Abstract
Background
Postoperative anastomotic leakage (PAL) is a serious complication of gastric cancer surgery. Although perioperative management has made considerable progress, anastomotic leakage (AL) cannot always be avoided. The purpose of this study is to evaluate whether intraoperative leak testing (IOLT) can reduce the incidence of PAL and other postoperative outcomes in gastric cancer surgery.
Materials and methods
In this meta-analysis, we searched the PubMed, Embase, and Cochrane Library databases for clinical trials to assess the application of IOLT in gastric cancer surgery. All patients underwent laparoscopic radical gastrectomy for gastric cancer surgery. Studies comparing the postoperative outcomes of IOLT and no intraoperative leak testing (NIOLT) were included. Quality assessment, heterogeneity, risk of bias, and the level of evidence of the included studies were evaluated. PAL, anastomotic-related complications, 30-day mortality, and reoperation rates were compared between the IOLT and NIOLT group.
Results
Our literature search returned 721 results, from which six trials (a total of 1,666 patients) were included in our meta-analysis. Statistical heterogeneity was low. The primary outcome was PAL. IOLT reduced the incidence of PAL [2.09% vs 6.68%; (RR = 0.31, 95% Cl 0.19–0.53, P < 0.0001]. Anastomotic-related complications, which included bleeding, leakage, and stricture, were significantly higher in the NIOLT group than in the IOLT group [3.24% VS 10.85%; RR = 0.30, 95% Cl 0.18–0.53, P < 0.0001]. Moreover, IOLT was associated with lower reoperation rates [0.94% vs 6.83%; RR = 0.18, 95% CI 0.07–0.43, P = 0.0002].
Conclusion
Considering the observed lower incidence of postoperative anastomotic leakage (PAL), anastomotic-related complications, and reoperation rates, IOLT appears to be a promising option for gastric cancer surgery. It warrants further study before potential inclusion in future clinical guidelines.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Gastric cancer is the fifth most commonly diagnosed cancer with over one million patients worldwide diagnosed each year [1, 2]. Approximately, one out of every twelve oncologic deaths can be attributed to gastric cancer [3]. Surgery is often the only curative treatment option for gastric cancer [4]. Although progress has been made in perioperative management, postoperative complication rates remain high following gastric cancer surgery, especially in low-volume centers [5]. Postoperative anastomotic leak (PAL) is a critical complication, with an incidence ranging from 2.1 to 14.6% in patients who underwent gastric cancer surgery [6,7,8,9]. These complications have far-reaching consequences, such as prolonged hospitalization, escalated healthcare costs, compromised quality of life, or even death [10,11,12].
Currently, detection of anastomotic continuity is performed through air or methylene blue testing, with or without gastroscopy. Intraoperative leak testing (IOLT) may be one of the most important preventive methods that can be performed during gastric cancer surgery [13]. If the IOLT is positive, the leak can be fixed during the operation to minimize the possibility of PAL. However, previous studies have shown controversial results with the use of IOLT. Some studies suggest that IOLT can reduce PAL [14,15,16], while other studies suggest that IOLT has no significant impact on PAL [17, 18]. Furthermore, IOLT may cause trauma in the anastomosis, or methylene blue may contaminate the area, leading to adverse reactions or necrosis [19]. Thus, the potential of IOLT for risk reduction remains a topic of debate in the literature.
IOLT is widely used in colorectal and bariatric surgery [20,21,22,23]. Limited studies evaluate the safety and feasibility of the anastomotic procedure with IOLT after gastric cancer surgery [24,25,26,27,28,29,30]. The aim of this study was to compare postoperative outcome of IOLT with no intraoperative leak testing (NIOLT) in gastric cancer surgery, which included PAL, anastomotic-related complications, 30-day mortality, and reoperation rates.
Materials and methods
This systemic review was registered at PROSPERO (CRD42023453854) and followed the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA)2020.
Literature search strategy
We performed a literature search for clinical studies using the PubMed, Embase, and Cochrane Library databases. Our search was focused on human studies. The following search strategy was used in PubMed and conducted in other databases accordingly: ((stomach neoplasms) and (endoscopy) and (intraoperative) and (anastomotic Leak)) or ((stomach neoplasms) and (stomach tube) and (intraoperative) and (anastomotic Leak)) or ((stomach neoplasms) and (endoscopy) and (intraoperative leak testing)) or ((stomach neoplasms) and (stomach tube) and (intraoperative leak testing)) or ((Gastrectomy) and (stomach tube) and (intraoperative leak testing)) or ((Gastrectomy) and (endoscopy) and (intraoperative) and (anastomotic Leak)) or ((Gastrectomy) and (stomach tube) and (intraoperative) and (anastomotic Leak)) or ((Gastrectomy) and (stomach tube) and (intraoperative) and (anastomotic Leak)) or ((endoscopy) and (intraoperative) and (anastomotic Leak)) or ((stomach tube) and (intraoperative) and (anastomotic Leak)) or ((endoscopy) and (intraoperative leak testing)) or ((stomach tube) and (intraoperative leak testing)). Studies including both an IOLT group and a NIOLT group were included. Clinical studies published before June 2023 were included. Moreover, we attempted to find all relevant literature by looking through the references of the included articles. In addition, we searched gray and unpublished literature through the PubMed, Embase, and Cochrane Library databases and the references attached to the relevant literature. We then analyzed the full text to find eligible studies.
Study selection
Studies were included in the meta-analysis if they met these criteria: (1) The clinical trials comparing the postoperative outcomes of IOLT with NIOLT in patients with gastric cancer who underwent radical gastrectomy. (2) PAL is a study outcome and the study also reported at least one of the following clinical outcomes: postoperative anastomotic-related complications, 30-Day mortality rates, or reoperation rates. (3) The study was published as a full text in English language. (4) Valid data and a full text of the study could be obtained successfully.
Exclusion criteria
Studies were excluded from our analysis for the following reasons: unavailable data, duplicate studies, only abstract available, animal experiments, reviews, case reports, and letters.
Data extraction
Articles were screened independently by two reviewers according to title and abstract. Disputes were resolved by a third reviewer. This process was then repeated with a full-text review for data extraction. The first author, publication year and origin country, number of subjects, mean age, BMI, tumor pathological stage, mode of operation, type of reconstruction, type and number of positive result on the intraoperative leak test, PAL, anastomotic-related complications, 30-day mortality, and reoperation rates were extracted. PAL can be diagnosed if patient met one of the following conditions: (1) Drainage of gastrointestinal or bile contents from the abdominal drainage tube; (2) Leakage of contrast medium from the drainage tube was observed on gastrointestinal radiography; (3) Extraction of methylene blue from the abdominal drainage tube after oral administration of methylene blue; (4) Incomplete gastrointestinal wall on abdominal CT examination and revealing gas and fluid leaks around the anastomosis; and (5) Identification of anastomotic leaks under endoscopy after surgery. We categorized anastomotic-related complications into three types: PAL, postoperative anastomotic bleeding, and postoperative anastomotic stricture.
Study quality and assessment of risk of bias
Two reviewers independently rated the risk of bias of the randomized control trials (RCTs) using the revised Cochrane risk of bias, version 2 (ROB 2) tool. The risk of bias in cohort studies was assessed by Risk of Bias in Non-Randomized Studies of Interventions (ROBINS-I).
Statistical analysis
Risk ratio (RR) and 95% confidence intervals (CIs) were calculated on pooled effects for dichotomous variables with a fixed-effect model. I2 was used to evaluate statistical heterogeneity with a value < 30% representing low heterogeneity, a value between 30 and 50% representing intermediate heterogeneity and > 50% representing high heterogeneity. Sensitivity, subgroup, and meta-regression analyses were performed to investigate potential sources of heterogeneity if necessary and possible. Begg’s and Egger’s tests were used to assess publication bias. P < 0.05 was regarded as statistically significant. Discrepancies were discussed and consensus was reached with an arbitrator. Stata software (version 17.0; Stata Corporation; College Station, TX) was used to perform all analysis.
Results
Literature search results
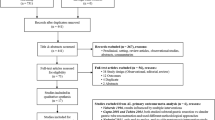
The systematic search revealed a total of 721 publications for possible inclusion (Fig. 1). Irrelevant publications, duplicate publications, or those not fitting our inclusion criteria were excluded based on title and abstract review. 129 publications were excluded based on the full text. Finally, six studies, including one prospective cohort study, four retrospective cohort studies, and one RCT were included [25,26,27,28,29,30].
Study characteristics
Our study included 1666 patients with 813 in the IOLT group and 853 in the NIOLT group. Four published studies [25, 27, 28, 30] implemented endoscopy for IOLT, while two studies adopted nasogastric tube for IOLT [26, 29]. Table 1 shows features of the included studies. Table 2 presents patient characteristics of the included studies.
Study quality
The risk of bias of the included studies are evaluated and listed in Fig. 2.
Intraoperative characteristics
There were 61 positive events including 11 air leakage, 20 venous bleeding, 8 mucosal tearing, 17 anastomotic leak, three arterial bleeding, and two anastomotic stricture events. Table 3 shows the types and number of positive events, which is identified by IOLT. Furthermore, additional reinforcing suturing was performed in 41 cases, endoscopic hemostasis in 16 cases, and re-anastomotic in three cases. After all repairs were completed, the leak test was conducted again until IOLT became negative.
Primary outcome-postoperative anastomotic leakage
Six studies reported PAL (Fig. 3). The PAL rates were 2.09% (17/813) in the IOLT group and 6.68% (57/853) in the NIOLT group. There was no significant heterogeneity (I2 = 0.0%, p = 0.95) when a fixed-effect model was used. PAL was significantly lower in the IOLT group than that in the NIOLT group (RR = 0.31, 95% Cl 0.19–0.53, P < 0.0001). No bias of publication was found with Begg’s (P = 1.000) and Egger’s (P = 0.494) tests.
Subgroup analysis
We performed subgroup analyses based on the different methods of intraoperative leak testing. Two studies employed air and methylene blue testing through the orogastric tube (OG group), while four studies used intraoperative endoscopy for leak testing (EN group). The PAL rate was 1.5% in patients with IOLT in the EN group, which was lower than the PAL rate of 4.1% in the OG group (P = 0.043). Furthermore, in the four studies with the EN group, PAL rate was lower in the IOLT group than in the NIOLT group (RR: 0.37, 95% CI 0.19–0.72, P = 0.004). Meanwhile, the two studies with an OG group, PAL rate was lower in the IOLT group than in the NIOLT group (RR: 0.24, 95% CI 0.10–0.58, P = 0.001) (Fig. 4).
Secondary outcomes
Postoperative anastomotic-related complications.
Four studies involving 955 patients evaluated the incidence of postoperative anastomotic-related complications. The incidence rates were 3.24% (15/494) in the IOLT group and 10.85% (51/461) in the NIOLT group. A fixed-effect model was used with no heterogeneity (I2 = 0.0%, P = 0.75). No bias of publication was found with Begg’s (P = 0.734) and Egger’s tests (P = 0.373). There was a statistically significant decrease in postoperative anastomotic-related complications rates in the IOLT group, when compared with that in the NIOLT group (RR = 0.30, 95% Cl 0.18–0.53, P < 0.0001) (Fig. 5).
30-Day mortality rates
Five studies included 30-Day mortality rates. The 30-day mortality rates were 0.13% (1/743) in the IOLT group and 0.64% (5/785) in the NIOLT group. Due to the lack of inter-study heterogeneity (I2 = 0.0%, P = 0.74), a fixed-effect model was used. The meta-analysis showed no significant difference in 30-day mortality rates between the two groups (RR = 0.33, 95% Cl0.06–1.73, P = 0.19) (Fig. 6).
Reoperation rates
Four studies involving 1,015 patients compared the incidence of reoperation rates. We found that IOLT was associated with a lower rate of reoperation (0.94% vs 6.83%; RR = 0.18, 95% CI 0.07–0.43, P = 0.0002) (Fig. 7). No bias of publication was found with Begg’s (P = 0.734) and Egger’s (P = 0.868) tests. Intermediate heterogeneity was detected (I2 = 48.5%, P = 0.14). Thus, a sensitivity analysis was conducted. For reoperation rates, heterogeneity primarily originated from the study conducted by Park et al. (Fig. 8). Statistical heterogeneity decreased in the three remaining studies and Park’s study was excluded (I2 = 32%, P = 0.23). A meta-analysis of the three trials demonstrated that the incidence of reoperation in the IOLT group is lower in the NIOLT group (RR: 0.05, 95% CI 0.01–0.40, P = 0.005).
Discussion
PAL is recognized as one of the most common and severe complications following gastric cancer surgery, with the potential to lead to hemodynamic instability, sepsis, multi-organ failure, and even mortality [18, 31]. It also associated with increased medical cost, length of hospital stay, and reoperation rate [12, 32]. PAL rate is an indication for the quality of gastric cancer surgery. IOLT, however, has the potential to reduce surgical complication in gastric cancer surgery [13]. To the best of our knowledge, this is the first meta-analysis, which compares the postoperative outcomes with or without IOLT in gastric cancer surgery. The main results of this study are as follows: (1) IOLT can reduce the incidence of PAL. (2) IOLT was associated with a reduction in anastomotic-related complications. (3) IOLT can reduce reoperation rate. (4) IOLT conducted by gastroscopy is better than that by oral gastric tube.
In this study, we found that IOLT can reduce the incidence of PAL. One study demonstrates that IOLT can successfully detect anastomotic leakage and allow for the repair of defects intraoperatively, which resulted in a reduction in PAL rates [24]. The result is consistent with our study. While some researchers found that IOLT cannot prevent all anastomotic leakage, such as late leakage and leakage caused by other factors, such as age, anemia, diabetes, malnutrition, or preoperative comorbidities [33, 34]. Our study demonstrates that IOLT has the ability to timely address anastomotic defects through additional suturing or re-anastomotic, which reduces anastomotic leakage. However, in this study, we also observed cases of PAL in patients showing negative results during intraoperative leak testing. This finding suggests that the etiology of anastomotic leakage is multifactorial and complex. Leak testing can address technical issues; it cannot prevent all risk factors associated with anastomotic leakage.
We also found that the implementation of intraoperative leak testing was associated with a reduction in anastomotic-related complications. Previous studies have suggested that intraoperative leak testing can reduce postoperative complications, such as anastomotic leakage, intraluminal bleeding, and anastomotic stricture [35, 36]. These findings are consistent with our study. IOLT allows direct visualization and repeated assessment of anastomoses, which enable the identification of potential defects and allow for timely repair, thereby improving postoperative outcomes. However, some studies have reported that intraoperative leak testing does not decrease postoperative anastomotic-related complications [17, 18]. In their opinion, insufflation and over-distention of the anastomosis have a negative impact on the newly constructed anastomosis. Gastroscopy or an oral gastric tube may injure the anastomosis. These factors potentially leading to anastomotic-related complications.
In this study, we found that IOLT could reduce reoperation rate, which may be attributed to the reduction of PAL, anastomotic bleeding, anastomotic stricture, etc. It is worth noting that in the study by Park et al., there were still five (1.6%) patients in the IOLT group who underwent reoperation after surgery. The possible reason for reoperation in the IOLT group was that while IOLT may aid in the early detection of anastomotic defects, it cannot address all factors leading to reoperation, such as diffuse peritonitis, sepsis with one or multi-organ failure, intraabdominal bleeding, or small bowel obstruction [31, 37, 38]. Further studies are needed to explore the impact of IOLT on reoperation rate in gastric cancer surgery.
The technique of IOLT has been applied in various ways in clinical practice. Some surgeons adopted air testing, while others use methylene blue testing with or without gastroscopy. Researchers found that IOLT performed with gastroscopy had a significantly lower incidence of PAL rates than that in IOLT performed with gastric tubes [39, 40]. These conclusions are consistent with our study findings. The difference in PAL rates between IOLT, conducted via gastroscopy or gastric tubes, could potentially be attributed to the following factors: Firstly, the direct visualization provided by gastroscopy during IOLT enables a more accurate assessment of anastomotic integrity. Secondly, the inherent properties of gastroscopy, such as its flexibility and ability to navigate intricate anatomic structures, which could contribute to its effectiveness in detecting even subtle abnormalities in the anastomotic site. It may be challenging to perform the procedure with the relatively rigid structure of gastric tubes, which may miss potential defects in the anastomosis. Thirdly, the utilization of gastroscopy allows for real-time adjustments and interventions, such as additional suturing or reinforcement to be performed. It is worth noting that the choice of IOLT technique may also be influenced by the availability of endoscopist, intraoperative gastroscopy equipment, as well as the surgeon’s experience and familiarity. Further comprehensive studies and standardized protocols are needed to establish the optimal approach for IOLT. We recommend the GAM procedure, which combines gastroscopy, air testing, and methylene blue testing for IOLT in gastric cancer surgery due to its comprehensive nature and superior results [41].
There are three limitations of our study. First, most of the included studies were retrospectively conducted, only one RCT was included, which may result in a high risk of bias in our study. Second, incomplete information of preoperative patient characteristics and intraoperative data were described, such as preoperative comorbidity, intraoperative gastrointestinal reconstruction methods, and surgical duration. Lastly, the lack of standardization of leak testing procedure may be a confounding factor in our study.
Conclusion
Considering the observed lower incidence of postoperative anastomotic leakage (PAL), anastomotic-related complications, and reoperation rates, IOLT appears to be a promising option for gastric cancer surgery. It warrants further study before potential inclusion in future clinical guidelines.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Jiang N, Deng JY, Ding XW, Zhang L, Liu HG, Liang YX, Liang H (2014) Effect of complication grade on survival following curative gastrectomy for carcinoma. World J Gastroenterol 20:8244–8252
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin 68:394–424
Rawla P, Barsouk A (2019) Epidemiology of gastric cancer: global trends, risk factors and prevention. Prz Gastroenterol 14:26–38
Brenkman HJ, Haverkamp L, Ruurda JP, van Hillegersberg R (2016) Worldwide practice in gastric cancer surgery. World J Gastroenterol 22:4041–4048
Pasquer A, Renaud F, Hec F, Gandon A, Vanderbeken M, Drubay V, Caranhac G, Piessen G, Mariette C (2016) Is centralization needed for esophageal and gastric cancer patients with low operative risk?: A Nationwide Study. Ann Surg 264:823–830
Makuuchi R, Irino T, Tanizawa Y, Bando E, Kawamura T, Terashima M (2019) Esophagojejunal anastomotic leakage following gastrectomy for gastric cancer. Surg Today 49:187–196
Carboni F, Valle M, Federici O, Levi Sandri GB, Camperchioli I, Lapenta R, Assisi D, Garofalo A (2016) Esophagojejunal anastomosis leakage after total gastrectomy for esophagogastric junction adenocarcinoma: options of treatment. J Gastrointes Oncol 7:515–522
Deguchi Y, Fukagawa T, Morita S, Ohashi M, Saka M, Katai H (2012) Identification of risk factors for esophagojejunal anastomotic leakage after gastric surgery. World J Surg 36:1617–1622
El-Sourani N, Bruns H, Troja A, Raab HR, Antolovic D (2017) Routine use of contrast swallow after total gastrectomy and esophagectomy: is it justified? Pol J Radiol 82:170–173
Aurello P, Cinquepalmi M, Petrucciani N, Moschetta G, Antolino L, Felli F, Giulitti D, Nigri G, D’Angelo F, Valabrega S, Ramacciato G (2020) Impact of anastomotic leakage on overall and disease-free survival after surgery for gastric carcinoma: a systematic review. Anticancer Res 40:619–624
Sierzega M, Kolodziejczyk P, Kulig J (2010) Impact of anastomotic leakage on long-term survival after total gastrectomy for carcinoma of the stomach. Br J Surg 97:1035–1042
Yoo HM, Lee HH, Shim JH, Jeon HM, Park CH, Song KY (2011) Negative impact of leakage on survival of patients undergoing curative resection for advanced gastric cancer. J Surg Oncol 104:734–740
Kanaji S, Ohyama M, Yasuda T, Sendo H, Suzuki S, Kawasaki K, Tanaka K, Fujino Y, Tominaga M, Kakeji Y (2016) Can the intraoperative leak test prevent postoperative leakage of esophagojejunal anastomosis after total gastrectomy? Surg Today 46:815–820
Causey MW, Fitzpatrick E, Carter P (2013) Pressure tolerance of newly constructed staple lines in sleeve gastrectomy and duodenal switch. Am J Surg 205:571–574
Sekhar N, Torquati A, Lutfi R, Richards WO (2006) Endoscopic evaluation of the gastrojejunostomy in laparoscopic gastric bypass. A series of 340 patients without postoperative leak. Surg Endosc 20:199–201
Kligman MD (2007) Intraoperative endoscopic pneumatic testing for gastrojejunal anastomotic integrity during laparoscopic Roux-en-Y gastric bypass. Surg Endosc 21:1403–1405
Bingham J, Lallemand M, Barron M, Kuckelman J, Carter P, Blair K, Martin M (2016) Routine intraoperative leak testing for sleeve gastrectomy: is the leak test full of hot air? Am J Surg 211:943–947
Sethi M, Zagzag J, Patel K, Magrath M, Somoza E, Parikh MS, Saunders JK, Ude-Welcome A, Schwack BF, Kurian MS, Fielding GA, Ren-Fielding CJ (2016) Intraoperative leak testing has no correlation with leak after laparoscopic sleeve gastrectomy. Surg Endosc 30:883–891
Lee JH, Chang CH, Park CH, Kim JK (2014) Methylene blue dye-induced skin necrosis in immediate breast reconstruction: evaluation and management. Arch Plast Surg 41:258–263
Kawai K, Iida Y, Ishihara S, Yamaguchi H, Nozawa H, Hata K, Kiyomatsu T, Tanaka T, Nishikawa T, Yasuda K, Otani K, Murono K, Watanabe T (2016) Intraoperative colonoscopy in patients with colorectal cancer: review of recent developments. Dig Endosc 28:633–640
Vallicelli C, Pirrera B, Alagna V, Fantini E, Palini GM, Zanini N, Garulli G (2020) Intraoperative endoscopy with immediate suture reinforcement of the defect in colorectal anastomosis: a pilot study. Updat Surg 72:999–1004
Minhem MA, Safadi BY, Tamim H, Mailhac A, Alami RS (2019) Does intraoperative endoscopy decrease complications after bariatric surgery? Analysis of American College of Surgeons National Surgical Quality Improvement Program database. Surg Endosc 33:3629–3634
Haddad A, Tapazoglou N, Singh K, Averbach A (2012) Role of intraoperative esophagogastroenteroscopy in minimizing gastrojejunostomy-related morbidity: experience with 2,311 laparoscopic gastric bypasses with linear stapler anastomosis. Obes Surg 22:1928–1933
Nishikawa K, Yanaga K, Kashiwagi H, Hanyuu N, Iwabuchi S (2010) Significance of intraoperative endoscopy in total gastrectomy for gastric cancer. Surg Endosc 24:2633–2636
Lieto E, Orditura M, Castellano P, Pinto M, Zamboli A, De Vita F, Pignatelli C, Galizia G (2011) Endoscopic intraoperative anastomotic testing may avoid early gastrointestinal anastomotic complications. A prospective study. J gastrointest Surg 15:145–152
Celik S, Almalı N, Aras A, Yılmaz Ö, Kızıltan R (2017) Intraoperatively testing the anastomotic integrity of esophagojejunostomy using methylene blue. Scand J Surg 106:62–67
Park JH, Jeong SH, Lee YJ, Kim TH, Kim JM, Kim DH, Kwag SJ, Kim JY, Park T, Jeong CY, Ju YT, Jung EJ, Hong SC (2020) Safety and efficacy of post-anastomotic intraoperative endoscopy to avoid early anastomotic complications during gastrectomy for gastric cancer. Surg Endosc 34:5312–5319
Alemdar A, Eğin S, Yılmaz I, Kamalı S, Duman MG (2021) Can intraoperative endoscopy prevent esophagojejunal anastomotic leakage after total gastrectomy? Hippokratia 25:108–112
Deng C, Liu Y, Zhang ZY, Qi HD, Guo Z, Zhao X, Li XJ (2022) How to examine anastomotic integrity intraoperatively in totally laparoscopic radical gastrectomy? Methylene blue testing prevents technical defect-related anastomotic leaks. World J Gastrointest Surg 14:315–328
Gao Z, Luo H, Ma L, Bai D, Qin X, Bautista M, Gong L, Peng Y, Hu J, Tian Y (2023) Efficacy and safety of anastomotic leak testing in gastric cancer: a randomized controlled trial. Surg Endosc 37:5265–5273
Chadi SA, Fingerhut A, Berho M, DeMeester SR, Fleshman JW, Hyman NH, Margolin DA, Martz JE, McLemore EC, Molena D, Newman MI, Rafferty JF, Safar B, Senagore AJ, Zmora O, Wexner SD (2016) Emerging trends in the etiology, prevention, and treatment of gastrointestinal anastomotic leakage. J Gastrointest Surg 20:2035–2051
Yi HW, Kim SM, Kim SH, Shim JH, Choi MG, Lee JH, Noh JH, Sohn TS, Bae JM, Kim S (2013) Complications leading reoperation after gastrectomy in patients with gastric cancer: frequency, type, and potential causes. J Gastric Cancer 13:242–246
Trapani R, Rausei S, Reddavid R, Degiuli M (2020) Risk factors for esophago-jejunal anastomosis leakage after total gastrectomy for cancer. A multicenter retrospective study of the Italian research group for gastric cancer. European J Surg Oncol 46:2243–2247
Tu RH, Lin JX, Zheng CH, Li P, Xie JW, Wang JB, Lu J, Chen QY, Cao LL, Lin M, Huang CM (2017) Development of a nomogram for predicting the risk of anastomotic leakage after a gastrectomy for gastric cancer. European J Surg Oncol 43:485–492
Nimeri A, Maasher A, Salim E, Ibrahim M, Al Hadad M (2016) The use of intraoperative endoscopy may decrease postoperative stenosis in laparoscopic sleeve gastrectomy. Obes Surg 26:1398–1401
Alasfar F, Chand B (2010) Intraoperative endoscopy for laparoscopic Roux-en-Y gastric bypass: leak test and beyond. Surg Laparosc Endosc Percutaneous Tech 20:424–427
Hummel R, Bausch D (2017) Anastomotic leakage after upper gastrointestinal surgery: surgical treatment. Visc Med 33:207–211
Kim DH, Park JH, Kim TH, Jung EJ, Jeong CY, Ju YT, Kim JY, Park TJ, Lee YJ, Jeong SH (2023) Risk factors for reoperation following radical gastrectomy in gastric cancer patients. Am Surg 89:1405–1413
Ruiz-Tovar J, Sola-Vera J, Miranda E, Muñoz JL, Perez-Rabasco E, Arroyo A, Calpena R (2014) Laparoscopic sleeve gastrectomy with endoscopic versus bougie calibration: results of a prospective study. J Laparoendosc Adv Surg Tech A 24:671–675
Alaedeen D, Madan AK, Ro CY, Khan KA, Martinez JM, Tichansky DS (2009) Intraoperative endoscopy and leaks after laparoscopic Roux-en-Y gastric bypass. Am Surg 75:485–488
Gao Z, Chen X, Bai D, Fahmy L, Qin X, Peng Y, Ren M, Tian Y, Hu J (2023) A novel intraoperative leak test procedure (GAM procedure) to prevent postoperative anastomotic leakage in gastric cancer patients who underwent gastrectomy. Surg Laparosc Endosc Percutaneous Tech 33:224–230
Acknowledgements
We want to thank Dr. Michael Hillel Kleinman from Surgical Associates of Houston, Texas. Dr. Michael Hillel Klein-man helped Dr. Yunhong Tian dedicate work to the surgical practice and research in Gastrointestinal Surgery.
Funding
This work was supposed by the Foundation of Sichuan Medical Association [S21025], the Cooperative project of Nanchong City with North Sichuan Medical College [20SXQT0321], and the Bureau of Science & Technology Nanchong City [22JCYJPT0007].
Author information
Authors and Affiliations
Contributions
YT, LH, and SL have made substantial contributions to the design of the work. YL and BL interpreted the patients’ data. LH, SL, and TH were major contributors in writing the manuscript. YT, LH, and LW have drafted the work or substantively revised it. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Disclosures
Heng Luo, Shunying Liu, Wentao Huang, Yu Lei, Yan Xing, Luke Wesemann, Binyu Luo, Wenjing Li, Jiani Hu, and Yunhong Tian have no conflicts of interest to disclose.
Ethical approval and consent to participate
This is a meta-analysis on anonymized data so ethical approval is considered unnecessary.
Consent for publication
No individual person’s data is included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luo, H., Liu, S., Huang, W. et al. A comparison of the postoperative outcomes between intraoperative leak testing and no intraoperative leak testing for gastric cancer surgery: a systematic review and meta-analysis. Surg Endosc 38, 1709–1722 (2024). https://doi.org/10.1007/s00464-024-10715-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-024-10715-z