Abstract
Introduction
Umbilical hernia repair (UHR) is a common operation with varying surgical approaches. Laparoscopic (LUHR) and open (OUHR) operations are routinely performed, but their impact on quality of life (QoL) is not well described. Our aim was to evaluate perioperative outcomes and QoL of LUHR versus OUHR.
Methods
The prospectively collected International Hernia Mesh Registry was queried for patients undergoing UHR with mesh placement. QoL was measured using the Carolinas Comfort Scale preoperatively and 1, 6, 12, and 24 months postoperatively. Propensity match was performed controlling for hernia defect size (HDS), recurrent hernias, and BMI.
Results
585 patients underwent 178 (30.4%) LUHR and 407 (69.6%) OUHR. LUHR patients had higher BMI, larger HDS, and more recurrent hernias (p < 0.05). Rates of other comorbidities were similar (p > 0.05). Tacks were used more frequently in LUHR (91.6% vs 1.7%, p < 0.001), and suture was used more often in OUHR (97.1% vs 47.8%, p < 0.001). Postoperative outcomes were similar (p > 0.05) except LUHR had higher rates of seroma (13.9% vs 4.3%, p < 0.001). Overall recurrence rates trended to favor OUHR, but not significantly (4.7% vs 8.4%, p = 0.07). The propensity match yielded 138 matched pairs. LUHR had more seromas and OUHR had higher infection rates (p < 0.05). Hernia recurrence was higher following LUHR (9.4% vs 2.9%, p = 0.02). QoL data were available for an average of 457 patients at each time period. QoL was superior in the OUHR group for pain and overall QoL at each time point and activity limitations at 6 and 12 months (p < 0.05). When examining patients who were asymptomatic preoperatively, OUHR had improved one-month overall QoL, but both groups had over 90% of patients report being asymptomatic postoperatively.
Conclusions
OUHR is associated with higher rates of surgical site infections, but significantly lower rates of seroma formation and hernia recurrence compared to LUHR, while having superior QoL in both short- and long-term follow-up. Asymptomatic patients tend to have excellent QoL outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Umbilical hernia repair is the second most common hernia operation performed in the US annually, with an incidence in the general population of 2% [1]. The two most common approaches to repair are laparoscopic (LUHR) and open (OUHR). While originally described as an open operation, the laparoscopic approach was introduced in the 1990s and has become a commonly practiced and effective technique. The use of mesh in both operations has been proven to decrease hernia recurrence rates [2]. Extensive research has been performed comparing the outcomes between the two techniques with varying results. Early studies focused on traditional outcomes measures: recurrence rates and complications. Previous studies found varied outcomes, including that OUHR had higher complication rates, length of stay, and recurrence rates [3,4,5,6]. In contrast, other studies found no difference in complications and recurrence rates between OVHR and LUHR [7,8,9]. In a study published in 2021 by Henriksen et al., a large retrospective analysis of over 6000 patients showed no significant difference between hernia recurrence rates [8]. This study additionally suggested that the likelihood of a severe complication requiring reoperation was increased during a laparoscopic hernia repair, while superficial surgical site infections and overall wound morbidity were increased with open repair [8]. The guidelines for treatment of umbilical and epigastric hernias from the European and Americas Hernia Societies also reflect this difference, making a weak recommendation that laparoscopic umbilical hernia repairs are indicated for larger > 4 cm hernia defects given the increased risk of wound morbidity with open repairs [10].
In the face of extensive research and conflicting data of the superior approach in outcomes, QoL data and patient reported outcomes have risen to new importance. Indeed, hernia operations are very often performed for QoL improvement, and therefore, the authors believe we should focus on QoL outcomes. There remains a paucity of evidence specifically evaluating QoL in patients undergoing umbilical hernia repair, with a recent review showing that patient report outcomes and QoL are poorly reported throughout the hernia literature [11, 12]. In a study from 2020, Fafaj et al. looked retrospectively at very short-term QoL outcomes and found no significant difference between OUHR and LUHR [7]. This study was focused on obese patients (BMI > 30), however, and provided no data on long-term outcomes. Colavita et al. previously studied the factors associated with an ideal outcomes and QoL in umbilical hernia repair, looking aspects such as approach, fixation technique, hernia characteristics, and suture type. They found that the use of sutures for mesh fixation with or without tacks as opposed to tacks alone was independently associated with an ideal QoL outcome. However, in that study, laparoscopic versus open technique, defect size, and absorbable versus permanent suture were not independently associated with an ideal outcome [13].
The aim of this study is to compare short and long-term QoL outcomes between LUHR vs OUHR, as well as the recurrence rates and complications. The study uses a prospectively collected international multicenter hernia database, which has traditionally had excellent patient follow-up, and a proven hernia QoL scale to create a data set that will translate to multiple settings and be useful to general surgeons.
Materials and methods
Study design
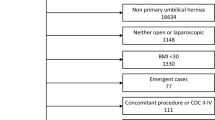
Approval was obtained from the Institutional Review Board of Carolinas Medical Center. Data were obtained from the International Hernia Mesh Registry (IHMR). This is an international, prospectively collected database that comprises centers from 13 countries across five continents. IHMR is registered as a clinical trial at ClinicalTrials.gov, ID NCT00622583 (https://www.clinicaltrials.gov/ct2/show/study/NCT00622583). Inclusion and exclusion criteria for participation in IHMR can be found in Table 1.
Data are collected prospectively and the collection encompasses patient demographic information, comorbidities, preoperative hernia characteristics, operative details, and postoperative outcomes with a goal follow-up of at least 2 years. Importantly, IHMR assesses pre- and postoperative QoL utilizing the Carolinas Comfort Scale (CCS). The CCS can be used to assess short and long-term QoL. The CCS has been validated for QoL assessment in patients undergoing hernia surgeries and is designed to assess short and long-term QoL. Studies have shown the CCS to be a superior assessment of QoL in hernia repair patients when compared to a generic Short Form 36 (SF-36) questionnaire [14, 15]. The survey assesses the incidence and severity of pain, activity limitation, and mesh sensation. It is given to patients without their surgeon in attendance to limit observer or collection bias. Each of these symptoms is assessed during seven different activities and at rest. Symptoms are scored on a six-point Likert scale (0 being no symptoms and 5 being disabling symptoms). For each symptom, an average score of zero (“none”) or one (“mild but not bothersome”) is classified as asymptomatic. Patients with an average score of 2.0 (“mild but bothersome”) or greater are deemed symptomatic. CCS scores were compared in patients undergoing LUHR versus OUHR. IHMR assesses QoL preoperative, and at 1 month, 6 months, 1 year, and 2 years postoperatively. At each time interval, groups are compared by average score of each symptom, as well as the overall average score.
Study was performed by querying IHMR for patient undergoing LUHR and OUHR with mesh from September 2007 to December 2019. Primary outcomes were QoL and hernia recurrence. Secondary outcomes were postoperative complications.
Propensity matching
A propensity-score nearest neighbor match was performed to compare patients undergoing LUHR and OUHR based on logistic regression analysis. This generated a 1:1 ratio of closely matched pairs. Matching criteria were hernia defect size, recurrent hernia, and BMI.
Statistical analysis
Descriptive statistics were reported as means with corresponding standard deviations for continuous variables, and percentages for categorical variables. Categorical variables were evaluated using Pearson’s Chi-squared tests and Fisher’s exact test when appropriate. Continuous and ordinal variables were evaluated using Wilcoxon–Mann–Whitney and the Kruskal–Wallis tests. Statistical significance was set at p ≤ 0.05, and all reported p values are two-tailed. Data were analyzed using Statistical Analysis Software, version 9.3 (SAS Institute, Inc., Cary, NC).
Results
A total of 585 umbilical hernia repairs with mesh were performed, with 178 (30.4%) LUHR and 407 OUHR (69.6%). Patient characteristics are shown in Table 2. Female patients accounted for 26.5% of patients undergoing umbilical hernia repair and the mean age was 51.8 years. The average BMI was approximately 3 points greater in laparoscopic patients, and laparoscopic patients accounted for a higher percentage of females. There were no statistically significant differences in the other preoperative comorbidities between the LUHR and OUHR groups.
Hernia and operative characteristics are detailed in Table 3. Laparoscopic hernias were more likely to be recurrent, incarcerated, and with a greater hernia defect size (HDS) (all p < 0.05). Mesh placement and fixation techniques differed between LUHR and OUHR, likely inherent to the differences in techniques for the two procedures. Open repairs had pre-peritoneal mesh placed in 55.5% of cases whereas LUHR patients were most likely to have an intraperitoneal only mesh (IPOM) (80.9%). Fixation techniques also expectantly differed with nearly all OUHRs undergoing suture fixation and nearly all LUHRs undergoing fixation with tacks alone or a combination or tacks and suture. Mesh weight was most likely to be midweight for both groups, 48.3% in the LUHR group and 63.1% in the OUHR.
Postoperative outcomes are compared in Table 4. The mean postoperative follow up for patients was 20 ± 11.0 months. Postoperative outcomes between the groups were largely similar on univariate analysis. While there trended toward an increased recurrence rate of LUHR (4.7% vs 8.4%, p = 0.07), it did not reach statistical significance. There were no differences in return to OR, hematoma, or superficial wound infection rates. However, LUHR had higher seroma rates compared to OUHR. Length of stay was also longer in the LUHR group, whose average LOS was over one day compared to an average LOS of under one day for the OUHR group.
Propensity score matching
Given the possible effects of the differences in BMI, recurrent hernias, and HDS, a propensity match was performed yielding 138 matched pairs. The seroma rate remained higher in the LUHR group (12.5% vs 4.4%, p = 0.01), however superficial wound infection rates were shown to be higher in OUHR (0.0% vs 3.7%, p = 0.02). The operative time and LOS continued to be longer in the laparoscopic group (all p < 0.05). Notably, the hernia recurrence was higher in the LUHR group at 9.4% vs 2.9% (p = 0.02).
Quality of life
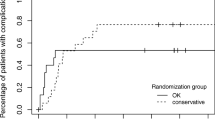
When considering all patients, QoL data were analyzed on an average of 457 patients (78.1% of total) preoperatively and at 1, 6, 12, and 24 months. Figure 1 shows comparisons for LUHR versus OUHR at each time interval for all four measured variables. Notably, preoperative QoL is similar between the groups in regard to pain, mesh sensation (only assessed in those with mesh in place preoperatively), and overall QoL. Activity limitation was worse in the LUHR group. Postoperatively, LUHR QoL never surpassed OUHR QoL in any variable at all follow-up intervals. OUHR had statistically significant improved QoL at in all four follow-up intervals for pain and overall QoL (all p < 0.05). Mesh sensation was improved in the OUHR group postoperatively at 1, 6, and 24 months (all p < 0.05). The OUHR group had decreased activity limitation at 1 and 24 months postoperatively (all p < 0.05).
We evaluated QoL data in the LUHR with regards to fascial closure. Fascial closure data were available on 66 (37.1%) of the 178 LUHR patients. Of those 66 patients, the fascial closure rate was 24.2%. Preoperatively, and at all four postoperative follow-up intervals, there was no difference in any QoL variables between LUHR patients who had their fascia closed and LUHR patients who did not have fascial closure (all p > 0.05).
To control for preoperative differences in QoL and the impact of preoperative symptoms on postoperative symptoms, we evaluated each variable individually using only patients who had a preoperative CCS score of less than 2 for the variable of interest (Fig. 2). Mesh sensation was not evaluated due to the low number of patients who had preoperative mesh. There was an average of 241 patients at each follow-up intervals for each of the CCS variables. Postoperative pain and activity limitation scores were low and decreased over time, and there were no differences between LUHR and OUHR at any time point (all p > 0.05). For all patients (LUHR and OUHR combined) with preoperative pain scores less than 2, only 5.2% at 12 months and 5.7% at 24 months reported a CCS of ≥ 2. Overall QoL was improved in the OUHR group in 1 month follow-up (p = 0.028), and similar at all other follow-up intervals (all p > 0.05).
Finally, we analyzed QoL in the propensity match subgroup with an average of 211 for each follow-up period. Pain and mesh sensation were similar preoperatively, yet the OUHR group had improved postoperative pain at 1 and 6 months follow-up, and improved mesh sensation at 6 months compared to LUHR (all p < 0.05). Activity limitation and overall QoL were worse preoperatively in the LUHR group (all p < 0.05), and postoperatively both variables were equivalent at 1, 12, and 24 months, with OUHR performing better for both at 6 months (all p < 0.05) (see Fig. 3).
Discussion
In an era where increased importance is being placed on patient reported outcomes, and for an operation often aimed at improving QoL, the tipping point when choosing between two procedures such as LUHR and OUHR that offer similar operative outcomes may, in fact, be postoperative QoL. In this evaluation of nearly 600 umbilical hernia repairs with mesh, postoperative outcomes and QoL were evaluated showing that for many patients, OUHR may afford patients improved QoL in the setting of similar or even superior surgical outcomes. The reach of this study is extensive as it utilizes the International Hernia Mesh Registry, a prospectively collected database from multiple centers across varying countries and continents. It effectively compares laparoscopic versus open umbilical hernia repair QoL data in one of the largest of such cohorts. In recent years, research has emerged evaluating QoL in laparoscopic versus open ventral hernia repair, however, there has less focus aimed at umbilical hernia repair.
A strength of this study involves utilizing the CCS, a QoL outcome survey that has been validated as a specific QoL assessment for hernia patients [14, 15]. It has been shown to be more effective in assessing QoL than generic QoL surveys [14]. The survey results were obtained by patient reported outcomes therefore limiting biases introduced by providers. Furthermore, it is given to patients in the absence of the surgeon further limiting observer and/or collection bias. The IHMR exclusively utilizes the CCS for its assessment of pre and postoperative QoL, and the database focuses on achieving high rates of long-term QoL follow-up. This is exemplified by the average of 457 survey responses (78.1% of the original cohort) per follow-up interval, including to 24 months postoperatively, making it an ideal database for evaluation of QoL outcomes in patients undergoing hernia repair with mesh.
In early research looking at laparoscopic versus open ventral hernia repair and QoL data, laparoscopic repairs were found to either have improved QoL or an equivocal difference when compared to open repairs. A 2008 review of 56 patients using the generic SF-36 survey and the CCS showed that laparoscopic ventral hernia repairs provided improved quality of life compared to open repairs at 6 months [15]. A subsequent randomized controlled trial comparing 84 patients found no difference in QoL between open and laparoscopic ventral hernia repairs through 1 year [16]. A study published in 2012 by Colavita et al. was one of the largest ventral hernia repair QoL studies published at that time. That study, which evaluated open and laparoscopic ventral hernia repairs and had excellent QoL follow-up, demonstrated an improved QoL after open repair in the short-term, with no difference in the long-term outcomes [17]. Our current study evaluating umbilical hernia repair shows improved QoL after open repair at all follow-up intervals in all four variables, in contrast to literature describing ventral hernia repair. This held true in both the entire cohort, and the propensity matched subgroup. This difference between ventral hernia repair and umbilical hernia repair may be due to the likely significant size variance in ventral compared to umbilical hernias.
While data looking at very short-term QoL outcomes after LUHR versus OUHR is limited, a 2020 retrospective review looking at short-term QoL outcomes in patients with BMI > 30 showed no difference between OUHR and LUHR (using HerQles score) [7]. This study specifically looked at outcomes only up to 30 days after surgery, while a strength of the current study is in its follow-up out to 2 years. This difference allows for longer term monitoring of mesh sensation, pain and activity limitations that would potentially not differ between OUHR and LUHR in the initial follow up. In another study published in 2013 by Colavita et al., they looked specifically at 363 umbilical hernia repairs and aimed at identifying predictors of ideal outcomes. Part of the ideal outcome measurement was QoL assessed using the CCS. An important finding of this study was that preoperative pain and other symptoms were significant predictors of postoperative pain and symptoms [13]. This finding is important to consider when evaluating hernia QoL data. In our study, we found that despite similar rates of reported preoperative pain, when compared to LUHR patients, the OUHR patients had improved pain related QoL at all intervals of follow-up. This trend was similar for mesh sensation and overall QoL. In this context, the improved QoL scores in the OUHR group when evaluating activity limitations may be less significant given the worse preoperative activity limitations in the LUHR group.
Given this knowledge of preoperative symptoms affecting the likelihood of postoperative symptoms, an analysis was performed on only patients reporting a normal preoperative QoL. This information would also be very important by adding to our ability to counsel asymptomatic patients regarding surgery preoperatively. In this analysis, despite the stringent definition used for negative QoL outcomes being a CCS score ≥ 2, patients reported remarkably good QoL postoperatively. Over 95% of LUHR and OUHR patients reported an ideal QoL in the context of pain and activity limitations at 2 years follow-up. Overall QoL also improved over time, with over 90% of patients reports ideal QoL at 2 years. Again, the knowledge that asymptomatic patients are at extremely low risk of having their QoL negatively impacted following an umbilical hernia repair with mesh is important, and can serve to ease anxiety concerning undergoing an UHR.
Hernia recurrence rates were equal between OVHR and LUHR on univariate analysis of the entire cohort, however, when controlling for BMI, recurrent hernias, and defect size, OUHR was found to have a statistically significant lower hernia recurrence rate with over 19 months average follow-up. Multiple studies, including a recent analysis of nearly 7000 patients from the Danish Hernia Database and National Patient Registry, have shown similar hernia recurrence rates when comparing LUHR and OUHR [7,8,9]. An important consideration is that in the setting of improved QoL, OUHR may be a superior technique in appropriate patients, whether it affords patients similar, or possibly even improved, recurrence rates.
As expected, this analysis of prospectively collected data confirms many of the previously reported outcome discrepancies when comparing LUHR and OUHR. Operative time was shorter in the OUHR while length of stay was longer in LUHR. Additionally, seroma rates were higher in LUHR. The overall analysis showed similar rates in superficial wound infections, however, the propensity matched data revealed a higher rate in OVHR, more in line with prior studies. Henriksen et al. in a 2021 review of 6855 patients also found that superficial skin infections were higher in OVHR [8]. A probable explanation for the increased rate of superficial wound infections in OVHR with propensity matching could be due to a larger peri-umbilical incision and the subcutaneous dissection. The increased risk of wound infections for OUHR is an important consideration when choosing an approach for umbilical herniorrhaphy, as patients who are high risk for infection may not be the best candidates for open repairs despite the benefits in QoL.
While minimally invasive approaches have come to the forefront of hernia repair and hernia research, the very common problem of the umbilical hernia, given the current data, may be best addressed via an open approach. With similar to improved recurrence rates, shorter operating times and length of stay, and significantly improved QoL, an OUHR should be strongly considered for each patient requiring an UHR. Further study is needed to determine ideal techniques, mesh types, and mesh fixation, although previous study utilizing earlier datasets from the IHMR database have deemed a mesh repair with suture fixation to lead to the most ideal outcomes [13]. Indeed, the fixation of the mesh may be a leading factor which decreases QoL in LUHR, and more sophisticated laparoscopic techniques, such as pre-peritoneal mesh placement, may shift QoL outcomes. Regardless, as previously mentioned, certain patients will likely still benefit from a LUHR, such as those who are at high risk for wound infections, or those whom an open operation may be technically challenging. Future research may be able to help delineate this patient population to aid in preoperative surgeon decision-making. With regards to QoL, this study has supplied a large multicenter subset of patients with strong long-term QoL reporting. Further evaluation as to QoL following umbilical hernia repair would benefit from a randomized controlled trial comparing hernia specific QoL outcomes in LUHR versus OUHR.
Our study must be taken in the context of its limitations. There are inherent limitations to analysis of data from large, multicenter databases, yet at the same time this offers our study generalizability across many different settings, practices, and populations. Additionally, the database focuses on collecting QoL data which is the primary outcome of this study. While there were key differences in certain preoperative characteristics, we were able to perform a propensity match controlling for these factors to analyze a subset of patients with similar preoperative qualities. Nonetheless, this study may fail to capture patient factors that influenced surgeons to choose either a LUHR or an OUHR, which may cause an unrecognized selection bias. Additionally, the database is limited in its ability to capture surgeon and hospital specific factors, such as experience and case volume, which are known factors that can influence hernia outcomes and recurrence rates.
In conclusion, OUHR has been found to have decreased recurrence rates when compared to LUHR, while providing patients improved short- and long-term QoL. Given these factors, in appropriate patients, OUHR may be the default approach for repairing umbilical hernias. OUHRs did have a higher rate of wound infections, which may play a role in patient selection when choosing between laparoscopic and open approaches, and there is likely still a subset of patients who will benefit from a laparoscopic approach. In the era of refining techniques and improving patient reported outcomes, further randomized controlled trials addressing QoL in umbilical hernia repair are warranted.
References
Dabbas N, Adams K, Pearson K, Royle G (2011) Frequency of abdominal wall hernias: is classical teaching out of date? JRSM Short Rep 2:1–6. https://doi.org/10.1258/shorts.2010.010071
Kaufmann R, Halm JA, Eker HH, Klitsie PJ, Nieuwenhuizen J, van Geldere D, Simons MP, van der Harst E, van ‘t Riet M, van der Holt B, Kleinrensink GJ, Jeekel J, Lange JF (2018) Mesh versus suture repair of umbilical hernia in adults: a randomised, double-blind, controlled, multicentre trial. The Lancet 391:860–869. https://doi.org/10.1016/S0140-6736(18)30298-8
Gonzalez R, Mason E, Duncan T, Wilson R, Ramshaw B (2003) Laparoscopic versus open umbilical hernia repair. JSLS 7:323–328
Solomon TA, Wignesvaran P, Chaudry MA, Tutton MG (2010) A retrospective audit comparing outcomes of open versus laparoscopic repair of umbilical/paraumbilical herniae. Surg Endosc 24:3109–3112. https://doi.org/10.1007/s00464-010-1097-8
Williams KN, Hussain L, Fellner AN, Meister KM (2020) Updated outcomes of laparoscopic versus open umbilical hernia repair in patients with obesity based on a national surgical quality improvement program review. Surg Endosc 34:3584–3589. https://doi.org/10.1007/s00464-019-07129-7
Köckerling F, Brunner W, Mayer F, Fortelny R, Adolf D, Niebuhr H, Lorenz R, Reinpold W, Zarras K, Weyhe D (2020) Assessment of potential influencing factors on the outcome in small (< 2 cm) umbilical hernia repair: a registry-based multivariable analysis of 31,965 patients. Hernia. https://doi.org/10.1007/s10029-020-02305-4
Fafaj A, Tastaldi L, Alkhatib H, Tish S, AlMarzooqi R, Olson MA, Stewart TG, Petro C, Krpata D, Rosen M, Prabhu A (2020) Is there an advantage to laparoscopy over open repair of primary umbilical hernias in obese patients? An analysis of the Americas hernia society quality collaborative (AHSQC). Hernia. https://doi.org/10.1007/s10029-020-02218-2
Henriksen NA, Jorgensen LN, Friis-Andersen H, Helgstrand F (2021) Open versus laparoscopic umbilical and epigastric hernia repair: nationwide data on short- and long-term outcomes. Surg Endosc. https://doi.org/10.1007/s00464-021-08312-5
Shaikh I, Willder JM, Kumar S (2013) Same day discharge, surgical training and early complications after open and laparoscopic repair of primary paraumbilical hernia. Hernia 17:505–509. https://doi.org/10.1007/s10029-013-1052-4
Henriksen NA, Montgomery A, Kaufmann R, Berrevoet F, East B, Fischer J, Hope W, Klassen D, Lorenz R, Renard Y, Garcia Urena MA, Simons MP (2020) Guidelines for treatment of umbilical and epigastric hernias from the European hernia society and Americas hernia society. Br J Surg 107:171–190
Sandø A, Rosen MJ, Heniford BT, Bisgaard T (2020) Long-term patient-reported outcomes and quality of the evidence in ventral hernia mesh repair: a systematic review. Hernia 24:695–705. https://doi.org/10.1007/s10029-020-02154-1
Harji D, Thomas C, Antoniou SA, Chandraratan H, Griffiths B, Henniford BT, Horgan L, Köckerling F, López-Cano M, Massey L, Miserez M, Montgomery A, Muysoms F, Poulose BK, Reinpold W, Smart N (2021) A systematic review of outcome reporting in incisional hernia surgery. BJS Open. https://doi.org/10.1093/bjsopen/zrab006
Colavita PD, Belyansky I, Walters AL, Zemlyak AY, Lincourt AE, Heniford BT, Augenstein VA (2014) Umbilical hernia repair with mesh: identifying effectors of ideal outcomes. Am J Surg 208:342–349. https://doi.org/10.1016/j.amjsurg.2013.12.031
Heniford BT, Walters AL, Lincourt AE, Novitsky YW, Hope WW, Kercher KW (2008) Comparison of generic versus specific quality-of-life scales for mesh hernia repairs. J Am Coll Surg 206:638–644. https://doi.org/10.1016/j.jamcollsurg.2007.11.025
Heniford BT, Lincourt AE, Walters AL, Colavita PD, Belyansky I, Kercher KW, Sing RF, Augenstein VA (2018) Carolinas comfort scale as a measure of hernia repair quality of life. Ann Surg 267:171–176. https://doi.org/10.1097/SLA.0000000000002027
Hope WW, Lincourt AE, Newcomb WL, Schmelzer TM, Kercher KW, Heniford BT (2008) Comparing quality-of-life outcomes in symptomatic patients undergoing laparoscopic or open ventral hernia repair. J Laparoendosc Adv Surg Tech 18:567–571. https://doi.org/10.1089/lap.2007.0192
Colavita PD, Tsirline VB, Belyansky I, Walters AL, Lincourt AE, Sing RF, Heniford BT (2012) Prospective, long-term comparison of quality of life in laparoscopic versus open ventral hernia repair. Ann Surg. https://doi.org/10.1097/sla.0b013e3182734130
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Heniford has been awarded education grants and received honoraria from W.L. Gore and Allergan. Dr. Augenstein has received honoraria for speaking for Medtronic, Allergan, Intuitive, Acelity, and W.L. Gore. Dr. Ayuso is a Commissioned Officer in the United States Army. Dr. Elhage, Dr. Pflederer, Dr. Shao, Dr. Deerenberg, Mr. Ku and Dr. Colavita have no potential conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elhage, S.A., Pflederer, C.T., Ayuso, S.A. et al. Multicenter analysis of laparoscopic versus open umbilical hernia repair with mesh: outcomes and quality of life (QoL). Surg Endosc 36, 6822–6831 (2022). https://doi.org/10.1007/s00464-021-08971-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08971-4