Abstract
Background
Although recent studies have shown that more than half of children with steroid-dependent nephrotic syndrome (SDNS) may continue to have active disease beyond childhood, the long-term outcome in this cohort treated with mycophenolate mofetil (MMF) after cyclosporine remains unknown, particularly in adulthood.
Methods
We conducted a retrospective study of 44 adult patients (median age, 22.3 years) who received MMF for complicated SDNS (median age at MMF initiation, 13.3 years) at a single center. Complicated SDNS was defined as the case continuing to relapse after cyclosporine (CsA) treatment. When patients experienced relapses despite MMF initiation, they additionally received a rituximab infusion. The primary endpoint was the probability of achieving treatment-free remission for > 2 years.
Results
Prior to MMF initiation, all patients received CsA for a median of 46 months and 19 received the 12-week cyclophosphamide. After switching from CsA to MMF, only four patients did not relapse during a median follow-up period of 9.6 years. At the last visit, only 15 of the 44 patients achieved treatment-free sustained remission. Multivariate analysis revealed that young age (< 6 years) at onset of nephrotic syndrome (odds ratio, 11.3) and the experience of steroid dependency during initial CsA treatment (odds ratio, 29.8) were the independent risk factors of active disease into adulthood after MMF initiation.
Conclusions
Although none developed renal insufficiency and severe adverse effects of therapy, the introduction of MMF after CsA treatment may not be necessarily associated with improved long-term outcome of children with complicated SDNS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although most children with minimal change nephrotic syndrome (MCNS) respond to steroids, approximately 50% of the patients develop frequent relapsing and/or steroid-dependent nephrotic syndrome (FR/SDNS). Despite the development of various effective steroid-sparing agents (SPA), recent surveys in the post-cyclosporine (CsA) era have revealed a high incidence of relapses beyond childhood in this cohort [1, 2]. At present, there is no consensus regarding first-line SPA for children with FR/SDNS.
In the last decade, several prospective studies, including ours, demonstrated the efficacy of mycophenolate mofetil (MMF) in preventing relapses in children with FR/SDNS [3,4,5], but without severe adverse effects such as CsA-induced nephrotoxicity. Furthermore, a recent randomized crossover study showed that prior CsA treatment was associated with higher efficacy of MMF in a subsequent treatment, potentially due to a carry-over effect from the initial CsA treatment [6]. However, the long-term outcome of patients after switching from CsA to MMF is lacking, especially in adulthood.
In the present study, we investigated the long-term outcome of children with SDNS who had received MMF after CsA treatment, as well as the risk factors of active disease into adulthood after the initiation of MMF.
Methods
Patients
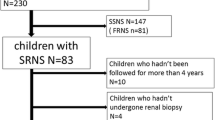
We retrospectively reviewed the medical records of 44 adult patients (> 18 years) with childhood-onset biopsy-proven MCNS who were treated with MMF at Saitama Children’s Medical Center. Prior to MMF treatment, all patients continued to have nephrotic syndrome (NS) relapses after CsA treatment (median duration, 42 months) and subsequently, MMF treatment was initiated between March 2005 and April 2014. The results from the short-term clinical course of 18 patients have been reported previously [7]. The patients with genetic steroid-resistant nephrotic syndrome (SRNS) were excluded from this study.
In this study, the definitions and criteria adopted for NS, complete remission, relapse, frequent relapse, and steroid dependency followed the clinical practice guideline for pediatric idiopathic NS in Japan [8]. Complicated SDNS was defined as the case continuing to relapse after CsA initiation. Treatment-free sustained remission was defined as the case achieving > 2-year remission without any treatment. All patients and their parents provided written informed consent. The ethics committee of the Saitama Children’s Medical Center approved the use of MMF and rituximab (RTX) in patients with complicated SDNS in this study (approval numbers, 2004-04-006, 2007-03-001).
Treatment
Before MMF initiation, all patients had received CsA treatment (Neoral, oral formulation, Novartis Pharma Co., Tokyo, Japan) for > 18 months and CPM (Endoxan, oral formulation, Shionogi Co., Osaka, Japan) was also administered at 2–2.5 mg/kg/day for 12 weeks (cumulative dose, 200 mg/kg) in 19 of the 44 patients. For patients with complicated SDNS after CsA treatment, MMF (CellCept, oral formulation, Chugai Co., Tokyo, Japan) was administered after patients achieved complete remission with prednisolone (PSL). As per the therapeutic protocol, MMF was introduced at an initial dose of 250 mg/12 h and adjusted to maintain a target pre-dose mycophenolic acid (MPA) level of 2 to 5 μg/mL (maximum 1 g twice daily), in accordance with previously reported findings [3]. Plasma MPA was measured by using an enzyme-mediated immune technique (Special Reference Laboratory; SRL Inc.). After MMF initiation, CsA was gradually tapered off at a dose of 50–100 mg every 4 weeks. For patients who were able to achieve PSL-free remission for > 1 year, MMF was gradually tapered off. Relapses were treated with PSL 2 mg/kg/day until proteinuria was undetectable for ≥ 3 consecutive days. PSL was administered on alternate days thereafter, and the dose was tapered off within 6 months at a rate of 5–10 mg every 2–4 weeks. When patients experienced multiple relapses of NS after MMF discontinuation, those with CsA-induced nephrotoxicity were re-treated with MMF and those without nephrotoxicity were re-treated with CsA. CsA was adjusted to maintain a 2-h post-dose CsA level of 400–600 ng/mL (maximum 75 mg twice daily). Since December 2007, RTX infusion (Rituxan, injection, Zenyaku Co., Tokyo, Japan) has been additionally administered when patients developed any condition requiring > 0.5 mg/kg or > 15 mg PSL on alternate days to maintain remission, despite treatment with MMF or CsA. According to the therapeutic protocol reported previously [9], RTX was intravenously administered in a single dose of 375 mg/m2 (maximum, 500 mg) during a proteinuria-free period. The primary endpoint was the probability of achieving treatment-free sustained remission.
Statistical analysis
Categorical variables were compared using chi-square or Fisher’s exact test as appropriate and were reported as frequencies and percentages. Unless indicated otherwise, continuous variables were expressed as median (range). Parametric two-sample t test or non-parametric Mann–Whitney U test were used as appropriate for comparing continuous variables. Logistic regression was used to identify an independent risk factor for active disease into adulthood. Kaplan–Meier curves depicted the percentage of patients achieving > 2-year remission without any treatment after MMF initiation. In all analyses, p values < 0.05 were considered to indicate statistical significance.
Results
The median age at NS diagnosis was 6.5 years (range, 1.4–13.5). Patients developed SDNS (n = 32) or initial SRNS (n = 12) and had received CsA at a median age of 8.9 years (range, 1.5–13.6) for a median of 46 months (range, 18–125). Although all patients with initial SRNS had a histologic diagnosis of MCNS and achieved complete remission after CsA initiation, they subsequently developed complicated SDNS. Despite the initiation of CsA treatment, 25 patients continued to have SDNS and 7 patients had received RTX before MMF initiation. The median age at MMF initiation was 13.3 years (range, 5.7–21.6; interquartile range, 10.5–14.4) and the median MMF dose required was 870 mg/m2 (interquartile range, 780–990), which maintained median pre-dose MPA levels of 2.9 μg/mL (interquartile range, 2.3–3.6) during the initial MMF treatment (median duration, 27 months; interquartile range, 19–47). During the median follow-up period after MMF initiation (median, 9.6 years; range, 4.6–13.7; interquartile range, 7.6–12.5), only four of the 44 patients did not relapse, while the remaining 40 had relapsed. Seventeen patients had an experience of SDNS during the initial treatment with MMF and 29 patients developed SDNS again after MMF discontinuation. Thus, re-treatment with MMF, CsA, and both MMF and CsA were required in 14, 2, and 13 patients, respectively. In addition, 26 patients received RTX after MMF initiation. Post-treatment renal biopsies were performed in all but one patient; 18 of the 43 patients showed evidence of CsA-induced nephrotoxicity defined by tubulointerstitial lesions.
At the last visit (median age, 22.3 years), 15 patients achieved treatment-free sustained remission (Group A), whereas 22 patients continued to receive immunosuppressive agents and/or RTX (MMF 12 patients; CsA 4 patients; RTX, 9 patients), and seven patients had treatment-free remission within 2 years (Group B, active disease into adulthood). Table 1 summarizes the clinical characteristics of the patients in both groups. Univariate analysis showed that the risk of active disease in adulthood (group B) was positively associated with young age at onset, young age at the initiation of CsA or MMF, and the experience of steroid dependency during CsA or MMF treatment. Multivariate analysis revealed that young age (< 6 years) at NS onset (odds ratio, 11.6; 95% confidence interval 1.05–127.8; P = 0.045) and the experience of steroid dependency during initial CsA treatment (odds ratio, 29.8; 95% confidence interval 3.3–270.5, P = 0.003) were independent risk factors of active disease into adulthood after the initiation of MMF. All patients who had these two risk factors (N = 14) continued active disease into adulthood. Only in 32 SDNS patients, excluding initial 12 SRNS patients, multivariate analysis also revealed that the experience of steroid dependency during initial CsA treatment (odds ratio, 11.1; 95% confidence interval 1.06–116.5, P = 0.045) was the independent risk factor of active disease into adulthood after the initiation of MMF. Kaplan–Meier curves revealed that the percentage of treatment-free sustained remission after MMF initiation was significantly lower in patients who had the experience of steroid dependency during initial CsA treatment than in those who did not have this experience (Supplementary Fig. 1, p < 0.001). Median MMF treatment duration was not statistically significant between the patients with and without this experience (31 vs. 26 months), and median number of relapses before sustained remission was 2 (range, 0–8) in Group A. At the last follow-up, although six patients (20%) in Group A received antihypertensive agents, all patients maintained complete remission of NS and none developed chronic kidney disease (CKD) stage ≥ 2. The mean SD score for height was − 0.5 ± 1.1 and short stature (below – 2SD) developed in four patients (minimum − 3.4 SD). All four patients with short stature at the last visit received RTX after puberty. At the time of RTX infusion, they already were below – 2SD.
We also performed stratification analysis between 12 SRNS and 32 SDNS patients at the initial disease onset. No significant differences in clinical characteristics, such as sex, age at NS onset, age at CsA or MMF initiation, the rate of CPM or RTX administration, and an experience of SDNS during CsA or MMF treatment, were observed between SRNS and SDNS patients. At the last visit, treatment-free remission was achieved in five of the 12 SRNS and 17 of the 32 SDNS patients, respectively, and the difference was not statistically significant. The rates of hypertension, short stature, and CsA-induced nephrotoxicity in the initial SRNS patients were relatively high compared with those in the SDNS patients, although these differences were not statistically significant (3/12 vs. 3/32, 3/12 vs. 1/32, and 7/11 vs. 11/32, respectively).
Discussion
This retrospective analysis of patients with childhood-onset MCNS who received MMF after CsA treatment shows that young age at NS onset and the experience of steroid dependency during initial CsA treatment were significant risk factors for active disease in adulthood. Using a homogenous treatment protocol in this single-center study, 44 adults had not developed CKD stage ≥ 2 at the last visit, but the rate of persistent disease into adulthood in this cohort was very high. The main strength of our study is the 10-year follow-up period after MMF initiation, whereas the observation period in previous studies was limited to <5 years [10, 11].
Further, previous follow-up studies have shown that MMF initiation allowed > 50% of patients with SDNS to avoid further SPA or to maintain remission without treatment at last visit. Banerjee et al. reported the outcome of 46 Indian patients with SDNS treated with MMF after treatment with levamisole and cyclophosphamide before MMF initiation [10]. Although the authors showed that 25 of these patients (54%) required no alternative SPA after MMF initiation, their follow-up period was relatively short (mean duration, 3.56 years) and sustained remission after MMF discontinuation was achieved in only eight of the 46 patients at last follow-up. More recently, Dehoux et al. conducted a retrospective study of 96 French children with SDNS followed for 4.7 years after MMF initiation [11]. Although they showed that 58 of the 96 patients (60%) were in remission without treatment at the last follow-up, most of these patients had received additional treatments such as RTX (38/58) and levamisole (4/58) after MMF initiation and only six patients did not relapse after MMF discontinuation. Thus, the authors concluded that MMF had no disruptive effect on the disease. In addition, because the included patients in our study were a more severe group: 12 of 44 were initially steroid resistant and 25 were still steroid dependent on CsA treatment, two-thirds of the patients were not able to achieve sustained remission at the last follow-up. Based on these findings, MMF as well as CsA may not have exerted a curative effect in children with SDNS; a significant number of this cohort may continue to relapse into adulthood.
In a long-term follow-up study after initial 2-year CsA treatment, Ishikura et al. noted that half of the patients (mean age, 18.7 years) continued to relapse frequently or received SPA at last observation, but none received MMF during the follow-up period [12]. Similar to our findings, Ishikura et al. found an association between NS relapse during initial CsA treatment and poor outcome at last observation. We identified that the experience of steroid dependency during initial CsA treatment was an independent risk factor of active disease into adulthood after MMF initiation. These data suggest that the identification of transition into adulthood with initial CsA treatment early in the disease course may allow appropriate counsel for patients and their families; appropriate timing of SPA and RTX may be instituted for severe forms of SDNS and thereby reduce morbidity associated with PSL and multiple relapses of NS.
Our finding that young age at NS onset (< 6 years) was a risk factor of active disease in adulthood is supported by results of previous follow-up studies in the pre-MMF era [1, 13]. While Dehoux et al. demonstrated that MMF was more effective when patients were treated at a younger age (< 6 years) [11], the age at MMF initiation was ≥ 6 years in all but one patient in our study. Therefore, additional studies are warranted to understand the long-term outcome of children < 6 years who were treated with MMF early in the disease course. It should nevertheless be borne in mind that the use of MMF at the time of febrile infection was a risk factor for hospitalization, especially in young patients, as we previously reported [14].
Previous studies demonstrated that children at younger age were at a greater risk for low MPA levels due to faster clearance, even when dosing per body surface area and may thus require higher doses of MMF [15, 16]. In our study, the age at MMF initiation was significantly younger in Group B than in Group A, which may contribute to significantly higher doses of MMF being required in Group B than in Group A to maintain target pre-dose MPA levels of approximately 3 μg/mL.
In conclusion, in this study, we have established that MMF initiation after CsA treatment may not be necessarily associated with improved long-term outcome of children with SDNS, when compared with data obtained prior to the advent of CsA and MMF [13, 17]. Although renal outcome itself of our patients with complicated SDNS, including initial SRNS, was favorable, these results imply that the development of novel treatment strategies to prevent active disease into adulthood is urgently required, especially for patients with the risk factors of persistent active disease. Our study is not without limitations. First, this was a retrospective single-center study, although data were collected in a prospective manner. Second, the number of patients in our study was too small to draw robust conclusions. Third, the duration of MMF treatment, age at MMF initiation, and the follow-up periods varied largely among our patients. However, to the best of our knowledge, our study is the longest follow-up period after MMF initiation (median 9.6 years) and the therapeutic protocol regarding use of both PSL and SPA was relatively homogeneous, compared with those of previous studies. Future prospective studies are needed to determine the suitable timing of MMF initiation for children with SDNS.
References
Fakhouri F, Bocquet N, Taupin P, Presne C, Gagnadoux MF, Landais P, Lesavre P, Chauveau D, Knebelmann B, Broyer M, Grünfeld JP, Niaudet P (2003) Steroid-sensitive nephrotic syndrome: from childhood to adulthood. Am J Kidney Dis 41:550–557
Rüth EM, Kemper MJ, Leumann EP, Laube GF, Neuhaus TJ (2005) Children with steroid-sensitive nephrotic syndrome come of age: long-term outcome. J Pediatr 147:202–207
Fujinaga S, Ohtomo Y, Umino D, Takemoto M, Shimizu T, Yamashiro Y, Kaneko K (2007) A prospective study on the use of mycophenolate mofetil in children with cyclosporine-dependent nephrotic syndrome. Pediatr Nephrol 22:71–76
Dorresteijn EM, Kist-van Holthe JE, Levtchenko EN, Nauta J, Hop WC, van der Heijden AJ (2008) Mycophenolate mofetil versus cyclosporine for remission maintenance in nephrotic syndrome. Pediatr Nephrol 23:2013–2020
Baudouin V, Alberti C, Lapeyraque A-L, Bensman A, André JL, Broux F, Cailliez M, Decramer S, Niaudet P, Deschênes G, Jacqz-Aigrain E, Loirat C (2012) Mycophenolate mofetil for steroid-dependent nephrotic syndrome: a phase II Bayesian trial. Pediatr Nephrol 27:389–396
Gellermann J, Weber L, Pape L, Tönshoff B, Hoyer P, Querfeld U (2013) Mycophenolate mofetil versus cyclosporin A in children with frequently relapsing nephrotic syndrome. J Am Soc Nephrol 24:1689–1697
Fujinaga S, Sakuraya K, Yamada A, Urushihara Y, Ohtomo Y, Shimizu T (2015) Positive role of rituximab in switching from cyclosporine to mycophenolate mofetil for children with high-dose steroid-dependent nephrotic syndrome. Pediatr Nephrol 30:687–691
Ishikura K, Matsumoto S, Sako M, Tsuruga K, Nakanishi K, Kamei K, Saito H, Fujinaga S, Hamasaki Y, Chikamoto H, Ohtsuka Y, Komatsu Y, Ohta T, Nagai T, Kaito H, Kondo S, Ikezumi Y, Tanaka S, Kaku Y, Iijima K, Japanese Society for Pediatric Nephrology; Japanese Society for Pediatric Nephrology (2015) Clinical practice guideline for pediatric idiopathic nephrotic syndrome 2013: medical therapy. Clin Exp Nephrol 19:6–33
Fujinaga S, Hirano D, Nishizaki N, Kamei K, Ito S, Ohtomo Y, Shimizu T, Kaneko K (2010) Single infusion of rituximab for persistent steroid-dependent minimal-change nephrotic syndrome after long-term cyclosporine. Pediatr Nephrol 25:539–544
Banerjee S, Pahari A, Sengupta J, Patnaik SK (2013) Outcome of severe steroid-dependent nephrotic syndrome treated with mycophenolate mofetil. Pediatr Nephrol 28:93–97
Dehoux L, Hogan J, Dossier C, Fila M, Niel O, Maisin A, Macher MA, Kwon T, Baudouin V, Deschênes G (2016) Mycophenolate mofetil in steroid-dependent idiopathic nephrotic syndrome. Pediatr Nephrol 31:2095–2101
Ishikura K, Yoshikawa N, Nakazato H, Sasaki S, Nakanishi K, Matsuyama T, Ito S, Hamasaki Y, Yata N, Ando T, Iijima K, Honda M, Japanese Study Group of Renal Disease in Children (2015) Morbidity in children with frequently relapsing nephrosis: 10-year follow-up of a randomized controlled trial. Pediatr Nephrol 30:459–468
Trompeter RS, Lloyd BW, Hicks J, White RH, Cameron JS (1985) Long-term outcome for children with minimal-change nephrotic syndrome. Lancet 16:368–370
Fujinaga S, Sakuraya K (2018) Should mycophenolate mofetil be administered prior to cyclosporine A as a steroid-sparing agent to children with steroid-dependent nephrotic syndrome? Pediatr Nephrol 33:2389–2390
Yoo EC, Alvarez-Elías AC, Todorova EK, Filler G (2016) Developmental changes of MPA exposure in children. Pediatr Nephrol 31:975–982
Hibino S, Nagai T, Yamakawa S, Ito H, Tanaka K, Uemura O (2017) Pharmacokinetics of mycophenolic acid in children with clinically stable idiopathic nephrotic syndrome receiving cyclosporine. Clin Exp Nephrol 21:152–158
Lewis MA, Baildom EM, Davis N, Houston IB, Postlethwaite RJ (1989) Nephrotic syndrome: from toddlers to twenties. Lancet 4:255–259
Funding
SF has received clinical research funding B at Saitama Children’s Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and/or national research committee at which the study was conducted with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary Figure 1
(DOCX 58 kb)
Rights and permissions
About this article
Cite this article
Fujinaga, S., Hirano, D., Nishino, T. et al. Long-term outcome of Japanese children with complicated minimal change nephrotic syndrome treated with mycophenolate mofetil after cyclosporine. Pediatr Nephrol 34, 2417–2421 (2019). https://doi.org/10.1007/s00467-019-04339-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-019-04339-y