.2.179
Shaikh N, Ewing AL, Bhatnagar S, Hoberman A (2010) Risk of renal scarring in children with a first urinary tract infection: a systematic review. Pediatrics 126:1084–1091. https://doi.org/10.1542/peds.2010-0685
Brandström P, Jodal U, Sillén U, Hansson S (2011) The Swedish reflux trial: review of a randomized, controlled trial in children with dilating vesicoureteral reflux. J Pediatr Urol 7:594–600. https://doi.org/10.1016/j.jpurol.2011.05.006
Shaikh N, Hoberman A, Keren R, Gotman N, Docimo SG, Mathews R, Bhatnagar S, Ivanova A, Mattoo TK, Moxey-Mims M, Carpenter MA, Pohl HG, Greenfield S (2016) Recurrent urinary tract infections in children with bladder and bowel dysfunction. Pediatrics 137:1–7. https://doi.org/10.1542/peds.2015-2982
Hewitt IK, Pennesi M, Morello W, Ronfani L, Montini G (2017) Antibiotic prophylaxis for urinary tract infection-related renal scarring: a systematic review. Pediatrics 139:e20163145. https://doi.org/10.1542/peds.2016-3145
Hoberman A, Greenfield SP, Mattoo TK, Keren R, Mathews R, Pohl HG, Kropp BP, Skoog SJ, Nelson CP, Moxey-Mims M, Chesney RW, Carpenter MA (2014) Antimicrobial prophylaxis for children with vesicoureteral reflux. N Engl J Med 370:2367–2376. https://doi.org/10.1056/NEJMoa1401811
Bachur R, Harper MB (2001) Reliability of the urinalysis for predicting urinary tract infections in young febrile children. Arch Pediatr Adolesc Med 155:60. https://doi.org/10.1001/archpedi.155.1.60
Shaikh N, Morone NE, Bost JE, Farrell MH (2008) Prevalence of urinary tract infection in childhood: a meta-analysis. Pediatr Infect Dis J 27:302–308. https://doi.org/10.1097/INF.0b013e31815e4122
Uhari M, Nuutinen M (1988) Epidemiology of symptomatic infections of the urinary tract in children. BMJ 297:450–452. https://doi.org/10.1136/bmj.297.6646.450
Winberg J, Andersen HJ, Bergström T, Jacobsson B, Larson H, Lincoln K (1974) Epidemiology of symptomatic urinary tract infection in childhood. Acta Paediatr 63:1–20. https://doi.org/10.1111/j.1651-2227.1974.tb05718.x
Yeunug CK, Godley ML, Dhillon HK, Gordon I, Duffy PG, Ransley PG (1997) The characteristics of primary vesico-ureteric reflux in male and female infants with pre-natal hydronephrosis. Br J Urol 80:319–327. https://doi.org/10.1046/j.1464-410x.1997.00309.x
Wennerström M, Hansson S, Jodal U, Stokland E (2000) Primary and acquired renal scarring in boys and girls with urinary tract infection. J Pediatr 136:30–34. https://doi.org/10.1016/S0022-3476(00)90045-3
Zaki M, Badawi M, Al Mutari G, Ramadan D, Adul Rahman M (2005) Acute pyelonephritis and renal scarring in Kuwaiti children: a follow-up study using 99mTc DMSA renal scintigraphy. Pediatr Nephrol 20:1116–1119. https://doi.org/10.1007/s00467-005-1880-2
Swerkersson S, Jodal U, Sixt R, Stokland E, Hansson S (2017) Urinary tract infection in small children: the evolution of renal damage over time. Pediatr Nephrol 32:1907–1913. https://doi.org/10.1007/s00467-017-3705-5
Schmidt-Ott KM, Mori K, Li JY, Kalandadze A, Cohen DJ, Devarajan P, Barasch J (2007) Dual action of neutrophil gelatinase-associated lipocalin. J Am Soc Nephrol 18:407–413. https://doi.org/10.1681/ASN.2006080882
Forster CS, Johnson K, Patel V, Wax R, Rodig N, Barasch J, Bachur R, Lee RS (2017) Urinary NGAL deficiency in recurrent urinary tract infections. Pediatr Nephrol 32:1077–1080. https://doi.org/10.1007/s00467-017-3607-6
Bennett MR, Nehus E, Haffner C, Ma Q, Devarajan P (2014) Pediatric reference ranges for acute kidney injury biomarkers. Pediatr Nephrol 30:677–685. https://doi.org/10.1007/s00467-014-2989-y
Roberts KB, Downs SM, Finell SME, Hellerstein S, Shortliffe LD, Wald ER, Zerin JM (2011) Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics 128:595–610. https://doi.org/10.1542/peds.2011-1330
Team RC (2017) R: a language and environment for statistical computing. R Foundation for Stastitical Computing, Vienna, Austria. https://www.r-project.org
Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez J-C, Müller M (2011) pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics 12:77. https://doi.org/10.1186/1471-2105-12-77
Paragas N, Kulkarni R, Werth M, Schmidt-Ott KM, Forster CS, Deng R, Zhang Q, Singer E, Klose AD, Shen TH, Francis KP, Ray S, Vijayakumar S, Seward S, Bovino ME, Xu K, Takabe Y, Amaral FE, Mohan S, Wax R, Corbin K, Sanna-Cherchi S, Mori K, Johnson L, Nickolas T, D’Agati V, Lin CS, Qiu A, Al-Awqati Q, Ratner AJ, Barasch J (2014) α-Intercalated cells defend the urinary system from bacterial infection. J Clin Invest 124:2963–2976. https://doi.org/10.1172/JCI71630
Steigedal M, Marstad A, Haug M, Damas JK, Strong RK, Roberts PL, Himpsl SD, Stapleton A, Hooton TM, Mobley HLT, Hawn TR, Flo TH (2014) Lipocalin 2 imparts selective pressure on bacterial growth in the bladder and is elevated in women with urinary tract infection. J Immunol 193:6081–6089. https://doi.org/10.4049/jimmunol.1401528
Price JR, Guran L, Lim JY, Megli CJ, Clark AL, Edwards SR, Denman MA, Gregory WT (2017) Neutrophil gelatinase–associated lipocalin biomarker and urinary tract infections. Female Pelvic Med Reconstr Surg 23:101–107. https://doi.org/10.1097/SPV.0000000000000366
Hatipoglu S, Sevketoglu E, Gedikbasi A, Yilmaz A, Kiyak A, Mulazimoglu M, Aydogan G, Ozpacaci T (2011) Urinary MMP-9/NGAL complex in children with acute cystitis. Pediatr Nephrol 26:1263–1268. https://doi.org/10.1007/s00467-011-1856-3
Forster CS, Jackson E, Ma Q, Bennett M, Shah SS, Goldstein SL (2018) Predictive ability of NGAL in identifying urinary tract infection in children with neurogenic bladders. Pediatr Nephrol 33:1365–1374. https://doi.org/10.1007/s00467-018-3936-0
Shaikh N, Hoberman A, Wise B, Kurs-Lasky M, Kearney D, Naylor S, Ann Haralam M, Colborn DK, Docimo SG (2003) Dysfunctional elimination syndrome: is it related to urinary tract infection or vesicoureteral reflux diagnosed early in life? Pediatrics 112:1134–1137. https://doi.org/10.1542/peds.112.5.1134
Saha D, Patel J, Buckingham D, Thornton D, Barber T, Watson JR (2017) Urine culture follow-up and antimicrobial stewardship in a pediatric urgent care network. Pediatrics 139:e20162103. https://doi.org/10.1542/peds.2016-2103
Arambašić J, Mandić S, Debeljak Z, Mandić D, Horvat V, Šerić V (2016) Differentiation of acute pyelonephritis from other febrile states in children using urinary neutrophil gelatinase-associated lipocalin (uNGAL). Clin Chem Lab Med 54:55–61. https://doi.org/10.1515/cclm-2015-0377
Acknowledgments
This work supported The Gerber Foundation. The funder did not have any role in either study design, data collection, interpretation, or analysis, the writing of this report, or the decision to submit this report for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This work was approved by the Cincinnati Children’s Hospital Institutional Review Board. Written informed consent was obtained from parents or guardians for participation in this study. All data is available from the corresponding author upon reasonable request.
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Forster, C.S., Loechtenfeldt, A.M., Shah, S.S. et al. Urine neutrophil gelatinase-associated lipocalin in girls with recurrent urinary tract infections. Pediatr Nephrol 35, 2121–2128 (2020). https://doi.org/10.1007/s00467-020-04654-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04654-9