Abstract
Background
Laparoscopic liver resection (LLR) of posterosuperior segments (PSS) is still technically demanding procedure for highly selective patients. There is no long-term survival comparative estimation after LLR and open liver resection (OLR) for colorectal liver metastases (CRLM) located in PSS. We aimed to compare long-term overall (OS) and disease-free survival (DFS) after parenchyma-sparing LLR with expanding indications and open liver resection (OLR) of liver PSS in patients with CRLM.
Methods
Two Russian centers took part in the study. Patients with missing data, hemihepatectomy and extrahepatic tumors were excluded. One of contraindications for LLR was suspicion for tumor invasion in large hepatic vessels. Logistic regression was used for 1:1 propensity score matching (PSM).
Results
PSS were resected in 77 patients, which accounted for 42% of the total number of liver resections for CRLM. LLR were performed in 51 (66%) patients. Before and after matching, no differences were found between groups in the following factors: median size of the largest metastatic tumor; proximity to the large liver vessels; the rate of anatomical parenchyma sparing resection of PSS; a positive response to chemotherapy before and after surgery. Regardless of matching, the size of the largest metastases was above 50 mm in more than one-third of patients who received LLR. Before matching, intraoperative blood loss, ICU stay and hospital stay were significantly greater in the group of OLR. No 90-day mortality was observed within both groups. There were no differences in long-term oncological outcomes: 5-year OS after PSM was 78% and 63% after LLR and OLR, respectively; 4-year DFS after PSM was 27% in both groups.
Conclusion
Laparoscopic parenchyma-sparing resection of PSS for CRLM are justified in majority of patients who have an indication for OLR if performed in high volume specialized centers expertized in laparoscopic liver surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The laparoscopic approach is increasingly used for liver resection worldwide. According to the European consensus conference, which was held in Southampton in 2017 laparoscopic technique was recommend as a standard practice for resection of the left lateral section and was approved for the majority of minor liver resection in the anterior segments. In contrast, a technically demanding resection for lesions located in liver posterosuperior segments (PSS) remains not yet well-standardized and should be performed in only expert centers [1].
The first articles described outcomes of laparoscopic liver resection (LLR) of PSS were published only 10 years ago [2]. Since this time, a little more than two dozen articles have been published on technical issues and analysis of immediate outcomes of PSS resection. Most authors evaluated the results of PSS resection without considering the nature of the lesions. Some of the articles analyzed short-term results of PSS resection for hepatocellular carcinoma. The only so far published meta-analysis of five studies, including 237 patients undergoing LLR, regardless nature of lesions, revealed the lack of differences in immediate outcomes after OLR and LLR of PSS [3].
Oncological results are the most important to determinate the suitability of a new technique for radical treatment of malignant tumors. Despite the highest prevalence of colorectal liver metastases (CRLM) among all liver cancers in Western countries, we were able to find only two publications on survival analysis after liver PSS resection for CRLM. Both of these articles analyzed a relatively short follow-up period with the estimation of 2-year and 3-year survival.
In our study, we aimed to compare long-term overall and disease-free survival after parenchyma-sparing LLR and open liver resection (OLR) of liver PSS in patients with CRLM based on propensity score matching (PSM) analysis.
Methods
Study design: an observational cohort study. We obtained OLR and LLR data that were recorded in a prospective database and analyzed retrospectively. All OLR and LLR were performed between April 2010 and December 2018.
Two Russian centers took part in this study: Moscow Clinical Research Center named after Loginov A.S. and Russian Research Center of Radiology and Surgical Technologies named after Granov A.M. (St. Petersburg). All patients provided informed consent prior to surgery. The primary inclusion criteria were anatomical or partial parenchyma-sparing liver resection for CRLM. Patients were excluded if the following criteria were presented: missing data, hemihepatectomy or extended hemihepatectomy, extrahepatic tumors (Fig. 1). Twelve-level Marioka criteria for defining the difficulty index of LLR were used [4].
Contraindications for LLR were multiple lesions (usually, more than 7) and their distribution in several liver segments, suspected tumor invasion in hilar tubular structures or/and inferior vena cava (IVC), severe viscera-parietal adhesions and large hernias after previous abdominal surgery, and patient intolerance to prolong pneumoperitoneum due to concomitant disease. The large tumor size (more than 5 cm), the proximity of the tumor to large hepatic vessels and/or IVC and previous open liver resection were not contraindications for a minimally invasive approach.
The primary endpoint of this study was a comparison of overall and disease-free survival after parenchyma-sparing LLR and OLR of PSS. The secondary point was a comparison of immediate outcomes of LLR and OLR of PSS. Immediate outcomes included blood loss; severe morbidity (more than II grade according to Clavien-Dindo classification); mortality; time of procedures; ICU stay; hospital stay and width of the free surgical margin. Perioperative mortality was defined as death within 90 days after the procedure or before hospital discharge.
Surgical technique
OLR was performed in a standard technique with laparotomy through a reversed L-shaped incision using ribs retractors in the supine position of the patient. Segments 7 and 8 were resected after full mobilization of the right lobe with the anterior approach to the Glissonean pedicles. Caudate lobe was resected after full left lobe and Spigel lobe mobilization without left lobe transection or resection for caudate lobe approaching. LLR was performed as pure laparoscopic procedures without a hand-assistant maneuver. An anti-Trendelenburg position (30°) of the table was used in all cases. In segment 7 resection the right-side-up or left lateral decubitus position was used with trocars placed, as described by Kazaryan et al. (2011) [5]. For segments 1, 4a and 8 resections, patients were treated in the supine position. The placing of the trocars for segment 4a and 8 resections was shifted to the left with the insertion of the optical port several centimeters higher and to the left of the umbilicus. One of the surgical trocars was inserted above the optical port and below the left costal arch, the other along the midline in the middle between the umbilicus and the xiphoid process. In the case of conversion, a hybrid technique was applied through the upper midline incision 8–12 cm long. Different techniques were used for liver parenchyma division depending on the type of approach. Water-jet or ultrasound destructors in combination with bipolar forceps were applied during LLR. Open approach implied the use of various techniques: crash clamping and mentioned above devices adapted for open procedures. Although the Pringle maneuver was not applied routinely, a tourniquet was installed around the hepatoduodenal ligament in all cases.
Statistical analysis
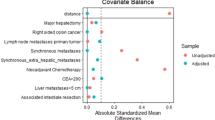
Propensity score matching was applied for balancing covariates and reducing the drawbacks of an observational study. Logistic regression was used for propensity score estimation with an 1:1 nearest-neighbor matching. Patients in groups were matched on following covariates: age; gender; American Society of Anesthesiologists score (ASA); TNM stage of the primary tumor; size of the largest metastases; multiple metastases; bilobar metastases; proximity to the large hepatic vessels; anatomical resection; response to neo-adjuvant chemotherapy; response to adjuvant chemotherapy.
Continuous data presented as median values were compared using the Mann–Whitney U test. Two-tailed Fisher's Exact Test was used for comparing categorical variables. Survival was estimated using Kaplan–Meier curves. Overall survival was calculated from the first liver resection until death by any cause. Disease-free survival was defined as the time from liver resection until relapse of the disease in any site or death of any cause. A P-value of less than 0.05 was considered statistically significant. SPSS version 23.0 (IBM SPSS, Inc., Chicago, IL) software package was applied for data analysis.
Results
One hundred eighty-five patients underwent liver resection for CRLM, including 93 LLR and 92 OLR. PSS were resected in 77 patients, which accounted for 42% of the total number of liver resections. LLR was performed in 51 patients, representing 66% of the total number of PSS resections.
Demographic data before and after matching are presented in Table 1. Preoperative data were well balanced in terms of factors affecting immediate outcomes and survival. Before and after matching, no differences were found in the median size of the largest metastatic tumor, proximity to the large liver vessels and rate of anatomical parenchyma sparing resection of PSS, as the most contributing factors for difficulty index. However, the difficulty index maintained an upward trend in the group of LLR before and after matching. A positive response to chemotherapy before and after surgery as the most important factor for survival was almost the same after matching in both groups. The median size of the largest metastatic tumor was 40 and 50 mm in the LLR group before and after PSM, respectively. The size of the largest metastases was above 50 mm in more than one-third of patients who received LLR, regardless of matching. Irrespectively to PSM, close adhesion of metastases to large hepatic vessels was registered in a quarter of patients who underwent LLR.
Immediate outcomes before and after matching are presented in Table 2. Before matching, intraoperative blood loss, ICU stay and hospital stay were significantly greater in the group of OLR. No differences were found after matching, nevertheless, there was an obvious tendency to reduce blood loss and hospital stay in the group of LLR. Conversion to hybrid technique was performed in two patients due to oncological reasons. Rate of major morbidity (> II, Clavien–Dindo) did not differ between groups before and after matching. No 90-day mortality was observed within both groups.
There were no differences in immediate and long-term oncological outcomes. The free surgical margin was almost the same after matching in both groups. In the whole series, the median time of follow-up before and after matching was 26 (6–134) and 28 (6–134) months, respectively. After PSM, the median follow-up period in groups of LLR and OLR was 26 (6–63) and 31 (7–134) months, respectively. Despite the lack of differences, the overall 5-year survival rate looked better in LLR group before PSM and appeared equal after matching (Figs. 2, 3). Disease-free 4-year survival did not differ before matching and became identical in both groups after PSM (Figs. 4, 5).
Discussion
It is well known that PSS is the most difficult part of the liver for surgical intervention, with both open and minimally invasive approach. The reason for the high difficulty of resection for lesions located in the posterosuperior region of the liver is not only poor visualization and restriction in manipulation but also the proximity of the large hepatic veins and their confluence with IVC. In this study, patients with parenchyma-sparing resection of segments 1, 4a, 7 and 8 were included. At several consensus conferences, the expert panel suggestion on PSS resection was unanimous regarding advanced expertise that is required for this highly complex type of resection, especially when performed anatomically. At a consensus conference in Louisville, laparoscopic resections of PSS were considered “major” resections from a technical point of view [6]. At the Second International Consensus Conference held in Morioka, the jury notes that parenchyma-sparing PSS resection is not minor operation and may be more complex laparoscopically than larger procedures resecting more liver parenchyma [7]. According to the latest international guidelines adopted two years ago in Southampton, the laparoscopic approach was recommended as standard practice for resection of lesions located in easy to reach segments. More complex procedures, including resection of PSS, have been suggested to be performed by experienced surgeons in selected patients in experienced and high volume centers [1]. In the previously published series of liver PSS resection, the authors drew attention to the need for patient selection. Indications limited the size of the tumor and excluded major vascular involvement [5, 8]. According to the expert’s recommendation, tumor adjacent to large hepatic vessels is not a contraindication for LLR, if performed in an expertized center [9].
Even though parenchyma-sparing resection of liver PSS remains a challenging procedure, clinical practice suggests that this type of procedure can be as safe and radical as OLR, if regularly performed in high volume specialized centers. In our practice, the rate of parenchyma-sparing liver PSS resection was 42% among all patients with CRLM. In this series, 66% of PSS resections were performed using the laparoscopic approach. Previous authors discovered diversity between LLR and OLR of PSS in the following factors, like the size of the metastatic tumors (> 30 mm); deep and multiple metastases; metastases adjacent to large vessels. All of the factors mentioned above were in favor of OLR or conversion to it [10]. Unlike these authors, we did not find any differences in preoperative tumor characteristics between LLR and OLR groups. The tumor size, large hepatic vessel proximity, rate of anatomical parenchyma-sparing resection of PSS were the same in both groups. It is well known that all of these three factors contribute to the difficulty index proposed by Japanese authors for the estimation of laparoscopic liver resection complexity [4]. Surprisingly, the difficulty index discovered the tendency to increase in the group of LLR compared to OLR.
In our series, we did not use transthoracic ports for resection of PSS segments. Liver posterior aspects appropriate visualization, which was described as the main advantage of the transthoracic approach, may be achieved through abdominal trocars by following consecutive steps of the procedure [11]. In the case of segment VIII resection, we found that the shifting of optical and working trocars position to the left provided an excellent view of the operation field and adequate dexterity of surgical manipulation. Regarding short-term outcomes, our study confirmed the suggestion on reduced blood loss and hospital stay after the LLR of PSS in comparison with open procedures [12].
The crucial issue about technically challenging laparoscopic parenchyma-sparing liver resection is oncological outcomes of this procedure. The gold standard remains OLR. At present, there are still no meta-analyses and randomized trials on long-term outcomes of PSS resection. The only prospective randomized study (Oslo-Comet Trial) included published this year subgroup analysis of immediate outcomes of PSS resection in patients with CRLM, where less blood loss and shorter hospital stay were revealed after LLR without differences in complication rate in comparison with OLR [13].
Oncological outcomes of LLR for CRLM are not inferior to those after OLR as it was confirmed on the last consensus conference in Southampton [1]. Despite the expert panel judgment on validation of LLR in selective patients with CRLM with the priority of parenchyma-sparing approach, there is still a limited number of studies investigated immediate oncological outcomes and long-term survival after LLR and OLR of PSS for CRLM. In two available articles, 2-year and 3-year disease-free survival was estimated. Two-year overall survival was evaluated at only one of these studies [9, 11].
In a multicenter study included analysis of six centers experience, outcomes of 52 OLR and 49 LLR of PSS were compared. Three-year disease-free survival was the same (36%) [11]. In the paper from MD Andersen center, the rate of LLR of PSS resection was only 11% referred to the whole number of PSS resections. Twenty-nine patients in each group were matched, including those, underwent major hepatectomy. No differences were found in short-term oncological outcomes, included 2-year disease-free and overall survival [9].
In our study, we did not find differences in 5-year overall and 4-year disease-free survival between LLR and OLR of PSS for CRLM. Non-significant improvement in overall 5-year survival in the laparoscopic group may be due to an increase in the number of patients with a positive response to neoadjuvant and adjuvant chemotherapy.
As there were no differences in the tumor characteristics, immediate outcomes and long-term survival between LLR and OLR before and after matching it may be suggested that laparoscopic approach is justified in the majority of patients whom open parenchyma-sparing PSS resection is indicated if LLR supposed to be performed by the expertized surgical team. Nevertheless, LLR of PSS should not be considered in patients with tumor invasion in large hepatic vessels and/or IVC.
The drawbacks of our study were its retrospective design and the limited number of patients included.
Conclusion
In our series of laparoscopic PSS resection for CRLM, expanding indications to laparoscopic approach has increased its rate to more than 50% of the whole number of PSS resections without the difference in immediate outcomes and long-term survival between LLR and OLR. In selected patients, laparoscopic parenchyma-sparing resection of PSS for CRLM is justified on the base of immediate and long-term oncological outcomes comparative estimation. Parenchyma-sparing resection of PSS for CRLM may be recommended as routine practice in high volume specialized centers expertized in laparoscopic liver surgery.
References
Abu Hilal M, Aldrighetti L, Dagher I, Edwin B, Troisi RI, Alikhanov R, Aroori S, Belli G, Besselink M, Briceno J, Gayet B, D'Hondt M, Lesurtel M, Menon K, Lodge P, Rotellar F, Santoyo J, Scatton O, Soubrane O, Sutcliffe R, Van Dam R, White S, Halls MC, Cipriani F, Van der Poel M, Ciria R, Barkhatov L, Gomez-Luque Y, Ocana-Garcia S, Cook A, Buell J, Clavien PA, Dervenis C, Fusai G, Geller D, Lang H, Primrose J, Taylor M, Van Gulik T, Wakabayashi G, Asbun H, Cherqui D (2018) The Southampton consensus guidelines for laparoscopic liver surgery. From indication to implementation. Ann Surg 268(1):11–18. https://doi.org/10.1097/SLA.0000000000002524
Cho JY, Han HS, Yoon YS, Shin SH (2008) Feasibility of laparoscopic liver resection for tumors located in the posterosuperior segments of the liver, with a special reference to overcoming current limitations on tumor location. Surgery 144:32–38. https://doi.org/10.1016/j.surg.2008.03.020
Machairas N, Prodromidou A, Kostakis ID, Spartalis E, Sotiropoulos GC (2018) Safety and efficacy of laparoscopic liver resection for lesions located on posterosuperiorsegments: a meta-analysis of short-term outcomes. Surg Laparosc Endosc Percutan Tech 28(4):203–208. https://doi.org/10.1097/SLE.0000000000000562
Wakabayashi G (2016) What has changed after the Morioka consensus conference 2014 on laparoscopic liver resection? Hepatobiliary Surg Nutr 5(4):281–289. https://doi.org/10.21037/hbsn.2016.03.03
Kazaryan AM, Røsok BI, Marangos IP, Rosseland AR, Edwin B (2011) Comparative evaluation of laparoscopic liver resection for posterosuperior and anterolateral segments. Surg Endosc 25:3881–3889. https://doi.org/10.1007/s00464-011-1815-x
Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, Koffron AJ, Thomas M, Gayet B, Han HS, Wakabayashi G, Belli G, Kaneko H, Ker CG, Scatton O, Laurent A, Abdalla EK, Chaudhury P, Dutson E, Gamblin C, D'Angelica M, Nagorney D, Testa G, Labow D, Manas D, Poon RT, Nelson H, Martin R, Clary B, Pinson WC, Martinie J, Vauthey JN, Goldstein R, Roayaie S, Barlet D, Espat J, Abecassis M, Rees M, Fong Y, McMasters KM, Broelsch C, Busuttil R, Belghiti J, Strasberg S, Chari RS, World Consensus Conference on Laparoscopic Surgery (2008) The international position on laparoscopic liver surgery: the Louisville statement. Ann Surg 250(5):825–830
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, Asbun H, O’Rourke N, Tanabe M, Koffron AJ, Tsung A, Soubrane O, Machado MA, Gayet B, Troisi RI, Pessaux P, Van Dam RM, Scatton O, Abu Hilal M, Belli G, Kwon CH, Edwin B, Choi GH, Aldrighetti LA, Cai X, Cleary S, Chen KH, Schön MR, Sugioka A, Tang CN, Herman P, Pekolj J, Chen XP, Dagher I, Jarnagin W, Yamamoto M, Strong R, Jagannath P, Lo CM, Clavien PA, Kokudo N, Barkun J (2015) Strasberg SM (2015) Recommendations for laparoscopic liver resection A report from the second international consensus conference held in Morioka. Ann Surg 261(4):619–629. https://doi.org/10.1097/SLA.0000000000001184
Coles SR, Besselink MG, Serin KR, Alsaati H, Di Gioia P, Samim M, Pearce NW, Abu Hilal M (2015) Total laparoscopic management of lesions involving liver segment 7. Surg Endosc 29:3190–3195. https://doi.org/10.1007/s00464-014-4052-2
Abu Hilal M, van der Poel MJ, Samim M, Besselink MG, Flowers D, Stedman B et al (2015) Laparoscopic liver resection for lesions adjusted to major vasculature: feasibility, safety and oncological efficiency. J Gastrointest Surg 19:692–698. https://doi.org/10.1007/s11605-014-2739-2
Okuno M, Goumard C, Mizuno T, Omichi K, Tzeng CD, Chun YS, Aloia TA, Fleming JB, Lee JE, Vauthey JN, Conrad C (2018) Operative and short-term oncologic outcomes of laparoscopic versus open liver resection for colorectal liver metastases located in the posterosuperior liver: a propensity score matching analysis. Surg Endosc 32(4):1776–1786. https://doi.org/10.1007/s00464-017-5861-x
Lee W, Han HS, Yoon YS, Cho JY, Choi Y, Shin HK (2014) Role of intercostal trocars on laparoscopic liver resection for tumors in segments 7 and 8. J Hepatobiliary Pancreat Sci 21(8):E65–E68. https://doi.org/10.1002/jhbp
Scuderi V, Barkhatov L, Montalti R, Ratti F, Cipriani F, Pardo F, Tranchart H, Dagher I, Rotellar F, Abu Hilal M, Edwin B, Vivarelli M, Aldrighetti L, Troisi RI (2017) Outcome after laparoscopic and open resections of posterosuperior segments of the liver. Br J Surg 104(6):751–759. https://doi.org/10.1002/bjs.10489
Aghayan DL, Fretland ÅA, Kazaryan AM, Sahakyan MA, Dagenborg VJ, Bjørnbeth BA, Flatmark K, Kristiansen R, Edwin B (2019) Laparoscopic versus open liver resection in the posterosuperior segments: a sub-group analysis from the OSLO-COMET randomized controlled trial. HPB (Oxford). https://doi.org/10.1016/j.hpb.2019.03.358
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Drs. Efanov M, Granov D, Alikhanov R, Rutkin I, Cvirkun V, Kazakov I, Vankovich A, Beketov M, Koroleva A and Kovalenko D have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Efanov, M., Granov, D., Alikhanov, R. et al. Expanding indications for laparoscopic parenchyma-sparing resection of posterosuperior liver segments in patients with colorectal metastases: comparison with open hepatectomy for immediate and long-term outcomes. Surg Endosc 35, 96–103 (2021). https://doi.org/10.1007/s00464-019-07363-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07363-z