Abstract
Background
The management of ventral incisional hernias (VIH) has undergone many iterations over the last 5 years due to evolution in surgical techniques and advancement in robotic surgery. Four general principles have emerged: mesh usage, retromuscular mesh placement, primary fascial closure, and usage of minimally invasive techniques when possible. The application of robotic retromuscular repairs in VIH allow these principles to be applied simultaneously. This qualitative review attempts to answer what robotic retromuscular repairs are described, which patients are selected for these techniques, and what are current outcomes.
Methods
Using the key words: “robotic retromuscular repair”, “robotic Rives Stoppa”, and “robotic transversus abdominis release”, a PubMed search of articles written up to December 2019 was critically reviewed.
Results
44 articles were encountered, 9 high-quality articles were analyzed for this manuscript. Level of evidence ranged from 2B to 2C. Robotic TAR patients had BMI of 33 kg/m2, defect sizes ranging from 7–14 cm wide to 12–19 cm long, longer OR times, no difference in surgical site events, and shorter length of stay (LOS). The techniques to perform robotic Rives Stoppa (RS) were heterogeneous; however, extended totally extraperitoneal (ETEP) approach is most described. Defect width for RS repairs ranged 4–7 cm and LOS was less than 1 day. Complication rates were low, there is no long-term data on hernia recurrence, and information on cost is limited.
Conclusion
In short-term follow-up, robotic retromuscular repairs show promise that VIH can be repaired with intramuscular mesh, few complications, and shorter LOS. Data on hernia recurrence, long-term complications, and rigorous cost analysis are needed to demonstrate generalizability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Over the last 5 years, hernia surgery has seen application of robotic surgery to advanced abdominal wall reconstruction. Surgeons are applying minimally invasive surgery to complex hernias that were formerly performed open. In this relatively short amount of time the early experience of surgeons with robotic retromuscular techniques has been published, but few authors have synthesized the collective knowledge of these results. This qualitative review intends to identify what patient factors are associated with robotic retromuscular ventral hernia repair, summarize early outcomes, and synthesize what information needs future investigation to demonstrate generalizability.
While surgeons generally agree on pre-operative optimization prior to hernia surgery, the specific surgical management of ventral incisional hernias remains heterogeneous [1]. Debate continues between open vs. minimally invasive techniques and optimal placement of mesh [2]. Some experts believe best practice should be dictated by rigorous evidence-based guidelines, while others feel experience, practice patterns, resources, and surgeon preference deserve more weight as the speed of surgical innovation does not always match the publication rate of high-quality literature [3, 4]. Despite these varying approaches, current evidence-based trends in management suggest four general principles have emerged in the present era to manage ventral hernias: mesh usage, retromuscular mesh placement, primary fascial closure, and minimally invasive technique. Robotic retromuscular repairs appear to be the most feasible techniques to achieve these four principles.
Evidence for current trends in management
The strongest evidence that mesh results in fewer hernia recurrences is in the randomized controlled trial by Luijendijk et al. [5]. This efficacy trial demonstrated that the incidence of recurrent hernia was reduced when mesh was used vs. primary suture repair at 36 months (24% vs. 43%, p = 0.02), and long-term follow-up maintained this statistically significant difference at 10 years post-surgery (32% vs. 63%, p = 0.02). Mesh placement technique in this trial was intraperitoneal and sewn to the fascial edge with 2 cm overlap. While there was no statistically significant difference in complications between the suture and mesh repair (8% vs. 17%, p = 0.17), granular review reveals clinically significant mesh-related complications such as skin erosion, mesh infection, and enterocutaneous fistula. The morbidity of bowel-related complications has prompted some surgeons to place mesh away from the intraperitoneal space.
Retromuscular mesh placement theoretically avoids the complications of intraperitoneal mesh. Given the heterogeneity of terminology describing mesh placement, we use the terminology described by Parker et al. for the purposes of this review [4]. Mesh in the retrorectus space is deep to the rectus muscle and superficial to the posterior rectus sheath. The lateral limits are the semilunar lines, and the superior and inferior limits are the costal margins and pubis. The Rives-Stoppa repair is the surgical technique where mesh placement is in the retrorectus space [6]. The retromuscular space is an extension of the retrorectus space laterally with the limits being the retroperitoneal fat along the psoas muscles bilaterally. This space is accessed by performing a transversus abdominis release (TAR) [7]. The strongest evidence supporting retromuscular mesh placement is a meta-analysis and systematic review by Holihan et al. [8] Mesh in the retromuscular space is associated with lower odds of hernia recurrence (OR = 0.218, 95%CI 0.06–0.47) and lower risk of surgical site infection (OR = 0.449, 95%CI 0.12–1.16). When compared to onlay, inlay, and underlay mesh placements, there is a 94.2% probability that the retromuscular space is best.
Primary fascial closure with addition of muscular component release for large defects provides tension free tissue apposition for improved tissue healing. The strongest evidence that primary fascial closure is superior comes from a recent meta-analysis showing lower hernia recurrence (OR = 0.138, 95%CI 0.08–0.23) and lower surgical site occurrence (OR = 0.569, 95%CI 0.34–0.94) [9]. Given the heterogeneity of techniques to accomplish primary fascial closure, a best technique could not be identified [10,11,12]. Of described techniques, only TAR, accomplishes a primary closure of wide defect while simultaneously maintaining retromuscular mesh placement [7]. In this technique, the surgeon incises the posterior lamella of the internal oblique medial to the semilunar line to avoid division of the neurovascular bundles supplying the rectus muscle, and mobilizes this posterior flap medially to provide primary fascial closure of the abdominal midline. TAR was exclusive to open surgical techniques, but became feasible to perform robotically in 2017 [13, 14].
Minimally invasive surgery leads to better post-operative outcomes, particularly in relation to wound morbidity, post-operative complications, and length of hospital stay [15]. This concept has been evaluated in laparoscopic ventral hernia repair, with the best evidence from Pierce et al. [16] Using a paired analysis from a multi-surgeon group, laparoscopic ventral hernia repairs resulted in fewer hernia recurrences (4.3% vs. 12.1%, p < 0.01), fewer wound complications (3.8% vs. 16.8%, p < 0.01), and shorter length of stay (2.4 days vs. 4.3 days, p < 0.01) than open surgery.
Given the proliferation of surgeons performing robotic retromuscular repairs to apply these surgical principles, the objective of this review intends address key questions surgeons have regarding these emerging surgical approaches.
Materials and methods
Using the key words “robotic retromuscular repair”, “robotic Rives Stoppa”, and “robotic transversus abdominis release”, we performed a PubMed search for all literature published prior to December 2019. 44 articles were eligible for review, 34 were excluded because they were case studies or duplicates. Ten articles were reviewed by two surgeons (DS and CRL), and 9 were considered to have high enough quality to review based on the Critical Skills Appraisal Programme (CASP) literature appraisal tool [17]. It was the authors’ original intent to perform a more rigorous systematic review and meta-analysis with strength of recommendations using the Consolidated Standards of Reporting Trials (CONSORT) guidelines; however, given the limited number of available studies for this emerging technique, a qualitative review to answer clinically relevant questions for practicing surgeons was performed instead [18]. The goal of this qualitative review is to answer the following key questions.
Key questions
-
1.
What robotic retromuscular hernia repairs are currently described in the published literature?
-
2.
What patient factors and operative details are associated with robotic transversus abdominis release and robotic Rives-Stoppa repairs?
-
3.
What are the current outcomes for robotic transversus abdominis release and robotic Rives-Stoppa repairs?
-
4.
How does robotic retromuscular repair compare to laparoscopic ventral hernia repair?
-
5.
What cost analyses of robotic retromuscular repairs exist?
Composite data from the reviewed articles answered the key questions, and a summary statement synthesizing the information was provided.
Results
Levels of evidence per the Centers of Evidence-Based Medicine criteria classified 7 retrospective cohort studies as Level 2B, and 2 case series as Level 2C.
Key question 1: what robotic retromuscular hernia repairs are currently described in the published literature?
The robotic transversus abdominis release (rTAR) was first described by Warren et al. in 2017 [13]. Per the authors’ description, a double dock technique is performed where retromuscular dissection is started on the contralateral posterior rectus sheath toward the semilunar line. Transversus abdominis release is performed and extended laterally in the pre-peritoneal space to the anterior axillary line. The robot is re-docked on the opposite side using mirror image trocars and the process is repeated. The posterior sheath is closed, uncoated mesh is placed in the pre-peritoneal space, and the anterior fascia is closed with self-fixating suture. These authors also described a subset of patients who received a robotic Rives Stoppa (rRS) repair. This technique was a single dock procedure with identical setup, mesh deployment, and fascial closure, except the retromuscular dissection was initiated at the ipsilateral rectus sheath. Selection for a rRS vs. rTAR was made at the time of operation and was based on the ability of the surgeon to obtain primary fascial closure without tension.
While the concept of rRS repair is universal, robotic methods to achieve this differ significantly in the selected literature. Two authors described a single dock technique with incising the ipsilateral posterior rectus sheath and crossing over the midline to include the defect [13, 19]. Subsequently, the contralateral rectus sheath is dissected to the contralateral semilunar line, and the anterior and posterior defects are closed. An uncoated mesh is placed in the retrorectus space, and ipsilateral posterior rectus sheath is closed [19]. Belyansky et al. achieve rRS using an extended totally extraperitoneal approach (ETEP) [20]. The ETEP rRS approach is the most published technique and appears to have the fastest adoption, with two surgical groups publishing 4 high-quality publications describing the technique and its outcomes [20,21,22,23].
ETEP rRS repairs are a modification of the technique Belyansky et al. described in 2018 and were originally performed laparoscopically [20]. After acquisition of the robotic platform, these techniques were performed with the same port placements as their laparoscopic predecessors. The concept of accessing the retrorectus space extraperitoneally was first described by Daes as a means to perform inguinal hernia repair more ergonomically [24]. Belyansky et al. applied this technique to access the retrorectus space for ventral hernia repairs. Hernias located in epigastrium are treated with ETEP access below the umbilicus, whereas hernias in the hypogastrium are treated with ETEP access above the umbilicus. Centrally located hernias are approached with lateral ETEP access at the semilunar line. In all approaches, both retrorectus spaces are connected by crossing over the pre-peritoneal fat of the falciform ligament superiorly, hernia defect medially, and linea alba inferiorly. The midline defect and posterior sheath defect are closed and uncoated mesh is placed in the retrorectus space without fixation. (Please refer to the submitted video to see an example of a rRS repair with ETEP access and lateral dock approach using the technique described by Belyansky et al.).
In the early experience of all authors, the decision to perform rTAR vs. rRS came through practice-based experience, and significant transition from a planned rRS to an unplanned rTAR occurred. The primary determinant in all cases was the surgeon’s ability to achieve primary fascial closure without tension [13, 19, 20, 22]. Belyansky et al. described the concept of an ETEP rTAR as an extension of the ETEP rRS, and found that 22% of patients required a unilateral transversus abdominis release [20]. Kudsi et al. found that 10% of patients required a unilateral transversus abdominis release to achieve primary closure of the fascia [23]. Transversus abdominis release is typically performed through a lateral dock during an attempted rRS. If there appears to be tension on the posterior sheath, the transversus abdominis of the contralateral side is released through the techniques previously described. If docking was performed in the epigastric region, a limited transversus abdominis release of only the tendinous portion of the muscle is performed bilaterally [20].
Synthesis of information: Performance robotic transversus abdominis release is most similar to its originally described open surgical procedure, and is achieved with a double docking robotic approach. Robotic Rives-Stoppa repairs are performed with at least two different robotic approaches (single dock with rectus sheath incision or extended extraperitoneal access without rectus sheath division). A modest proportion of patients (10%-22%) have a planned robotic Rives-Stoppa repair convert to robotic transversus abdominis release.
Key question 2: what patient factors and operative details are associated with robotic transversus abdominis release and robotic Rives-Stoppa repairs?
Five authors reported their early experiences with rTAR [13, 19, 25,26,27]. Among patients who received a rTAR, patient age ranged from 52–63 years old, 24–42% were male, BMI was 33–35 kg/m2, and a majority of patients were ASA class 3 (please refer to Table 1). Only defect width was reported consistently and ranged from 12–14 cm wide. Among authors reporting defect length, the average length was 19–22 cm. Mesh sizes were reported inconsistently, however, average mesh width ranged from 19–39 cm, length was 42 cm, and mesh area ranged from 435–759 cm2. Rates of primary fascial closure ranged from 98%-100%, and operative times ranged from 245–365 min. Only one author reported operative blood loss as 49 ml [25].
Two studies directly compared rTAR to open TAR (oTAR) [25, 26]. When compared to their oTAR cohorts, both authors found that rTAR patients had no statistically significant differences in age, sex, BMI, or hernia width (please refer to Table 2). Only operating room time appeared to be statistically significant, with rTAR being longer than oTAR (299–365 min vs. 211–287 min, p < 0.01). Bittner et al. had more granular data and demonstrated that there were no differences defect length, mesh area, or rate of primary fascial closure between the robotic and open surgical techniques [26]. Martin-Del-Campo et al. showed that the robotic technique had significantly less blood loss (49 vs. 149 ml, p < 0.001) [25].
Regarding rRS repairs, more heterogeneous data exist. One study reported on ipsilateral rRS, two studies reported on ETEP rRS repairs, and one study reported broadly on a mixed group robotic of retromuscular repairs (88% rRS, 12% rTAR) [14, 19, 20, 22] (please refer to Table 3). Ages ranged from 51–55 years old, BMI from 30–34 kg/m2, and male sex 38–51%. Only two studies reported ASA class, with most patients being ASA 2 or 3 [19, 22]. Defect widths ranged from 4–7 cm. Defect length, mesh width, and mesh length were not reported; however, two authors reported using a mesh area ranging from 240–526 cm2. Only one author reported on primary fascial closure, however, the rate was 98%. The OR time was consistently reported by all authors and ranged from 102–183 min.
No studies were found comparing open Rives-Stoppa repair to rRS; however, Carbonell et al. performed a multi-surgeon comparison of open retromuscular repairs and robotic retromuscular repairs with nearest neighbor propensity matching, where 12% of the patients analyzed had rTAR and 88% had rRS [14]. When compared to open repairs, robotic repairs had similar age, sex, BMI, defect width, defect length, rates of primary fascial closure, and mesh sizes. Similar to the single surgeon experiences, robotic surgeries had statistically longer operating room time (45% 240 + minutes) when compared to open surgeries (33% 60–119 min, 30% 120–179 min) [14].
Only one author performed a regression analysis to determine which patient factors are associated with converting a planned rRS repair to an unplanned rTAR. Gokcal et al. noted 10% of patients who required the addition of a unilateral transversus abdominis release despite initial attempts at RS in order to achieve primary fascial closure [22]. Multivariate regression analysis determined that the presence of an incisional hernia (OR 4.86, 95%CI 1.72–13.8, p = 0.003), off-midline hernia (OR 4.88, 95%CI 1.16–20.6, p = 0.031), and increasing defect size (OR 1.01, 95%CI 1.00–1.03, p = 0.043) were independently associated with conversion to rTAR.
Synthesis of information: rTAR patients tend to be between 50–60 years old, overweight with BMI 33–35 kg/m2, ASA class 3, and have a defect width 12–14 cm in diameter. Large meshes can be placed and primary fascial closure is almost always achieved. Operating times, in the early experience of these authors, were greater than 240 min and were longer than their open TAR procedures. rRS repair patients have similar ages, BMI, sex, and ASA class to rTAR patients. Defect widths appear to be smaller, ranging from 4–7 cm. Similar to rTAR, rRS patients can accommodate large meshes and have high rates of primary fascial closure. Operating times for rRS are generally shorter than rTAR; however, 10–22% of patients require an rTAR at the time of surgery. These patients have associated incisional hernias, off-midline hernias, and the odds of converting to unilateral rTAR increase by 1% for every 1 cm increase in hernia width.
Key question 3: what are the current outcomes for robotic transversus abdominis release and robotic Rives-Stoppa repairs?
The 5 authors reporting outcomes for rTAR consistently reported hospital length of stay (LOS) and proportion of surgical site events (SSE) [13, 19, 25,26,27] (see Table 4). Hospital LOS was short and ranged from 1–3 days. SSE, defined as wound complications that are not necessarily infected (i.e., hematoma, seroma), ranged from 3–52%. Only 3 authors described proportions of patients needing surgical site occurrence needing procedural interventions (SSOPI), such as interventional radiology guided drainage. This rate was also low and ranged from 4–6%. Only 4 authors reported non-SSE post-operative complication rates (0–19%) [13, 25, 26, 28]. Non-SSE post-operative complications were broad in scope, had low event rates when stratified by category, and it is difficult to interpret if more than one of these complications occurred in the same patient (refer to Table 4). No authors reported deaths from rTAR. Although inconsistently reported, 30-day readmission rates were low, ranging from 6–8%, and reoperation rates for complications were low as well, ranging from 0–2%. No studies reported hernia recurrences and the length of follow-up ranged from 23–180 days (see Table 4).
Two authors compared post-operative outcomes of rTAR vs. oTAR and had similar single surgeon experiences [25, 26]. There were no statistically significant differences between SSE between the robotic and open procedures, and there were very low event rates for these specific complications. For both authors, LOS was significantly shorter for rTAR when compared to oTAR (see Table 5). Post-operative complications were different for each author with Bittner et al. reporting no significant difference between rTAR vs. oTAR (19.2% vs. 30.2%, p = 0.32) and Martin-Del-Campo et al. reporting fewer complications with rTAR vs. oTAR (0% vs. 17.1%, p = 0.007) [25, 26]. Only one author offered granularity regarding the nature of post-operative complications and there appeared to be broad distribution over various organ systems. Additionally, it is difficult to discern if more than one complication occurred in the same patient [26].
Only three authors reported outcomes of rRS repairs, and all had similar results (please see Table 6). The rate of SSE was low and ranged from 2–9%, and the rate of SSOPI was similarly low ranging from 0–1%. No patients died after rRS repair. LOS was low for all studies, ranging from 0–1 day. Only one author reported observations of post-operative complications at 33%, with pain as the predominant complication (31%) [22]. Readmission rates were low ranging from 2–11%, and reoperation rate was similarly low ranging from 0 to 2%. Only one recurrent hernia was noted with 180 day follow-up [21].
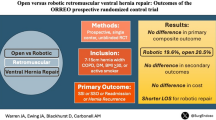
No comparative studies between rRS and open RS repairs exist; however, the propensity matched study by Carbonell et al. revealed differences in SSE and SSOPI. When compared to open surgical repair, robotic surgical repairs had fewer surgical site occurrences (14% vs. 32%, p < 0.001) and no difference in SSOPI (4% vs 5%, p = 0.8). No differences in mortality (2 vs. 0, p = 0.6), post-operative complications (2% vs. 4%, p = 0.5), readmissions (6% vs. 5%, p = 0.6), or reoperations (2% vs. 3%, p = 0.7) were noted [14]. LOS was statistically significant, and lower for robotic hernia repairs (2 vs. 3 days, p < 0.001). No recurrent hernias were reported.
Synthesis of information: The follow-up time for all published literature on robotic retromuscular repairs is less than 1 year at present, thus there is little information regarding the primary outcome of interest, recurrent ventral hernia. All studies report short-term outcomes with rTAR having LOS of 1–3 days and rRS ranging from 0–1 day. Reporting of post-operative seroma and hematoma is highly variable and can be as high as 52%; however, the proportion of surgical site events requiring intervention is very low ranging from 1–6%. Interpretation of the post-operative complication rates is difficult, but appears to have a low event rate. There are no differences in mortality, post-operative complications, readmissions, or reoperations. When compared to open surgical procedures, rTAR has shorter LOS without difference in surgical site event.
Key question 4: how does robotic retromuscular repair compare to laparoscopic ventral hernia repair?
Only one author compared outcomes of rTAR to laparoscopic ventral hernia repair with intraperitoneal only mesh (IPOM) [13]. At the time of publication, laparoscopic ventral hernia repair with IPOM was the standard of care for minimally invasive ventral hernia repair. The technique of laparoscopic IPOM employed in this study is consistent with general practice for this procedure. When compared laparoscopic IPOM, rTAR patients had the same patient demographics, defect width (6.5 cm vs 6.9 cm, p = 0.508), and defect area (82.5 cm2 vs. 88.0 cm2, p = 0.685). rTAR patients had a higher proportion of primary fascial closure (96% vs. 50.5%, p < 0.001), and utilized larger meshes (width: 18.7 vs. 16.4, p = 0.005 and area: 435 cm2 vs 339 cm2, p = 0.014). rTAR also had longer operating room times (245 min vs. 122 min, p < 0.001), but associated with shorter LOS (1 vs. 2 days, p = 0.004). Interestingly, rTAR had fewer bowel injuries (1.9% vs. 8.7%, p = 0.011) but more post-operative seromas (53% vs. 18%, p < 0.001). The rate of seromas needing procedural intervention, however, was low at 2%. There was no statistically significant difference in SSI (3.8% vs. 0.97%, p = 0.59) between rTAR and laparoscopic IPOM, and similar to other published literature at the time, no data are currently available on hernia recurrence rates.
Synthesis of information: When compared to laparoscopic IPOM in a similar patient population, robotic retromuscular repairs have longer OR time, but are able to achieve more primary fascial closure and accommodate larger mesh. Post-operatively, robotic retromuscular repairs have a shorter LOS, but a higher seroma rate, and no difference in SSI or SSOPI.
Key question 5: what cost analyses of robotic retromuscular repairs exist?
Three authors reported cost analysis from a health care systems perspective. Warren et al. compared the direct hospital cost between laparoscopic IPOM vs. robotic retromuscular repairs and found no statistically significant difference ($13,943 vs. $19,532, p = 0.07) [13]. While no itemization of cost was provided, the authors acknowledged that more complete analysis is warranted accounting for operative time, uncoated vs. coated mesh, suture vs. laparoscopic tack fixation, and shorter length of stay. Halpern et al. were unable to get their actual hospital cost data, but provided a bottom up cost estimation based on length of stay, complications, surgical site infection, readmissions, and operating room time. Based on best estimates from medical literature, rTAR provided a cost savings of $5770 per procedure when compared to oTAR [19]. Lu et al. reported statistically significant higher cost of rRS repairs vs. laparoscopic RS repairs ($6751 vs. $5091, p = 0.005); however, no itemization of cost or cost calculation was provided.
Synthesis of information: The cost analyses for robotic retromuscular repairs vs. other surgical technique are difficult to interpret. Two studies demonstrate that robotic repairs may have cost savings or no difference when compared to standard care (i.e., open or laparoscopic surgery), one study demonstrates robotic repairs are associated with a higher cost. Cost itemization was inconsistently reported, and indirect or opportunity cost savings were not accounted for. No differentiation between hospital charges and actual health care cost calculations using charge to cost ratios were provided. Patient preference was not accounted for in any cost analysis.
Conclusions
The robotic approach to retromuscular repairs is feasible in the current era and can accomplish current tenets of ventral hernia repair: mesh usage, retromuscular mesh placement, primary fascial closure, and minimally invasive surgical approach. All techniques evaluated in this review not only used mesh, but were able to accommodate large sizes relative to their associated hernia defect size. All studies of rTAR and rRS were able to achieve primary fascial closure in nearly all patients consented for the technique. Furthermore, all authors were able to maintain a planned minimally invasive approach without conversions to open surgery.
A surprising finding was the proportion of planned Rives-Stoppa repairs that required conversion to transversus abdominis release. The difference between offering transversus abdominis release vs. Rives-Stoppa repair appears to be practiced based on the surgeon’s perception of the likelihood of fascial closure. No authors offered an evidence-based defect width cut off for selecting rTAR over rRS; however, these retrospective studies are hypothesis generating. Defect size greater than 7 cm, presence of incisional hernia, and off-midline incisions serve as starting points to assess the odds that unplanned rTAR will be needed. The crossover between procedures also highlights that surgeons who adapt robotic retromuscular repairs should have expertise in performing both rRS and rTAR.
The advantage of robotic retromuscular repairs is in reduction of length of hospital stay when compared to both open and laparoscopic procedures. rTAR had a statistically significant decrease in LOS when compared to oTAR. While no formal study comparing rRS to open RS was done, a high proportion of patients in the propensity matched study by Carbonell et al. were RS repairs and a statistically significant decrease in LOS was shown (2 vs. 3 days) [14]. While one may argue that this may not be a clinically significant difference, the single surgeon series on ETEP rRS patients showed that some patients were discharged on hospital day zero, thus requiring no hospital length of stay. When compared to laparoscopic IPOM, a standard of care minimally invasive procedure, LOS was also shorter with rTAR. Hypotheses for this disparity could be explained by fewer bowel injuries experienced in the robotic arm, perhaps supporting the improved dexterity and precision provided by the robotic platform.
The disadvantage to robotic retromuscular repairs is the increase in operative time when compared to open surgical techniques and laparoscopic IPOM. Across all studies, there was a statistically significant increased operating room time when compared to existing surgical techniques. In isolation this may not seem promising; however, secular changes, such as increasing surgeon and system efficiency with robotic surgery, may demonstrate this difference is not statistically or clinically significant as experience builds with these techniques.
Post-operative complication data are difficult to interpret due to low event rates and inconsistent reporting; however, surgical site event analysis reveals that very few patients required any procedural intervention regardless of the true proportion. Seroma is the most common finding after robotic retromuscular repairs, but it is unknown if certain authors routinely screened for post-operative seroma, accounting for the wide variation in reporting. Additionally, practice changes such as prophylactic drain placement were not described to reduce this complication. With more experience, practice-based learning may have occurred and several authors may have changed their approach to managing seromas. It is also reassuring that the majority of these surgical site events did not require procedural intervention, regardless of varying detection rates.
The primary outcome of interest, recurrent ventral hernia, is largely unreported given the short follow-up of all studies evaluated. This is understandable as all studies are of early surgeon experiences with less than 1 year follow-up. Recurrent ventral hernia can occur up to two years post-operatively, and follow-up studies demonstrating the efficacy of these techniques are needed.
High-quality cost studies that correlate health care cost with clinical results are absent. Opponents of robotic surgery feel cost savings are diminished by the high direct cost of maintaining robotic systems. LOS is decreased significantly in all studies evaluated, and this important indirect cost savings was not accounted for in any cost analysis provided by the studies examined. Additionally, complication rates for robotic repairs were very low across all studies. LOS and complications are the primary drivers of health care cost, and these variables should be accounted for in studies reporting cost. No studies reported using charge to cost ratios in their calculations, and differentiation between hospital charges and actual cost were not clear. High-quality cost-effectiveness analysis studies looking at the effect of indirect cost savings from decreased LOS and cost utility analysis accounting for patient preferences will be needed to answer the question of whether robotic retromuscular repair favors cost savings from a health systems and patient perspective.
Future directions of study for robotic retromuscular repairs are clinical efficacy and clinical effectiveness studies looking at hernia recurrence rates. Traditionally, clinical efficacy is demonstrated through randomized controlled trials. Given the complexity of these procedures, few surgeons can perform robotic retromuscular repair at present. Thus, a randomized controlled trial looking at clinically efficacy would have intervention bias if participating surgeons were not equally skilled at robotic and open techniques. These retrospective studies are hypothesis generating and show that robotic retromuscular repairs are feasible to accomplish, can benefit patients, have minimal harms, and have potential cost savings. We advocate for continuing education, exposure of this technique in residency training, and post residency mentorship for surgeons to acquire skills necessary to robotic retromuscular repairs. With the development of a larger group of surgeons able to perform robotic surgery, multicenter clinical effectiveness trials could be developed to examine if robotic retromuscular repairs reduce hernia recurrence and generalize to a larger group of surgeons.
Robotic retromuscular repairs show advantage by accomplishing advanced minimally invasive abdominal wall reconstructions and decreased length of hospital stay. The event rate for complications and interventions for complications appears low; however, long-term data regarding hernia recurrence are required to evaluate efficacy. Given low harms we advocate for continuing learning of these technique for future evaluation of generalizability.
References
Liang MK, Holihan JL, Itani K et al (2017) Ventral Hernia Management: Expert Consensus Guided by Systematic Review. Ann Surg 265(1):80–89
Kockerling F, Simon T, Adolf D et al (2019) Laparoscopic IPOM versus open sublay technique for elective incisional hernia repair: a registry-based, propensity score-matched comparison of 9907 patients. Surg Endosc 33(10):3361–3369
Van Hoef S, Tollens T (2019) Primary non-complicated midline ventral hernia: is laparoscopic IPOM still a reasonable approach? Hernia : The J Hernias and Abdominal Wall Surgery 23(5):915–925
Parker SG, Halligan S, Liang MK et al (2020) International classification of abdominal wall planes (ICAP) to describe mesh insertion for ventral hernia repair. Br J Surg 107(3):209–217
Luijendijk RW, Hop WC, van den Tol MP et al (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 343(6):392–398
Stoppa RE, Rives JL, Warlaumont CR, Palot JP, Verhaeghe PJ, Delattre JF (1984) The use of Dacron in the repair of hernias of the groin. The Surgical clinics of North America 64(2):269–285
Novitsky YW, Elliott HL, Orenstein SB, Rosen MJ (2012) Transversus abdominis muscle release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg 204(5):709–716
Holihan JL, Nguyen DH, Nguyen MT, Mo J, Kao LS, Liang MK (2016) Mesh Location in Open Ventral Hernia Repair: A Systematic Review and Network Meta-analysis. World J Surg 40(1):89–99
Holihan JL, Askenasy EP, Greenberg JA, et al. (2016) Component Separation vs Bridged Repair for Large Ventral Hernias A Multi-Institutional Risk Adjusted Comparison, Systematic Review, and Meta-Analysis. Surg Infect (Larchmt)17(1): 17–26
Stoikes N, Webb D, Powell B, Voeller G (2013) Preliminary report of a sutureless onlay technique for incisional hernia repair using fibrin glue alone for mesh fixation. The American surgeon 79(11):1177–1180
Butler CE, Campbell KT (2011) Minimally invasive component separation with inlay bioprosthetic mesh (MICSIB) for complex abdominal wall reconstruction. Plast Reconstr Surg 128(3):698–709
Bueno-Lledo J, Torregrosa A, Ballester N et al (2017) Preoperative progressive pneumoperitoneum and botulinum toxin type A in patients with large incisional hernia. Hernia 21(2):233–243
Warren JA, Cobb WS, Ewing JA, Carbonell AM (2017) Standard laparoscopic versus robotic retromuscular ventral hernia repair. Surg Endosc 31(1):324–332
Carbonell AM, Warren JA, Prabhu AS et al (2018) Reducing Length of Stay Using a Robotic-assisted Approach for Retromuscular Ventral Hernia Repair: A Comparative Analysis From the Americas Hernia Society Quality Collaborative. Ann Surg 267(2):210–217
Coccolini F, Catena F, Pisano M et al (2015) Open versus laparoscopic cholecystectomy in acute cholecystitis. Systematic review and meta-analysis. Int J Surg (London, England) 18:196–204
Pierce RA, Spitler JA, Frisella MM, Matthews BD, Brunt LM (2007) Pooled data analysis of laparoscopic vs. open ventral hernia repair 14 years of patient data accrual. Surg Endosc 21(3):378–386
Zeng X, Zhang Y, Kwong JS et al (2015) The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evidence-based Med 8(1):2–10
Agha RA, Barai I, Rajmohan S et al (2017) Support for reporting guidelines in surgical journals needs improvement: A systematic review. Int J Surg (London, England) 45:14–17
Halpern DK, Howell RS, Boinpally H, Magadan-Alvarez C, Petrone P, Brathwaite CEM (2019) Ascending the Learning Curve of Robotic Abdominal Wall Reconstruction. Journal of the Society of Laparoendoscopic Surgeons 23(1):e2018–00084
Belyansky I, Reza Zahiri H, Sanford Z, Weltz AS, Park A (2018) Early operative outcomes of endoscopic (eTEP access) robotic-assisted retromuscular abdominal wall hernia repair. Hernia 22(5):837–847
Lu R, Addo A, Ewart Z, et al. Comparative review of outcomes: laparoscopic and robotic enhanced-view totally extraperitoneal (eTEP) access retrorectus repairs. Surgical endoscopy. 2019.
Gokcal F, Morrison S, Kudsi OY (2019) Robotic retromuscular ventral hernia repair and transversus abdominis release: short-term outcomes and risk factors associated with perioperative complications. Hernia 23(2):375–385
Kudsi OY, Gokcal F (2019) Lateral approach totally extraperitoneal (TEP) robotic retromuscular ventral hernia repair. Hernia. https://doi.org/10.1007/s10029-019-02082-9
Daes J (2012) The enhanced view-totally extraperitoneal technique for repair of inguinal hernia. Surg Endosc 26(4):1187–1189
Martin-Del-Campo LA, Weltz AS, Belyansky I, Novitsky YW (2018) Comparative analysis of perioperative outcomes of robotic versus open transversus abdominis release. Surg Endosc 32(2):840–845
Bittner JGT, Alrefai S, Vy M, Mabe M, Del Prado PAR, Clingempeel NL (2018) Comparative analysis of open and robotic transversus abdominis release for ventral hernia repair. Surg Endosc 32(2):727–734
Halka JT, Vasyluk A, DeMare AM, Janczyk RJ, Iacco AA (2018) Robotic and hybrid robotic transversus abdominis release may be performed with low length of stay and wound morbidity. Am J Surg 215(3):462–465
Bittner R, Bain K, Bansal VK et al (2019) Update of Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))-Part A. Surg Endosc 33(10):3069–3139
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Santos, Dr. Ledet, Ms. Limmer, and Ms. Gibson have no conflicts or interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Santos, D.A., Limmer, A.R., Gibson, H.M. et al. The current state of robotic retromuscular repairs—a qualitative review of the literature. Surg Endosc 35, 456–466 (2021). https://doi.org/10.1007/s00464-020-07957-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-020-07957-y