Abstract
Purpose
Most patients with acute right colonic uncomplicated diverticulitis can be managed conservatively. The aim of this study was to assess the clinical and radiologic risk factors for recurrence in patients with right colonic uncomplicated diverticulitis.
Methods
The present survey included 469 patients who were successfully managed conservatively for the first episode of right colonic uncomplicated diverticulitis between 2002 and 2012 in a referral center, and records were reviewed from collected data. Patients were divided into two groups: a nonrecurrent and a recurrent group. The clinical and radiologic features of all patients were analyzed to identify possible risk factors for recurrence. The Kaplan-Meier method and Cox regression were used.
Results
Seventy-four (15.8 %) patients had recurrence, and 15 (3.2 %) received surgery at recurrence within a median follow-up of 59 months. The mean recurrence interval after the first attack was 29 months. In univariate and multivariate analyses, risk factors for recurrence were confirmed multiple diverticula (relative risk [RR], 2.62; 95 % confidence interval [CI], 1.56–4.40) and intraperitoneally located diverticulitis (RR, 3.73; 95 % CI, 2.13–6.52). Of 66 patients with two risk factors, 36 (54.5 %) had recurrence and 10 (15.2 %) received surgery at recurrence.
Conclusions
In patients with right colonic uncomplicated diverticulitis who have multiple diverticula and intraperitoneally located diverticulitis, the possibility of recurrence and surgical rate are high. Poor outcome may be cautioned in these patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Right colonic diverticulitis is more common in Eastern than in Western countries [1]. Previously, the diagnosis of right colonic diverticulitis was difficult to ascertain because its symptoms are similar to those of acute appendicitis [2]. With the addition of radiologic evaluations, diverticulitis can be definitively diagnosed [3, 4]. Current medical treatment strategies are effective for the treatment of acute right colonic uncomplicated diverticulitis [5–8].
The recurrence rate after conservative management for right colonic uncomplicated diverticulitis varies among studies (approximately 7.1–20.5 %) [7, 9, 10]. The causes of recurrence are not yet understood. The aims of this study were to investigate the risk factors for recurrence after conservative treatment and to predict recurrence in patients with acute right colonic uncomplicated diverticulitis.
Methods
Patients
After obtaining approval from our institutional review board, we reviewed 505 patients diagnosed with acute right colonic diverticulitis at the time of first attack from prospective collected data between 2002 and 2012. The most common symptom was right lower quadrant pain or whole abdominal pain, except hematochezia (seven patients) and diarrhea (two patients).
The diagnosis was performed by computed tomography (CT) and/or ultrasonography (USG). After treatment, patients underwent colonoscopy, colon study, or 3-dimensional (3D) colon CT to determine the disease state and confirm the diagnosis.
Twenty-eight patients were managed initially by surgery (N = 25) or percutaneous drainage (N = 3) for complicated diverticulitis. Eight patients showed resistance to conservative treatment and underwent subsequent surgery. These patients were excluded from the study.
We enrolled the remaining 469 patients who were diagnosed with uncomplicated diverticulitis and managed successfully by conservative treatment.
The conservative management comprised antibiotic therapy and/or bowel rest until symptoms were relieved. We divided the patients into two groups, a nonrecurrent and a recurrent group, and analyzed the data regarding the clinical and radiologic features of all patients.
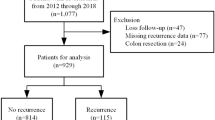
Patients were reviewed by examining their medical charts and by telephone interview to identify recurrence with a median follow-up time of 59 months (Fig. 1). The recurrence of diverticulitis was defined as the presence of repeated symptoms confirmed by radiologic evaluations. If a patient had the same symptoms as those of first attack but did not have available radiologic evidence, the patient was considered to have nonrecurrence and was censored statistically because of the possibility of other diseases, such as colitis or lymphadenopathy. If the radiologic evaluation showed a different location than that observed the first time, the patient was not considered to have recurrence. The patient should have had interval no abdominal symptoms without analgesics or antibiotics for at least 1 month after the first episode to be considered to have recurrence.
Radiologic evaluations
All patients received radiologic evaluations. CT was performed in 302 patients (64.4 %) and USG in 124 (26.4 %). The indeterminate 43 patients underwent both examinations. Radiologic scan data were available on a PACS (INFINITT Technology, Seoul, Korea), and all images were reviewed at a PACS monitor. All examinations were reinterpreted retrospectively by an experienced abdominal radiologist without knowledge of the clinical information. Ambiguous radiologic findings were additionally interpreted by a senior abdominal radiologist.
Uncomplicated diverticulitis was defined by the presence of an inflamed diverticulum, localized colonic wall thickening, inflammation of the subserosa, and edema of the mesentery. The inflamed diverticulum occasionally contained a fecalith. We considered small-sized (less than 3 cm) pericolic abscesses as uncomplicated because most patients presenting with this disease entity can be treated conservatively.
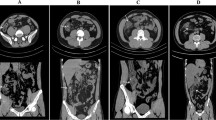
The location of the diverticulitis (i.e., cecum and ascending colon, intraperitoneal, and retroperitoneal) and the number of diverticula (i.e., solitary and multiple) were evaluated based on radiologic findings. We assessed the location of the diverticulitis as intraperitoneal or retroperitoneal considering the protrusion direction of the diverticulitis. When the diverticulitis was located above the vasa recta vessel within the mesentery and above the peritoneal reflection on the lateral side of the colon, it was considered as intraperitoneal. By contrast, when the diverticulitis was located below the vasa recta within the mesentery and below the peritoneal reflection, it was considered retroperitoneal (Fig. 2). The number of diverticula was also determined based on the radiologic findings. When diverticula, including diverticulitis, were only observed once, it was considered solitary. When multiple diverticula were observed, except for the main diverticula causing diverticulitis, it was considered multiple (diverticulosis). When the patient presented with multiple inflamed diverticula, the location of diverticulitis was assigned based on the most severe inflamed diverticulum. Diverticulitis was considered to be located in the cecum or the ascending colon on the basis of its location relative to the ileocecal (IC) valve.
Statistical analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences software (SPSS Inc., version 12.0 for Windows). The cross table chi-square test, Fisher’s exact test, and independent t test were used. The Cox proportional hazards models were used for the multivariate analysis of variables predicting recurrence. Hazard ratios with 95 % confidence intervals are presented. A value of P < 0.05 was considered statistically significant.
Results
A total of 469 patients (269 men and 200 women) were enrolled in this study. The mean age at the onset of right colonic diverticulitis was 38.7 ± 11.7 years (range, 18–77). Diverticulitis was more often located in the ascending colon (61.2 %) than in the cecum (38.8 %). Ninety-three (19.8 %) patients had suspected perforation or abscess formation as determined by radiologic studies.
Mean hospital stay and length of antibiotic use were 6.1 ± 3.1 and 5.8 ± 2.1 days, respectively. Mean body temperature at admission was 37.1 ± 0.5 °C, and only 40 patients (8.5 %) had a temperature higher than 38 °C.
Mean white blood cell (WBC) count at admission was 11.2 ± 3.5 (103/μL), mean percentage of neutrophil count was 73.1 ± 9 (%), and C-reactive protein was 55.7 ± 41.2 (mg/L).
Of the patients included, 33 had comorbidities—14 had heart disease, 7 had endocrine diseases, 6 had cerebrovascular diseases, 3 had malignancies, 2 had liver cirrhosis, and 1 had multiple sclerosis. Twenty-seven patients had a history of previous operation, which was mostly appendectomy.
According to the radiologic findings, the diverticulitis lesion was located intraperitoneally in 221 (47.1 %) patients and retroperitoneally in 248 (52.9 %) patients. Bowel wall thickening and fecalith were present in 295 (62.9 %) and 113 (24.1 %) patients, respectively. Solitary diverticulum was detected in 304 patients (64.8 %) and multiple diverticula in 165 (35.2 %) patients.
Follow-up colonoscopy and colon study reports were available for 181 and 27 patients. There were 76 patients who had no evidence of diverticulum or diverticulitis. Of these, 69 were diagnosed with solitary diverticulum, whereas 7 with multiple diverticula in the initial radiologic scan. Twenty-nine (16 %) patients had incidental findings of adenomatous polyp, and there was no patient with diagnosis of colorectal cancer on colonoscopy.
The median follow-up time was 59 months (range, 8–145 months). Of the 469 patients, 74 (15.8 %) had recurrence during this period. Five patients had more than three attacks. The mean recurrence interval after the first attack was 29 months.
Four patients complained of recurrent right abdominal pain during the follow-up period after recovery of diverticulitis, although no radiologic evidence was obtained. Two patients developed diverticulitis at different sites in the first and second attacks; these patients were excluded from the recurrent group.
Most of the 74 recurrent patients were treated conservatively again, although 15 underwent surgery for complicated disease or resistance to therapy and 2 received percutaneous drainage.
The recurrent group showed a higher frequency of multiple diverticula and intraperitoneally located diverticulitis than the nonrecurrent group (P < 0.001). The clinical and laboratory findings of the two groups were not significantly different. No significant differences in the presence of an abscess or perforation were observed between the recurrent and nonrecurrent groups. The presence of fecalith and adjacent bowel wall thickening were also not significantly different (Table 1).
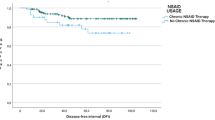
Multivariate analysis using the Cox proportional hazards model showed that multiple diverticula and intraperitoneally located diverticulitis were significantly related to an increased risk of recurrence (Table 2).
There were 66 patients with intraperitoneally multiple diverticula on the initial radiologic scan. They had 36 recurrent episodes (54.5 %). Of these, ten (15.2 %) received surgery for complicated disease or resistance to antibiotic therapy.
Discussion
Uncomplicated diverticulitis is currently managed conservatively. Even in cases of complicated diverticulitis with abscesses, percutaneous drainage without operation is a useful management strategy [11]. Most patients with right colonic diverticulitis can be successfully managed with conservative therapy. However, the management of recurrent right colonic diverticulitis remains controversial. Studies have shown that uncomplicated recurrent right colonic diverticulitis can be managed conservatively without surgery [6–8]. Weizman et al. reported that surgical management may be required for patients with recurrent diverticulitis [12]. If the risk factors of recurrence are known, patients with high risk factors can be closely followed up and recurrence may be detected earlier.
We analyzed patients with uncomplicated diverticulitis at the first attack, which was confirmed by radiologic studies and treated successfully by conservative therapy.
Although the right colon is a retroperitoneal organ, we determined the direction of diverticulitis by analyzing the protrusion. Inflamed tissues show as enhanced and infiltrated on radiologic imaging. Although the normal peritoneum cannot be observed clearly by radiologic imaging, the peritoneum around the inflammatory tissue can be detected [13, 14]. Therefore, we were able to determine the location of the lateral peritoneal reflection. On the medial aspect, the vasa recta vessel was enhanced by inflamed tissue. The mesentery includes the vasa recta vessel and, therefore, serves as an indicator of the mesentery. Strictly speaking, the retroperitoneum is posterior to the mesenteric membrane. However, when diverticulitis is located in the boundary of the mesentery, it is unclear whether it is retroperitoneal or intraperitoneal because the site of diverticulitis is edematous and shows a deviated anatomy. In these cases, the vasa recta vessel can be used as a landmark for the detection of the mesentery.
Our results showed that diverticulosis is a risk factor for recurrence. The etiological and pathological differences between solitary and multiple diverticula are controversial. Some reports indicated that solitary diverticulum in the right colon is congenital in origin and a true type in terms of pathology and that multiple diverticula is acquired and a false type [15, 16]. In contrast, Lee reported that solitary and multiple diverticula were variations of the same disease [17]. Other reports suggested that right colonic diverticulitis in Mongolian people was related to consuming a Western-style diet regardless of the number of diverticula [18, 19]. Floch et al. suggested that fiber deficiency increased intracolonic pressure, led to diverticula formation, and caused a change in the microecology that preceded diverticulitis [20]. Therefore, patients with multiple diverticula may have a stronger propensity for diverticula formation than patients with a solitary diverticulum and may be at high risk for inflammation.
Although there was typical feature of diverticulitis from solitary diverticulum on radiologic finding, the disease evidence may not be detected by follow-up colonoscopy. There is a potential possibility of spontaneous resolution or missing tiny lesion.
Our results showed that intraperitoneally located diverticulitis was a risk factor for recurrence. Diverticulitis can include intraperitoneally located or retroperitoneally located lesions. The retroperitoneum is thought to be a barrier against intracolonic pressure; however, no studies have addressed the tissue pressure in the intra- and retroperitoneal space. Another hypothesis was the possibility of a missed diagnosis or spontaneous resolution of the recurred retroperitoneal diverticulitis. Some reports have indicated that the presenting symptoms of a retroperitoneal abscess are often insidious, and focal physical findings might be subtle [21, 22]. These factors often result in a hidden recurrence. The recurrence of retroperitoneally located diverticulitis may go unnoticed if the inflammation is mild. Mild diverticulitis can improve without bowel rest or admission [23–25]. If the condition of a patient with recurrence improves spontaneously without admission or a radiologic evaluation, the recurrence may remain undetected and insignificant clinically.
When we analyzed 66 patients with both risk factors, we observed high recurrence rate and surgical rate at recurrence. They had a tendency to resist antibiotic therapy. In operative findings, we revealed bowel wall thickening with extensive phlegmon including microabscesses in most patients.
Hall et al. reported that family history, a long segment of involved colon, and the presence of retroperitoneal abscesses were associated with recurrence in mainly left colonic diverticulitis [26]. We suggest that the predictive factors of recurrence in right colonic diverticulitis are different from those of left colonic disease.
Despite some limitations related to the retrospective design, this study provides valuable information because of the long-term follow-up and substantial materials.
In conclusion, after successful conservative treatment for right colonic uncomplicated diverticulitis, the presence of multiple diverticula and intraperitoneally located diverticulitis were identified as risk factors for recurrence, and the appropriate treatment strategy should be needed in patients with poor outcome.
References
Kim JH, Cheon JH, Park S, Kim BC, Lee SK, Kim TI et al (2008) Relationship between disease location and age, obesity, and complications in Korean patients with acute diverticulitis: a comparison of clinical patterns with those of Western populations. Hepatogastroenterology 55:983–986
Shin JH, Son BH, Kim H (2007) Clinically distinguishing between appendicitis and right-sided colonic diverticulitis at initial presentation. Yonsei Med J 48:511–516
Lawrimore T, Rhea JT (2004) Computed tomography evaluation of diverticulitis. J Intensive Care Med 19:194–204
Rotert H, Nöldge G, Encke J, Richter GM, Dux M (2003) The value of CT for the diagnosis of acute diverticulitis. Radiologe 43:51–58
Shyung LR, Lin SC, Shih SC, Kao CR, Chou SY (2003) Decision making in right-sided diverticulitis. World J Gastroenterol 9:606–608
Komuta K, Yamanaka S, Okada K, Kamohara Y, Ueda T, Makimoto N et al (2004) Toward therapeutic guidelines for patients with acute right colonic diverticulitis. Am J Surg 187:233–237
Yang HR, Huang HH, Wang YC, Hsieh CH, Chung PK, Jeng LB et al (2006) Management of right colon diverticulitis: a 10-year experience. World J Surg 30:1929–1934
Kim TJ, Lee IK, Park JK, Lee YS, Si Y, Jung H et al (2011) Is conservative treatment with antibiotics the correct strategy for management of right colonic diverticulitis?: a prospective study. J Korean Soc Coloproctol 27:188–193
Lee IK, Kim SH, Lee YS, Kim HJ, Lee SK, Kang WK et al (2007) Diverticulitis of the right colon: tips of preoperative diagnosis and treatment strategy. J Koeran Soc Coloproctol 23:223–231
Matsushima K (2010) Management of right-sided diverticulitis: a retrospective review from a hospital in Japan. Surg Today 40:321–325
Durmishi Y, Gervaz P, Brandt D, Bucher P, Platon A, Morel P et al (2006) Results from percutaneous drainage of Hinchey stage II diverticulitis guided by computed tomography scan. Surg Endosc 20:1129–1133
Weizman AV, Nguyen GC (2011) Diverticular disease: epidemiology and management. Can J Gastroenterol 25:385–389
Filippone A, Cianci R, Di Fabio F, Storto ML (2011) Misty mesentery: a pictorial review of multidetector-row CT findings. Radiol Med 116:351–365
DeMeo JH, Fulcher AS, Austin RF Jr (1995) Anatomic CT demonstration of the peritoneal spaces, ligaments, and mesenteries: normal and pathologic processes. Radiographics 15:755–770
Vajrabukka T, Saksornchai K, Jimakorn P (1980) Diverticular disease of the colon in a far-eastern community. Dis Colon Rectum 23:151–154
Radhi JM, Ramsay JA, Boutross-Tadross O (2011) Diverticular disease of the right colon. BMC Res Notes 4:383. doi:10.1186/1756-0500-4-383
Lee YS (1986) Diverticular disease of the large bowel in Singapore. An autopsy survey. Dis Colon Rectum 29:330–335
Lin OS, Soon MS, Wu SS, Chen YY, Hwang KL, Triadafilopoulos G (2000) Dietary habits and right-sided colonic diverticulosis. Dis Colon Rectum 43:1412–1418
Nakaji S, Danjo K, Munakata A, Sugawara K, MacAuley D, Kernohan G et al (2002) Comparison of etiology of right-sided diverticula in Japan with that of left-sided diverticula in the West. Int J Colorectal Dis 17:365–373
Floch MH, Bina I (2004) The natural history of diverticulitis: fact and theory. J Clin Gastroenterol 38:S2–7
Edwards JD, Eckhauser FE (1986) Retroperitoneal perforation of the appendix presenting as subcutaneous emphysema of the thigh. Dis Colon Rectum 29:456–458
Tunuguntla A, Raza R, Hudgins L (2004) Diagnostic and therapeutic difficulties in retroperitoneal abscess. South Med J 97:1107–1109
Etzioni DA, Chiu VY, Cannom RR, Burchette RJ, Haigh PI, Abbas MA (2010) Outpatient treatment of acute diverticulitis: rates and predictors of failure. Dis Colon Rectum 53:861–865
Park HC, Kim BS, Lee BH (2011) Management of right colonic uncomplicated diverticulitis: outpatient versus inpatient management. World J Surg 35:1118–1122
Biondo S, Lopez Borao J, Millan M, Kreisler E, Jaurrieta E (2012) Current status of the treatment of acute colonic diverticulitis: a systematic review. Colorectal Dis 14:e1–e11. doi:10.1111/j.1463-1318.2011.02766.x
Hall JF, Roberts PL, Ricciardi R, Read T, Scheirey C, Wald C et al (2011) Long-term follow-up after an initial episode of diverticulitis: what are the predictors of recurrence? Dis Colon Rectum 54:283–288
Conflict of interest
This paper is not supported by any grant, funding source, or commercial interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Park, HC., Kim, B.S., Lee, K. et al. Risk factors for recurrence of right colonic uncomplicated diverticulitis after first attack. Int J Colorectal Dis 29, 1217–1222 (2014). https://doi.org/10.1007/s00384-014-1941-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-014-1941-8