Abstract
Background
Anticoagulation of the continuous renal replacement therapy (CRRT) circuit is an important technical aspect of this medical procedure. Most studies evaluating the efficacy and safety of citrate use have been carried out in adults, and little evidence is available for the pediatric patient population. The aim of this study was to compare regional citrate anticoagulation versus systemic heparin anticoagulation in terms of the lifetime of hemofilters in a pediatric population receiving CRRT at a pediatric center in Bogota, Colombia.
Methods
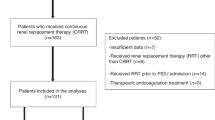
This was an analytical, observational, retrospective cohort study in which we assessed the survival of 150 hemofilters (citrate group 80 hemofilters, heparin group 70 hemofilters) used in a total of 3442 hours of CCRT (citrate group 2248 h, heparin group 1194 h). Hemofilter survival was estimated beginning at placement and continuing until filter replacement due to clotting or high trans-membrane pressures.
Results
Hemofilter survival was higher in the citrate group than in the heparin group (72 vs. 18 h; p <0.0001). Bivariate analysis showed that the hemofilter coagulation risk was significantly increased when heparin was used, regardless of hemofilter size and pump flow (hazard ratio 3.70, standard error 0.82, 95% confidence interval 2.39–5.72; p <0.00001).
Conclusions
Regional citrate anticoagulation could be more effective than heparin systemic anticoagulation in terms of prolonging the hemofilter lifetime in patients with acute renal injury who require CRRT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Continuous renal replacement therapy (CRRT) is a treatment for patients with acute kidney injury (AKI), fluid overload, and severe metabolic disturbances in the pediatric intensive care unit (PICU) [1]. Circuit anticoagulation is an important technical issue in this therapy, and its primary purpose is to prevent thrombotic processes once the blood comes in contact with the extracorporeal circuit. Heparin is the most widely used anticoagulant. However, heparin therapy is associated with an increased risk of bleeding and thrombocytopenia, the development of resistance to its action in critically ill patients, and the stimulation of proinflammatory effects by impaired phagocytosis [2].
Citrate anticoagulation offers an interesting alternative as its anticoagulation effect is regional (reversed immediately postfilter) and is therefore associated with lower rates of bleeding complications [2]. Since its introduction for clinical use in 1980, there have been several studies in adults trying to establish the safety and efficacy of regional citrate anticoagulation [3–8]. A systematic review and meta-analysis [9, 10] have shown, with some limitations due to the heterogeneity of the selected studies, that citrate may be more effective than other alternatives for anticoagulation because it will extend the lifetime of the circuit (due to a lower risk of bleeding) and, although it has been associated with an increased risk for metabolic disorders, these had no relevant clinical consequences. However, citrate must be handled by experienced personnel due to the potential for increased complications inherent to the treatment.
If regional citrate anticoagulation decreases the frequency of bleeding complications and prolongs the lifetime of hemofilters, it could decrease the costs of CRRT. Given the potential benefits of regional citrate anticoagulation, it is therefore important to know the results of the use of this therapy in the pediatric patient population. However, relevant studies on this patient population are scarce [11]. Since Bunchman et al. [12, 13] established the first protocol for CRRT using citrate in children, there have been only nine additional pediatric studies reporting the use of this strategy [11, 14–23].
The main objective of this study was to compare the lifetime of hemofilters using regional citrate anticoagulation versus systemic heparin anticoagulation in a population of children needing CRRT in the PICU.
Materials and methods
An analytical, observational, retrospective cohort study was carried out in which patients were followed from admission through to discharge from the PICU of the Fundación Cardioinfantil in Bogota, Colombia.
For the descriptive analysis, we included subjects between 1 month and 18 years of age with AKI or exacerbated chronic kidney disease who had received CRRT during hospitalization in the PICU from January 2008 to July 2013. The subjects were divided into two groups: one group comprising patients who received regional citrate anticoagulation and the second group comprising those who received anticoagulation with unfractionated heparin. Patients who had received alternative forms of anticoagulation during the study period were excluded from the analysis.
Therapy was defined as various renal replacement therapies, including slow continuous ultrafiltration, continuous venovenous hemodiafiltration, continuous venovenous hemofiltration (CVVH), and continuous venovenous hemodialysis, which patients received for a total of >12 h over a number of sessions. The therapy modality was selected according to the patient’s clinical condition (hemodynamic stability, primary diagnosis), and the objective of the therapy (solute removal, water removal, cytokine removal, etc.). All of the therapies received one of the two types of anticoagulation.
In the heparin anticoagulation protocol, an initial intravenous bolus of unfractionated heparin in the range of 20–50 IU/kg body weight was administered, followed by continuous infusion of heparin at a rate of 5 to 20 IU/kg/h, adjusted to achieve a target partial thromboplastin time (PTT) ratio of approximately 1.5- to 2-fold the control or a postfilter PTT of between 180–200 s [24].
In the citrate group, 3.22 % acid citrate dextrose formula A (ACD-A) was administered in the prefilter port, with an infusion rate (in ml/h) equivalent to 1.5-fold the pump flow (Qb) (Qb × 1.5 in ml/h), in order to maintain a concentration of ionized calcium postfilter (venous port) from 0.25 to 0.4 mmol/L. A calcium gluconate infusion was administered in the postfilter port at a concentration of 20 mg/dl, with an infusion rate (in ml/h) corresponding to 25% of the Qb (Qb in ml/h/4) in order to maintain the concentration of prefilter ionized calcium (arterial port) at between 1.0 and 1.2 mmol/L. The monitoring of the concentrations of ionized calcium and venous blood gases pre- and postfilter were determined at the first, second, and fourth hour of therapy, and then every 4 h until the therapy was concluded. At the same time intervals, the acid–base status of the patient was monitored by the analysis of arterial blood gases obtained through the arterial prefilter port. The infusion rate adjustments of both calcium gluconate and ACD-A were made based on changes in ionized calcium concentrations determined in the pre- and postfilter ports.
In addition to establishing and comparing the total lifetime of hemofilters in the two study groups, we determined and compared the average length of stay of the patient in the PICU, the incidence of mortality, and the frequency of severe bleeding (defined as bleeding associated with hypotension, tachycardia, need for red blood cell transfusion or a 2 g/dl drop in hemoglobin within 24 h). The frequency of metabolic complications, such as hypocalcemia (ionized calcium concentration of <1 mmol/L or serum total calcium concentration of <9 mg/dl), hypercalcemia (total ionized calcium concentration of >1.2 mmol/L or serum total calcium concentration of >11 mg/dl), metabolic alkalosis (bicarbonate concentration of >24 meq/L), hypomagnesemia (plasma magnesium concentration of <1.4 mg/dl), and hypernatremia (sodium plasma concentration of >145 mql/L) were only measured in the regional citrate anticoagulation group due to incomplete records in the systemic heparin anticoagulation group.
The protocol was submitted for review and the study was approved by the institutional ethics committee.
Statistical analysis
Four units of analysis were considered in this study, according to the outcome of interest: patients, admissions, therapies, and hemofilters, keeping in mind that the same patient may have been admitted more than once to the PICU and that each hemofilter may have been used for more than one therapy.
The demographic and clinical characteristics of the study subjects and the variables associated with the filter were described. Relative frequency measures, comparative tables, and histogram-type frequency distribution graphs were used for qualitative variables, where applicable. Central tendency measures (mean, median, and mode) and dispersion or variability measures (percentiles, range or standard deviation, coefficient of variation or homogeneity) were used for quantitative variables, depending on the normality of the distribution of the data, which was evaluated using the Shapiro–Wilk test. The unit of analysis was the hemofilters and, since a patient could provide more than one filter, it was adjusted for the additional variance caused by clustering. For calculating the useful life of hemofilters using citrate anticoagulation versus heparin anticoagulation, we performed an analysis for each specific event, the event being the lifetime of the filter from the time it was placed until it was replaced/discontinued due to therapy completion, thrombotic occlusion, or system dysfunction with transmembrane pressures of >280 mmHg.
Hemofilter changes due to discharge of the patient from the PICU as a result of improvement or death were taken as censorship. Survival estimates were made using the Kaplan–Meier method. The median survival for each group, with its respective 95% confidence intervals (CIs), was reported, and a comparison of the curves was tested using a log-rank test. The magnitude of the effect of the anticoagulant on clotting in the filter was analyzed using Cox’s non-parametric proportional hazards model, which was adjusted for potential confounding variables (size of the filter and pump flow) that could affect the lifetime of the filter.
A sample size of 120 filters, 60 per group, was calculated to be sufficient to identify a significant difference in time to occlusion of the filters, with a type I error of 5% and a power of 80%, estimating a percentage of censure of 5% and taking into account the intra-patient variation that might arise. The sampling was non-probabilistic and included the entire study population. All analyses were performed using STATA version 9 software (StataCorp LP, College Station, TX).
Results
Description of the population
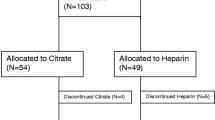
Thirty-two patients (17 in the citrate group and 15 in the heparin group) with 46 admissions (30 in the citrate group and 16 in the heparin group) were included in the analysis. The demographic and clinical characteristics of the patients were similar in both groups (Table 1), except for the length of hospital stay, which was higher in the heparin group (p = 0.021).
Description of hemofilters
A total of 150 hemofilters were used in all therapies, 80 in the citrate patient group and 70 in the heparin patient group. A significant difference was observed in the size distribution of the filter between the two groups (p = 0.007). In both groups, the most frequently used filter size was 0.7 m2. However, the proportion of 0.4-m2 filters was much lower in the citrate group than in the heparin group. Similarly, there was a significant difference in the number of therapies per filter between the two groups (p = 0.0045), with the number being higher in the citrate group (Table 2).
Description of therapies
A total of 3442 h of dialysis therapy (citrate group 2248 h heparin group 1194 h) were included in the analysis. The characteristics of the therapies were similar in both groups, except for one significant difference in the distribution of the type of therapy (p = 0.000) and in the Qb used (p = 0.0027). For example, there was a higher proportion of CVVH in the citrate anticoagulation group. In both anticoagulant therapy groups the average Qb was 3.45 ml/kg, and the most frequently used Qb was between 100 and 200 ml/min. However, the proportion of Qb at <100 ml/min was much higher in the citrate group than in the heparin group. The patients’ pH was normal, and a tendency towards alkalosis was seen in the citrate group, which suggests accumulation (Table 3).
Analysis of hemofilter lifetime
In the citrate anticoagulation group there were 56 events (hemofilter removal due to clotting or dysfunction of the circuit evidenced by transmembrane pressures of >280 mmHg). The heparin group presented 63 events. The median duration of hemofilters was significantly higher in the group receiving citrate as anticoagulant than in the group receiving heparin as anticoagulant [72 (95% CI 48–96) vs. 18 (95% CI 12–24) h; p < 0.0001] (Fig. 1). A bivariate analysis was performed with the possible confounding variables according to clinical experience, and no statistical relationships between the size of the filter and Qb and the duration of the hemofilter were found (Table 4). Cox’s proportional risk analysis showed that the risk of hemofilter clotting when heparin was used as an anticoagulant is 3.7-fold higher than when citrate was used (hazard ratio 3.70, standard error 0.82; 95% CI 2.39–5.72; p < 0.00001).
Description of complications
Bleeding
Among all of the subjects in the study, 15 episodes of severe bleeding occurred, with the frequency of this type of adverse event being similar in both groups (p = 0.605). At least one risk factor for bleeding was identified in the citrate group (disseminated intravascular coagulation, plasmapheresis, prolonged clotting times and other coagulation defects) in 77.7% of cases, compared with 66.6% for the heparin group. Both groups had a 30% incidence of bleeding episodes which, given the complexity of the patients and the risk factors, we consider to be a reasonable figure (Table 5).
Metabolic complications in the citrate group
There were no episodes of hypernatremia. The most frequent complication was metabolic alkalosis (86.6%), followed by hypocalcemia (60%), hypomagnesemia (46.6%) and hypercalcemia (13.3%). Phosphate levels were not recorded (Fig. 2). No association was found between metabolic complications and the average flow of citrate or the average ratio of total calcium to ionized calcium (T/I Ca2+) above or below 2.25. The only association found was between the mean postfilter flow of calcium gluconate and hypomagnesemia, with the former being higher when hypomagnesemia was present (p = 0.0028).
Discussion
A small number of analytical observational studies have been carried out in the pediatric population that have analyzed the safety of citrate versus heparin as anticoagulant in renal replacement therapy. The authors of three studies [25–27] considered citrate to be more effective in preventing clotting of the circuit and prolonging its lifetime, although its use required greater monitoring of pH and electrolytes, which in turn requires nurses with specialized skills. The major limitation to any definitive drawing of conclusions based on the results of these studies is the low number of patients included.
Studies in adult populations aimed at analyzing the lifetime of hemofilters anticoagulated with citrate versus heparin have produced variable results, with some reporting that citrate is better [4–6] and others failing to demonstrate this outcome [7–9].
In the systematic review by Zhang et al. [10], six randomized controlled trials in adults met the selection criteria. Four of these studies compared regional citrate anticoagulation versus systemic anticoagulation with unfractionated heparin [4–6, 8]. In the other two studies, the control group received regional anticoagulation with unfractionated heparin or systemic anticoagulation with nadroparin [7, 8]. Of the four trials whose control groups received systemic anticoagulation with heparin, three (302 circuits, with 153 in the heparin group and 149 in the citrate group) reported a significantly higher filter lifetime in the citrate group compared to the control group [4–6], while the other study (142 circuits) found no difference between the two groups [8]. Despite the heterogeneity of the studies included (I 2 = 99 %), overall circuit survival was significantly higher in the citrate group than in the control group, with a mean difference of 23 h (95 % CI 0.45–45.61).
In the current study, the total lifetime of the hemofilters was significantly higher in the citrate group than in the heparin group, with a mean difference of 54 h regardless of pump flow and the size of the hemofilter. Taking into account that the descriptive analysis revealed that there was a higher proportion of therapies with a Qb of <100 ml/min in the citrate group than in the heparin group (43.9 vs. 17.53 %), it can be deduced that the use of citrate prolongs the lifetime of hemofilters despite the use of a lower Qb, which is especially important in the pediatric population as these patients often need a low Qb.
The available evidence in children is limited. However, compared with other pediatric studies, the lifetime of hemofilters anticoagulated with citrate in our study (72 h, 95 % CI 48–96 h) is similar to that reported by Bunchman et al. [2] (71.3 ± 7.2 h), but higher than that observed by Elhanan et al. [15] (55.6 ± 22.0 h), Brophy et al. [20] (44.7 ± 35.9 h) and Chadha et al. [22] (51 ± 8 h).
The main problem with heparin is that it causes systemic anticoagulation in addition to circuit regional anticoagulation [2]. In Zhang et al.’s systematic review [10], in a total of 517 patients (citrate group 257, control group 260), 12 and 47 bleeding episodes were reported in the citrate group and the control group, respectively. The calculated relative risk (RR) was 0.28 (95 %CI 0.15–0.50), although the definition of bleeding events was not uniform across the studies. The bleeding rate was also significantly lower in the citrate group than in the control group, findings which are similar to those reported in a meta-analysis carried out by Wu et al. [9] (RR 0.34, 95% CI 0.17–0.65) and Yu-jie et al. [28] (odds ratio 0.25, 95% CI 0.12–0.54).
In a study of 18 children on intermittent hemodialysis with a history of bleeding or at high risk for bleeding complications who were receiving regional citrate anticoagulation [23], no patients developed new bleeding events. In contrast, in the control group of 14 children on acute hemodialysis and receiving systemic anticoagulation with heparin, a third of the patients developed new bleeding complications or worsening of previous bleeding (p = 0.006). Systemic bleeding was not documented in the study of Elhanan et al. [15], involving 22 children on CRRT and regional citrate anticoagulation.
As opposed to previously reported results, the frequency of episodes of severe bleeding in our study cohort was similar in both groups (p = 0.605). However, in the citrate group at least one risk factor for bleeding was identified in 77.7% of cases, compared to 66.6 % of cases in the heparin group. In addition, 100% of the bleeding events in the heparin group were systemic (upper gastrointestinal, central nervous system, intra-abdominal bleeding), while in the citrate group local bleeding (high flow catheter insertion site) made up 30% of the events. There was also no significant difference in mortality between the two groups (p = 0.859) and no deaths attributable to bleeding. On the contrary, the proportion of deaths in this study was lower (25%) than that reported in studies published since 2000, in which the mortality in children with AKI receiving CRRT varies from 32.1 to 58.9 % [29, 30].
The reported frequency of metabolic complications associated with the use of regional citrate anticoagulation is variable in both adult and pediatric patient population studies. For example, in a study of 209 adults (37 received only citrate, 87 received low-dose heparin + citrate, and 85 received only heparin), metabolic alkalosis was seen in 50% of patients treated with citrate [31]. Zhang et al. [10], in their systematic review, found that metabolic events were reported very heterogeneously across the studies and, therefore, it was not possible to analyze them. However, in the meta-analysis conducted by Wu et al. [9], there was no significant difference in the incidence of metabolic alkalosis in the citrate group compared to the heparin group (RR 0.92, 95% CI 0.23–3.68), while the overall incidence of hypocalcemia in patients with citrate was higher (4.8 vs. 0.8%) (RR 3.51, 95% CI 1.17–10.60).
In our study we documented no episodes of hypo- or hypernatremia. The most frequent complication was metabolic alkalosis followed by hypocalcemia, hypomagnesemia, and hypercalcemia. No analyses were made in the heparin group because the records were incomplete. Although the frequency of metabolic complications is not negligible, these events were not clinically significant, and only in one case was it necessary to suspend citrate therapy due to severe metabolic alkalosis. This was possibly related to the close monitoring these patients undergo according to institutional protocol, through a determination of acid–base status and pre- and postfilter concentrations of total and ionized calcium, based on which timely adjustments are made to ACD-A and calcium gluconate infusion rates.
The variability in the frequency of electrolyte and acid–base disturbances depends in part on the accuracy with which the protocols are applied [2]. However, two factors have reported in children which are associated with the increased risk of citrate toxicity in this patient population. First, it has been determined that the citrate load administered to children is higher than that administered to adults, taking into account that the pediatric dose depends on blood flow (calculated in ml/kg/min) [11]. Second, lower citrate clearance rates have been reported in CRRT, compared to intermittent hemodialysis, and the rates are even lower when this therapy is used in children [32–34]. In adults, clearance rates of 35–50 % have been reported, compared with rates of only 20 % in pediatric patients [22].
The T/I Ca2+ ratio is proportional to the serum concentration of citrate. It has been established that a ratio of >2.25 suggests an accumulation of citrate and that one of >2.4 is an independent risk factor for 28-day mortality in critically ill patients with AKI on CRRT with citrate as anticoagulant [28]. Although in 66.6 and 30% of admissions the average T/I Ca2+ ratio was higher than 2.25 and 2.4, respectively, we found no association between the development of some form of metabolic complication and a T/I Ca2+ ratio that was higher or lower than 2.25 (p = not significant), and there was no difference in mortality between the citrate and heparin groups (p = 0.859). Based on these results, we infer that the population could have other risk factors and/or triggers for complications apart from citrate use.
The main limitation of this study arises from possible data confusion and selection bias, given its retrospective nature. Incomplete data in the medical records made it difficult to evaluate various aspects, such as the association between hematocrit and the lifetime of hemofilters, as well as the frequency of metabolic complications in the heparin group. For this reason, conclusions cannot be drawn from this study regarding the relationship between anticoagulation modalities and the risk of metabolic complications. With the current design, we also could not assess the effect of the T/I Ca2+ ratio related to medium-term mortality and, due to the low number of bleeding events, it was not possible to establish a statistical association between these and bleeding risk factors unrelated to circuit anticoagulation.
Despite these limitations, the social and theoretical relevance of the study is that, to date, most studies evaluating the efficacy and safety of citrate have been carried out in adult populations and, therefore, the evidence available for the pediatric patient population is limited. Furthermore, this study is among those reporting the greatest number of therapy hours to date in the pediatric population and provides the first local description of the use of this anticoagulation strategy in children.
Conclusions
Regional citrate anticoagulation could be more effective than heparin systemic anticoagulation in terms of prolonging the lifetime of the hemofilter. This finding suggests that citrate anticoagulation is an effective strategy for anticoagulation in pediatric CRRT. Further research protocols are needed to assess the safety of using citrate in this population.
References
Sutherland SM, Alexander SR (2012) Continuous renal replacement therapy in children. Pediatr Nephrol 27:2007–2016
Oudemans-van Straaten HM, Kellum JA, Bellomo R (2011) Clinical review: Anticoagulation for continuous renal replacement therapy-heparin or citrate? Crit Care 15:202–211
Hetzel GR, Schmitz M, Wissing H, Ries W, Schott G, Heering PJ, Isgro F, Kribben A, Himmele R, Grabensee B, Rump LC (2011) Regional citrate versus systemic heparin for anticoagulation in critically ill patients on continuous venovenous haemofiltration: a prospective randomized multicentre trial. Nephrol Dial Transplant 26:232–239
Kutsogiannis DJ, Gibney RT, Stollery T, Gao J (2005) Regional citrate versus systemic heparin anticoagulation for continuous renal replacement in critically ill patients. Kidney Int 67:2361–2367
Monchi M, Berghmans D, Ledoux D, Canivet JL, Dubois D, Damas P (2004) Citrate vs. heparin for anticoagulation in continuous venovenous hemofiltration: a prospective randomized study. Intensive Care Med 30:260–265
Oudemans-Van Straaten HM, Bosman RJ, Koopmans M, Van der Voot P, Wester J, Van der Spoel J, Dijksman L, Zandstra D (2009) Citrate anticoagulation for continuous venovenous hemofiltration. Crit Care Med 37:545–552
Betjes MG, van Oosterom D, van Agteren M, Van de Wetering J (2007) Regional citrate versus heparin anticoagulation during venovenous hemofiltration in patients at low risk for bleeding: similar hemofilter survival but significantly less bleeding. J Nephrol 20:602–608
Fealy N, Baldwin I, Johnstone M, Egi M, Bellomo R (2007) A pilot randomized controlled crossover study comparing regional heparinization to regional citrate anticoagulation for continuous venovenous hemofiltration. Int J Artif Organs 30:301–307
Wu MY, Hsu YH, Bai CH, Bai CH, Lin YF, Wu CH, Tam KW (2012) Regional citrate versus heparin anticoagulation for continuous renal replacement therapy: a meta-analysis of randomized controlled trials. Am J Kidney Dis 59:810–818
Zhang Z, Hongying N (2012) Efficacy and safety of regional citrate anticoagulation in critically ill patients undergoing continuous renal replacement therapy. Intensive Care Med 38:20–28
Davis TK, Neumayr T, Geile K, Doctor A, Hmeil P (2014) Citrate anticoagulation during continuous renal replacement therapy in pediatric critical care. Pediatr Crit Care Med 15:471–485
Bunchman TE, Maxvold NJ, Barnett J, Hutchings A, Benfield M (2002) Pediatric hemofiltration: Normocarb dialysate solution with citrate anticoagulation. Pediatr Nephrol 17:150–154
Bunchman TE, Maxvold NJ, Brophy PD (2003) Pediatric convective hemofiltration: Normocarb replacement fluid and citrate anticoagulation. Am J Kidney Dis 42:1248–1252
Symons JM, Brophy PD, Gregory MJ, Mcafee N, Somers MJ, Bunchman TE, Goldstein SN (2003) Continuous renal replacement therapy in children up to 10 kg. Am J Kidney Dis 41:984–989
Elhanan N, Skippen P, Nuthall G, Krahn G, Seear M (2004) Citrate anticoagulation in pediatric continuous venovenous hemofiltration. Pediatr Nephrol 19:208–212
Hothi DK, St George-Hyslop C, Geary D, Bohn D, Harvey E (2006) Continuous renal replacement therapy (CRRT) in children using the AQUARIUS. Nephrol Dial Transplant 21:2296–2300
Bunchman TE, Hackbarth RM, Maxvold NJ, Winters JW, Barletta GM (2007) Prevention of dialysis disequilibrium by use of CVVH. Int J Artif Organs 30:441–444
Rajasekaran S, Jones DP, Avent Y, Shaffer M, Elbahlawan L, Henderson N, Barfield RC, Morrison R, Tamburro RF (2010) Outcomes of hematopoietic stem cell transplant patients who received continuous renal replacement therapy in a pediatric oncology intensive care unit. Pediatr Crit Care Med 11:699–706
Symons JM, Chua AN, Somers MJ, Baum M, Bunchman T, Benfield M, Brophy P, Blowey D, Fortenberry J, Chand D, Flores F, Hackbarth R, Alexander S, Mahan J, Mcbryde K, Goldstein S (2007) Demographic characteristics of pediatric continuous renal replacement therapy: A report of the prospective pediatric continuous renal replacement therapy registry. Clin J Am Soc Nephrol 2:732–738
Brophy PD, Somers MJ, Baum MA, Symons J, Mcafee N, Fortenberry J, Rogers K, Barnett J, Blowey D, Baker C, Bunchman T, Goldstein S (2005) Multi-centre evaluation of anticoagulation in patients receiving continuous renal replacement therapy (CRRT). Nephrol Dial Transplant 20:1416–1421
Askenazi DJ, Goldstein SL, Koralkar R, Fortenberry J, Baum M, Hackbarth R, Blowey D, Bunchman TE, Brophy PD, Symons J, Chua A, Flores F, Somers MJ (2013) Continuous renal replacement therapy for children ≤10 kg: A report from the prospective pediatric continuous renal replacement therapy registry. J Pediatr 162:587.e3–592.e3
Chadha V, Garg U, Warady B, Alon U (2002) Citrate clearance in children receiving continuous venovenous renal replacement therapy. Pediatr Nephrol 17:819–824
Kreuzer M, Bonze K, Buscher R, Offner G, Ehrich J, Pape L (2010) Regional citrate anticoagulation is safe in intermittent high-flux haemodialysis treatment of children and adolescents with an increased risk of bleeding. Nephrol Dial Transplant 25:3337–3342
Smoyer WE, McAdams C, Kaplan BS, Sherbotie JR (1995) Determinants of survival in pediatric continuous hemofiltration. J Am Soc Nephrol 6:1401–1409
Fernández SN, Santiago MJ, López-Herce J, García M, Del Castillo J, Alcaraz AJ, Bellón JM (2014) Citrate anticoagulation for CRRT in children: comparison with heparin. Biomed Res Int 2014:786301
Liet JM, Allain-Launay E, Gaillard-LeRoux B, Barrière F, Chenouard A, Dejode JM, Joram N (2014) Regional citrate anticoagulation for pediatric CRRT using integrated citrate software and physiological sodium concentration solutions. Pediatr Nephrol 29:1625–1631
Soltysiak J, Warzywoda A, Kociński B, Ostalska-Nowicka D, Benedyk A, Silska-Dittmar M, Zachwieja J (2014) Citrate anticoagulation for continuous renal replacement therapy in small children. Pediatr Nephrol 29:469–475
Liao YJ, Zhang L, Zeng XX, Fu P (2013) Citrate versus unfractionated heparin for anticoagulation in continuous renal replacement therapy. Chin Med J 126:1344–1349
Basu RK, Devarajan P, Wong H, Wheeler DS (2011) An update and review of acute kidney injury in pediatrics. Pediatr Crit Care Med 12:339–347
Fortenberry J, Paden M, Goldstein (2013) Acute kidney injury in children: an update on diagnosis and treatment. Pediatr Clin N Am 60:669–688
Morgera S, Scholle C, Voss G, Haase M, Vargas-Hein O, Krausch D, Melzer C, Rosseau S, Zuckermann-Becker H, Neumayer HH (2004) Metabolic complications during regional citrate anticoagulation in continuous venovenous hemodialysis: single-center experience. Nephron 97:c131–c136
Swartz R, Pasko D, O’Toole J, Starmann B (2004) Improving the delivery of continuous renal replacement therapy using regional citrate anticoagulation. Clin Nephrol 61:134–143
Link A, Klingele M, Speer T, Rbah R, Poos J, Lemer-Graber A, Fliser D, Bohm M (2012) Total-to-ionized calcium ratio predicts mortality in continuous renal replacement therapy with citrate anticoagulation in critically ill patients. Crit Care 16:R97
Kozik-Jaromin J, Nier V, Heemann U, Kreymann B, Bohler J (2009) Citrate pharmacokinetics and calcium levels during high-flux dialysis with regional citrate anticoagulation. Nephrol Dial Transplant 24:2244–2251
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare there exists no conflict of interest.
Ethics statement
This study was approved by the institutional ethics committee.
Additional information
The original version of this article was revised to correct the rendering of the name of the author Jaime Fernández Sarmiento.
An erratum to this article is available at http://dx.doi.org/10.1007/s00467-016-3568-1.
Rights and permissions
About this article
Cite this article
Rico, M.P., Fernández Sarmiento, J., Rojas Velasquez, A.M. et al. Regional citrate anticoagulation for continuous renal replacement therapy in children. Pediatr Nephrol 32, 703–711 (2017). https://doi.org/10.1007/s00467-016-3544-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3544-9