Abstract
Background
Cameron lesions (CL) are common complications of large hiatal hernia (HH) disease and are known to result in chronic blood loss with resultant microcytic anemia. There is support in the literature that repair of HH may lead to resolution of CL and restore normal hemoglobin levels. This study aimed to determine the impact of elective HH repair on resolution of anemia and the quality of life (QOL) in patients with CL.
Method
A single-institution, retrospective review analyzed all patients with history of CL or anemia (hemoglobin < 12.0 gm/dl in women, < 13.5 gm/dl in men) who underwent HH repair from January 2012 to May 2019. Four validated surveys were used to assess QOL: Reflux Symptom Index (RSI), gastroesophageal reflux disease health-related QOL (GERD-HRQL), laryngopharyngeal reflux health-related QOL (LPR-HRQL), and QOL and swallowing disorders (SWAL) survey. History of iron supplements and perioperative hemoglobin were also noted.
Result
Ninety-six patients were included in this study. The mean age was 67.4 ± 10.8 years and 79% of patients were female. CL were endoscopically identified in 61.5% of patients preoperatively, and the rest of the patients experienced anemia of undiagnosed origin but had a high suspicion for CL. Mean follow-up after HH repair was 17.3 months (range, 1 month–5 years). Mean preoperative hemoglobin was 11.01 ± 2.9 gm/dl and 13.23 ± 1.6 gm/dl postoperatively (p < 0.01). Forty-two (73.7%) patients had resolution of anemia during follow-up and 94.5% stopped supplemental oral iron. Finally, QOL scores significantly improved after surgical intervention: RSI (63%), GERD-HRQL (77%), LPR-HRQOL (72%), and SWAL (13%).
Conclusion
Elective HH repair in patients with chronic anemia secondary to CL may potentially resolve CL and anemia and contribute to significant QOL improvements. Future studies will prospectively assess the resolution of CL with biochemical and endoscopic follow-up to confirm the preliminary findings of our analysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hiatal Hernia (HH) disease is a common pathology with a prevalence of 0.8–2.9%. [1,2,3] Iron deficiency anemia (IDA) is a known complication of large hiatal hernias owing to erosions on the gastric mucosal surface at the diaphragmatic hiatus. Cameron and Higgins (1986) described the formation of linear ulcerations along the herniated gastric mucosa and correlated these with occult gastrointestinal bleeding [4]. These linear erosions, known as Cameron lesions (CL), are endoscopically present in about 3–5% of patients with a known history of hiatal hernias and are the primary source of blood loss leading to chronic IDA [5]. Despite the decades since their identification and description, the pathophysiology of CL remains unclear, although mechanical trauma secondary to traction forces at the hiatus during respiration and acid-related mucosal injuries have been suggested [6, 7].
HH repair entails the reduction of the herniated contents, closure of the diaphragmatic defect, and fundoplication, and some studies have demonstrated that repair of HH may lead to resolution of CL and restore normal hemoglobin levels [5, 8, 9]. It is therefore reasonable to postulate whether corrective strategies to resolving IDA due to CL should include surgical repair of HH. Most of these studies contained small surgical case series and lack data regarding improvement in quality of life (QOL) following surgical repair.
This study aimed to evaluate the resolution of anemia as well as the improvements in QOL outcomes among a cohort of patients with a history of chronic anemia due to CL after elective HH repair.
Methods
Study design
Institutional Review Board approval was granted for this protocol. We conducted a single-institution retrospective review of patients undergoing HH repair between January 2012 and May 2019. We identified all patients with preoperative anemia defined, according to the World Health Organization (WHO) criteria, as serum hemoglobin (Hgb) levels < 12.0 gm/dl in women and < 13.5 gm/dl in men measured within 1 month before surgery [10]. When available, preoperative upper endoscopy results were reviewed for identification of CL. We excluded patients who had other identifiable cause of IDA such as, but not limited to, autoimmune diseases, iron-deficient diet, cancer, and other hematological disorders. The majority of the study population were referred for surgical intervention at our center only after completing an extensive evaluation at outside centers to establish a diagnosis of IDA. As a result of this, further comprehensive hematological data analysis was not performed. Some patients were not anemic at the time of preoperative evaluation but were included in the study due to a recurrent history of anemia and continued dependency on iron supplementation. Patient demographic information, iron supplementation, transfusion history of packed red blood cells (PRBC), and perioperative data were analyzed. Follow-up was completed by review of outpatient records, a telephone interview with the patient, or both. The most recent recorded Hgb level, at least 1 month following surgery, was used to determine the presence and degree of anemia. Primary outcomes included anemia resolution, as determined by the return of Hgb to normal levels according to WHO criteria, and, when applicable, complete discontinuation of iron supplementation or need for PRBC transfusion; we also examined postoperative improvement in QOL outcomes. Secondary outcomes included perioperative complications including presence of/development of postoperative ileus (> 5 days), urinary tract infection (UTI), venous thromboembolism (VTE), respiratory complications (pneumonia, atelectasis, etc.), acute renal insufficiency, and cardiac complications (congestive heart failure, myocardial infarction, etc.), and readmission and reoperation rates.
Operative technique
Our operative approach involves the reduction of all herniated intrathoracic viscera including the stomach by taking down hernia sac adhesions. This is followed by division of the short gastric vessels with an energy device. Mediastinal dissection of the esophageal adhesions is undertaken to obtain adequate intraperitoneal esophageal length, a minimum of 2 cm. An esophageal lengthening procedure in the form of Collis gastroplasty is performed only with shortened esophagus following an unsuccessful dissection to return the gastroesophageal junction to an intraabdominal position [11]. Retroesophageal crural closure is performed around a (56 Fr) bougie within the esophagus. A Nissen or partial fundoplication is then performed in standard fashion based on parameters of preoperative esophageal manometry.
QOL outcome metrics
Quality of life (QOL) assessments were obtained either in-person, via telephone, or by electronic communication between the clinical team and patients who consented for data collection and participation in this research. Patient QOL metrics were analyzed using four validated surveys administered preoperatively and postoperatively at 1 month, 6 months, and then annually following surgery. These included the Reflux Symptom Index (RSI), gastroesophageal reflux disease health-related QOL (GERD-HRQL), laryngopharyngeal reflux QOL (LPR-HRQL), and swallowing QOL (SWAL-QOL) instruments [12,13,14,15].
The RSI is a validated nine-item outcomes instrument that documents symptom severity for laryngopharyngeal reflux based on a five-point scale per question and ranging in total from 0 to 45 points [15]. The instrument was designed to evaluate both typical and atypical symptoms of GERD, such as difficulty breathing, chronic cough, hoarseness, or globus sensation. The 45-point GERD-HRQL tool is a quantitative method of measuring typical symptom severity in GERD patients and was used to assess for any measurable improvement in these symptoms when identified concomitant to atypical symptoms [14]. Scores varied from 0 to 45 as in the RSI also with a five-point scale per question. The LPR-HRQL questionnaire is a validated survey assessing the frequency and severity of vocal changes, dysphonia, cough, and the overall QOL impact of gastric reflux on a standard seven-point Likert scale [13]. Forty-three questions are subdivided into hierarchical categories including vocal quality, cough, throat clearing, swallow, and the overall impact of acid reflux scored to a ten point maximum per question with a total of 314 points possible. Lastly, the SWAL-QOL survey assesses ten QOL concepts through a 44-item tool with a maximum of 70 points to differentiate normal swallowing behaviors of patients suffering from oropharyngeal dysphagia [12]. The SWAL-QOL is especially sensitive to differences in the severity of clinical dysphagia compared to other survey instruments.
Statistical analysis
Study data were collected and managed using Research Electronic Data Capture (REDCap) electronic data capture tools hosted at Anne Arundel Medical Center [16]. REDCap is a secure, web-based application designed to support data capture for research studies, providing an intuitive interface for validated data entry; audit trails for tracking data manipulation and export procedures; automated export procedures for seamless data downloads to common statistical packages; and procedures for importing data from external sources. Statistical analysis of study data included the utilization of Pearson’s χ2 and Student’s T tests for preoperative and postoperative metrics, while one-way ANOVA was performed with post hoc analysis using a Tukey correction for QOL outcomes over the postoperative follow-up intervals. A logistic regression analysis was performed to determine predictors of anemia resolution. P value < 0.05 was considered statistically significant for all analyses. All statistical analysis was performed using MathWorks MATLAB_R2018b (MathWorks, Natick, MA, USA).
Results
Ninety-six patients met the inclusion and exclusion criteria and were included in the analysis [21 males (21%) and 75 females (79%)]. The mean age, Body Mass Index (BMI), HH diameter, and ASA score were 67.4 ± 10.8 years, 29.8 ± 5.1 kg/m2, 6.1 ± 1.8 cm, and 2.5 ± 0.5, respectively (Table 1). Intraoperatively, the average herniated percentage of stomach in the mediastinum was 66% (range, 15–100%). Fifty-nine patients (61.5%) had preoperative endoscopic confirmation of CL, while the remainder had a high suspicion of CL based on finding of a sizeable HH and a diagnosis of exclusion after a history of negative hematological and gastrointestinal investigations. Gastroesophageal reflux disease (GERD) was the leading comorbidity (90.6%) among the study population. The distribution of comorbidities is outlined in Table 1.
Patients had a mean operative time of 100 ± 25 min and blood loss 19.7 ± 28.4 mL on average. All patients underwent a HH repair as the primary procedure. 89.6% of patients also underwent a Nissen fundoplication. 30.2% required a Collis gastroplasty in addition to a Nissen fundoplasty to return the gastroesophageal junction to the abdominal cavity to ensure a short tension-free fundoplication in addition to re-establishing the angle of His. The remaining patients had a partial fundoplasty [11]. A subset of our patients were redo HH patients (2.1%) and redo Nissen fundoplication (1%). Four patients required gastropexy via gastrostomy tube placement. There was only one intraoperative complication involving a distal esophageal injury, which was recognized at the time of surgery and repaired in a primary fashion. Postoperative complications included venous thromboembolic events (1%), arrhythmia (2.1%), pneumonia/pneumonitis (2.1%), pneumothorax (2.1%), prolonged Ileus (2.1%), oral intolerance (2.1%), and need for antibiotic treatment (2.1%) (Table 2.). There were four readmissions (4.2%) within 30 days after surgery and three reoperations (3.1%) by the latest follow-up. Two re-operative patients presented with failure to thrive secondary to intractable nausea and vomiting. A gastrostomy tube was endoscopically placed in one patient and a jejunostomy tube in the other, both for nutritional support. The third re-operative patient presented with a perforation at the gastroesophageal junction 4 months after HH repair and antireflux surgery due to non-adherence to our dietary regimen and required open exploration.
Anemia-related outcomes are outlined in Table 3. Patients reported significant resolution of anemia and discontinuation of related treatments after surgical repair (p ≤ 0.05) during a mean follow-up of 17.3 months (range, 1 month–5 years). 80.6% of anemic patients with endoscopic confirmation of Cameron’s Lesions achieved resolution of anemia at latest follow-up compared to 65.4% of anemic patients with a diagnosis of exclusion (p = 0.199). Approximately 15% of patients remained persistently anemic following surgery. There was also a significant improvement in mean Hgb level, outline in Table 3, during an average follow-up of 17.3 months (range, 1 month–5 years).
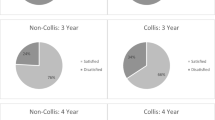
Post hoc ANOVA statistical analysis of QOL metrics revealed that patients reported significant improvements following HH repair for all metrics (Fig. 1). All of the validated QOL scores demonstrated significant improvement at latest follow-up. There were improvements in RSI (63%), GERD-HRQL (77%), LPR-HRQOL (72%), and SWAL (13%), respectively. At latest follow-up, 70% of patients reported being satisfied with their condition and almost 60% discontinued use of antireflux medication (Table 4). A logistic regression was performed to determine predictors of anemia resolution (Table 5). Results of this analysis showed discontinuation of antireflux medication after surgical repair was predictive of anemia resolution, which we describe below.
Graphical representation for QOL outcomes from baseline to most recent follow-up. A Percentage of patients using a proton pump inhibitor (PPI). B Percentage of patients who had stated that they were satisfied with their present condition. C Average score for the validated survey instruments Reflux Symptom Index (RSI), gastroesophageal reflux disease health-related QOL (GERD-HRQL), laryngopharyngeal reflux QOL (LPR-HRQL) at each interval, and swallowing QOL (SWAL-QOL). Error bars are represented as 95% confidence interval
Discussion
Hiatal hernia disease can manifest broadly including dysphagia, reflux, shortness of breath, and anemia secondary to CL. First-line treatment of IDA due to CL is medical management with long-term iron supplementation and high-dose proton pump inhibitors. Resolution of anemia following surgical repair has been well established in the literature [2, 5, 9]. Thus, surgical intervention is recommended when anemia is refractory to medical management, and reports show that about 70–90% of patients with IDA due to CL will achieve resolution of anemia following surgical repair. However, the majority of these studies contain small surgical case series [2, 9]. Also, there is a lack of data on the QOL of patients following surgical treatment.
To our knowledge, we present here the most extensive series of patients with a diagnosis of CL evaluated for resolution of anemia and improvement in QOL outcomes after surgery. Our results demonstrate that patients whose anemia was attributed to diaphragmatic hernia experienced resolution of their anemia and also achieved significant QOL improvements after surgical correction. Our experience and results support the efficacy of operative therapy for paraesophageal hernia disease when diagnosed in appropriately selected symptomatic patients. We believe early diagnosis and elective repair of symptomatic paraesophageal hernia is warranted. This approach will be most effective in the prevention of long-term sequelae from symptomatic HH including IDA secondary to CL. There is also support in the literature that emergent repair typically carries a significantly increased risk of mortality and morbidity as well as a higher utilization of hospital resources compared with elective repair of large hiatal hernias [17]. As shown by our data (Table 5), patients with IDA secondary to CL did not benefit from preoperative antireflux medications. Although acid inhibition together with iron supplementation is effective in treating anemia secondary to CL, surgical intervention may indeed provide a definite cure to the underlying etiology- HH [7, 18].
Our high-volume tertiary foregut disease center employs a comprehensive preoperative assessment to work up all patients presenting with anemia to determine underlying etiology. All patients suspected of CL and/or IDA should undergo a multi-disciplinary work-up, involving hematological and gastrointestinal evaluations. This significantly reduces the risk of missed diagnoses outside of advanced HH disorders, which may be concomitantly present and be responsible for IDA. Optimal postsurgical outcomes in this population are strongly linked to appropriate candidate selection based on this objective assessment. Patients suspected of having IDA secondary to CL should undergo hematological work-up, including a complete blood count and serum ferritin levels, to confirm evidence of anemia as well as low iron stores, respectively [19, 20]. A comprehensive endoscopic evaluation of the gastrointestinal tract including colonoscopy, small bowel studies, and esophagogastroduodenoscopy (EGD), with particular attention given to antegrade and retrograde visualization of the hernia neck and adjacent tissue, is also necessary to confirm evidence of CL and rule out other etiologies of blood loss. Due to the difficulty in identifying CL on initial EGD, repeat endoscopy may be needed in patients with persistent IDA of unknown cause [18, 21]. The presence of reflux symptoms requires further evaluation including 24-h pH test and esophageal motility testing in selected patients. Following a complete evaluation to rule out other causes of blood loss, surgery can then be offered to patients with HH and concomitant CL and/or IDA. Postoperative hematological and endoscopic follow-up, when indicated, may be necessary to confirm the resolution of IDA and CL.
In addition to significant improvements in QOL with surgical therapy, the majority of our patients were able to discontinue antireflux therapy and iron supplementation after surgery. Discontinuation offers additional financial benefits to the patient and healthcare system, and reduces unnecessary pharmacologic therapy and the adverse side effects linked to long-term use of antireflux medications and iron supplements.
This was a retrospective study at a single high-volume foregut center with results that may not be broadly applicable to all surgeons or surgical centers. A prospective study following patients with IDA due to CL, when present, with comprehensive biochemical (including iron studies) and endoscopic follow-up will provide a greater appreciation of the unique treatment outcomes associated with surgical repair. The possibility of recall bias is inherent to all studies that rely on any retrospective analysis. However, we prospectively collect momentary QOL data at predetermined time points which reduce recall bias, and thus we are confident in the generalizability of our QOL data to the larger HH patient population.
Conclusions
Our findings suggest that CL are strongly associated with chronic anemia in patients with a history of large HH and require a high index of suspicion particularly in patients with a history of IDA of unknown cause. These findings present our initial investigations into the resolution of IDA and CL following successful HH repair. Our study demonstrates that surgical repair provides both clinical resolution of IDA and improvements in QOL for appropriately selected patients. Ongoing prospective evaluations at our center into laboratory testing and endoscopic follow-up for this patient population are underway.
References
Chevrollier G, Brown A, Keith S et al (2019) Preoperative anemia: a common finding that predicts worse outcomes in patients undergoing primary hiatal hernia repair. Surg Endosc 33(2):535–542. https://doi.org/10.1007/s00464-018-6328-4
Trastek VF, Allen MS, Deschamps C, Pairolero PC, Thompson A (1996) Diaphragmatic hernia and associated anemia: response to surgical treatment. J Thorac Cardiovasc Surg 112(5):1340–1345. https://doi.org/10.1016/S0022-5223(96)70149-6
Kimer N, Schmidt PN, Krag A (2010) Cameron lesions: an often overlooked cause of iron deficiency anaemia in patients with large hiatal hernias. BMJ Case Rep. https://doi.org/10.1136/bcr.06.2010.3129
Cameron AJ (1976) Incidence of iron deficiency anemia in patients with large diaphragmatic hernia. A controlled study. Mayo Clin Proc 51(12):767
Gray DM, Kushnir V, Kalra G et al (2015) Cameron lesions in patients with hiatal hernias: prevalence, presentation, and treatment outcome. Dis Esophagus 28(5):448–452. https://doi.org/10.1111/dote.12223
Windsor CW, Collis JL (1967) Anaemia and hiatus hernia: experience in 450 patients. Thorax 22(1):73–78. https://doi.org/10.1136/thx.22.1.73
Moskovitz M, Fadden R, Min T, Jansma D, Gavaler J (1992) Large hiatal hernias, anemia, and linear gastric erosion: studies of etiology and medical therapy. Am J Gastroenterol 87(5):622–626
Skipworth RJE, Staerkle RF, Leibman S, Smith GS (2014) Transfusion-dependent anaemia: an overlooked complication of paraoesophageal hernias. Int Sch Res Notices 2014:479240–479244. https://doi.org/10.1155/2014/479240
Carrott P, Markar S, Hong J, Kuppusamy M, Koehler R, Low D (2013) Iron-deficiency anemia is a common presenting issue with giant paraesophageal hernia and resolves following repair. J Gastrointest Surg 17(5):858–862. https://doi.org/10.1007/s11605-013-2184-7
World Health Organization (2011) Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. http://www.who.int/iris/handle/10665/85839. Accessed 1 Apr 2019
Weltz AS, Zahiri HR, Sibia US, Wu N, Fantry GT, Park AE (2017) Patients are well served by Collis gastroplasty when indicated. Surgery 162(3):568–576. https://doi.org/10.1016/j.surg.2017.04.005
McHorney CA, Robbins J, Lomax K et al (2002) The SWAL–QOL and SWAL–CARE outcomes tool for oropharyngeal dysphagia in adults: III. Documentation of reliability and validity. Dysphagia 17(2):97–114. https://doi.org/10.1007/s00455-001-0109-1
Keefe MA (2006) Validation of a quality-of-life instrument for laryngopharyngeal reflux. Yearb Otolaryngol Head Neck Surg 2006:129–130. https://doi.org/10.1016/S1041-892X(08)70113-6
Velanovich V (2007) The development of the GERD-HRQL symptom severity instrument. Dis Esophagus 20(2):130–134. https://doi.org/10.1111/j.1442-2050.2007.00658.x
Belafsky PC, Postma GN, Koufman JA (2002) Validity and reliability of the Reflux Symptom Index (RSI). J Voice 16(2):274–277. https://doi.org/10.1016/S0892-1997(02)00097-8
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Polomsky M, Hu R, Sepesi B et al (2010) A population-based analysis of emergent versus elective hospital admissions for an intrathoracic stomach. Surg Endosc 24(6):1250–1255. https://doi.org/10.1007/s00464-009-0755-1
Panzuto F, Di Giulio E, Capurso G et al (2004) Large hiatal hernia in patients with iron deficiency anaemia: a prospective study on prevalence and treatment. Aliment Pharmacol Ther 19(6):663–670. https://doi.org/10.1111/j.1365-2036.2004.01894.x
Short MW, Domagalski JE (2013) Iron deficiency anemia: evaluation and management. Am Fam Phys 87(2):98–104
Goddard AF, McIntyre AS, Scott BB, British Society of Gastroenterology (2000) Guidelines for the management of iron deficiency anaemia. Gut 46(Suppl 3-4):IV1
Cameron AJ, Higgins JA (1986) Linear gastric erosion. A lesion associated with large diaphragmatic hernia and chronic blood loss anemia. Gastroenterology 91(2):338
Funding
No financial support was received for this study.
Author information
Authors and Affiliations
Contributions
All authors certify that they accept responsibility as an author and have contributed to the concept, data gathering, analysis, manuscript drafting, and give their final approval.
Corresponding author
Ethics declarations
Disclosures
Dr. Park, Addo, Zahiri, Brooks, and Mr. Broda have no conflict of interest or financial or relevant financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Addo, A., Broda, A., Reza Zahiri, H. et al. Resolution of anemia and improved quality of life following laparoscopic hiatal hernia repair. Surg Endosc 34, 3072–3078 (2020). https://doi.org/10.1007/s00464-019-07054-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07054-9