Abstract
Background
Three-dimensional (3D) printing is a disruptive technology that is quickly spreading to many fields, including healthcare. In this context, it allows the creation of graspable, patient-specific, anatomical models generated from medical images. The ability to hold and show a physical object speeds up and facilitates the understanding of anatomical details, eases patient counseling and contributes to the education and training of students and residents. Several medical specialties are currently exploring the potential of this technology, including general surgery.
Methods
In this review, we provide an overview on the available 3D printing technologies, together with a systematic analysis of the medical literature dedicated to its application for abdominal surgery. Our experience with the first clinical laboratory for 3D printing in Italy is also reported.
Results
There was a tenfold increase in the number of publications per year over the last decade. About 70% of these papers focused on kidney and liver models, produced primarily for pre-interventional planning, as well as for educational and training purposes. The most used printing technologies are material jetting and material extrusion. Seventy-three percent of publications reported on fewer than ten clinical cases.
Conclusion
The increasing application of 3D printing in abdominal surgery reflects the dawn of a new technology, although it is still in its infancy. The potential benefit of this technology is clear, however, and it may soon lead to the development of new hospital facilities to improve surgical training, research, and patient care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Over time, novel technologies and the introduction of diagnostic imaging have re-shaped the practice of surgery. Today, modern multi-detector computed tomography (MDCT) and magnetic resonance imaging (MRI) systems, in combination with the advances in image processing, allow the generation of detailed 3D virtual models of a patient’s anatomy, to support the diagnosis and the planning process of complex interventional management. However, the use of 3D reconstructions is often limited by the lack of a computer platform with access to the patient’s data and the absence of dedicated software for image processing and display. That can be impractical for many aspects of its potential use: pre-treatment interventional planning, patient counseling, teaching to students and residents and intraoperative guidance. But with the right tools in place, 3D printing can enable the transition from the virtual world to the real one, providing the tactile feedback of an anatomical model and ensuring its ready availability in any desired setting, including the patient’s bedside. Although originally introduced 30 years ago for industrial production as a tool for rapid prototyping, today 3D printing is gaining popularity in many fields, including healthcare, thanks to its ability to reproduce complex geometries, such as that typical of solid organs and major blood vessels. The increasing adoption of 3D printing in a wide range of medical and surgical specialties mirrors the rapid spread of this technology in the global market. Moreover, the creation of a single copy of a patient-specific anatomical model is in keeping with the growing personalization of treatment, one of the keys of modern precision medicine.
The underlying technology of every 3D printer is based on the same general concept: the selected object is manufactured through a layer-by-layer process. Initially, the virtual model is divided into thin layers of equal width. Then, each layer is sent to the 3D printer, which deploys its material in the specified sequence. The various printers available on the market differ in the way layers are deposited and cured, according to the type of material employed.
The American Society for Testing and Materials International (ASTM International), an organization that develops and publishes consensus technical standards for a vast array of products and materials, recognizes seven main categories of 3D printers [1], classified by their materials and curing systems:
Vat photopolymerization this process involves the use of a photopolymer resin, hardened by means of a light source. The most common technology is stereolithography (SLA), which uses an ultraviolet (UV) laser to cure the resin layer by layer.
Material jetting this approach resembles that of an inkjet paper printer, where the printing material is dropped through small-diameter nozzles. Base materials are photopolymer resins, hardened by a UV lamp. One of the main advantages of this printing process is the ability to combine several materials, with different colors and varying degrees of transparency and deformability, while maintaining high resolution and performance.
Binder jetting this technique involves the use of two base materials, a chalk powder and a liquid binder. The powder is distributed in uniform layers and the binder is applied through small nozzles to glue together powder particles according to the 3D virtual model. Furthermore, it enables the printing of full-color scale models, thanks to the use of color inkjet cartridges.
Material extrusion this is the most popular and cheapest 3D printing technology available on the market. These printers work using thermoplastic filaments, which are pushed through a heating chamber and extruded through a small nozzle; the melted material is deployed layer by layer, following a path designated by the 3D virtual model. The most common material extrusion technology is fused deposition modeling (FDM—a term trademarked by Stratasys®) or fused filament fabrication (FFF—the open source equivalent term).
Powder bed fusion (best known as Selective Laser Sintering) this technology involves the use of a powerful laser source capable of melting plastic, metal or ceramic powder particles into the desired 3D object. The laser selectively fuses the powdered material by scanning the cross-sections on the surface of the powder bed.
Sheet lamination with this technique, sheets of material are bonded together through external forces; different mechanisms can be employed to achieve interlayer bonding, such as adhesive bonding (e.g., a sheet of paper), thermal bonding, clamping or ultrasonic welding (e.g., sheet metal).
Direct energy deposition (DED) here, 3D-printed components are created by melting a metal powder directly during its deposition. In this process, typically applied in the high-tech metal industry, metal powders or filaments are melted by an energy source (electron beam, laser or plasma arc) and deployed with a great degree of freedom, thanks to machines with up to five axes of movement.
Three-dimensional printing for abdominal surgery is usually related to the creation of physical replicas of a patient-specific anatomical model, but its use can also be extended to the production of surgical instruments or implantable devices. Regardless to the specific medical specialty, a 3D-printed anatomical model can be generated for one or more of the following purposes:
Surgical planning to facilitate the planning of a given procedure by showing the anatomical details of the surgery site and anticipating technical problems; to select the most suitable surgical device (e.g., prosthesis, etc.) among those available; and to define the management strategy, including the best access to the anatomical target.
Education and training to facilitate the comprehension of a surgical procedure on the part of residents and junior surgeons.
Simulation thanks to the use of deformable materials that enable dissection, suturing and performance of anastomosis on patient-specific platforms.
Anatomical comprehension for a better understanding of fine anatomical details which may influence the management of the underlying disease (not just for surgery).
Patient counseling to enhance the patient’s understanding of the planned intervention and his/her awareness of the expected outcomes and associated risks.
Surgical tools for the development of ad hoc 3D-printed tools for experimental research in surgical techniques and technologies.
In this paper, we present a systematic literature review on the use of 3D printing for abdominal surgery to provide up-to-date information on the current state of the application of this technology. All the advantages linked to the availability of a physical object have been extensively reported in other fields such as orthopedic surgery or maxillofacial surgery, while the diffusion in abdominal surgery is still limited. This is mainly due to the higher complexity in medical image processing of soft abdominal tissues, with respect to bones or vessels with medium contrast injection, making more difficult to create the virtual model to be 3D printed. In this context, an overview of state of art applications in abdominal surgery will possibly boost the spread of 3D printing also in this field.
We will also join the discussion by providing information on our 5-year experience with 3D printing for medical applications at a general hospital.
Materials and methods
Search criteria
Three databases were used for the query: PubMed, Web of Science, and Embase. The search strings were first run on PubMed and then adapted to the other databases, according to the specific formulation constraints of each. A filter for the language was applied, limiting the search to documents in English. No filter on the publication year and no filter on the type of publication were applied, thus including conference proceedings, editorial material, meeting abstracts, technical notes, posters, etc. The query was applied to both the title and the abstract. Search strings were made up of three groups of keywords combined through the AND operator. Keywords of each group define, respectively (i) the technology of interest, i.e. 3D printing, (ii) the aim of its use (planning, preparation, evaluation, training or education) and (iii) the anatomical region of application (the abdominal cavity), also specifying the main structures of interest, i.e. the liver, pancreas, kidney, spleen, and biliary ducts. Keywords coming from the database dictionary (e.g., “Mesh” terms for PubMed and “Emtree” words for Embase) were included when available, along with their corresponding free term, since they involve two different search engines (e.g., “Printing, Three-Dimensional” [Mesh] and “Three-Dimensional Printing”). With respect to the anatomical regions, we also included partial terms (e.g., biliar*, pancrea*) to overcome nomenclatural limitations.
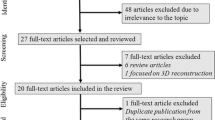
Data analysis criteria
The output of the selected search queries was processed using RefWorks software [2], to eliminate duplicates. Afterwards, papers were analyzed according to the exclusion criteria listed in Table 1. The screening was first run relying only on the publications’ title and abstract, then on a full text basis.
The resulting publications were then analyzed to retrieve the information pertaining to the specific use of the 3D printing technology. In particular, data were collected on: the 3D printing category and the specific machine and materials described in the report, the type of application of the 3D printed model (surgical planning, education and training, simulation, anatomical comprehension or patient counseling) and the target anatomical district. The number of clinical cases reported in each publication was also recorded. For the nature of the present work, no Institutional Review Board approval or written consent is required.
Results
Search queries produced a total of 296 records on the three databases (Fig. 1) as of December 19th, 2018. After duplicate removal, 184 papers were analyzed according to the selected exclusion criteria, leading to a final pool of 97 publications.
A pattern of progressive increases in the number of publications on 3D printing for abdominal surgery is clearly visible over the last 10 years (Fig. 2), even if with lower numbers with respect to the diffusion in other surgical specialties. The trend follows a similar spread of 3D printing technology on the global market. The first publication appeared in 2008 [3]. Thirty-five publications are in the form of abstracts, conference proceedings, supplements or posters. Seventeen publications belong to only a few research groups (Sugimoto et al. [4,5,6,7,8,9,10,11], Chandak et al. [12,13,14], Fang [15,16,17], and Marconi et al. [18,19,20]).
Technology
Three-dimensional printing technology can be used either for the direct realization of the final model or for the production of a mold, to cast the desired material. The latter application, also called “indirect 3D printing,” combines the advantages of geometrical freedom brought by standard 3D printing with the use of highly deformable materials unsuitable for direct printing or complex to handle (typically silicone, latex or polyurethane). Seventy-nine of the analyzed publications reported a direct 3D printing approach, with only 11 describing an indirect approach [21,22,23,24,25,26,27,28,29,30,31], while in seven papers both approaches were used to generate the final model [3, 32,33,34,35,36,37].
Thirty-six articles reporting on direct 3D printing described using material jetting technology, considered to be the most reliable in generating anatomical models of abdominal organs, thanks to its accurate control of the mechanical properties [6, 10,11,12,13,14, 18, 19, 29, 34, 35, 38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62]. In only three cases was this technology adopted for indirect printing, through the creation of a mold in which a silicone mixture was poured [29, 34, 35].
Twenty-two publications reported using material extrusion [22, 23, 25, 27, 30, 31, 33, 37, 49, 63,64,65,66,67,68,69,70,71,72,73,74,75]. This technology is characterized by a lower degree of accuracy and resolution and less control over material properties as compared to material jetting. However, the materials employed are much cheaper (e.g., acrylonitrile butadiene styrene or polylactic acid thermoplastic filaments). That is why this technology is the most popular for indirect 3D printing applications, to create the mold which is subsequently destroyed to retrieve the casted model [22, 23, 25, 27, 30, 31, 33, 37].
Ten publications described employing binder jetting technology [3, 20, 24, 32, 35, 76,77,78,79,80], which produces a high-chromatic resolution and is less expensive than material jetting. However, the resulting printed objects are extremely fragile, unsuitable for the production of finer parts, like small blood vessels. On the other hand, this technology is useful for molding applications [35]. Less frequently used technologies are powder bed fusion—with the use of polyamide powders [38, 44, 62, 81, 82]—and vat photopolymerization [83,84,85,86,87], both employed in only five reports. Finally, 28 publications did not mention the 3D printing technology used [3,4,5,6,7,8,9, 15,16,17, 21, 26, 28, 34, 36, 70, 88,89,90,91,92,93,94,95,96,97,98,99]. This might have to do with the practice of outsourcing 3D printing to external laboratories or private companies.
Anatomical district
The distribution of 3D-printed objects in relation to the anatomical district of interest is summarized in Fig. 3.
Kidney
Our analysis showed that the most common 3D-printed anatomical model was of the kidney, with 45 cases. In 21 cases the model was generated in the presence of a kidney mass to assess its resectability [6, 8, 18, 23, 29, 43, 53, 55, 59, 60, 62, 65, 67, 70, 73, 77, 89, 90, 93, 95, 99], which also occurred with four pediatric patients [12,13,14, 92]. In five cases, the 3D models were used in the planning process for a living donor kidney transplantation [12,13,14, 18, 96]. These surgical procedures were all performed through a laparoscopic or robotic approach (partial or radical nephrectomy) [28, 36, 38, 73, 74]. In nine cases, the 3D models were generated to evaluate resectability with no mention of the planned surgical technique [4, 26, 37, 48, 50, 69, 83, 88, 98]. In seven cases, the 3D-printed models were used to plan a kidney stone removal, through a percutaneous nephrolithotomy approach [3, 21, 49, 54, 66, 74, 89]. Finally, a 3D-printed kidney was also used as an aid in obtaining the informed consent of patients scheduled for a cryoablation procedure [56].
Liver
Liver models were the subject of 26 reports. A common indication in this setting is the planning of a major hepatectomy [31, 34, 35, 61, 78] or of complex hepatic tumor resection [4, 39, 87, 94, 97]. In two cases the models were used as an additional tool in the assessment of hepatic metastases from colorectal carcinoma following chemotherapeutic treatment [22, 33]. In two reports, the underlying disease was a hepatoblastoma [45], with one case involving pediatric patients [92]. Planning of living donor hepatic transplantation represented an additional indication, both in the adult [46] as well as in the pediatric [91] population. Elsewhere, 3D-printed replicas of the liver generated from healthy patients’ medical images [79] as well as from cadaveric scans [80] were used to highlight the normal liver anatomy for educational purposes [81]. Other 3D-printed liver models were employed for training purposes in procedures involving the extrahepatic biliary tree, such as endoscopic maneuvers (flexible choledoscopy [58], laparoscopic choledochal surgery [24] or laparoscopic hepatobiliary surgery [11]). Finally, models were also printed for non-specified hepatic surgery [69], hepatolithiasis [16], complex liver resection [17] and for the production of liver phantoms for the validation of a hepatic vessel segmentation algorithm [85].
Pancreas
Nine publications focused on 3D printing of the pancreas [10, 15, 18, 19, 40, 41, 69, 76, 77], either limited to the reproduction of this gland only, or in combination with a 3D reconstruction of surrounding structures and organs, to plan a pancreatectomy in the setting of a pancreatic tumor.
Spleen
Models of the spleen were produced to plan a splenectomy [18, 20] or to assess the management of a splenic artery aneurysm: either in view of its endovascular treatment or before a laparoscopic or robotic surgery [44, 64]. One case dealt with the reproduction of a large number of abdominal organs, including the spleen, for evaluation of a pediatric malignancy [92].
Abdominal vessels
One report explored the use of 3D-printed models to assess abdominal visceral aneurysms [63]—including splenic, hepatic, gastric, epigastric, gastroduodenal and pancreatico-duodenal aneurysms. Another publication reported the case of a left renal artery aneurysm model [75]. A model of central mesenteric vascular anatomy was also generated for intraoperative navigation during radical D3 right hemicolectomy for cancer (central mesocolic excision) [86]. Furthermore, we found four publications dealing with the 3D printing of models for the planning, simulation or anatomical evaluation of abdominal aorta surgery (due to abdominal aneurysm or occlusive disease) [27, 42, 68, 84]. Six publications were aimed at producing a 3D-printed model of the whole abdominal cavity [5, 9, 25, 32, 73]; due to the preliminary nature of some of these studies, no details were presented on the specific structures addressed, while in two cases the production of a complete phantom for surgical simulation was described [25, 32].
Others
Seven reports dealt with the generation of segments of the gastrointestinal tract, including models of bile ducts [57, 58, 71] and of perianal fistulae [72]. Models were generated for endoscopic submucosal dissection [82], for the planning of percutaneous endoscopic gastrostomy [30] and for the planning of endoscopic submucosal dissection. A model was also created for enhanced visualization of multiple esophageal diverticula [51].
Other publications dealt with the generation of models to simulate robot-assisted radical [38, 62] or partial [8] prostatectomy or for the simulation of a laparoscopic hysterectomy [47] and flexible uteroscopy [52].
Number of clinical cases
Seventy of the analyzed publications presented the use of 3D-printed objects to manage a single clinical case or fewer than ten cases. Only 13 reports described the generation of 3D-printed models for more than ten clinical cases, while 14 publications did not mention the exact number of treated cases.
Type of application
Each report was also labeled with respect to the intended use of the 3D-printed model (Fig. 4), using up to three categories of application for each publication. The most common intended use for 3D-printed models was surgical planning (55 papers), followed by education and training (39 papers) and anatomical comprehension of the area of interest (35 papers).
In 11 cases, the additional recognized value of the model was linked to intraoperative navigation: the surgeon reported the use of these graspable objects to enhance his/her orientation during the procedure. In ten publications, the use of the 3D model was purposely aimed to facilitate explanation to the patient and his/her family of the underlying disease and the planned intervention, with its related technical challenges. Eight reports presented the realization of a complete phantom for surgical simulation: these models included several abdominal structures, typically placed into a reproduction of the abdominal cavity. Particular attention was paid to the material to be used for abdominal organs, to reproduce the haptic characteristics of the tissues as well. Given the difficulty of obtaining realistic mechanical properties with direct 3D printing technology, the molding technique was usually employed in this setting [24, 25, 27, 32, 37]. Only four papers dealt with the production of surgical instrumentation: a liver retractor for surgical resection and/or ablation [94], an overtube system for endoscopic submucosal dissection, enabling independent use of two manipulators [82], and 3D printed models to be used for the design of fenestrated stent grafts to repair endovascular aneurysms [42, 68]. Finally, three publications dealt with preclinical applications, such as the validation of new segmentation algorithms (for hepatic vessels [85] or for the pancreatic parenchyma [76]) or the comparison between homemade and professional 3D printers for anatomical model production [98].
Discussion
Three-dimensional printing technology is playing an emerging role in medicine, as highlighted by the growing amount of medical literature on this topic. The literature review presented here shows how 3D printing technology has started to spread in the area of abdominal surgery as well. A relevant increase occurred in the number of publications on this subject in the last 10 years, moving from 2–3 publications per year in 2008–2009 to 20–30 papers per year in 2017–2018. Three-dimensional printing technology came into general surgery later with respect to other surgical specialties such as orthopedics or maxillofacial surgery, due to the higher complexity of the image elaboration process, which must be mastered to generate a model suitable for 3D printing. The kidney and liver are the most addressed anatomical districts, possibly thanks to their regular morphology and good visibility on medical images, while the most common application is surgical planning, followed by education, training and anatomical comprehension. The most frequently employed 3D printing technologies are material jetting and material extrusion, although many reports do not provide technical details on the manufacturing process. Seventy-three percent of publications report on fewer than ten clinical cases. The presence of a significant amount of preliminary products of research, such as abstracts and posters, suggests that the adoption of 3D printing technology in this area is not yet a consolidated practice. The potential clinical benefit of 3D-printed anatomical replicas is highlighted in all the reports considered in this review. For surgical planning, the most common intended use of 3D-printed objects, the publications considered in this review unanimously recognize the value of this technology in aiding the surgeon to understand the target anatomy, select the most effective surgical strategy, identify the best access for the laparoscopic approach and anticipate certain intraoperative challenges. Three-dimensional printed models also proved to be useful tools for educational purposes, training and preoperative counseling. Three-dimensional printing has enabled the transition from the virtual world to the physical one: from a technological point of view, the advent of new 3D printers allows the combination of different materials with high resolution for the production of realistic replicas that reflect intraoperative conditions. The high number of reports of renal models is probably due to reasons of technical feasibility: kidneys are clearly visible in medical images (MRI and CT) and, consequently, easier to segment and reconstruct. Moreover, they feature a smooth and regular morphology of parenchyma and vasculature, limiting problems in the production and finishing of 3D-printed models. The combination of 3D visual feedback with the manual exploration of the physical 3D-printed model is able to improve detailed anatomical comprehension and to increase, in accordance, surgical proficiency [20]. In fact, 3D-printed models, as compared with the available alternatives (namely MDCT scan images and 3D digital reconstructions), allow a faster and clearer understanding of a patient’s anatomy. Less experienced users such as medical students and residents can perceive the highest benefit, since they lack the experience that is required to build a mental image of the anatomy based on radiological images. Three-dimensional printed models help to transfer complex anatomical information to clinicians, which proves to be useful in preoperative planning, as well as for training and intraoperative navigation. The assessment of anatomical information takes less time when using 3D-printed models than when performed with the corresponding virtual 3D reconstruction or with conventional analysis of 2D slices of MDCT scans [18].
Deformable materials can also be used to reproduce the morphological and mechanical properties of human tissue with greater accuracy, paving the way for more realistic surgical planning, and opening up a new frontier for training on patient-specific platforms. These models are suitable for surgical dissection and the division of vessels and their anastomosis, enabling a realistic simulation of the critical steps of selected procedures and consequently supporting the assessment of operative challenges and of the most suitable technical solution for these. The availability of standardized 3D-printed training models will also facilitate basic research on surgical training, especially in minimally invasive surgery [100]. Preoperative counseling with the patient and his/her family with the support of a 3D model is a valuable opportunity to set realistic expectations regarding the extent of surgery and to discuss possible complications; this can often make the patient more confident when he/she enters the operating room. The availability of a life-size 3D model has positive implications concerning informed consent and other legal issues. Patients’ awareness of the proposed intervention results increased markedly when a 3D-printed model was available [101]. A further application which deserves to be mentioned is the potential use of 3D printing technology to the production of patient-specific tools to be used during the intervention. Although we did not find any example coming from the abdominal surgery field, this kind of application is becoming popular in different specialties as ENT-surgery [102].
The Pavia experience: 3D4Med, a clinical laboratory for 3D printing
In addition to the above analysis on the available literature on 3D printing for abdominal surgery, we would like to report briefly on our experience in the exploitation of 3D printing technology at our university hospital. “3D4Med” is the name of the clinical laboratory for 3D printing at the Policlinico San Matteo of Pavia, established through a collaboration between the hospital and the Department of Civil Engineering and Architecture of the University of Pavia. The laboratory—which is located in the main lobby of the hospital, together with an open exhibition of 3D-printed anatomical objects—aims to provide patient-specific 3D-printed anatomical models for a wide range of clinical specialties. In the past 5 years, 3D4Med has generated 3D models in reply to queries from general, ENT-maxillofacial, orthopedic, vascular and cardiac surgeons. To cover the widest range of applications, the laboratory is equipped with a variety of 3D printers, such as PolyJet™, desktop SLA, and binder jetting, and employs three full-time biomedical engineers. The usual requests addressed by the laboratory fall into two main categories: the need for visual inspection only and the need for mechanical interaction (simulation). When the model is intended for visual inspection only, the focus is on creating a high-resolution replica of the anatomy of interest. Several manufacturing solutions permit the creation of this kind of model; the mechanical properties of the printed materials are of secondary importance, with the emphasis placed on chromatic properties and transparencies, to best highlight crucial anatomical information. To enhance the visibility of hidden or less accessible structures, the anatomical model can be made of artificially produced interlocking parts. This technique allows the user to open the model and assess its internal anatomy, which may not always be clearly visible from the external surface even when a transparent material is used. Indeed, the use of transparent material will invariably produce some degree of optical deformation of the model’s interior, altering the user’s visual perception. When a model is instead generated for simulation purposes, we utilize materials that can mimic the biomechanical features of the tissues or organs involved. Given that we are dealing with soft tissues and organs, deformable materials are mandatory. In this context, having the ability to combine multiple materials within the same product improves the quality of the simulation by reproducing the different mechanical behavior of different tissues. Such models are suitable for the simulation of certain key steps of open, laparoscopic and robotic intervention for the general surgeon (e.g., vessel clamping, cutting and suturing) (Figs. 5, 6).
The fixed costs of establishing our 3D printing laboratory were in the range of 500,000 euros (including the space, air-intake controls, office equipment, computers, energy consumption and three industrial printers). The cost of the material used to produce a single model ranges from 100 to 700 euros, depending on the type of material and the quantity that has to be used. In addition, the generation of the virtual 3D model that is sent to the printer entails an average of 5 h of computer work by a specifically trained technician. The printing time needed to produce each model is between 9 and 22 h, but no human involvement is required for this phase; usually the printer runs overnight. Some post-printing refining is generally needed to remove the support material and glitter the external surface of the model (an hour of manual work). It is therefore difficult to say how much a 3D-printed model costs, since that depends on its quality and on the whole output of the laboratory, which will dilute the fixed costs. To keep these costs sustainable, our advice is to include 3D printing as part of a hospital’s range of services, rather than embarking upon specialty-oriented production.
Conclusions
Our review showed the growing role of 3D printing technology in the field of abdominal surgery. According to our experience and to the reports available in the literature, we can draw the following conclusions on the various applications.
Surgical planning and anatomical comprehension
This is the leading field of application of 3D printing in medicine, regardless to the surgical specialty. According to our experience, the higher the anatomical complexity and/or the lower the experience of the surgeon, the higher the benefit brought by the use of a 3D-printed replica.
Education, training and simulation
A good cost-effective practice—especially in university hospitals—could be to collect the most representative 3D-printed models produced for surgical planning purposes to show them to medical students during the teaching activity. This would dramatically improve the comprehension of the specific pathology and the surgical procedure. As for the surgical training, abdominal surgery must face the still limited performance of deformable materials, but the production of patient-specific models to test in advance the intervention would be probably one of the leading research areas of the forthcoming years.
Patient counseling
Commonly, lawsuits for malpractice against the hospital are originated from a poor understanding of operative risks and complications. In our experience, the use of a 3D-printed model to explain the surgical intervention to the patient and his/her relatives increase their comprehension of the technical aspects of the intervention. In case of limited availability of 3D printing facilities, patient-specific models reconstructed from standard anatomies could be employed instead of patient-specific ones.
In conclusion, we believe that 3D printing technology has the potential to permanently join the armamentarium of the general surgeon as a useful tool for management, planning, research and education purposes as well as an effective support for dialogue with our patients and their families. A lot still needs to be done to achieve this goal, especially on the quantification of the actual impact of the technology on the clinical practice. This should be the next research goal on the topic of 3D printing application to the medical field.
References
ASTM F2792-12a (2012) Standard terminology for additive manufacturing technologies (withdrawn 2015). ASTM International, West Conshohocken. www.astm.org
RefWorks software Copyright© 2019 ProQuest LLC
Bruyere F, Leroux C, Brunereau L, Lermusiaux P (2008) Rapid prototyping model for percutaneous nephrolithotomy training. J Endourol 22(1):91–96
Sugimoto M, Azuma T (2016) 3D printed patient-specific bio-tangible surgical simulation and navigation system for laparoscopic and robotic liver and kidney surgery. Surg Endosc 30:s182
Sugimoto M (2014) New multicolored multimaterial bioelastic organ replication using hybrid mdct and 3D printing technology for tangible digestive surgery simulation. United European Gastroenterol J 2(1):a198
Shiga Y, Sugimoto M, Iwabuchi T, Kawano Y, Yokoyama H, Ooiwa Y, Shimmbori M, Hariu K, Yamamoto R (2014) Benefit of three-dimensional printing in robotic laparoscopic renal surgery: tangible surgical navigation using a patient-based three-dimensional printed kidney. Urology 84(4):s256–s257
Sugimoto M (2014) Patient-specific bio-elastic organ manufacturing by multi-material 3D printer in laparoscopic surgery simulation and navigation. Surg Endosc 20:s10
Sugimoto M (2013) Integrated simulation and navigation system for robotic surgery using bio-texture modeling by multi-material 3D printing. Surg Endosc 27:s4
Sugimoto M (2013) Bio-texture modeling of digestive organ by multi-material 3D printer: feasibility in therapeutic simulation and navigation. Surg Endosc 27:s355
Sugimoto M (2012) Bio-texture modeling technology of gastrointestinal hepatobiliary pancreatic organs by multimaterial 3D printing system. Gastroenterology 142(5):s345
Sugimoto M, Azuma T (2012) Bio-texture modeling by multi-material 3D printing system for laparoscopic surgical simulation and navigation. Surg Endosc 26:s290
Chandak P, Byrne N, Karunanithy N, Stojanovic J, Marks SD, Uwechue R, Gogalniceanu P, Kessaris N, Mamode N (2017) Clinical use of 3D printing in complex pediatric renal transplantation—a phase 2A study of the ideal framework. Transpl Int 30:157
Chandak P, Byrne N, Newton V, Coleman A, Stojanovic J, Marks SD, Kessaris N, Mamode N (2017) Classification of abdominal vascular anomalies and use of 3D printing to support complex renal transplantation in children. Lancet 389:s32
Chandak P, Byrne N, Karunanithy N, Callaghan C, Mushtaq I, Marks SD, Stojanovic J, Ahmed Z, Kessaris N, Mamode N (2016) Using 3D printing in complex pediatric renal transplantation. Am J Transplant 16:749–750
Fang CH (2016) Application of 3D printing technique in the diagnosis and treatment for pancreatic and periampullary neoplasms. HPB 18:e357
Fang CH (2016) The establishment and value of three-dimensional visualization (MI-3DVS) diagnosis platform in the treatment of hepatolithiasis. HPB 18:e508
Fang CH (2016) The application of the liver 3D printing of a medical image three-dimensional visualization system in complex liver resection. HPB 18:e156
Marconi S, Pugliese L, Botti M, Peri A, Cavazzi E, Latteri S, Auricchio F, Pietrabissa A (2017) Value of 3D printing for the comprehension of surgical anatomy. Surg Endosc 31(10):4102–4110
Marconi S, Pugliese L, Del Chiaro M, Pozzi Mucelli R, Auricchio F, Pietrabissa A (2016) An innovative strategy for the identification and 3D reconstruction of pancreatic cancer from CT images. Updates Surg 68(3):273–278
Pietrabissa A, Marconi S, Peri A, Pugliese L, Cavazzi E, Vinci A, Botti M, Auricchio F (2016) From CT scanning to 3-D printing technology for the preoperative planning in laparoscopic splenectomy. Surg Endosc 30(1):366–371
Ghazi A, Campbell T, Melnyk R, Feng C, Andrusco A, Stone J and Erturk E (2017) Validation of a full-immersion simulation platform for percutaneous nephrolithotomy using 3D printing technology. J Endourol
Choi YR, Kim JH, Park SJ, Hur BY, Han JK (2017) Therapeutic response assessment using 3D ultrasound for hepatic metastasis from colorectal cancer: application of a personalized, 3D-printed tumor model using CT images. PLoS ONE 12(8):e0182596
Golab A, Smektala T, Kaczmarek K, Stamirowski R, Hrab M, Slojewski M (2017) Laparoscopic partial nephrectomy supported by training involving personalized silicone replica poured in three-dimensional printed casting mold. J Laparoendosc Adv Surg A 27(4):420–422
Burdall OC, Makin E, Davenport M, Ade-Ajayi N (2016) 3D printing to simulate laparoscopic choledochal surgery. J Pediatr Surg 51(5):828–831
Liao Y, Wang L, Xu X, Chen H, Chen J, Zhang C, Lei H, Wang R, Zhang S, Gu X, Zhena X, Zhou L (2017) An anthropomorphic abdominal phantom for deformable image registration accuracy validation in adaptive radiation therapy. Med Phys 44(6):2381–2396
Adams F, Qiu T, Fritz B, Pollak S, Miernik A, Wetterauer U, Fisher P (2016) Experimental 3D-printed kidney model based on medical imaging data of human cadavers for educational and surgery planning purposes. Eur Urol Suppl 15(3):e358
Condino S, Carbone M, Ferrari V, Alberti A, Forestieri F, Cioni R, Caramella D, Ferrari M, Mosca F (2011) Fabrication strategy to build a patient specific physical simulator for endovascular training. Int J Comput Assist Radiol 6:s272–s273
Smektala T, Golab A, Krolikowski M, Slojewski M (2016) Low-cost silicone renal replicas for surgical training-technical note. Arch Esp Urol 69(7):434–436
Monda SM, Weese JR, Anderson BG, Vetter JM, Venkatesh R, Du K, Andriole GL, Figenshau RS (2018) Development and validity of a silicone renal tumor model for robotic partial nephrectomy training. Urology 114:114–120
Nahkahn JY, Lee GH, Lee JH, Kim DH, Yung KW, Choi KD, Song HJ, Yung HY (2018) The efficacy of a novel percutaneous endoscopic gastrostomy simulator using three-dimensional printing technologies. J Gastroenterol Hepatol 34(4):659–665
Witowski J, Sitkowski M, Wysocki M, Malina Z, Malczak P, Major P, Pedziwiatr M, Budzynski A (2018) 3D printing in laparoscopic liver resections: an initial experience. Surg Endosc 32(1):s271
Kanngott HG, Wunscher JJ, Wagner M, Preukschas A, Wekerle AL, Neher P, Suwelack S, Speidel S, Nickel F, Oladokun D, Maier-Hein L, Dillmann R, Meinzer P, Muller-Stich BP (2015) OpenHELP (Heidelberg Laparoscopic Phantom): development of an open-source surgical evaluation and training tool. Surg Endosc 29(11):3338–3347
Witowski JS, Pedziwiatr M, Major P, Budzynski A (2017) Cost-effective, personalized, 3D-printed liver model for preoperative planning before laparoscopic liver hemihepatectomy for colorectal cancer metastases. Int J Comput Assist Radiol Surg 12(12):2047–2054
Asthana S, Lochan R, Jacob M, Medappil N, Reddy J, Saif R, Raja K, Panackel C, Sakpal M, Ganjoo N (2018) Three-dimensional printing with biotexture modeling assisted donor left hepatectomy. Transplantation 102(5):130
Javan R, Zeman MN (2018) A prototype educational model for hepatobiliarry interventions: unvailing the role of graphic designers in medical 3D printing. J Digit Imaging 31(1):133–143
Giron-Vallejo O, Garcia-Calderon D, Ruiz-Pruneda R, Cabello-Laureano R, Domenech- Abellan E, Fuster-Soler JL, Ruiz-Jimenez JI (2018) Three-dimensional printed model of bilateral Wilms tumor: a useful tool for planning nephron sparing surgery. Pediatr Blood Cancer 65(4):e26894
Glybochko PV, Rapoport LM, Alyaev YG, Sirota ES, Bezrukov EA, Fiev DN, Byadretdinov IS, Bukatov MD, Letunovskiy AV, Kolorev DO (2018) Multiple application of three-dimensional soft kidney models with localized kidney cancer: a pilot study. Urologia J 85(3):99–105
Porpiglia F, Bertolo R, Checcucci E, Amparore D, Autorino R, Dasgupta P, Wiklund P, Tewari A, Liatsikos E, Fiori C (2017) Development and validation of 3D printed virtual models for robot-assisted radical prostatectomy and partial nephrectomy: urologists’ and patients’ perception. World J Urol 36(2):201–207
Madurska MJ, Poyade M, Eason D, Rea P, Watson AJ (2017) Development of a patient-specific 3D-printed liver model for preoperative planning. Surg Innov 24(2):145–150
Andolfi C, Plana A, Kania P, Banerjee PP, Small S (2017) Usefulness of three-dimensional modeling in surgical planning, resident training, and patient education. ***J Laparoendosc Adv Surg Techn A 27(5):512–515
Zheng YX, Yu DF, Zhao JG, Wu YL, Zheng B (2016) 3D printout models vs. 3D-rendered images: which is better for preoperative planning. J Surg Educ 73(3):518–523
Koleilat I, Jaeggli M, Ewing JA, Androes M, Simionescu DT, Eidt J (2016) Interobserver variability in physician-modified endograft planning by comparison with a three-dimensional printed aortic model. J Vasc Surg 64(6):1789–1796
Bernhard JC, Isotani S, Matsugasumi T, Duddalwar V, Hung AJ, Suer E, Baco E, Satkunasivam R, Djaladat H, Metcalfe C, Hu B, Wong K, Park D, Nguyen M, Hwang D, Bazargani ST, De Castro Abreu AL, Aron M, Ukimura O, Gill IS (2016) Personalized 3D printed model of kidney and tumor anatomy: a useful tool for patient education. World J Urol 34(3):337–345
Itagaki MW (2015) Using 3D printed models for planning and guidance during endovascular intervention: a technical advance. Diagn Interv Radiol 21(4):338–341
Souzaki R, Kinoshita Y, Ieiri S, Hayashida M, Koga Y, Shirabe K, Hara T, Maehara Y, Hashizume M, Taguchi T (2015) Three-dimensional liver model based on preoperative CT images as a tool to assist in surgical planning for hepatoblastoma in a child. Pediatr Surg Int 31(6):593–596
Zein NN, Hanouneh IA, Bishop BP, Samaan M, Eghtesad B, Quintini C, Miller C, Yerian L, Klatte R (2013) Three-dimensional print of a liver for preoperative planning in living donor liver transplantation. Liver Transplant 19(12):1304–1310
Ajao MO, Clark NV, Kelil T, Cohen SL, Einarsson JI (2017) Case report: three-dimensional printed model for deep infiltrating endometriosis. J Minim Invasive Gynecol 24(7):1239–1242
Wake N, Rude T, Kang SK, Stifelman MD, Borin JF, Sodickson DK, Wang WC, Chandarana H (2017) 3d printed renal cancer models derived from MRI data: application in pre-surgical planning. Abdom Radiol 42(5):1501–1509
Vernez SL, Spradling K, Dolan B, Dutta R, Okhunov Z, Youssef RF, Kaler K, Landman J, Clayman RV (2016) Three-dimensional printed kidney models with extensive urolithiasis: an over resident educational tool for planning percutaneous nephrolithotomy. J Urol 195(4):e212–e213
Gershman B, Psutka SP, Matsumoto JM, King BF, Kawashima A, Morris JM, Leibovich BC (2016) Use of personalized printed three-dimensional kidney models for simulation before nephron sparing surgery: methodology and examples from a case series. Urol Pract 3(2):124–133
Dickinson KJ, Matsumoto J, Cassivi SD, Reinersman JM, Flatcher JG, Morris J, Wong Kee Song LM, Blackmon SH (2015) Individualizing management of complex esophageal pathology using three-dimensional printed models. Ann Thorac Surg 100(2):692–697
Rajagopal V, Janardan R, Miyaoka R, Monga M, Sweet RM (2009) Modeling and simulation for flexible utheroscopy. J Endourol 23(6):1035–1036
Byadretdinov I, Glybochko P, Alyaev Y, Rapoport L, Bezrukov E, Sirota E (2018) Application of 3d printed models for localized renal cancer treatment. Eur Urol Suppl 17(2):e669–e670
Christiansen AR, Shorti RM, Smith CD, Prows WC, Bishoff JT (2018) Intraoperative utilization of advanced imaging modalities in a complex kidney stone case: a pilot case study. World J Urol 36(5):733–743
Lee H, Nguyen NH, Hvang SI, Lee HJ, Hong SH, Byun SS (2018) Personalized 3d kidney model produced by rapid prototyping method and its usefulness in clinical applications. Int Braz J Urol 44(5):857–858
Schmit C, Matsumoto J, Yost K, Alexander A, Ness L, Kurup AN, Atwell T, Leibovich B, Smith G (2018) Impact of a 3D printed model on patients’ understanding of renal cryoablation: a prospective pilot study. Abdom Radiol (NY) 44(1):304–309
Li A, Tang R, Rong ZX, Zeng JP, Xiang CH, Yu LH, Zhao WP, Dong JH (2018) The use of three-dimensional printing model in the training of choledochoscopy techniques. World J Surg 42(12):4033–4038
Tang R, Ma LF, Li A, Yu LH, Rong ZX, Zhang XJ, Xiang CH, Liao HE, Dong JH (2018) Choledochoscopic examination of a three-dimensional printing model using augmented reality techniques: a preliminary proof of concept study. Surg Innov 25(5):492–498
Wake N, Bjurlin MA, Rostami P, Chandarana H, Huang WC (2018) three-dimensional printing and augmented reality: enhanced precision for robotic assisted partial nephrectomy. Urology 116:227–228
Maddox MM, Feibus A, Liu J, Wang JL, Thomas R, Silberstein JL (2018) 3D-printed soft-tissue physical models of renal malignancies for individualized surgical simulation: a feasibility study. J Robot Surg 12(1):27–33
Yang T, Lin S, Xie Q, Ouyang W, Tan T, Li J, Chen Z, Yang J, Wu H, Pan J, Hu C, Zou Y (2018) Impact of 3D printing technology on the comprehension of surgical liver anatomy. Surg Endosc. https://doi.org/10.1007/s00464-017-5457-5
Porpiglia F, Bertolo R, Checcucci E, Amparore D, Autorino R, Dasgupta P, Wiklund P, Tewari A, Liatsikos E, Fiori C (2018) Development and validation of 3D printed virtual models for robot-assisted radical prostatectomy and partial nephrectomy: urologists’ and patients’ perception. World J Urol 36(2):201–207
Shibata E, Takao H, Amemiya S, Ohtomo K (2017) 3D-printed visceral aneurysm models based on CT data for simulations of endovascular embolization: evaluation of size and shape accuracy. AJR 209(2):243–247
Takao H, Amemiya S, Shibata E, Ohtomo K (2017) 3D printing of preoperative simulation models of a splenic artery aneurysm: precision and accuracy. Acad Radiol 24(5):650–653
Von Rundstedt FC, Scovell JM, Agrawal S, Zaneveld J, Link RE (2017) Utility of patient-specific silicone renal models for planning and rehearsal of complex tumor resections prior to robot-assisted laparoscopic partial nephrectomy. BJU Int 119(4):598–604
Atalay HA, Ulker V, Alkan I, Canat HL, Ozkuvanci U, Altunrende F (2016) Impact of three-dimensional printed pelvicaliceal system models on residents’ understanding of pelvicaliceal system anatomy before percutaneous nephrolithotripsy surgery: a pilot study. J Endourol 30(10):1132–1137
Zhang Y, Ge HW, Li NC, Yu CF, Guo HF, Jin SH, Liu JS, Na YQ (2016) Evaluation of three-dimensional printing for laparoscopic partial nephrectomy of renal tumors: a preliminary report. World J Urol 34(4):533–537
You JH, Kang SG, Kim BM (2013) A novel measurement technique for the design of fenestrated stent grafts: comparison with three-dimensional aorta models. Exp Clin Cardiol 18(1):48–52
Sampogna G, Pugliese R, Elli M, Vanzulli A, Forgione A (2017) Routine clinical application of virtual reality in abdominal surgery. Minim Invasive Ther 26(3):135–143
Kelly B, Casey C, Simpson D, O’Cearbhaill E, Hegazy M, McCann J, Mulvin D, Maguire B (2017) 3D printing of renal malignancies and their arterial supply to improve outcomes in laparoscopic partial nephrectomy. Ir J Med Sci 186(2):s96
Bundy JJ, Weadock WJ, Chick JFB, Srinivasa RN, Patel N, Jonson E, Khayat M, Jeffers B, Gemmete JJ, Srinivasa RN (2018) Three-dimensional printing facilitates creation of a biliary endoscopy phantom for interventional radiology-operated endoscopy training. Curr Probl Diagn Radiol 48:456–461
Sahnan K, Adegbola SO, Tozer PJ, Patel U, Ilangovan R, Warusavitarne J, Faiz OD, Hart AL, Philips RKS, Lung PFC (2018) Innovation in the imaging of perianal fistula: a step towards personalized medicine. Ther Adv Gastroenterol. https://doi.org/10.1177/1756284818775060
Sanchez-Sanchez A, Giron-Vallejo O, Ruiz-Pruneda R, Fernandez-Ibieta M, Garcia-Calderon D, Villamil V, Gimenez-Aleixandre MC, Montoya-Rangel CA, Bermejo JPH (2018) Three-dimensional printed model and virtual reconstruction: an extra tool for pediatric solid tumors surgery. Eur J Pediatr Surg Rep 6(1):e70–e76
Golab A, Smektala T, Krolikowski M, Slojewski M (2018) Percutaneous nephrolithotomy using an individual 3-dimensionally printed surgical guide. Urol Int 100(4):485–487
Holzem KM, Jayarajan S, Zayed MA (2018) Surgical planning with three-dimensional printing of a complex renal artery aneurysm. J Vasc Surg 4(1):19
Schwaiger J, Kagerer M, Traeger M, Gillen S, Dobritz M, Kleeff J, Feussner H and Lueth TC (2012) Manufacturing of patient-specific pancreas models for surgical resections. In: IEEE international conference on robotics and biomimetics (Robio 2012)
Mahmoud A, Bennett M (2015) Introducing three-dimensional printing of a human anatomic pathology specimen: potential benefits for undergraduate and postgraduate education and anatomic pathology practice. Arch Pathol Lab Med 130(8):1048–1051
Xiang N, Fang C, Fan Y, Yang J, Zeng N, Liu J, Zhu W (2015) Application of liver three-dimensional printing in Hepatectomy for complex massive hepatocarcinoma with rare variations of portal vein: preliminary experience. Int J Clin Exp Med 8(10):18873–18878
Kong X, Nie L, Zhang H, Wang Z, Ye Q, Tang L, Li J, Huang W (2016) Do three-dimensional visualization and three-dimensional printing improve hepatic segment anatomy teaching? A randomized controlled study. J Surg Educ 73(2):264–269
Kong X, Nie L, Zhang H, Wang Z, Ye Q, Tang L, Huang W, Li J (2016) Do 3D printing models improve anatomical teaching about hepatic segments to medical students? A randomized controlled study. World J Surg 40(8):1969–1976
Watson RA (2014) A low-cost surgical application of additive fabrication. J Surg Educ 71(1):14–17
Meining A, Roppenecker DB, Luth TC (2015) Development and evaluation of a 3D-printed overtube system made for endoscopic submucosal dissection (ESD). Gastrointest Endosc 81(5):157–158
Knoedler M, Feibus AH, Lange A, Maddox MM, Ledet E, Thomas R, Silberstein JL (2015) Individualized physical 3-dimensional kidney tumor models constructed from 3-dimensional printers result in improved trainee anatomic understanding. Urology 85(6):1257–1261
Celby JB, Heaton CM, Rosen D (2011) Intervention planning tool incorporating rapid prototyping and manufacturing technologies for vascular/interventional radiologists. Int J Comput Assist Radiol 6:s337
Conversano F, Franchini R, Demitri C, Massoptier L, Montagna F, Maffezzoli A, Malvasi A, Casciaro S (2011) Hepatic vessel segmentation for 3D planning of liver surgery. Experimental evaluation of a new fully automatic algorithm. Acad Radiol 18(4):461–470
Luzon JA, Andersen BT, Stimec BV, Fasel JHD, Bakka AO, Kazaryan AM, Ignjatovic D (2018) Implementation of 3D-printed superior mesenteric vascular models for surgical planning and/or navigation in right colectomy with extended D3 mesenterectomy: comparison of virtual and physical models to the anatomy found at surgery. Surg Endosc 33(2):567–575
Yang TY, Tan TB, Yang JL, Pan J, Hu C, Li JH, Zou Y (2018) The impact of using three-dimensional printed liver models for patient education. J Int Med Res 46(4):1570–1578
Lin JC, Myers E (2016) Three-dimensional printing for preoperative planning of renal artery aneurysm surgery. J Vasc Surg 64(3):810
Ng TL, Li CF, Kan WM, Ng CM, Kan CF, Ngai HY, Au WH (2017) 3D printing of kidney models for urological surgeries: our initial experience. Int J Urol 24:45
Rude T, Wake N, Sodickson DK, Stifelman M, Borin J, Chandarana H, Huang WC (2016) An analysis of the effect of 3D printed renal cancer models on surgical planning. Int J Comput Assist Radiol 11(1):s91
Que W, Zong L (2016) Application of 3D printing techniques in pediatric living donor liver transplantation. Transplantation 100(5):s170–s171
Souzaki R, Kinoshita Y, Ieiri S, Kawakubo N, Koga Y, Jimbo T, Obata S, Miyoshi K, Kohashi K, Oda Y, Hara T, Hashizume M, Taguchi T (2015) Efficacy of three-dimensional printing model based on preoperative CT images for the surgery of pediatric malignancies. Pedriatr Blood Cancer 62:s189
Kumar R, Rao N, Ramachandran R, Singh P, Tandon N (2014) Laparoscopic adrenalectomy for pheochromocytoma: comparative outcome analysis of small versus large tumors. Int J Urol 21:a111–112
Wallach D, Peterhans M, Brun B, Banz V, Candinas D, Weber S (2012) Development of a surgical template system for application in image guided liver surgery. HBP 14:131
Byun SS, Lee H, Hong SK, Lee SE (2018) Personalized 3D kidney model produced by rapid prototyping method and its usefulness in clinical applications. Int J Urol 25:362
Chan TCT, Kan CF, Kan RWM, Li TCF, Ng CM, Ngai HY, Au WH (2018) Application of 3D printing technology in laparoscopic donor nephrectomy. Surg Pract 22:22
Gomez-Perez B, Lopez-Lopez V, Robles R, Garcia D, Lopez-Conesa A, Brusadin R, Alconchel F, Navarro A, Parrilla P (2018) Applicability of 3D printing in the planning of complex liver surgery (LIV3DPRINT). HPB 20:s498
Liu DT, Sun ZH, Chaichana T, Ducke W, Fan ZM (2018) Patient-specific 3D printed models of renal tumours using home-made 3D printer in comparison with commercial 3D printer. J Med Imaging Health Inform 8(2):303–308
Yu X, Gang F, Mingfeng L, Mingji Y, Xi-Aming P, Weiqin H (2018) Three dimensional printing assisted laparoscopic partial nephrectomy for patients with renal cancer. Int J Urol 25:389
Nickel F, Hendrie JD, Kowalewski KF, Bruckner T, Garrow CR, Mantel M, Kenngott HG, Romero P, Fischer L, Müller-Stich BP (2016) Sequential learning of psychomotor and visuospatial skills for laparoscopic suturing and knot tying—a randomized controlled trial “The Shoebox Study” DRKS00008668. Langenbecks Arch Surg 401(6):893–901
Marone EM, Rinaldi LF, Pietrabissa A, Argenteri A (2017) Effectiveness of 3D printed models in obtaining informed consent to complex aortic surgery in 25 patients. J Cardiovasc Surg 59(3):488–489
Steinemann DC, Müller PC, Apitz M, Nickel F, Kenngott HG, Müller-Stich BP, Linke GR (2018) An ad hoc three dimensionally printed tool facilitates intraesophageal suturing in experimental surgery. J Surg Res 223:87–93
Acknowledgements
The authors want to acknowledge Ms. Chiara Rebuffi (Fondazione IRCCS Policlinico San Matteo, Scientific Library) for her support in the definition of the search strings on scientific databases. The present work has been supported by the research project “Pancreatic ductal adenocarcinoma (PDAC): development of a new communication platform between radiologists, surgeons and pathologists based on virtual and 3D printed reconstructions of the pancreas and the tumor mass” (PE-2013-02358887) funded by the Italian Ministry of Health. The study falls under the framework of the 3D@UniPV project (ww.unipv.it/3d), one of the strategic research areas of the University of Pavia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Andrea Pietrabissa, Stefania Marconi, Erika Negrello, Valeria Mauri, Andrea Peri, Luigi Pugliese, Enrico Maria Marone e Ferdinando Auricchio have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix

Rights and permissions
About this article
Cite this article
Pietrabissa, A., Marconi, S., Negrello, E. et al. An overview on 3D printing for abdominal surgery. Surg Endosc 34, 1–13 (2020). https://doi.org/10.1007/s00464-019-07155-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07155-5