Abstract
Background
One-lung ventilation (OLV) is the standard and widely applied ventilation approach used in video-assisted thoracoscopic surgery for esophageal cancer (VATS-e). To address the disadvantages of OLV with respect to difficulties in intubation and induction, as well as the risk of respiratory complications, two-lung ventilation (TLV) with artificial pneumothorax has been introduced for use in VATS-e. However, no studies have yet compared TLV and OLV with postoperative infection and inflammation in the prone position over time postoperatively. Here, we investigated the efficacy of TLV in patients undergoing VATS-e in the prone position.
Methods
Between April 2010 and December 2016, 119 patients underwent VATS-e under OLV or TLV with carbon dioxide insufflation. Clinical characteristics, surgical outcomes, and postoperative outcomes, including oxygenation and systemic inflammatory responses, were compared between patients who underwent OLV and those who underwent TLV.
Results
Clinical characteristics other than pT stage were comparable between groups. The TLV group had shorter thoracic operation time than the OLV group. No patients underwent conversion to open thoracotomy. The PaO2/FiO2 ratios of the TLV group on postoperative day (POD) 5 and on POD7 were significantly higher than those of the OLV group. C-reactive protein levels on POD7 were lower in the TLV group than in the OLV group. There were no significant differences with respect to postoperative complications between the OLV and TLV groups. In the TLV group, the white blood cell count on POD7 was significantly lower than that in the OLV group; body temperature showed a similar trend immediately after surgery and on POD1.
Conclusions
In this study, we demonstrated that, compared with OLV, TLV in the prone position provides better oxygenation and reduced inflammation in the postoperative course. Accordingly, TLV might be more useful than OLV for ventilation during esophageal cancer surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Esophageal cancer is the sixth most common cause of cancer-related mortality worldwide [1]. Esophagectomy is the primary therapeutic approach for patients diagnosed with curable esophageal cancer. However, esophagectomy is a complex procedure that requires manipulation in the chest and abdomen, as well as the neck in many cases; these procedures can be associated with significant morbidity and mortality [2]. Video-assisted thoracoscopic surgery for esophageal cancer (VATS-e) was originally introduced by Cuschieri in 1993 [3]. Importantly, VATS-e reduces the incidence of postoperative systemic inflammatory response syndrome (SIRS) and related pulmonary complications [4, 5]. VATS-e is a feasible and safe surgical approach for reliable minimally invasive esophagectomy associated with reduced perioperative complications [6]. One-lung ventilation (OLV) is the standard ventilation in both conventional open thoracotomy and VATS-e; it can provide adequate surgical space in the right thoracic cavity by collapsing the right lung [7]. However, OLV exhibits several disadvantages, including difficulty in anesthetic induction/intubation and maintenance, as well as a risk of respiratory complications [8]. Such problems in patients undergoing OLV often result from inappropriate anesthetic management, which may affect postoperative respiratory function due to poor lung expansion, CO2 retention, or lung hyperinflation [9].
Palanivelu et al. introduced two-lung ventilation (TLV) with CO2 artificial pneumothorax for use during VATS-e in 2006 [10]. This approach yields better perioperative outcomes, including improvement of intraoperative respiratory function, easier introduction of the endotracheal tube, and management of anesthesia [11,12,13]. However, no studies have yet compared TLV and OLV with postoperative infection and inflammation in patients undergoing VATS-e in the prone position over time postoperatively except one that only observed the inflammatory responses [14]. Here, we retrospectively examined the efficacy of TLV with artificial pneumothorax in patients undergoing VATS-e.
Materials and methods
Patients and surgical procedure
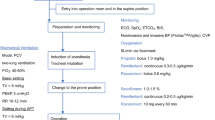
A total of 119 consecutive patients who underwent VATS-e for esophageal cancer with R0 resection in our institute, during the period from April 2010 to December 2016, were included in this study. OLV was used until April 2014 (71 patients), and TLV was then introduced (48 patients). In the OLV group, patients were intubated using a double-lumen endotracheal tube (Broncho Cath, Covidien, Tokyo, Japan). In the TLV group, patients were intubated with a single-lumen endotracheal tube in the conventional manner. All inductions and intubations were performed by experienced anesthesiologists.
Intraoperative posture was well supported and fixed in a semi-prone position with the right arm abducted above the head; the table was rotated to the right, and the patient was arranged in a prone position. VATS-e was performed by two surgeons—a surgical operator and an endoscopist—both standing on the left side of the operating table; the video monitor was placed on the opposite side of the operating table. Two working ports were inserted at the fifth and seventh intercostal spaces on the posterior axillary retrograde line; the camera port was inserted at the ninth intercostal space on the posterior axillary line. CO2 insufflation (CO2 pressure = 6 mmHg) was used to create an artificial pneumothorax. Two- or three-field lymphadenectomy was performed as necessary. Gastric conduit reconstruction was achieved by laparoscopic procedure. The gastric conduit was pulled through the posterior mediastinum to the neck. Anastomosis was manually performed in the cervical position. Then, a jejunostomy catheter was placed in all patients for postoperative enteral nutrition.
Postoperative care, including respiratory, chest drain management, and nutritional care, was performed in the same manner during the observation period. Thoracic epidural analgesia was applied to all patients. The blood samples were collected preoperatively, immediately after surgery, postoperative day (POD) 1, 3, 5, and 7. Whenever an arterial line was inserted, blood was collected from the arterial line. PaO2 / FiO2 ratio were calculated by the results of arterial blood gas. The pathologic stage of disease was determined in accordance with the Tumor–Node–Metastasis (TNM) Classification of Malignant Tumors by the International Union Against Cancer (7th edition) [15]. Data regarding preoperative status, surgical procedures, and postoperative clinical and laboratory values were collected from medical records and nursing charts. In-hospital mortality was defined as death that occurred during an in-hospital stay.
Informed consent was obtained from all participants prior to entry into the study. This study was approved by the Ethics Committee of National Defense Medical College Hospital.
Statistical analysis
JMP Pro software (version 14.2.0, SAS Institute, Inc., Cary, NC, USA) was used for statistical analysis. Numerical data are presented as the mean ± standard deviation. Intergroup comparisons were performed using the Wilcoxon rank-sum test. Categorical data are presented as number or percentage (%). Intergroup comparisons were performed using the Chi-squared test. Differences with P values < 0.05 were considered to be statistically significant. A quadratic regression method with least-squares estimates was applied to model the learning curve.
Results
Attenuation of the learning curve effect for a particular operator was observed with OLV, but not with TLV (Fig. 1). All VATS-e procedures were successfully performed, and there were no incidences of conversion to open thoracotomy due to intraoperative complications (e.g., endotracheal and lung injuries or vascular injuries). A short intraoperative video segment is attached in the Supplementary Material (video). The clinical characteristics of the two groups are summarized in Table 1. The pT stage was significantly higher in the TLV group than in the OLV group (P = 0.038) However, there were no significant differences in clinical characteristics between the two groups, including age, sex, pulmonary function, renal function, neoadjuvant therapy, tumor location, TNM staging (except pT stage), field of lymphadenectomy, or abdominal procedure. The surgical variables are summarized in Table 2. The TLV group had significantly shorter thoracic time. However, there were no significant differences in preoperative time from the start of anesthesia until the incision, total operative time, intraoperative blood loss, intraoperative blood transfusion, or total number of dissected lymph nodes (LNs) between the two groups.
Perioperative changes in PaO2/FiO2 ratio and CRP
The TLV group exhibited a significant increase in the PaO2/FiO2 ratio on postoperative day (POD) 5 and on POD7 (Fig. 2). C-reactive protein (CRP) levels were significantly lower on POD7 in the TLV group than in the OLV group (Fig. 3).
Perioperative changes in SIRS criteria
We also assessed the postoperative time course of changes for each factor of the SIRS criteria. White blood cell count on POD7 and body temperature from immediately after the operation until POD1 in the TLV group were significantly lower than those in the OLV group (P < 0.05) (Fig. 4). No differences were observed in heart rate or respiratory rate between the two groups.
Comparison of postoperative outcomes between OLV and TLV procedures
Postoperative outcomes are summarized in Table 3. There were no significant differences in the incidences of postoperative complications, 30-day mortality rates, or in-hospital stays between the two groups.
Discussion
In this study, we demonstrated several advantages of TLV over OLV with respect to thoracic operation time, postoperative oxygenation, and systemic inflammation. In addition, there was no significant difference in intraoperative blood loss, intraoperative blood transfusion, harvested lymph nodes, and postoperative outcomes between the two groups.
Saikawa et al. previously reported that TLV was more effective than OLV for the maintenance of stable hemodynamics and oxygenation during the perioperative period, in a study of 14 patients who underwent VATS-e [16]. In that study, although the left mediastinal pleurae were damaged by the thoracoscopic procedure and bilateral pneumothorax that occurred, there were no increases in airway pressure or instances of apparent circulatory depression. In contrast, some reports have shown that, although the use of TLV resulted in shorter thoracic operation time relative to the use of OLV, no differences were observed in pulmonary complications between the two groups [12, 13]. To the best of our knowledge, there have been no reports regarding the time courses of postoperative oxygenation or inflammation. Although our results also indicated that there were no differences in pulmonary complications, we found that the PaO2/FiO2 ratio was significantly higher in the TLV group on POD5 and POD7 and that the CRP level was significantly lower on POD7 in the TLV group. The white blood cell count on POD7 and body temperature from immediately after the operation until POD1 were both significantly lower in the TLV group.
Prior studies reported that surgical variables of TLV, such as operative time and hospital stay, were superior to those of OLV in patients who underwent VATS-e by experienced surgeons [12, 13]. Our results also showed that the TLV group had significantly shorter thoracic operation time than the OLV group. These results suggest that, to secure space in the right thoracic cavity, CO2 artificial pneumothorax in TLV can provide a superior surgical view, compared with collapse of the right lung in OLV. A hard, large-caliber, double-lumen endotracheal tube placed in the main bronchus limits endotracheal mobility during surgery, making it difficult to remove LNs along the recurrent laryngeal nerve in OLV. In addition, TLV did not require the positioning of double-lumen tube and inflation or deflation of the balloon by anesthesiologist. These may contribute to the superiority of TLV over OLV with respect to the operation time during the thoracic procedure.
There were two limitations in this study. First, this was a single-center, retrospective study; the study design thus might have led to selection bias. Second, the patients in the OLV group had more advanced pT stages than patients in the TLV group; this may have influenced the results with respect to mobilization of the esophagus.
In conclusion, the current study demonstrated that TLV with artificial pneumothorax can be beneficial for postoperative oxygenation and systemic inflammation in patients undergoing VATS-e. Thus, TLV might be more useful than OLV for ventilation during VATS-e in the prone position.
References
Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin D, Forman D (2013) Bray F (2015) GLOBOCAN 2012 v1.0, cancer incidence and mortality worldwide: IARC CancerBase no. 11. International Agency for Research on Cancer, Lyon
Durkin C, Schisler T, Lohser J (2017) Current trends in anesthesia for esophagectomy. Curr Opin Anaesthesiol 30:30–35
Cuschieri A (1993) Endoscopic subtotal oesophagectomy for cancer using the right thoracoscopic approach. Surg Oncol 2(Suppl 1):3–11
Nomura S, Tsujimoto H, Aosasa S, Saitoh D, Hase K, Ono S, Yamamoto J, Ueno H (2018) Impact of angiotensin-converting enzyme 2 levels on postoperative pneumonia after esophagectomy. J Surg Res 224:200–206
Tsujimoto H, Takahata R, Nomura S, Yaguchi Y, Kumano I, Matsumoto Y, Yoshida K, Horiguchi H, Hiraki S, Ono S, Yamamoto J, Hase K (2012) Video-assisted thoracoscopic surgery for esophageal cancer attenuates postoperative systemic responses and pulmonary complications. Surgery 151:667–673
Luketich JD, Pennathur A, Franchetti Y, Catalano PJ, Swanson S, Sugarbaker DJ, De Hoyos A, Maddaus MA, Nguyen NT, Benson AB, Fernando HC (2015) Minimally invasive esophagectomy: results of a prospective phase II multicenter trial-the eastern cooperative oncology group (E2202) study. Ann Surg 261:702–707
Liu Z, Liu X, Huang Y, Zhao J (2016) Intraoperative mechanical ventilation strategies in patients undergoing one-lung ventilation: a meta-analysis. SpringerPlus 5:1251
Blank RS, Colquhoun DA, Durieux ME, Kozower BD, McMurry TL, Bender SP, Naik BI (2016) Management of one-lung ventilation: impact of tidal volume on complications after thoracic surgery. Anesthesiology 124:1286–1295
Lohser J, Slinger P (2015) Lung injury after one-lung ventilation: a review of the pathophysiologic mechanisms affecting the ventilated and the collapsed lung. Anesth Analg 121:302–318
Palanivelu C, Prakash A, Senthilkumar R, Senthilnathan P, Parthasarathi R, Rajan PS, Venkatachlam S (2006) Minimally invasive esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position—experience of 130 patients. J Am Coll Surg 203:7–16
Zhang R, Liu S, Sun H, Liu X, Wang Z, Qin J, Hua X, Li Y (2014) The application of single-lumen endotracheal tube anaesthesia with artificial pneumothorax in thoracolaparoscopic oesophagectomy. Interact Cardiovasc Thorac Surg 19:308–310
Cai L, Li Y, Sun L, Yang XW, Wang WB, Feng F, Xu GH, Guo M, Lian X, Zhang HW (2017) Better perioperative outcomes in thoracoscopic-esophagectomy with two-lung ventilation in semi-prone position. J Thorac Dis 9:117–122
Lin M, Shen Y, Wang H, Fang Y, Qian C, Xu S, Ge D, Feng M, Tan L, Wang Q (2018) A comparison between two lung ventilation with CO2 artificial pneumothorax and one lung ventilation during thoracic phase of minimally invasive esophagectomy. J Thorac Dis 10:1912–1918
Zhang BJ, Tian HT, Li HO, Meng J (2018) The effects of one-lung ventilation mode on lung function in elderly patients undergoing esophageal cancer surgery. Medicine 97:e9500
Sobin LH, Gospodarowicz MK, Wittekind C (2011) TNM classification of malignant tumours. Wiley, New York
Saikawa D, Okushiba S, Kawata M, Okubo T, Kitashiro S, Kawarada Y, Suzuki Y, Kato H (2014) Efficacy and safety of artificial pneumothorax under two-lung ventilation in thoracoscopic esophagectomy for esophageal cancer in the prone position. Gen Thorac Cardiovasc Surg 62:163–170
Acknowledgements
The authors would like to thank Enago (www.enago.com) for the English language review.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
SN and HT conceived the idea of this research, designed the protocol, and supervised the analysis of the results. YI, SF, KK, MH, NI, YY, SH, DS, TI, KH, and YK developed and supervised all work and analyzed the results. HU supervised the study.
Corresponding author
Ethics declarations
Disclosures
All authors (Shinsuke Nomura, Hironori Tsujimoto, Yusuke Ishibashi, Seiichiro Fujishima, Keita Kouzu, Manabu Harada, Nozomi Ito, Yoshihisa Yaguchi, Daizoh Saitoh, Takehiko Ikeda, Kazuo Hase, Yoji Kishi, Hideki Ueno) report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nomura, S., Tsujimoto, H., Ishibashi, Y. et al. Efficacy of artificial pneumothorax under two-lung ventilation in video-assisted thoracoscopic surgery for esophageal cancer. Surg Endosc 34, 5501–5507 (2020). https://doi.org/10.1007/s00464-019-07347-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07347-z