Abstract
Background
Gastroesophageal reflux disease requiring an operative solution is common. Minimally invasive surgery to generate an anti-reflux barrier at the distal esophagus following the principle of the “floppy Nissen” technique has become the gold standard. Advanced robotic-assisted systems may deliver more consisted outcomes.
Methods
This registry study analyzed safety and efficacy of the Senhance® surgical system in the surgical treatment of reflux disease and procedural proficiency. Data from 237 consecutive patients operated in a single center were evaluated. Historic standard laparoscopies from the same center were analyzed to compare robotic surgery learning curve effects.
Results
Using the Senhance® Surgical System, during the first 50 patients there was a significant decrease in surgery time which was maintained over the duration of study, pointing to the surgical staff’s system-specific learning. After this phase, procedural times were comparable between the robotic-assisted and traditional laparoscopic surgery. The effect of learning was greater than for standard laparoscopy. For 237 patients, there were four conversions to laparoscopic surgery. Two serious adverse events were recorded, both cardiac in nature and not related to the use of the robot.
Conclusions
Robotic fundoplication was swiftly implemented in a non-university hospital with 65 surgical beds. The operating time was no longer than in standard laparoscopy, the procedure was more standardized than open or laparoscopic surgery and hospitalization times may have been sustainably shortened. The autonomy at the system’s digital platform (cockpit) to conduct robotic fundoplications is a big step forward in surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Robotic surgery in the upper gastrointestinal tract traditionally has been performed with several robotic systems often in a university setting with one specific operating room (OR) team and one operating surgeon. Overall, OR time was found to increase and acquisition, running and maintenance costs were deemed expensive [1]. The aim of this study was to observe the implementation of a Senhance® Surgical System (Asensus Surgical, Durham, North Carolina, USA) with movable arms, reusable instruments, and haptic feedback. The study results were recorded from the European TRUST registry [2]. The study is still ongoing, and this paper summarizes the findings of the analyses conducted for one high volume non-university center.
Minimally invasive surgery is causally linked to shorter hospital stays, less pain, and smaller incisions. Robotic platforms have been developed which show high accuracy and precision, including elimination of tremor and more recently haptic feedback, meaning that there is kinesthetic communication between the surgeon and the maneuverable instruments [3]. First experiences with robotic assisted surgery to perform fundoplication were collected in the late 1990s. Overall, the outcome matches that of laparoscopic fundoplication [4].
Reflux disease is clinically and endoscopically diagnosed, then iteratively treated with proton pump inhibitors, weight loss, and dietary adaptations before setting an indication for fundoplication, when symptoms cannot be controlled with more than 6 months’ therapy with proton pump inhibitors or patients deny taking PPI’s over decades [5, 6]. Fundoplication can be performed using different surgical methods which aim to reconstruct the esophageal sphincter. When open surgery and laparoscopic fundoplication according to Nissen were compared in a randomized clinical trial with long-term follow-up, laparoscopic fundoplication was found to be more successful in terms of fewer incisional hernias and fewer defective fundal wraps [7]. In conventional laparoscopy, close cooperation between the operating surgeon and the supporting surgeon maneuvering the camera is required. Trocar angulation can be straining for the supporting surgeon [8] and the assistant’s training level can have an impact on the procedural time [9].
The Senhance® Surgical System (Senhance® System) was developed with the laparoscopic surgeon in mind. Whilst the surgeon is seated at an ergonomic working platform (so-called cockpit), the assistant places the manipulator arms with trocars, and the surgeon directs the movements of the arms and instruments and remotely controls their activity (such as grasping, dissecting, cutting, approximating, suturing with articulating instruments, so-called parameters of autonomy delegated to the robot, [10]). The surgeon uses a high-definition 3D monitor for visualization of the situs. Particularly the suturing of the fundal wrap is thought to benefit from the accuracy and precision afforded by robotic delivery [11]. These factors in less accessible anatomical locations can be improved with the aid of a camera that trails close-up views in 3D and can be independently coordinated by the eye movement of the surgeon at the console. The significance of good quality camera navigation has already been documented for conventional laparoscopic fundoplication [12]. The advantage of the robotic camera control is the ability to hold perfectly still for an optimal 3D vision as well as less cleaning of the camera compared to human camera control. A recent retrospective study showed a significant post-interventional increase in patient-perceived quality of life after treatment of their gastroesophageal reflux using robotic Nissen fundoplication [13].
Materials and methods
Study design
A multicenter registry study (TRUST Registry) across five European nations was conceived to record safety, efficacy, and procedural proficiency of robotic assisted surgical intervention using the Senhance® system for indications specific to the centers. The registry captures surgical procedural data including conversions, i.e., the change-over of robotic-assisted laparoscopy to open laparoscopies, and data from a pre-discharge questionnaire. Adverse events were recorded for a total of 1 year after the procedure. The study is still ongoing, and this report summarizes findings of the analysis conducted on 7 July 2022 for one high volume surgical center (Evangelisches Krankenhaus Wesel, Germany), which specializes in reflux disease and repair, and which had a large enough cohort to study the center’s surgical team’s learning curve.
Patients
Patients were selected for fundoplication when suffering from esophageal reflux as a non-responder to proton pump inhibitors, a large hiatal hernia (> 3 cm) in gastroscopy, or significant acid reflux measured by pH Metry without achalasia. Achalasia patients were diagnosed by high-resolution manometry and sometimes barium swallow x-ray to determine the height of the stricture. Male and female adult patients with the indication for surgical intervention of gastroesophageal reflux disease who were surgically treated by robotic fundoplication with the support of the Senhance® system were consecutively included in the TRUST Registry study, beginning 17 July 2019.
Ethics and regulations
Ethical approval for the data collection under the TRUST registry study was obtained from the ethics committee of the initiating center (EC Ärztekammer Westfalen-Lippe and Westfälische Wilhelms-Universität) on 02 August 2018, local secondary votes were obtained following legal requirements.
For prospective data collection, adult patients were enrolled after obtaining their informed consent, for retrospective data collection, patients gave their informed consent to handle their data after robotic surgery. The study followed ISO14155 and MDR for the use within its intended purpose of a CE marked medical device with regulatory approval in Europe, following the medical association’s professional code of conduct, and data protection regulation.
The study was published in the German Clinical Trials register (DRKS-ID: DRKS00013461) and on clinicaltrials.gov (NCT03385109). A safety advisory committee of experts and independent assessors assessed all adverse events (Fig. 1).
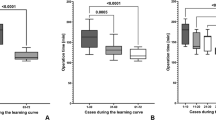
a Regression analysis for all patients consecutively plotted, against surgery duration. b Box Whisker plots from data shown in Table 2. Patients were ordered consecutively, and surgery time was plotted. c Representation of surgery times plotted for consecutive patients extracted for individual surgeons (1, 2, 3)
Procedure
Standard local anesthesia for the creation of the port sites was injected. The Senhance® System was used according to the manufacturer’s specifications. The five trocars were positioned as in a standard laparoscopic fundoplication procedure (using 10 mm-and 5 mm-trocars) (Fig. 2). Use of 5 mm articulating instruments has been documented in the test phase by our group as advantageous in this system [15]. The Martin arm was used as a liver retractor. The patient was positioned according to Fowler (15–18°) (Fig. 3).
Table height was adjusted according to body weight or abdominal size, and between 135 and 145 cm from the floor to the umbilicus. Prior to performing routine operations, three surgeons were trained for robotic surgery during a three-day training program which included hands-on training in the European Training Center of Asensus Inc. in Milan, Italy [8]. Two of these three surgeons regularly performed laparoscopy and fundoplication (Hansen, Menke). The OR was adapted for the Senhance® System and OR nurses were all trained with the system. To perform hiatoplasty and hemi-fundoplication, non-absorbable barbed suture gage 2–0 or non-absorbable polyester multifilament suture gage 2–0 was used. The intraabdominal pressure (during operative pneumoperitoneum) was standardized at 12 mmHg. Abdominal wall closure was performed with absorbable braided suture gage 3–0 and skin closure with monofilament nylon suture gage 4–0.
Endpoints
Adverse and serious adverse events were assessed by the operator and entered into the database and consecutively re-evaluated by the safety board led by Professor Willeke. Particularly, potentially robot related adverse events were evaluated (primary endpoint). Efficacy of Senhance® Surgical Robotic system supported procedures—based on indicators of procedural success, % conversion to standard laparoscopic surgery or open surgery and patient reported outcome for pain recorded using Visual Analog Scale (VAS)—was a secondary endpoint. The VAS was a ten-point scale, where 0 is no pain, 5 stands for moderate and 10 means worst possible pain. Further secondary endpoints procedural times (cut-suture time, console time, docking time of the system) and hospitalization times were recorded and analyzed. General patient demographics were recorded and reported.
Historic data for standard laparoscopic fundoplication
Data was retrieved from the hospital’s registry for quality in care management recorded for the Society of Surgeons for all 167 patients undergoing laparoscopic fundoplication from 2016 to 2019 and anonymized. Perceived pain, pain medication, incision-to-suture times and hospital stay times were analyzed and expressed as means ± SD. Surgical learning time was analyzed for one surgeon and benchmarked against a senior surgeon.
Statistical analysis
Registry data were analyzed by descriptive statistics using the statistical software SAS® 9.4 (TS1M6 or later) for Microsoft Windows. Metric values are presented as mean and median; the measure of variation is given as standard variations and quartiles. All statistical tests were two-sided using a significance level (alpha) of 0.05. All confidence intervals were two-sided 95% confidence intervals. The statistical analyses were performed using SAS. For the analysis of surgery times across groups, the general linear model, GLM, procedure was used. For the dependent variable, the values the surgery time were replaced by ranks. The χ2 test was used for comparison of percentages.
Registry and historic data from the hospital’s safety registry was not quantitatively compared because there was no demographic information and criteria for discharge from surgical wards changed as of October 2017 [16].
Results
Cohort
At an average of 9.48 cases per month, 58.23% of all gastrointestinal laparoscopic procedures performed with the Senhance® robotic system at the study center were fundoplications. In total, 237 cases were analyzed in July 2022, of them 221 first cases and 16 reoperations (6 male and 10 female patients). There were more women than men in the cohort, and patients were mostly overweight (BMI > 25 kg/m2). With regard to prior abdominal surgeries, 21.1% had had at least one open abdominal surgery, 36.7% had had at least one laparoscopic abdominal surgery; taken together, 49.4% had had at least one abdominal surgery (Table 1). Most fundoplications (95.4%) were performed according to Lortat-Jacob [17]. Hiatoplasty was performed in 91.14% and was mostly dorsal. The indications were mostly reflux esophagitis and hiatal repair, large hernia, or gastroesophageal reflux disease. Duration of stay for 234 patients was (average ± SD) 3.6 ± 1.7 days, with a range of 2–19 days. Local anesthesia for the creation of the port sites was administered in 99.6% of the patients.
Analysis of safety
Severe adverse events were only seen in 2 of the 237 patients and were cardiac in nature, with one case requiring emergency cardiac stent implantation. With this, the safety profile of the robotic fundoplication was good compared to the acute complications of laparoscopic fundoplication, because in robotic fundoplication we did not see esophageal perforation, bleeding or infection. To evaluate the prolonged complications of robotic fundoplication, our study includes a short follow-up time; a reoperation occurred in 4 out of 237 patients because of persistent dysphagia due to adhesions with esophageal stenosis. In literature, persistent dysphagia due to fundoplication related stenosis without herniation may occur in 10% of cases [14], which means robotic fundoplication is at the lower end of prolonged complications in larger groups described for laparoscopic procedures.
Analysis of efficacy
In four patients, robotic fundoplication was converted into standard laparoscopic surgery. The conversion occurred within the first 25 cases for three patients and once more in the next 25 cases that were followed consecutively (Table 2). There were no conversions to open surgery. Postprocedural pain (one day after) was recorded using the pain visual analog scale. Analgesics were used mainly at WHO medication level 1 (43.83%). 40.85% required combination analgesia levels 1 and 3 (Table 3). Pain at discharge was scored lower across a lower range compared to post procedurally (Table 4).
Technological-logistical analysis
Three robotic arms were used. Typically, the camera trocar was inserted supra-umbilically, robotic arm one in the left lumbar region and robotic arm two in the right hypochondrial region (Figs. 2, 3).
Adverse effects related to the medical device were recorded as follows for the first 158 laparoscopies conducted with the Senhance® system: In one case, the console malfunctioned and conversion to laparoscopic surgery ensued. In another, there was trocar collision for anatomical reasons (hepatomegaly). There was camera malfunction in one case and other robotic malfunctions in five cases. No malfunctioning was recorded for all ensuing cases (159 to 237). As a further device related observation, we saw limited motion of the robot-arms in only two cases. With readjustments of the positioning of the arms this could be solved.
The camera (with 3D function) was always positioned in the 10 mm-trocar. Mostly, the 30° optic was used, occasionally the 0°. Passive, monopolar or bipolar instruments were used. Ultrasonic was used in 98.7% of cases. The monopolar L-hook electrode (diameter 5 mm, 310 mm length) was used in 2.1% of cases and the articulating bipolar atraumatic grasper (diameter 5 mm, 310 mm length) in 0.4% of cases. In the category of passive instruments (5 mm diameter), the Johan grasper (length 310 mm) was used in 92.41%. A needle holder (left) (5 mm diameter, 310 mm length) was used in 97.47%. In 38.8% of cases, the sutures were fixated with clips and the rest was sutured. Surgery was performed by one of three expert surgeons but the other members of the OR team, including anesthetists, were random. The pool of assisting surgeons consisted of eight assistant surgeons and three console-trained surgeons. All participating surgeons received training according to manufacturer’s guidelines. Surgery, docking, and console times were recorded for all robotic assisted fundoplications.
Analysis of learning
Surgery times were plotted for all patients as they were consecutively entered in the database. Incision-to-suture time was 80.7 ± 28.5 min (mean ± SD). Docking time (i.e., camera connected to the robot arm to start of console time) was 5.4 ± 4.0 min and console time (i.e., robotic start to robotic end) was 46.9 ± 23.5 min (mean ± SD). Regression analysis showed a significant decline in surgery time for the consecutively treated patients (Fig. 1A). In fact, surgery time shortened by 0.14 min per patient, implying learning. Next, patients were divided into groups of 25 (and a final group of 37) to analyze any time dependent change in delivery of the robotic fundoplications for subgroups (Table 2). After the first 25 patients, a reduction in surgery time was already observed. There was a significant reduction in surgery time after the first fifty patients, which was maintained throughout (Fig. 1B). Individual performance for three lead surgeons is plotted in Fig. 1C. Of note, the procedures for patients 1–50 were conducted over a time span of 17 months, the next group of 25 patients were treated over 4 months, then intervals shortened to three months and then to two months.
Next, we extracted anonymized data from historic laparoscopic fundoplications conducted in our center prior to the introduction of Senhance®.
Retrospective analysis of 167 patients undergoing laparoscopic fundoplication from 2016 to 2019 showed that two conversions to open surgery were needed. Length of hospital stay time in this historic data set was much longer (6.4 ± 1 days (n = 165), compared with 3.6 ± 1.7 days (averages ± SD), see above). Pain was managed at WHO level 1 in 98.4% of 167 cases; of these 88% required analgesia levels 1 and 2, 16.2% levels 1 and 3, while 13.8% received analgesics across all three levels. Overall, pain severity postoperatively and at discharge was similarly scored in the historic compared to the robotic surgeries: postoperatively (at one day) 2.94 ± 1.69 and at discharge 0.74 ± 1.13 using the VAS scale (n = 164, three missing data). Previously, level 3 analgesics were preferentially given when levels 1 and 2 were co-administered. For 2017 and 2018, operating times were extracted for a junior and teamed senior surgeon and analyzed. There was a decline in surgical time (incision-to-suture) for the junior surgeon in 2018 (from 99.54 ± 22.9 for n = 13 to 91.24 ± 24.9 min, for n = 34). The senior surgeon spent 77.9 ± 21.2 min on each case in 2017 (n = 13) and 88.7 ± 39.9 min in 2018 (n = 30), likely due to more re-do surgeries in that year. Overall incision-to-suture times for all 142 primary laparoscopies (excluding repairs) from 2016 to 2019 for all six surgeons were 81.2 ± 28.4 min. This value is comparable to that recorded for the robotic assisted surgery time of the 237 patients reported in this study (80.7 ± 28.5 min, see above).
Discussion
This report is the center-specific extract of data collected as part of an ongoing large registry study [18]. The completeness of datasets benefitted from careful trial monitoring of data entries. Gastroesophageal reflux disease, reflux esophagitis and symptomatic hiatal hernias, large hernias and intrathoracic stomach were indications for robotic assisted fundoplication that were recorded in the registry of one participating center using the Senhance® system. Robotic assisted surgery for gastroesophageal reflux was introduced against a backdrop of highly successful laparoscopic surgeries [19], which were hailed an innovative advancement over open surgery that significantly reduced hospital stays, treatment costs, mortality, and morbidity [20]. In other indications of upper gastrointestinal surgery, robotic versus laparoscopic Heller myotomy was performed to treat achalasia (due to increased sphincter tonus) and was found in a retrospective study to be safer (avoidance of esophageal perforations) but equally effective [21]. Robotic fundoplication has been used successfully to repair sliding as well as large paraesophageal hernias, which are inherently difficult to approach in minimally invasive surgery. In this study, learning curves were deemed important to increase the greater surgical dexterity afforded by the system [22]. Washington et al. demonstrated over a two-year period a decrease in operating time by the same surgeon performing robotic assisted hiatal hernia repair and moreover, avoidance of conversion to open surgery [23]. A randomized clinical trial of patients with reflux disease found that conversion to standard laparoscopy from robotic fundoplication was necessary in one of 25 cases. Skin-to skin time was 78 ± 17.5 (average ± SEM) with a range of 48–104 min [24]. In our cohort, four of 237 cases were performed laparoscopically when the Senhance® system experienced a technical problem, and this occurred only at the inception of use of the robotic system at our site.
Evidence of a significant learning effect was shown in our study when analyzing the surgery times of all consecutively treated patients. When querying the length of surgery over time for all fundoplications performed at the site, there was a significantly decreased duration, indicative of an increase in robot-associated surgical aptitude. An exchange of best practices within the robotic surgical team facilitates improved quality and reduced procedural times in robotic fundoplication. This exchange should involve the entire OR team to include surgeons, nurses, and anesthesiologists. The learning curve is related to the robotic-specific surgical skills, but the largest improvement was standardizing the position of the movable arms, the small number of instruments and instrument-changing, avoiding camera failure with cleaning as a consequence. The situation of the operating surgeon distanced from the patient at the console allows for an optimized positioning of the patient on the operating table as opposed the classic beach chair position, in which the surgeon has to stand in between the patient’s legs. As these factors became standardized in the teams, the OR time became more stable, so that the anesthesiologists could calculate medication and OR time better with anesthetics given.
In other publications, the success of robotic fundoplications performed at one center was analyzed in a prospective study of 100 patients with complex histories of failed procedures, large hiatal hernias, or possibly considerable postoperative adhesions. A decrease of surgery duration over time and greater inclusion of patients who had had previous abdominal surgeries was found when stratifying patients into consecutive groups over the entire study duration from January 2013 to September 2019 [25]. This again indicates an increase in user confidence of the robotic system and is in keeping with findings from our study that analyses registry data of a large group of patients treated at one center. Compared to our historic data on laparoscopic fundoplication, it suggests that technical advance and surgical agility combine to maintain a skin-to-skin time that shows an equal procedural time in both methods (overall means of 81.2 and 80.7 min with comparable SDs), while hospital time can be further reduced (from a week to a few days). This might not only be a result of improved techniques and patient care, though, since a change in reimbursement policy during the study might have influenced hospitalization times [16]. Nevertheless, we do see a difference in in-hospital times after robotic assisted surgery, without a significant difference in pain score, pain medication, blood loss or complications. Therefore, we need larger studies to find a statistical significance.
Historic data were analyzed to obtain the extent of learning times in standard laparoscopies. They corroborate the impression that initial surgery times recorded for the first 25 patients receiving procedures with the Senhance® system were indeed longer than usual, assuming that senior surgeons took the lead when introducing the system to the site.
The robotic generation of minimally invasive surgery overcomes restrictions of conventional laparoscopies [10, 26]. Our data shows that duration of surgery time can be stably minimized after training and that the development of routine best practice by the entire team (contrasting with Samar et al. [27]) is essential. We note from our center an increase in Senhance® assisted fundoplication in which skillsets are maintained and produce shortened surgery times as the team expands.
Finally, it would be useful to measure among the surgical staff their appraisal of physical and psychological strains experienced in laparoscopic versus robotic surgery. This aspect was instrumental for the design of the Senhance® system but its subjective impact on practitioners’ skills to perform minimal invasive surgery has not yet been evaluated as part of a study. Scores to do so exist [28]. A future, pragmatic, study with longer follow-up, could provide evidence on the factors to decide in favor of using the Senhance® system and the frequency of hiatal repairs for our center. In conclusion, our registry study of real-world data collected at one high-throughput center from patients with reflux disease, for which there was a clinical need for surgery, showed safety, efficacy and procedural proficiency of robotic fundoplication. Moreover, we could demonstrate a learning associated improvement of surgical skills using the Senhance® system, as evidenced by a significant reduction of surgery time. The long-term outcome of our cohort of patients will be subject to further analyses. From other studies, there are early indications of competitive long-term efficacy of robotic fundoplications in comparison with conventional laparoscopic fundoplication [29].
References
Higgins RM, Frelich MJ, Bosler ME, Gould JC (2017) Cost analysis of robotic versus laparoscopic general surgery procedures. Surg Endosc 31(1):185–192. https://doi.org/10.1007/s00464-016-4954-2
The TRUST European Registry working group: Frank Willeke, Dietmar Stephan, Siegen, Germany; Narimantas Salamavicius, Klaipeda, Lithuania; Zeljko Kastelan, Zagreb, Croatia; Yuri Slabadzin, Minsk, Belarus; Ludger Staib, Esslingen, Germany; Johannes Schmidt, Landshut, Germany; Michael Lein, Offenbach, Germany; Christian Jackisch, Offenbach, Germany; Olaf Hansen, Wesel, Germany; Burghard Abendstein, Feldkirch, Austria
Rudiman R (2021) Minimally invasive gastrointestinal surgery: From past to the future. Ann Med Surg 71:102922. https://doi.org/10.1016/j.amsu.2021.102922
Rebecchi F, Allaix ME, Morino M (2017) Robotic technological aids in esophageal surgery. J Vis Surg 3:7. https://doi.org/10.21037/jovs.2017.01.09
Koop H et al (2014) S2k guideline: gastroesophageal reflux disease guided by the German Society of Gastroenterology: AWMF register no 021–013. Z Gastroenterol 52(11):1299–1346
Labenz J, Armstrong D, Leodolter A, Baldycheva I (2015) Management of reflux esophagitis: does the choice of proton pump inhibitor matter? Int J Clin Pract 69(7):796–801. https://doi.org/10.1111/ijcp.12623
Salminen PT, Hiekkanen HI, Rantala AP, Ovaska JT (2007) Comparison of long-term outcome of laparoscopic and conventional Nissen fundoplication: a prospective randomized study with an 11-year follow-up. Ann Surg 246(2):201–206. https://doi.org/10.1097/01.sla.0000263508.53334.af
Stephan D, Sälzer H, Willeke F (2018) First experiences with the new Senhance® telerobotic system in visceral surgery. Visc Med 34(1):31–36. https://doi.org/10.1159/000486111
Moore MD, Afaneh C, Gray KD, Panjwani S, Fahey TJ 3rd, Pomp A, Zarnegar R (2017) The impact of the robotic platform on assistant variability in complex gastrointestinal surgery. J Surg Res 219:98–102. https://doi.org/10.1016/j.jss.2017.05.127
Fiorini P, Goldberg KY, Liu Y, Taylor RH (2022) Concepts and trends in autonomy for robot-assisted surgery. Proc IEEE Inst Electr Electron Eng 110(7):993–1011. https://doi.org/10.1109/JPROC.2022.3176828
Schmitz R, Willeke F, Darwich I, Kloeckner-Lang SM, Saelzer H, Labenz J, Borkenstein DP, Zani S (2019) Robotic-assisted nissen fundoplication with the Senhance® Surgical System: technical aspects and early results. Surg Technol Int 35:113–119
Huettl F, Lang H, Paschold M, Bartsch F, Hiller S, Hensel B, Corvinus F, Grimminger PP, Kneist W, Huber T (2020) Quality-based assessment of camera navigation skills for laparoscopic fundoplication. Dis Esophagus 33(11):42. https://doi.org/10.1093/dote/doaa042
Konstantinidou SK, Kostaras P, Anagnostopoulos GE, Markantonis SL, Karalis V, Konstantinidis K (2021) A retrospective study on the evaluation of the symptoms, medications and improvement of the quality of life of patients undergoing robotic surgery for gastroesophageal reflux disease. Exp Ther Med 21(2):174. https://doi.org/10.3892/etm.2020.9605
Yadlapati R, Hungness ES, Pandolfino JE (2018) Complications of antireflux surgery. Am J Gastroenterol 113(8):1137–1147. https://doi.org/10.1038/s41395-018-0115-7
Stephan D, Darwich I, Willeke F (2020) First clinical use of 5 mm articulating instruments with the Senhance® robotic system. Surg Technol Int 37:63–67
Aßfalg V, Hassiotis S, Radonjic M, Göcmez S, Friess H, Frank E, Königstorfer J (2022) Einführung des Entlassmanagements an einer Universitätsklinik für Chirurgie: Explorative Analyse von Kosten, Verweildauer und Patientenzufriedenheit [Implementation of discharge management in the surgical department of a university hospital: exploratory analysis of costs, length of stay, and patient satisfaction]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 65(3):348–356. https://doi.org/10.1007/s00103-022-03497-z
Montinaro L, Paradies G, Leggio S (2002) The Lortat-Jacob operation by laparoscopic access to treat gastroesophageal reflux in pediatric patients. Preliminary results. Surg Endosc 16(10):1438–1440. https://doi.org/10.1007/s00464-001-9131-5
Stephan D, Darwich I, Willeke F (2021) The TransEnterix European Patient Registry for robotic-assisted laparoscopic procedures in urology, abdominal, thoracic, and gynecologic surgery (“TRUST”). Surg Technol Int 38:103–107. https://doi.org/10.52198/21.STI.38.GS1394
Zaninotto G, Molena D, Ancona E (2000) A prospective multicenter study on laparoscopic treatment of gastroesophageal reflux disease in Italy: type of surgery, conversions, complications, and early results. Surg Endosc 14(3):282–288. https://doi.org/10.1007/PL00021300
Richards KF, Fisher KS, Flores JH, Christensen BJ (1996) Laparoscopic Nissen fundoplication: cost, morbidity, and outcome compared with open surgery. Surg Laparosc Endosc 6(2):140–143
Horgan S, Galvani C, Gorodner MV, Omelanczuck P, Elli F, Moser F, Durand L, Caracoche M, Nefa J, Bustos S, Donahue P, Ferraina P (2005) Robotic-assisted Heller myotomy versus laparoscopic Heller myotomy for the treatment of esophageal achalasia: multicenter study. J Gastrointest Surg 9(8):1020–1029
Arcerito M, Changchien E, Falcon M, Parga MA, Bernal O, Moon JT (2018) Robotic fundoplication for gastroesophageal reflux disease and hiatal hernia: initial experience and outcome. Am Surg 84(12):1945–1950
Washington K, Watkins JR, Jeyarajah DR (2020) The first year is the hardest: a comparison of early versus late experience after the introduction of robotic hiatal hernia repair. J Robot Surg 14(1):205–210. https://doi.org/10.1007/s11701-019-00967-6
Morino M, Pellegrino L, Giaccone C, Garrone C, Rebecchi F (2006) Randomized clinical trial of robot-assisted versus laparoscopic Nissen fundoplication. Br J Surg 93(5):553–558. https://doi.org/10.1002/bjs.5325
Luberice K, Ross S, Crespo K, De La Cruz C, Dolce JK, Sucandy I, Rosemurgy AS (2021) Robotic complex fundoplication in patients at high-risk to fail. JSLS 25(2):e2020.00111. https://doi.org/10.4293/JSLS.2020.00111
Basunbul LI, Alhazmi LSS, Almughamisi SA, Aljuaid NM, Rizk H, Moshref R (2022) Recent technical developments in the field of laparoscopic surgery: a literature review. Cureus 14(2):e22246. https://doi.org/10.7759/cureus.22246
Samar AM, Bond A, Ranaboldo C (2022) Comparison of FreeHand® robot-assisted with human-assisted laparoscopic fundoplication. Minim Invasive Ther Allied Technol 31(1):24–27. https://doi.org/10.1080/13645706.2020.1771373
Wijsman PJM, Molenaar L, Van’t Hullenaar CDP, van Vugt BST, Bleeker WA, Draaisma WA, Broeders IAMJ (2019) Ergonomics in handheld and robot-assisted camera control: a randomized controlled trial. Surg Endosc 33(12):3919–3925. https://doi.org/10.1007/s00464-019-06678-1
Lang F, Huber A, Kowalewski KF, Kenngott HG, Billmann F, Billeter AT, Fischer L, Bintintan VV, Gutt CN, Müller-Stich BP, Nickel F (2022) Randomized controlled trial of robotic-assisted versus conventional laparoscopic fundoplication: 12 years follow-up. Surg Endosc 36(8):5627–5634. https://doi.org/10.1007/s00464-021-08969-y
Acknowledgements
Funding was received from Asensus Surgical to conduct the study. Christina Hönig, safety controller (Evangelisches Krankenhaus Wesel GmbH) is acknowledged for her help in extracting data on conventional laparoscopic surgery times. Independent data analysis, statistical evaluation, and drafting of the manuscript were outsourced to CRO Dr Kottmann GmbH &Co. KG (Hamm, Germany). The STROBE checklist was followed.
Funding
Asensus Surgical Inc., Durham NC, U.S.A. as part of the TRUST registry sponsorship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Vivianda Menke and Olaf Hansen have no conflicts of interest or financial ties to disclose, Frank Willeke has received structural support for the implementation of the TRUST study, Tanja Kottmann is the CEO of CRO Dr. Kottmann.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Menke, V., Kottmann, T., Willeke, F. et al. Learning curves and procedural times in Senhance®-robotic assisted fundoplication: results from 237 consecutive patients undergoing robotic fundoplication in a single center as part of the European TRUST Robotic Surgery Registry Study. Surg Endosc 37, 8254–8262 (2023). https://doi.org/10.1007/s00464-023-10226-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10226-3