Abstract
Background
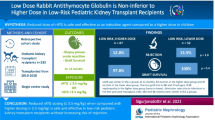
Chronic antibody-mediated rejection (cAMR) is the leading cause of late kidney graft loss, but current therapies are often ineffective. Rabbit anti-human thymocyte immunoglobulin (rATG) may be helpful, but its use is virtually undocumented.
Methods
Data were analyzed retrospectively from nine pediatric kidney transplant patients with cAMR were treated with rATG (1.5 mg/kg × 5 days) at our center after non-response to pulsed prednisolone, intravenous immunoglobulin, rituximab, and increased immunosuppressive intensity (including switching to belatacept in some cases), with or without bortezomib.
Results
The median time from diagnosis to cAMR was 179 days. rATG was started 5–741 days after diagnosis. Median estimated glomerular filtration rate (eGFR) increased from 40 mL/min/1.73 m2 when rATG was started to 62 mL/min/1.73 m2 9 months later (p = 0.039). Four patients showed substantially higher eGFR after 9 months and 2 patients showed a small improvement; eGFR continued to decline in 3 patients after starting rATG. No grafts were lost during follow-up. At last follow-up, donor-specific antibodies (DSAs) were no longer detectable in 4 out of 8 patients for whom data were available, median fluorescence intensity had decreased substantially in 1 out of 8 patients; anti-HLA DQ DSAs persisted in 2 out of 8 patients. No adverse events with a suspected relation to rATG, including allergic reactions, leukocytopenia or infections, were observed in any of the patients.
Conclusions
In this small series of patients, rATG appears a promising treatment for unresponsive cAMR. Further evaluation, including earlier introduction of rATG, is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The key role of antibodies in the immunological response to organ transplantation, which has been neglected for decades, has recently become more fully appreciated. Development of antibodies against alloantigens is central to the effector mechanisms of the adaptive immune system, and can culminate in chronic antibody-mediated rejection (cAMR) [1]. cAMR can follow a variable clinical course, with either subclinical or clinically evident proteinuria and gradual loss of graft function over several years [2, 3], but 15–20% of adult kidney grafts fail within the first year after diagnosis of AMR [4] and it is the leading cause of late kidney graft loss [5, 6]. The North American Pediatric Renal Trials and Collaborative Studies reported in 2014 that 50.7% of all graft failures are caused by rejection, with chronic rejection accounting for 35.8% of these failures, and it is likely that many of these were in fact AMR [7]. Data on the frequency of cAMR in children are lacking, but their relatively naïve immune system could potentially place them at even greater risk, compounded in adolescents by a high risk for non-adherence to the immunosuppressive regimen [8].
Chronic AMR has a complex pathophysiology. Donor-specific antibodies (DSAs) against human leukocyte antigen (HLA) play a central role in chronic graft deterioration [9], and post-transplant development of DSAs is associated with a higher risk for AMR and graft loss in adults [9, 10] and children [11]. cAMR is notoriously difficult to treat, particularly once it has progressed to transplant glomerulopathy, and few controlled studies have been conducted in this area [12]. In addition to maintaining or increasing the intensity of maintenance immunosuppression, treatment is aimed at eliminating the antibodies (notably DSAs) that have induced AMR and, second, to inhibit production of further antibodies by targeting of B-cells and plasma cells (the source of DSAs). A further approach is to inhibit the complement cascade. Removal of circulating DSAs is typically attempted using intravenous immunoglobulin G (IVIG) [13]. The addition of plasmapheresis, or immunoadsorption in the event of nonresponse to plasmapheresis, can be helpful. Randomized controlled trials in adults have shown that plasmapheresis removes 50% of antibodies, but rebound occurs and administration of IVIG increases response rate to 50–90% [14, 15]. However, extracorporeal therapy is a therapeutic challenge in small children. To deplete B-cells, the chimeric monoclonal anti-CD20 antibody rituximab is an established option for refractory AMR [6] but CD20-negative plasma cells are unaffected. Where cAMR does not respond to depletional agents, newer agents such as plasma-derived C1 esterase inhibitor [16] and the anti-interleukin-6 receptor antagonist tocilizumab [17] have shown promising results.
Rabbit anti-human thymocyte immunoglobulin (rATG) has a well-established role in induction therapy, but some centers also use rATG to suppress antibody production after diagnosis of cAMR following kidney [13] or heart [18] transplantation. In recent years, it has been recognized that rATG not only depletes T-cells—including the helper T-cells required to elicit a B-cell response to antibodies—but may also suppress memory and switch memory B-cell subpopulations [19,20,21,22,23]. The use of rATG to treat cAMR, however, is based only on tangential evidence from prophylactic applications: namely, that it prevents production of DSAs de novo post-transplant [24] and that it contributes to the effectiveness of pre-transplant desensitization protocols [25].
To our knowledge, experience of treating cAMR with rATG is virtually undocumented. We report here a retrospective analysis of nine pediatric kidney transplant patients in whom rATG was given at our center after a poor response to other therapeutic options.
Materials and methods
This was a retrospective review of cases from a single center (Department of Pediatric Nephrology, Hannover Medical School, Germany). Cases were identified from all patients who regularly attended the pediatric nephrology outpatient department between 2006 and 2016. Data were collected from medical records. As each case was classified as an “individual healing attempt” according to German law, no ethics approval was required.
During the study period, all patients received basiliximab induction therapy. The initial maintenance regimen comprised cyclosporine (CsA) with prednisolone. At week 4 post-transplant, the CsA trough concentration was halved and everolimus was started. If protocol biopsy at month 6 showed normal histology, prednisolone was tapered and discontinued [26]. Details of the immunosuppressive regimen, including dosing and target concentrations, have been published previously [27].
The panel reactive antibody (PRA) value was defined as the percentage of panel cells that reacted with patient serum in the complement-dependent cytotoxicity screening. HLA matches were calculated for the loci HLA-A, HLA-B, HLA-C, HLA-DR, and HLA-DQ at the time of organ allocation. For high-resolution typing, CTS-Sequence kits (Heidelberg, Germany) and Olerup-SSP kits (Saltsjöbaden, Sweden) were used. HLA antibodies were measured before engraftment and at least annually post-transplant, or if the glomerular filtration rate (GFR) decreased by more than 20% from baseline. Measurements were made using the LABScreen single-antigen beads Luminex kit (One Lambda, Canoga Park, CA, USA) which uses single HLA-coated beads and enables identification of IgG alloantibody specificities against HLA-A, -B, -C, -DRB1/3/4/5, -DQA1, -DQB1, -DPA1, and -DPB1 antigens. Because no clinically validated cut-off for the Luminex assay is recommended by the provider company, a mean fluorescence intensity of >1,000 was used to define the cut-off for antibody positivity as this appears to be predictive for adverse outcomes, including cAMR, following kidney transplantation [28,29,30]. Renal biopsy was performed if a patient was positive for DSAs according to this definition, and if estimated glomerular filtration rate (eGFR) decreased by >20%. cAMR was diagnosed according to the Banff 2013 criteria, combining pathological diagnosis and evidence for DSAs [31]. If cAMR was diagnosed, the initial treatment was six pulses of prednisolone (6 pulses of 300 mg/m2 body surface area [BSA]), weekly courses of IVIG starting on day 2 (1 g/kg × 4 doses), and between one and four monthly infusions of rituximab starting on day 6 (375 mg/m2 BSA), as described by Billing et al. [32]. If serum creatinine increased rapidly, the patient was given six sessions of immunoadsorption. If the patient had low trough concentrations of everolimus (<4 μg/l) or CsA (<60 mg/l) the dose was increased and, in steroid-free patients, prednisolone was re-started at a dose of 3 mg/m2 BSA. If trough concentrations of everolimus and CsA were adequate, CsA was changed to tacrolimus (trough concentration 8–10 mg/l) and/or everolimus was changed to mycophenolate mofetil (MMF). In cases of non-adherence to the calcineurin inhibitor (CNI) regimen—considered a likely cause of DSA development—patients were switched from CNI therapy to belatacept (with everolimus) if the patient agreed to continuous intravenous therapy [33]. Adherence was assessed by a combination of self-reporting and physician assessment. If graft function did not improve and the mean fluorescence values of DSAs did not decline in response to these interventions, bortezomib therapy was applied, as described by Walsh et al. [34]. Where graft function still showed progressive deterioration, or where the response was considered inadequate, rATG (Thymoglobulin®) was administered via a peripheral line at a dose of 1.5 mg/kg over 4 h for 5 consecutive days (total dose 7.5 mg/kg).
Renal function was assessed by eGFR using the Schwartz formula [35]. The ratio of urinary albumin/creatinine was measured as a marker for proteinuria. Renal data are reported for the 9 months before diagnosis of cAMR, at the time of cAMR diagnosis and the time of rATG introduction, and for the 9 months after start of rATG therapy. Data are shown only for post-transplant measurements, and thus 9 months of pre-rATG values are not included if cAMR was diagnosed less than 9 months after transplantation. Available data were too sparse for meaningful analysis at later time points, i.e., beyond 9 months.
Every 3 months, patients were monitored for Epstein–Barr virus (EBV), cytomegalovirus, and BK polyomas virus by polymer chain reaction (LightCycler®; Roche Diagnostics, Basel, Switzerland). Full blood counts were performed daily for 1 week post-transplant, then every 2 weeks. CD3 counts were not monitored.
As data were not normally distributed, results are primarily presented as median values and ranges. Mean values and standard variations were also determined. Statistical analysis was performed using the Mann–Whitney U test and p < 0.05 was defined as significant.
Results
Patient population and immunosuppression
Nine patients were assessed (3 female, 6 male), all of whom had received a first kidney transplant. Two patients received a living-donor graft (patients #2 and #6; patient #6 was transplanted pre-emptively). Key characteristics are shown in Table 1. All patients were followed for 9 months after the start of rATG therapy. All patients received induction with basiliximab, with an initial maintenance regimen comprising CsA and steroids. All patients were switched to low-exposure CNI therapy with CsA and everolimus at week 4 post-transplant (Table 2). In 1 patient, CsA was later switched to extended-release tacrolimus because of an episode of acute cellular rejection; the same patient was converted from everolimus to sirolimus to enable once-daily administration.
Diagnosis and management of cAMR
The median time between transplantation and diagnosis of cAMR was 179 days. Patients were a median age of 14.7 years at the time of diagnosis (Table 1). The pathological findings confirming diagnosis of active cAMR are summarized in Table 3. None of the patients underwent a repeat biopsy. Thrombotic microangiopathy was excluded in each case based on findings from clinically-indicated biopsies. In patients #4, #8, and #6, cellular rejection of BANFF grade Ia was also diagnosed, with cellular rejection BANFF grade Ib in patient #9. One patient (#8) did not fully meet the Banff 2013 criteria, as Luminex testing of DSAs was not available at the time of diagnosis. All 9 patients received pulsed prednisolone, four IVIG infusions, and rituximab. Additionally, 2 patients (#1 and #8) received immunoadsorption and bortezomib was given to 8 patients (all except patient #8, in whom post-transplant Luminex data on DSAs were unavailable).
Following diagnosis of cAMR, the immunosuppression regimen was modified in a tailored manner, by increasing CNI exposure or switching to tacrolimus, increasing mammalian target of rapamycin (mTOR) inhibitor exposure or, less frequently, introducing MMF (Table 2). Three patients (#2, #4, and #5) switched from CNI therapy to belatacept, all with everolimus. All 3 patients were considered non-adherent, and were EBV IgG-positive. The remaining 6 patients (patients #1, #3, #6, #7, #8, and #9) were considered to be adequately adherent to the immunosuppressive regimen.
Before the introduction of rATG, these interventions led to an improvement in eGFR in 3 patients (#4, #5, and #9), whereas eGFR continued to deteriorate in the other 6 patients. However, as the improvement in eGFR was only moderate in patients #4, #5, and #9, the decision was made to initiate rATG therapy in all cases. All patients received the planned five doses (total dose 7.5 mg/kg). The delay between diagnosis of cAMR and introduction of rATG ranged from 5 days to 741 days (Table 1). All patients received the full cumulative dose of rATG (7.5 mg/kg).
Donor-specific antibodies
None of the patients had pre-formed DSAs against HLA at the time of transplantation. At the time of cAMR diagnosis, 5 patients had DSAs against HLA-DQ, 1 against HLA-A, 1 against HLA-B, and 1 against both HLA-DQ and HLA-A (Table 1). At last follow-up, DSAs were no longer detectable in 4 patients. The median fluorescence intensity (MFI) level remained largely unchanged in 3 patients (#1, #3, and #7), all of whom had anti-HLA-DQ DSAs, and decreased to a clinically relevant extent [36] in 1 patient (#4; Table 1).
Graft function
Median eGFR declined from 100 (range 57–126) mL/min/1.73 m2 at 9 months before the cAMR diagnosis to 48 mL/min/1.73 m2 at the time of diagnosis, with a subsequent decrease to 40 (range 17–57) mL/min/1.73 m2 at the point of rATG introduction (Fig. 1). Over the 9 months following rATG initiation, it increased progressively to 62 (range 13–87) mL/min/1.73 m2 (p = 0.039 versus time of rATG introduction). Four patients (#4, #5 #8, and #9) showed substantial recovery of eGFR (increasing by between 28 and 41 mL/min/1.73 m2) and 2 patients showed a small improvement (#3 [10 mL/min/1.73 m2), #6 [7 mL/min/1.73 m2; Fig. 2). Three patients continued to show deteriorating renal function after rATG introduction (#1: 36 to 30 mL/min/1.73 m2; #2: 48 to 21 mL/min/1.73 m2; #7: 27 to 13 mL/min/1.73 m2). eGFR values in these 3 patients at the time of cAMR diagnosis were not lower than in the other patients (Fig. 1, Table 1).
Estimated glomerular filtration rate (eGFR) during the 9 months before the diagnosis of chronic antibody-mediated rejection (cAMR) and 9 months after the introduction of rabbit antithymocyte globulin (rATG). Data are shown only for post-transplant measurements. Horizontal bars indicate median values; crosses indicate mean values; boxes indicate interquartile ranges; and whiskers indicate maximum and minimum values. If only two values were available, individual values are shown
Individual values for the change in estimated glomerular filtration rate (eGFR) during the 9 months before the diagnosis of chronic antibody-mediated rejection (cAMR) and 9 months after the introduction of rabbit anti-human thymocyte globulin (rATG), with eGFR at the time of starting rATG as the reference point (zero). Median values are shown in black
Ratios of urinary albumin/creatinine showed no consistent pattern after the introduction of rATG. At time of cAMR diagnosis, values varied from <5 mg/mmol (patients #1, #4, #5, and #6) to >900 mg/mmol (patients #2 and #3). After the introduction of rATG, the ratio remained stable in 3 patients (#1, #6, and #7), decreased in 3 patients (#3, #5, and #8), and increased in 3 patients (#2, #4, and #9; Fig. 3). The median urinary albumin/creatinine ratio was 22.9 mg/mmol at the time of starting rATG and 13.5 mg/mmol at month 9 (p = 0.29).
Urinary albumin/creatinine ratio during the 9 months before the diagnosis of chronic antibody-mediated rejection (cAMR) and 9 months after the introduction of rabbit anti-human thymocyte globulin (rATG). Data are shown only for post-transplant measurements. Horizontal bars indicate median values; crosses indicate mean values; boxes indicate interquartile ranges; and whiskers indicate maximum and minimum values. If only two values were available, individual values are shown
No grafts were lost during follow-up and none of the patients required dialysis during the 9-month follow-up period after starting rATG.
Tolerability of rATG
No adverse events with a suspected association with rATG administration, including allergic reactions, leukocytopenia or hospitalization for severe infection (or hospitalization for any other reason), were observed in any of the patients. There were no episodes of EBV, cytomegalovirus or BK polyomavirus infections in any of the patients during the observation period.
Discussion
The results presented here suggest that rATG might be a useful component of the armamentarium for treating cAMR. Current management of cAMR remains unsatisfactory, and no drugs are approved for its treatment. The conventional combination of IVIG and rituximab has largely been adopted based on its successful use in desensitizing highly sensitized patients before kidney transplantation [37]. New therapies have been investigated, including induction of plasma cell apoptosis by the proteasome inhibitor bortezomib, but this does not appear to reduce DSA levels when used as a monotherapy [38]. Novel agents, for example, the monoclonal anti-interleukin 6 receptor antibody [39] and C1 esterase inhibitor, have shown early promise [39], and the complement inhibitor eculizumab [40] may potentially be helpful in patients with intensive activation of the terminal complement complex, but firm evidence is not yet available. Against this background, application of rATG—an agent familiar to the transplant community over many years of use—is of potential interest.
In this series of nine children with cAMR and declining renal function, the addition of a 5-day course of rATG as a rescue therapy was associated with a substantial improvement in graft function in 4 cases and a small improvement in a further 2 cases. The remaining 3 patients continued to deteriorate. Strikingly, the 4 patients in whom eGFR improved (#4, #5, #8, and #9) all had cAMR diagnosed within the first 4 months after transplantation; late-onset cAMR proved less responsive. In 4 of the 8 patients in whom post-transplant Luminex data were available, DSAs present at the time of cAMR diagnosis had become undetectable, and MFI values were reduced after the intensive combined immunosuppressive treatment in 1 further patient. The remaining 3 patients still had significant levels of anti-HLA-DQ DSA, which is often the dominant form of DSAs [41] and is frequently hard to eliminate. No consistent changes were detected concerning the ratio of urinary albumin to creatinine.
The key safety concerns related to rATG therapy—higher risk for malignancy or infection—have diminished substantially under modern dosing regimens [42, 43]. In our series, no leukocytopenia or thrombocytopenia was detected. Despite the intensive immunosuppressive regimens administered, none of the patients had to be hospitalized because of severe infections. rATG infusions were generally well-tolerated in our patients and the complete rATG course of five injections was administered as planned in all 9 children. Nevertheless, longer-term follow-up would be essential in future studies of rATG for the management of cAMR in children to monitor risks, particularly for post-transplant lymphoproliferative disorder.
This cohort represented a hard-to-treat group in whom a series of other interventions had failed to arrest the decline in graft function. Thus, although numbers are small, these results are highly encouraging. We did not initiate rATG earlier as the evidence base is inadequate. Future studies could usefully explore the earlier introduction of rATG, likely in combination with one or more other therapies such as rituximab. The 3 patients who continued to deteriorate despite rATG therapy, showed no distinguishing features compared with responders, although none had been diagnosed with cAMR early post-transplant. A longer-term goal would be to determine which cases of cAMR are most likely to respond to rATG therapy.
Immunologically, the addition of rATG to rituximab appears rational. rATG includes a wide range of T-cell and non-T-cell antigen specificities, including antibodies against B-cell, plasma cell, and natural killer (NK) cell markers [44, 45], and in vitro it induces complement-independent apoptosis of activation and naïve B-cells, and plasma cells [46]. Clinically, T-cells and NK cells are depleted under rATG administration [19,20,21]. NK cells are central to the inflammatory processes in the graft during AMR and their depletion may promote graft survival [47]. Mature B-cells and plasma cells remain unaffected by rATG in vivo [19,20,21], but CD19+CD27+ memory and switch memory B-cells appear to be selectively suppressed for a prolonged period when rATG is used in desensitization protocols or as induction before kidney transplantation [19,20,21,22,23]. It seems feasible that rATG might inhibit memory B-cells by suppressing the availability of antigen-specific helper T-cells. Rituximab, in contrast, depletes mature B-cells [21, 46], but is less effective at depleting memory B-cells [21, 48, 49]. The immunological effects of the two agents may thus be complementary for targeting B-cells and their antibodies in patients with AMR.
Published data relating to rATG treatment of AMR are remarkably sparse and to our knowledge limited to cases of acute AMR, not cAMR. In one early study, published in 2004, a total of 27 patients with presumed acute AMR were treated with rituximab and plasmapheresis, with steroids in most cases, and 22 of the patients also received rATG [49]. Outcomes were good, with a death-censored graft survival rate of 89% after a mean of 605 days’ follow-up [50]. Zheng et al. treated 4 adults with acute AMR using rATG monotherapy and concluded that mild or moderate AMR was ameliorated, but not cured [51]. Two other published case reports have described successful outcomes using rATG combined with eculizumab, plasmapheresis, and IVIG [52] or high-dose corticosteroids, IVIG, and plasmapheresis [53].
We recognize that this represents a small study population. This retrospective analysis has additional limitations. The group of patients was notably heterogeneous. There were wide variations in the time between diagnosis of cAMR and initiation of rATG, and the individualized treatment regimens prescribed before rATG therapy also differed between patients, for example, with or without the introduction of belatacept and/or bortezomib therapy, although all patients were treated with steroid pulses, rituximab, and intravenous immunoglobulins. Inevitably, this limits the strength of conclusions that can be drawn about the effects of rATG as a single agent. Bortezomib has been associated with a transient decrease in DSA levels when used to treat AMR in pediatric kidney transplant recipients [54, 55], which may have contributed to outcomes. Additionally, pre-implantation and surveillance biopsies, in addition to biopsies and measurement of DSA MFIs directly before and after rATG administration, would have provided useful information, but were not performed because of the retrospective nature of this study. Similarly, monitoring of T-cell and B-cell subsets would have been helpful. However, this small cohort is relatively typical of pediatric kidney transplant patients, including the high incidence of non-adherence, necessitating a switch in immunosuppression, which is a leading risk factor for the development of DSAs [56]. There was also extensive HLA mismatching (from 2 to 8 mismatches) in the group, characteristic of the problems of achieving good matches in pediatric recipients.
Nevertheless, the current series of patients represents the largest dataset so far regarding use of rATG to treat cAMR. Used here as rescue therapy after a poor response to a sequence of other interventions, rATG appears a promising component of the treatment regimen. In the absence of prospective or comparative analysis, these observations may help to inform treatment choices in this challenging situation, and suggest that rATG might be a viable option for managing cAMR. However, an important caveat is that all patients had previously received multiple interventions in response to the diagnosis of cAMR, and it is not possible to reliably disentangle the effect of rATG. Prospective trials are urgently required, designed specifically to examine the impact of rATG, with adequate follow-up for safety monitoring. Investigation into the earlier introduction of rATG into the management of cAMR should also be carried out.
Change history
08 February 2018
The article “Rabbit anti-human thymocyte immunoglobulin for the rescue treatment of chronic antibody-mediated rejection after pediatric kidney transplantation”, written by Yasemen Cihan, Nele Kanzelmeyer, Jens Drube, Martin Kreuzer, Christian Lerch, Imke Hennies, Kerstin Froede, Murielle Verboom.
References
Clatworthy MR (2011) Targeting B cells and antibody in transplantation. Am J Transplant 11:1359–1367
Loupy A, Jordan SC (2013) Transplantation: donor-specific HLA antibodies and renal allograft failure. Nat Rev Nephrol 9:130–131
Fotheringham J, Angel C, Goodwin J, Harmer AW, McKane WS (2011) Natural history of proteinuria in renal transplant recipients developing de novo human leukocyte antigen antibodies. Transplantation 91:991–996
Sadaka B, Alloway RR, Woodle ES (2013) Management of antibody-mediated rejection in transplantation. Surg Clin North Am 93:1451–1466
Sellarés J, De Freitas DG, Mengel M, Reeve J, Einecke G, Sis B, Hidalgo LG, Famulski K, Matas A, Halloran PF (2012) Understanding the causes of kidney transplant failure: the dominant role of antibody-mediated rejection and nonadherence. Am J Transplant 12:388–399
El-Zoghby ZM, Stegall MD, Lager DJ, Kremers WK, Amer H, Gloor JM, Cosio FG (2009) Identifying specific causes of kidney allograft loss. Am J Transplant 9:527–535
NAPRTCS 2014 Annual Transplant Report. Available at https://web.emmes.com/study/ped/annlrept/annualrept2014.pdf Accessed 26 May 2017
Kreuzer M, Prüfe J, Oldhafer M, Bethe D, Dierks ML, Müther S, Thumfart J, Hoppe B, Büscher A, Rascher W, Hansen M, Pohl M, Kemper MJ, Drube J, Rieger S, John U, Taylan C, Dittrich K, Hollenbach S, Klaus G, Fehrenbach H, Kranz B, Montoya C, Lange-Sperandio B, Ruckenbrodt B, Billing H, Staude H, Heindl-Rusai K, Brunkhorst R, Pape L (2015) Transitional care and adherence of adolescents and young adults after kidney transplantation in Germany and Austria: a binational observatory census within the TRANSNephro trial. Medicine (Baltimore) 94:e2196
Loupy A, Lefaucheur C, Vernerey D, Prugger C, Duong van Huyen JP, Mooney N, Suberbielle C, Frémeaux-Bacchi V, Méjean A, Desgrandchamps F, Anglicheau D, Nochy D, Charron D, Empana JP, Delahousse M, Legendre C, Glotz D, Hill GS, Zeevi A, Jouven X (2013) Complement-binding anti-HLA antibodies and kidney-allograft survival. N Engl J Med 369:1215–1226
Hourmant M, Cesbron-Gautier A, Terasaki PI, Mizutani K, Moreau A, Meurette A, Dantal J, Giral M, Blancho G, Cantarovich D, Karam G, Follea G, Soulillou JP, Bignon JD (2005) Frequency and clinical implications of development of donor-specific and non-donor- specific HLA antibodies after kidney transplantation. J Am Soc Nephrol 16:2804–2812
Kim JJ, Balasubramanian R, Michaelides G, Wittenhagen P, Sebire NJ, Mamode N, Shaw O, Vaughan R, Marks SD (2014) The clinical spectrum of de novo donor-specific antibodies in pediatric renal transplant recipients. Am J Transplant 14:2350–2358
Djamali A, Kaufman DB, Ellis TM, Zhong W, Matas A, Samaniego M (2014) Diagnosis and management of antibody-mediated rejection: current status and novel approaches. Am J Transplant 14:255–271
Burton SA, Amir N, Asbury A, Lange A, Hardinger KL (2015) Treatment of antibody-mediated rejection in renal transplant patients: a clinical practice survey. Clin Transpl 29:118–123
Montgomery RA, Zachary AA, Racusen LC, Leffell MS, King KE, Burdick J, Maley WR, Ratner LE (2000) Plasmapheresis and intravenous immune globulin provides effective rescue therapy for refractory humoral rejection and allows kidneys to be successfully transplanted into cross-match-positive recipients. Transplantation 70:887–895
Rocha PN, Butterly DW, Greenberg A, Reddan DN, Tuttle-Newhall J, Collins BH, Kuo PC, Reinsmoen N, Fields T, Howell DN, Smith SR (2003) Beneficial effect of plasmapheresis and intravenous immunoglobulin on renal allograft survival of patients with acute humoral rejection. Transplantation 75:1490–1495
Montgomery RA, Orandi BJ, Racusen L, Jackson AM, Garonzik-Wang JM, Shah T, Woodle ES, Sommerer C, Fitts D, Rockich K, Zhang P, Uknis ME (2016) Plasma-derived C1 esterase inhibitor for acute antibody-mediated rejection following kidney transplantation: results of a randomized double-blind placebo-controlled pilot study. Am J Transplant 16:3468–3478
Choi J, Aubert O, Vo A, Loupy A, Haas M, Puliyanda D, Kim I, Louie S, Kang A, Peng A, Kahwaji J, Reinsmoen N, Toyoda M, Jordan SC (2017) Assessment of tocilizumab (anti-interleukin-6 receptor monoclonal) as a potential treatment for chronic antibody-mediated rejection and transplant glomerulopathy in HLA-sensitized renal allograft recipients. Am J Transplant. doi:10.1111/ajt.14228
Chih S, Tinckam KJ, Ross HJ (2013) A survey of current practice for antibody-mediated rejection in heart transplantation. Am J Transplant 13:1069–1074
Büchler M, Longuet H, Lemoine R, Herr F, Gatault P, Thibault G, Ternant D, Foulon C, Pilorge B, Lemay D, Sung C, Halimi JM, Baron C, Lebranchu Y (2013) Pharmacokinetic and pharmacodynamic studies of two different rabbit antithymocyte globulin dosing regimens: results of a randomized trial. Transpl Immunol 28:120–126
Kho MM, Bouvy AP, Cadogan M, Kraaijeveld R, Baan CC, Weimar W (2012) The effect of low and ultra-low dosages Thymoglobulin on peripheral T, B and NK cells in kidney transplant recipients. Transpl Immunol 26:186–190
Ramos EJ, Pollinger HS, Stegall MD, Gloor JM, Dogan A, Grande JP (2007) The effect of desensitization protocols on human splenic B-cell populations in vivo. Am J Transplant 7:402–407
Pankewycz O, Leca N, Kohli R, Wallace PK, Said M, Feng L, Alnimri M, Patel S, Laftavi MR (2011) Low-dose rabbit antithymocyte globulin induction therapy results in prolonged selective lymphocyte depletion irrespective of maintenance immunosuppression. Transplant Proc 43:462–465
Gurkan S, Luan Y, Dhillon N, Allam SR, Montague T, Bromberg JS, Ames S, Lerner S, Ebcioglu Z, Nair V, Dinavahi R, Sehgal V, Heeger P, Schroppel B, Murphy B (2010) Immune reconstitution following rabbit antithymocyte globulin. Am J Transplant 10:2132–2141
Brokhof MM, Sollinger HW, Hager DR, Muth BL, Pirsch JD, Fernandez LA, Bellingham JM, Mezrich JD, Foley DP, D’Alessandro AM, Odorico JS, Mohamed MA, Vidyasagar V, Ellis TM, Kaufman DB, Djamali A (2014) Antithymocyte globulin is associated with a lower incidence of de novo donor-specific antibodies in moderately sensitized renal transplant recipients. Transplantation 97:612–617
Pascual J, Zuckermann A, Djamali A, Hertig A, Naesens M (2016) Rabbit antithymocyte globulin and donor-specific antibodies in kidney transplantation--a review. Transplant Rev (Orlando) 30:85–91
Pape L, Lehner F, Blume C, Ahlenstiel T (2011) Pediatric kidney transplantation followed by de novo therapy with everolimus, low-dose cyclosporine a, and steroid elimination: 3-year data. Transplantation 92:658–662
Pape L, Offner G, Kreuzer M, Froede K, Drube J, Kanzelmeyer N, Ehrich JH, Ahlenstiel T (2010) De novo therapy with everolimus, low-dose ciclosporine a, basiliximab and steroid elimination in pediatric kidney transplantation. Am J Transplant 10:2349–2354
Gupta A, Murillo D, Yarlagadda SG, Wang CJ, Nawabi A, Schmitt T, Brimacombe M, Bryan CF (2016) Donor-specific antibodies present at the time of kidney transplantation in immunologically unmodified patients increase the risk of acute rejection. Transpl Immunol 37:18–22
Malheiro J, Tafulo S, Dias L, Martins LS, Fonseca I, Beirão I, Castro-Henriques A, Cabrita A (2015) Analysis of preformed donor-specific anti-HLA antibodies characteristics for prediction of antibody-mediated rejection in kidney transplantation. Transpl Immunol 32:66–71
Eskandary F, Bond G, Regele H, Kozakowski N, Kikić Z, Wahrmann M, Haslacher H, Oberbauer R, Ramassar V, Halloran P, Böhmig GA (2014) Late antibody-mediated rejection in a large prospective cross-sectional study of kidney allograft recipients--preliminary results of the screening phase of the BORTEJECT trial. Clin Transpl 2014:189–195
Haas M, Sis B, Racusen LC, Solez K, Glotz D, Colvin RB, Castro MC, David DS, David-Neto E, Bagnasco SM, Cendales LC, Cornell LD, Demetris AJ, Drachenberg CB, Farver CF, Farris AB 3rd, Gibson IW, Kraus E, Liapis H, Loupy A, Nickeleit V, Randhawa P, Rodriguez ER, Rush D, Smith RN, Tan CD, Wallace WD, Mengel M, Banff meeting report writing committee (2014) Banff 2013 meeting report: inclusion of c4d-negative antibody-mediated rejection and antibody-associated arterial lesions. Am J Transplant 14:272–283
Billing H, Rieger S, Süsal C, Waldherr R, Opelz G, Wühl E, Tönshoff B (2012) IVIG and rituximab for treatment of chronic antibody-mediated rejection: a prospective study in paediatric renal transplantation with a 2-year follow-up. Transplant Int 5:1165–1173
Lerch C, Kanzelmeyer NK, Ahlenstiel-Grunow T, Froede K, Kreuzer M, Drube J, Verboom M, Pape L (2017) Belatacept after kidney transplantation in adolescents: a retrospective study. Transpl Int 30:494–501
Walsh RC, Alloway RR, Girnita AL, Woodle ES (2012) Proteasome inhibitor-based therapy for antibody-mediated rejection. Kidney Int 81:1067–1074
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Reed RP, Zhang Z, Gebel H, Bray RA, Guleria I, Lunz J, Mohanakumar T, Nickerson P, Tambur AR, Zeevi A, Heeger PS, Gjertson D (2013) Comprehensive assessment and standardization of solid phase multiplex-bead arrays for the detection of antibodies to HLA. Am J Transplant 13:1859–1870
Vo AA, Lukovsky M, Toyoda M, Wang J, Reinsmoen NL, Lai CH, Peng A, Villicana R, Jordan SC (2008) Rituximab and intravenous immune globulin for desensitization during renal transplantation. N Engl J Med 359:242–251
Sberro-Soussan R, Zuber J, Suberbielle-Boissel C, Candon S, Martinez F, Snanoudj R, Rabant M, Pallet N, Nochy D, Anglicheau D, Leruez M, Loupy A, Thervet E, Hermine O, Legendre C (2010) Bortezomib as the sole post-renal transplantation desensitization agent does not decrease donor-specific anti-HLA antibodies. Am J Transplant 10:681–686
Haririan A (2015) Current status of the evaluation and management of antibody-mediated rejection in kidney transplantation. Curr Opin Nephrol Hypertens 24:576–581
Frémeaux-Bacchi V, Legendre CM (2015) The emerging role of complement inhibitors in transplantation. Kidney Int 88:967–973
Tagliamacco A, Cioni M, Comoli P, Ramondetta M, Brambilla C, Trivelli A, Magnasco A, Biticchi R, Fontana I, Dulbecco P, Palombo D, Klersy C, Ghiggeri GM, Ginevri F, Cardillo M, Nocera A (2014) DQ molecules are the principal stimulators of de novo donor-specific antibodies in nonsensitized pediatric recipients receiving a first kidney transplant. Transpl Int 27:667–673
Mohty M, Bacigalupo A, Saliba F, Zuckermann A, Morelon E, Lebranchu Y (2014) New directions for rabbit antithymocyte globulin (Thymoglobulin®) in solid organ transplants, stem cell transplants and autoimmunity. Drugs 74:1605–1634
Hertig A, Zuckermann A (2015) Rabbit antithymocyte globulin induction and risk of post-transplant lymphoproliferative disease in adult and pediatric solid organ transplantation: an update. Transpl Immunol 32:179–1787
Popow I, Leitner J, Grabmeier-Pfistershammer K, Majdic O, Zlabinger GJ, Kundi M, Steinberger P (2013) A comprehensive and quantitative analysis of the major specificities in rabbit antithymocyte globulin preparations. Am J Transplant 13:3103–3113
Rebellato LM, Gross U, Verbanac KM, Thomas JM (1994) A comprehensive definition of the major antibody specificities in polyclonal rabbit antithymocyte globulin. Transplantation 57:685–694
Zand MS, Vo T, Huggins J, Felgar R, Liesveld J, Pellegrin T, Bozorgzadeh A, Sanz I, Briggs BJ (2005) Polyclonal rabbit antithymocyte globulin triggers B-cell and plasma cell apoptosis by multiple pathways. Transplantation 79:1507–1515
Kohei N, Tanaka T, Tanabe K, Masumori N, Dvorina N, Valujskikh A, Baldwin WM 3rd, Fairchild RL (2016) Natural killer cells play a critical role in mediating inflammation and graft failure during antibody-mediated rejection of kidney allografts. Kidney Int 89:1293–1306
Kamburova EG, Koenen HJ, Borgman KJ, Ten Berge IJ, Joosten I, Hilbrands LB (2013) A single dose of rituximab does not deplete B cells in secondary lymphoid organs but alters phenotype and unction. Am J Transplant 13:1503–1511
Jackson AM, Kraus ES, Orandi BJ, Segev DL, Montgomery RA, Zachary AA (2015) A closer look at rituximab induction on HLA antibody rebound following HLA-incompatible kidney transplantation. Kidney Int 87:409–416
Becker YT, Becker BN, Pirsch JD, Sollinger HW (2004) Rituximab a treatment for refractory kidney transplant rejection. Am J Transplant 4:996–1001
Zheng J, Xue W, Qing X, Jing X, Hou J, Tian X, Guo Q, He X, Cai J (2014) Treatment of biopsy-proven acute antibody-mediated rejection using Thymoglobulin (ATG) monotherapy and a combination of rituximab, intravenous immunoglobulin, and plasmapheresis: lesson learned from primary experience. Clin Transpl 2014:223–230
Chehade H, Rotman S, Matter M, Girardin E, Aubert V, Pascual M (2015) Eculizumab to treat antibody-mediated rejection in a 7-year-old kidney transplant recipient. Pediatrics 132:e551–e555
Kutzler HL, Ye X, Rochon C, Martin ST (2016) Administration of antithymocyte globulin (rabbit) to treat a severe, mixed rejection episode in a pregnant renal transplant recipient. Pharmacotherapy 36:e18–e22
Kizilbash S, Claes D, Ashoor I, Chen A, Jandeska S, Matar RB, Misurac J, Sherbotie J, Twombley K, Verghese P (2017) Bortezomib in the treatment of antibody-mediated rejection in pediatric kidney transplant recipients: a multicenter Midwest Pediatric Nephrology Consortium study. Pediatr Transplant 21(3):e12873. doi:10.1111/petr.12873
Pearl MH, Nayak AB, Ettenger RB, Puliyanda D, Palma Diaz MF, Zhang Q, Reed EF, Tsai TW (2016) Bortezomib may stabilize pediatric renal transplant recipients with antibody-mediated rejection. Pediatr Nephrol 31:1341–1348
O’Leary JG, Samaniego M, Barrio MC, Potena L, Zeevi A, Djamali A, Cozzi E (2016) The influence of immunosuppressive agents on the risk of de novo donor-specific HLA antibody production in solid organ transplant recipients. Transplantation 100:39–53
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The study received no external funding. Medical writing support by a freelance medical writer was funded by Sanofi.
Ethics
This retrospective study did not require ethical approval.
Conflicts of interest
Lars Pape has received speaker’s honoraria and travel grants from Novartis Pharmaceuticals. None of the other authors has any conflicts of interest to declare.
Additional information
A correction to this article is available online at https://doi.org/10.1007/s00467-017-3858-2.
Rights and permissions
About this article
Cite this article
Cihan, Y., Kanzelmeyer, N., Drube, J. et al. Rabbit anti-human thymocyte immunoglobulin for the rescue treatment of chronic antibody-mediated rejection after pediatric kidney transplantation. Pediatr Nephrol 32, 2133–2142 (2017). https://doi.org/10.1007/s00467-017-3725-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-017-3725-1