Abstract
Background
Right-sided colonic diverticulitis (RCD) is an Asian-centric disease. The optimal treatment for acute uncomplicated RCD remains a controversial area. This study aimed to compare the safety and efficacy of laparoscopic diverticulectomy (LD) with non-operative treatment (NT) in patients with uncomplicated RCD.
Methods
A single-center, prospective, non-randomized controlled study ran from 2009 to 2017. Patients with first episode of uncomplicated RCD were divided into two treatment arms, LD or NT with bowel rest and broad-spectrum antibiotics, based on their choice. The primary outcome was recurrent diverticulitis during follow-up. Secondary outcomes were treatment success and complications.
Results
A total of 155 patients were enrolled, with 81 in the NT arm and 74 in the LD arm. Mean follow-up was 49 months. The treatment success rate for the NT arm was 90.1% and for the LD arm, 86.5% (P = 0.480). There was no significant difference in the complication rate between the LD arm, 12.2% and the NT arm, 8.6% (P = 0.472). LD was better than NT in preventing recurrent diverticulitis. Nine patients in the NT arm and none in the LD arm had recurrence (P = 0.003). The number needed to treat to prevent recurrence was nine.
Conclusion
Non-operative management with bowel rest and antibiotics for uncomplicated RCD is safe and effective. Alternatively, LD is also safe and effective, with the added benefit of preventing recurrences. While both treatments could be reasonably offered for uncomplicated RCD, LD is an appealing option when recurrence is a concern.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Right-sided colonic diverticulitis (RCD) is more common in Asian than in Western populations. In Western countries, RCD constitutes about 1% to 3.6% of all colonic diverticular diseases [1, 2]. In Asian populations, RCD is more prevalent compared to left-sided colonic diverticulitis, accounting for 70% to 98% of colonic diverticulitis cases [3,4,5]. The pathogenesis of right-sided diverticula remains controversial, and the natural history of RCD is not well understood. Furthermore, there is no clear guidelines on the management of RCD. Non-operative management with intravenous antibiotics and bowel rest in patients with uncomplicated RCD have been reported to be effective in some studies [6,7,8,9]. However, these patients are at risk of disease progression requiring emergent surgical intervention. The risk of disease progression while on non-operative management is not well reported in the literature. Furthermore, approximately 15% to 20% of patients with RCD develop recurrence after non-operative treatments [6, 10]. In contrast, operative management for RCD has been advocated as a safe and effective strategy to reduce recurrence [11,12,13,14,15,16]. Conventional surgical approaches for RCD include open diverticulectomy or right hemicolectomy when multiple diverticuli are found, or when neoplastic disease cannot be excluded. When technically feasible, laparoscopic diverticulectomy is equally effective to open surgery in outcomes, while offers additional values to patients such as improved pain control, better patient satisfaction, and shorter hospital stays [14,15,16]. Given these additional advantages and equivalent outcome, we chose to select laparoscopic surgery as an upfront surgical strategy in this prospective study, comparing the short-term and long-term outcomes of laparoscopic diverticulectomy (LD) versus non-operative treatment (NT) in patients with uncomplicated RCD. We hypothesized that both treatments are equally safe and effective, and LD has a lower recurrence rate over NT.
Materials and methods
Patients and study design
This was a prospective, single-center, non-randomized controlled study comparing recurrence rate between patients with uncomplicated RCD who underwent LD versus patients who underwent NT. The study was performed between 2009 and 2017 at People of Gia Dinh hospital, a tertiary referral center in Ho Chi Minh City, Vietnam. The protocol was approved by the local ethic committee. From 2009 to 2014, patients were consecutively enrolled to the study at the time radiological diagnosis of RCD became available. All enrolled patients were managed by the same surgical team. Written informed consent was obtained from all patients and relatives before enrollment. Data were analyzed according to the intention to treat principle.
Eligibility criteria
Patients older than 18 years with clinical diagnosis of right-sided abdominal pain suspicious for RCD were assessed for eligibility. These patients subsequently underwent further clinical and radiological assessment with either ultrasound (US), computerized tomographic (CT) scan, or both. Only patients with clear radiological evidence of RCD are included in the study. Criteria for RCD in US were: (1) surrounding echogenic fat, (2) diverticular wall thickening, (3) adjacent lymph node enlargement, (4) intra-diverticular or peri-diverticular fluid collection, and (5) intra-diverticular echogenic material. Criteria for RCD in CT images were: (1) presence of a diverticula, (2) thickening of the cecal wall, (3) peri-colonic fat infiltration, (4) intramural air bubbles, and (5) a normal appendix. Patients with signs of appendicitis on imaging (inflamed appendix larger than 6 mm in diameter, thickened wall more than 2 mm (target sign), peri-appendiceal inflammation, presence of fecalith) were excluded. Other exclusion criteria were presence of hemodynamic instability and/or multi-organ failure, American Society of Anesthesiologists (ASA) classification III or higher, severe ileus, generalized peritonism on examination, perforation, abscesses, fistula, intestinal obstruction on imaging, and failure to give consent.
Study interventions and description of surgical technique
The study had two arms: the LD arm and the NT arm. In the LD arm, surgery was performed within 12 h of study enrollment. Three ports were used: one 10-mm camera port at the umbilicus, and two 5-mm instrument ports at the suprapubic and the left iliac fossae. We used a combination of sharp and blunt dissection to separate and visualize the terminal ileum, the appendix, the cecum, and the diverticulum. A laparoscopic resection of the diverticulum was performed with dissection of diseased tissue down to the base of the diverticulum, subsequently followed by intracorporal suture repair with Monosyn 3-0, a synthetic absorbable monofilament (B-Braun, Vietnam) (Fig. 1). Post operation, patients were kept nil by mouth and on intravenous antibiotics until clinical and laboratory improvements were evident. Treatments for patients in the NT group included bowel rest and intravenous broad-spectrum antibiotics, including a beta lactamase and metronidazole, followed by a week of oral antibiotics after discharge, most often amoxicillin/clavulanic acid (Augmentin, GlaxoSmithKline) or ciprofloxacin (Cipro, Bayer) in patients with Augmentin allergy. Oral intake resumed when patient was afebrile and non-tender. Study members provided enhanced patient education on compliance to antibiotics to patients and family members upon discharge and verified compliance to treatment during follow-up.
Major steps in laparoscopic diverticulectomy for right-sided diverticulitis. A Identification of the inflamed diverticulum (triangle), cecum (asterisk), terminal ileum (thin arrow) and appendix (not shown). Note the inflamed fatty tissue surrounding the diverticulum. The cecum and terminal ileum are normal; B dissection of the diverticulum. Noted the inflamed adipose tissue are being dissected off the diverticulum; C, D The neck of the diverticulum (thick arrow) is being divided close to the cecal base. All inflamed tissues were removed as seen in (D); E Suture line after intracorporeal laparoscopic repair
Study endpoints
All patients in both groups were followed up for at least 12 months. Outpatient visits were performed after discharge 1 week, 1 month, 6 months, and 12 months. After 12 months, patients were followed up via telephone biannually. During this follow-up period, if patients had signs and symptoms suggestive of recurrence of RCD, they were recalled for CT scan. The primary endpoint was recurrence after one month of discharge, which was defined as CT evidence of recurrent RCD. Recurrence within one month from discharge was considered as treatment failure. Secondary endpoints included treatment success and complications. Complications were classified using the Clavien-Dindo classification [17], based on the therapy required to treat them. There are five main grades. Grade I complication does not require any intervention, pharmacological or procedural. Grade II requires pharmacological treatments. Grade III requires surgical, endoscopic, or radiological interventions. Grade IV consists of life-threatening complications, and death results in Grade V [17]. In the NT arm, treatment success was defined as clinical improvement and discharge without progression of disease requiring surgical intervention. In the LD arm, treatment success was defined as successful completion of laparoscopic diverticulectomy without conversion to open surgery.
Sample size calculation
Analysis of available data in the literature during protocol development suggested that the recurrence rate would be 15% in the NT group [6, 10]. In the LD group, we assumed that this proportion would be lower than 1%. To achieve statistical power of 80% to detect difference using a 5% two-sided significance level with Pearson’s Chi square test, the target sample size was 116 patients with 58 patients in each arm. With the estimated lost to follow-up of 25%, the required number of patients in each group was 74 patients.
Statistical analysis
The primary endpoint is the recurrence rate in each arm. The cumulative proportion of recurrent diverticulitis was calculated by Kaplan–Meier estimate and illustrated by the Kaplan–Meier curves with the number of patients at risk indicated below the plot at specific time points. Two-sided log-rank test was used to compare the recurrence rate between the two treatments. Secondary outcomes, including treatment success and complications, were analyzed using two-sided Fisher’s exact test. Other variables were compared between the two groups using Mann–Whitney test for numeric variables and Fisher’s exact test for categorical variables, where appropriate. Statistical significance was defined when P value was less than 0.05. All analyses were performed with R statistical software (Version 3.2.3, Austria) [18].
Results
Patients’ flow
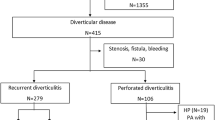
During the study recruitment period from 2009 to 2014, 416 patients were screened for eligibility at our institution, of which 261 patients were excluded and 155 patients with diagnosis of uncomplicated RCD were enrolled and followed up. Laparoscopic diverticulectomy versus non-operative treatment options were discussed with patients. Patient was enrolled to each respective study arm depends on their treatment preference (Fig. 2). In the LD group, 74 patients underwent LD, out of which ten patients required conversion to open surgery. In the NT group, 81 patients received NT, out of which eight patients required surgical interventions. There were 40 patients lost to follow-up after outpatient visits at one month; among these patients, 18 patients were in the LD group and 22 patients were in the NT group.
Study’s flowchart. In this patient, diverticulitis was confirmed intraoperatively. However, there was no perforation and the inflammation was minimal. Decision was made to not perform diverticulectomy; incidental appendectomy was performed to prevent future diagnostic uncertainty. ASA American Society of Anesthesiologists physical status classification
Baseline data
Patient’s characteristics are shown in Table 1. The two groups did not differ significantly in terms of age, gender, body mass index, current smoking, ASA status, previous abdominal surgery history, comorbidities, and white blood cell counts (Table 1).
Treatment success and complication rates
There was no significant difference in the treatment success and the complication rate between the two groups (Table 2). In the LD group, 64 patients (86.5%) were successfully treated with laparoscopic diverticulectomy; ten patients (13.5%) required conversion to open diverticulectomy and were considered failure of therapy. In the NT group, 73 patients (90.1%) were treated successfully; eight (9.9%) had signs and symptoms of disease progression after 24-h period of the NT, and thus required surgical interventions, out of which six cases were operated using laparoscopic technique. Complications occurred in nine patients (12.2%) in the LD group and seven patients (8.6%) in the NT group. There was one Clavien-III complication in the LD group in which the small bowel was inadvertently injured, requiring laparoscopic repair on the second postoperative day. All other complications in the LD group were Clavien-I. There was no mortality within the two groups.
Recurrence rate
The Kaplan–Meier curve of recurrence rate across the two treatment groups is shown in Fig. 3. There was no recurrence in the LD group despite a longer length of follow-up (51.7 ± 33.1 months) compared to nine recurrences found in the NT group (mean length of follow-up was 46.4 ± 31.0 months). The number needed to treat (NTT) to prevent recurrence was nine. Among these recurrences, seven patients continued to have successful non-operative treatments; two cases had complications and were treated by laparoscopic colectomy. The Kaplan–Meier estimated recurrence rate was significantly higher in the NT group compared to the LD group (16.6% and 0%, respectively, P = 0.003). Additionally, six of these nine recurrences occurred after 12 months of follow-up, and three occurred within the first 12 months. The mean recurrence interval after the first attack was 38 months.
Kaplan–Meier analysis of recurrence rates across treatments. The Kaplan-Meier estimates with 95% confidence intervals of recurrence of diverticulitis for all patients. Solid line indicates patients in NT group and dashed line indicates patients in LD group. The numbers of patients at risk are shown below the graph at baseline and each year of follow-up. LD laparoscopic diverticulectomy, NT non-operative treatment
Discussion
The optimal treatment for uncomplicated RCD remains controversial and deficient in prospective data. We aimed to address this gap with this prospective series comparing the outcome of LD versus NT in patients with uncomplicated RCD. Data from this study suggest that both LD and NT are efficacious in treating uncomplicated RCD with no significant difference in perioperative complications (Table 2). However, LD has two additional benefits over NT. Firstly, LD limits the morbidity of sepsis and perforation with disease progression and secondly, it reduces recurrence risk (Fig. 3). Eight patients (9.9%) in the NT group experienced disease progression with abscess formation, worsening peritonitis requiring emergent surgical intervention. Three of these eight patients required more extensive surgery in which right-sided colectomy were performed. No patient in the LD group experienced disease progression and only one experienced Clavien-III complication secondary to preventable technical error. Additionally, there was no recurrence in the LD group.
Distinction between RCD and appendicitis is challenging based on signs and symptoms alone [19]. The patients who were initially screened for study eligibility had subtle historical features atypical of appendicitis: longer yet more indolent course of right iliac fossa pain without toxicity, less nausea and vomiting, and low Alvarado score (0–3) [20]. These patients subsequently underwent further radiological evaluation before being enrolled. Both US and CT have high specificity and sensitivity in the diagnosis of RCD. In particular, CT performed with 98% sensitivity and specificity in distinguishing RCD from acute appendicitis [21, 22]. Abdominal US, on the other hand, has a diagnostic accuracy rate of 99.5% for diverticulitis in a study of 934 patients who presented with right-sided abdominal pain [23]. Only patients with clear radiological features of RCD were further enrolled. Any patient with equivocal radiological features and in whom appendicitis cannot be excluded were not enrolled. We understand that our inclusion and exclusion criteria were strict and restrictive which may limit the external validity of the study results. However, we intentionally designed them to be restrictive to limit the possibility of inadvertently including patients with appendicitis to the study groups, particularly in the NT group. Eighty-two patients underwent surgery (74 in the LD group and 8 in the NT group) and none of these patients had appendicitis diagnosed intraoperatively and on pathology. There was one patient in the NT group who developed generalized peritonitis required surgical exploration. Intraoperative findings showed a mildly inflamed diverticulum and a normal appendix. The operating surgeon decided to perform appendectomy to avoid future diagnostic uncertainty and left the diverticulum alone in view of minimal inflammation. Patient recovered well under antibiotics coverage and was discharged on postoperative day 1.
This prospective study offers compelling evidence to consider LD as upfront treatment for RCD in appropriate circumstance. Right colonic diverticulitis has significant recurrence rate, between 8 and 20% during follow-up of up to 60 months [8,9,10, 24,25,26], of which 5% to 33% of the recurrent cases have significant complications of perforation, peritonitis, and sepsis that required surgical interventions [9, 10, 25, 26]. This study, with a mean follow-up of 46.4 months, showed a recurrence rate of 16.6%. Two out of nine recurrences required surgical intervention. Furthermore, RCD occurs in relatively younger patient demographic. In this study, the mean age is 35.5 years old. Existing literatures report similar trend of younger patients with RCD, with a mean age of 32.9 to 43.9 years [25,26,27,28]. The NNT to avoid recurrence is nine. Thus, given the good safety profile and lower recurrence rate, LD could be discussed and offered to patients, especially in younger patients, or patients who live in remote, underserved areas, or those with higher risks of recurrence such as multiple diverticula, diverticula not limited to the right colon, and intraperitoneally located peritonitis [10, 25]. Additionally, the risk of disease progression must also be communicated clearly to patients who opted for NT as the risk of disease progression is approximately 10% in patients managed conservatively.
The optimal choice of surgery for RCD remains unclear, especially when RCD is diagnosed intraoperatively. Options range from open to minimally invasive, from diverticulectomy to colonic resection with primary anastomosis. The results from our study add to the existing body of evidence that advocate for laparoscopic diverticulectomy and appendectomy as first-line surgical treatment [7, 13, 14]. Laparoscopic diverticulectomy can be safely performed, without special equipment, in patients whose inflamed diverticulum can be visualized without difficulty. In our surgical group, 10.8% of the patients had minor complications (Clavien-I) and one experienced Clavien-III complication of bowel injury from preventable technical error. There was no mortality in the LD arm. This is consistent with the low complication rate reported in the literature [11, 13, 28, 29]. There were ten conversions to open in our LD group (13.5%), which were mainly due to technical difficulties encountered with severe inflammation, contamination, bowel edema, and dilation. Monari et al. [28] reported a conversion rate of 35.7%, when big abscess or small bowel dilatation was encountered. However, their retrospective series probably included patients with complicated RCD which explained the higher conversion rate. In their subgroup analysis, patients underwent laparoscopic diverticulectomy also had no recurrence after a mean follow-up of 30.6 months [28]. Other retrospective data [15] reported a 92.7 months RCD-free period after surgery with a recurrence rate between 1 and 3% in surgically treated RCD patients [6, 26, 27, 30]. Laparoscopic diverticulectomy is a minimally invasive surgical procedure with low complication rate and a very low recurrence rate when compared to right colectomy [14,15,16, 21]. Given the advantages of low complication and comparable recurrence rate to colonic resection, LD is an attractive surgical treatment for uncomplicated RCD over colectomy [13, 28].
Results from our study suggest that patients who are treated non-operatively should be followed up for longer than 12-month period. In our study, of the nine recurrences in the NT groups, six occurred long after 12 months with the mean recurrence interval of 38 months. In a series of 152 RCD patients managed non-operatively [26], ten patients (6.6%) experienced recurrence within 12 months, four (2.6%) between 24 to 36 months and one (0.7%) at 105 months. Another study from Korea [10] reported a mean recurrence interval of 29 months after the first attack. Despite the difference in the recurrence interval reported in these two Korean studies and this series, all data seem to suggest that most recurrences are amenable to non-operative treatments.
During follow-up after the first episode of RCD, it remains unclear whether a colonoscopy should be offered. In our current practice, we do not offer colonoscopy if the history is not significant for risks of colorectal cancer. Chan and Tan concluded that colonoscopy is not required during follow-up in Asian patients in Singapore less than 50 years of age who are recently diagnosed with diverticulitis [31]. Given that all enrolled patients were under the age of 50 in our study and there was no significant red flag in their history, we did not offer any colonoscopy during the follow-up period. An additional consideration to be made when following up patients who are treated non-operatively is whether elective surgery should be offered to avoid recurrence. This is an interesting topic for future investigations.
A major limitation in our study is the lack of randomization. However, randomization was difficult given the nature of local patient’s preference and belief system. A patient preference randomized control trial could in theory, addresses the issues of patient’s preference; however, it would be difficult, complex, and costly to carry this out in the resource-limited environment where we practice. Furthermore, very often in our setting, patients would, for socioeconomic reasons, change decision about surgery at the last moment, making randomization difficult. We hoped to mitigate the shortcomings of our lack of randomization by offering a large, prospective set of data that were collected over a decent length of longitudinal follow-up to offer new insights on the management of uncomplicated RCDs. Another limitation to our study is that the enrolled population is entirely Vietnamese. Whether the results can be generalized to non-Asian ethnicities remains a topic of future research with our series providing the initial data on the safety and outcome of both non-operative and LD approach. With RCDs being more common in the Asian population, the results of this study can be generalized to other ethnicities that share similar genetic background to Vietnamese such as the Han Chinese, the Koreans, and related ethnicities in the Indochina regions.
In conclusion, for patients with uncomplicated RCD, both LD and NT are good treatment strategies with equivalent profile in safety and efficacy. However, patients managed non-operatively are at higher risks of disease progression and higher recurrence risks than patients treated with LD. Thus, NT with antibiotics and bowel rest could be an initial option for the treatment of uncomplicated RCD if both patients and physicians understand and accept these risks. In contrast, LD is safe and effective in patients who are concerned about disease progression and recurrence.
References
Sardi A, Gokli A, Singer JA (1987) Diverticular disease of the cecum and ascending colon. A review of 881 cases. Am Surg 53:41–45
Jacobs DO (2007) Clinical practice. Diverticulitis. N Engl J Med 357:2057–2066
Manabe N, Haruma K, Nakajima A, Yamada M, Maruyama Y, Gushimiyagi M, Yamamoto T (2015) Characteristics of colonic diverticulitis and factors associated with complications: a Japanese Multicenter, retrospective, cross-sectional study. Dis Colon Rectum 58:1174–1181
Tanase I, Paun S, Stoica B, Negoi I, Gaspar B, Beuran M (2015) Epidemiology of diverticular disease—systematic review of the literature. Chirurgia (Bucur) 110:9–14
Paik PS, Yun JA (2017) Clinical features and factors associated with surgical treatment in patients with complicated colonic diverticulitis. Ann Coloproctol 33:178–183
Komuta K, Yamanaka S, Okada K, Kamohara Y, Ueda T, Makimoto N, Shiogama T, Furui J, Kanematsu T (2004) Toward therapeutic guidelines for patients with acute right colonic diverticulitis. Am J Surg 187:233–237
Yang HR, Huang HH, Wang YC, Hsieh CH, Chung PK, Jeng LB, Chen RJ (2006) Management of right colon diverticulitis: a 10-year experience. World J Surg 30:1929–1934
Kim MR, Kye BH, Kim HJ, Cho HM, Oh ST, Kim JG (2010) Treatment of right colonic diverticulitis: the role of nonoperative treatment. J Korean Soc Coloproctol 26:402–406
Tan KK, Wong J, Sim R (2013) Non-operative treatment of right-sided colonic diverticulitis has good long-term outcome: a review of 226 patients. Int J Colorectal Dis 28:849–854
Park HC, Kim BS, Lee K, Kim MJ, Lee BH (2014) Risk factors for recurrence of right colonic uncomplicated diverticulitis after first attack. Int J Colorectal Dis 29:1217–1222
Lane JS, Sarkar R, Schmit PJ, Chandler CF, Thompson JE Jr (1999) Surgical approach to cecal diverticulitis. J Am Coll Surg 188:629–634 discussion 634–635
Fang JF, Chen RJ, Lin BC, Hsu YB, Kao JL, Chen MF (2003) Aggressive resection is indicated for cecal diverticulitis. Am J Surg 185:135–140
Papaziogas B, Makris J, Koutelidakis I, Paraskevas G, Oikonomou B, Papadopoulos E, Atmatzidis K (2005) Surgical management of cecal diverticulitis: is diverticulectomy enough? Int J Colorectal Dis 20:24–27
Lee IK, Kim SH, Lee YS, Kim HJ, Lee SK, Kang WK, Ahn CH, Oh ST, Jeon HM, Kim J-G (2007) Diverticulitis of the right colon: tips for preoperative diagnosis and treatment strategy. J Korean Soc Coloproctol 23:223–231
Lee IK, Lee YS, Kim SJ, Gorden DL, Won DY, Kim HJ, Cho HM, Jeon HM, Kim JG, Oh ST (2010) Laparoscopic and open surgery for right colonic diverticulitis. Am Surg 76:486–491
Kwon JW, Kim BS, Park HC, Oh HK, Shin R, Ryoo SB, Park KJ, Lee BH (2012) Surgical treatment of complicated right colonic diverticulitis: laparoscopic versus open surgery. Surg Endosc 26:2926–2930
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Core Team R (2017) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Shyung L-R, Lin S-C, Shih S-C, Kao C-R, Chou S-Y (2003) Decision making in right-sided diverticulitis. World J Gastroenterol 9:606
Alvarado A (1986) A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med 15:557–564
Lee IK (2010) Right colonic diverticulitis. J Korean Soc Coloproctol 26:241–245
Cole M, Ayantunde AA, Payne J (2009) Caecal diverticulitis presenting as acute appendicitis: a case report. World J Emerg Surg 4:29
Chou Y-H, Chiou H-J, Tiu C-M, Chen J-D, Hsu C-C, Lee C-H, Lui W-Y, Hung G-S, Yu C (2001) Sonography of acute right side colonic diverticulitis. Am J Surg 181:122–127
Kim TJ, Lee IK, Park JK, Lee YS, Si Y, Jung H, Kim HJ, Lee SC, Cheung DY, Gorden LD, Oh ST (2011) Is conservative treatment with antibiotics the correct strategy for management of right colonic diverticulitis?: a prospective study. J Korean Soc Coloproctol 27:188–193
Park SM, Kwon TS, Kim DJ, Lee YS, Cheung DY, Oh ST, Kim JG, Lee IK (2014) Prediction and management of recurrent right colon diverticulitis. Int J Colorectal Dis 29:1355–1360
Ha GW, Lee MR, Kim JH (2017) Efficacy of conservative management in patients with right colonic diverticulitis. ANZ J Surg 87:467–470
Lee IK, Jung SE, Gorden DL, Lee YS, Jung DY, Oh ST, Kim JG, Jeon HM, Chang SK (2008) The diagnostic criteria for right colonic diverticulitis: prospective evaluation of 100 patients. Int J Colorectal Dis 23:1151–1157
Monari F, Cervellera M, Pirrera B, D’Errico U, Vaccari S, Alberici L, Tonini V (2017) Right-sided acute diverticulitis: a single Western center experience. Int J Surg 44:128–131
Hildebrand P, Kropp M, Stellmacher F, Roblick UJ, Bruch HP, Schwandner O (2007) Surgery for right-sided colonic diverticulitis: results of a 10-year-observation period. Langenbecks Arch Surg 392:143–147
Park HC, Kim BS, Lee BH (2011) Management of right colonic uncomplicated diverticulitis: outpatient versus inpatient management. World J Surg 35:1118–1122
Chan DKH, Tan KK (2017) There is no role for colonoscopy after diverticulitis among Asian patients less than 50 years of age. Gastrointest Tumors 3:136–140
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Le Huy Luu, Dr. Nguyen Lam Vuong, Dr. Vo Thi Hong Yen, Dr. Do Thi Thu Phuong, Dr. Bui Khac Vu, Dr. Nguyen Viet Thanh, Dr. Nguyen Thien Khanh, and Dr. Nguyen Van Hai have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luu, L.H., Vuong, N.L., Yen, V.T.H. et al. Laparoscopic diverticulectomy versus non-operative treatment for uncomplicated right colonic diverticulitis. Surg Endosc 34, 2019–2027 (2020). https://doi.org/10.1007/s00464-019-06981-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06981-x