Abstract
Background
Laparoscopic liver resection (LLR) has evolved over time, yet its role in extra-pancreatic biliary cancer has been limited due to several factors. We aimed to evaluate the short-term outcome of LLR in extra-pancreatic biliary tract cancer.
Methods
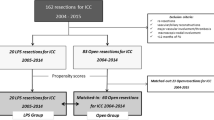
From January 2002 to 2016, all patients who underwent LLR for extra-pancreatic biliary tract cancer including gallbladder cancer (GBC), intra-hepatic cholangiocarcinoma (ICC), and peri-hilar cholangiocarcinoma (PHC) with curative intent (R0 or R1) at Institute Mutualiste Montsouris were identified from prospectively collected databases. Patient characteristics, and perioperative outcomes, were analyzed in all three groups.
Results
A total of 35 patients were included: 10 with GBC, 14 with ICC, and 11 with PHC. There were 19 (54%) women and median age was 71 years. Median operative time was 240 min, and estimated blood loss was 200 ml. Conversion to an open procedure was more common in patients with PHC (45% vs. 7% for ICC and 0% for GBC, p = 0.010). R0 resection was achieved in 10 (100%), 12 (86%), and 8 (73%) patients in GBC, ICC, and PHC groups, respectively (p = 0.204). Postoperative morbidity was reported in 19 (54%) patients of whom 12 (34%) had minor complications. Postoperative mortality was reported in 4 (11%) patients; one (7%) in GBC group, one (7%) in ICC group, and two (18%) in PHC, p = 0.681. Median hospital stay was 11 days.
Conclusions
The present series suggests that LLR is feasible in GBC, challenging but achievable in ICC but unsuitable for the moment in PHC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic liver resection (LLR) has developed markedly over the last two decades, and its indications have expanded to the management of most liver tumors. However, adoption of the minimally invasive approach in biliary tract cancer has been slower due to technical challenges specific to each type of biliary cancer [1].
LLR for gallbladder cancer (GBC) is technically feasible in terms of the limited liver resection required; the distance of the tumor is far from the important hilar structures and the rare requirement of complex biliary and vascular reconstructions [2]. However, the initial reports in late 1990s about port site recurrence made suspected GBC a contraindication to laparoscopic cholecystectomy and contributed to the late introduction of LLR in management of GBC [3]. Recently, several studies have demonstrated the safety of the minimally invasive approach in GBC but more data are needed to have better view of the long-term outcome [2,3,4,5]. Intrahepatic cholangiocarcinoma (ICC) is not well presented in the LLR studies, representing only 5 to 7% of laparoscopic resections in the largest published series [1, 6]. This is related to the major or extended liver resections required in addition to lymphadenectomy and the frequent need for vascular and/or biliary reconstructions [1, 6, 7]. Finally, peri-hilar cholangiocarcinoma (PHC) was the last to be adopted by the minimal invasive approach due to complexity of the procedure, including the requirement for extended liver resection, lymphadenectomy, biliary-enteric reconstruction in addition to dissection of tumors from the vascular structures within the portal triad to achieve R0 resection [4]. Published data about the minimally invasive approach in PHC are limited to a few reports with small number of patients [4, 8].
A preliminary report of three centers experienced in minimally invasive surgery, including ours, presented their experience in LLR of extra-pancreatic cholangiocarcinoma focusing on the surgical procedures and technical aspects [4]. The report demonstrated the safety and feasibility of the minimal invasive approach in extra-pancreatic cholangiocarcinoma [4]. However, impact of LLR on the short-term outcomes is not clear.
Given this uncertainty, the present study aimed to evaluate the role of LLR in management of extra-pancreatic biliary cancer (including GBC, ICC, and PHC), with emphasis on short-term outcomes.
Patients and methods
Study population
From January 2002 to 2016, all patients who underwent LLR for extra-pancreatic biliary tract cancer (GBC, ICC and PHC) with curative intent (R0 or R1) at Institute Mutualiste Montsouris were identified. Patients with distal cholangiocarcinoma who underwent Whipple’s procedure were excluded.
Patients who required conversion to laparotomy were included and analyzed with intention-to-treat. Follow-up was updated to July 2017. Data were retrospectively retrieved from a prospectively maintained database. The data included demographic variables, primary tumor characteristics and management, operative data, tumor pathology and short- and long-term outcomes. Patients were compared according to type of extra-pancreatic biliary tract cancer. This study was approved by the institutional review board and conducted in accordance with the Declaration of Helsinki.
Preoperative evaluation
All patients had routine laboratory testing, including complete blood count, liver and kidney function tests, coagulation profile, serum electrolytes and tumor markers (CA-19-9). Magnetic resonance cholangiopancreatography (MRCP) was used in all patients to assess the extent of liver disease and to determine the resection planes. Tri-phasic abdominal CT scan was used to assess vascular invasion, and three-dimensional reconstruction was obtained in complex surgeries for planning. Resectability of peri-hilar cholangiocarcinoma was determined by Blumgart staging system [9]. Chest and abdominal CT scan was used to rule out metastasis, as well as PET-CT if metastasis suspicion was high. The decision for hepatectomy was taken by a multidisciplinary board that included surgeons, medical oncologists and radiologists.
Surgical procedures
Operative procedures, including positioning of trocars, were as previously described [4, 7, 10, 11]. Liver resectability was always confirmed by intraoperative ultrasonography. Major hepatectomy was defined as the resection of three or more contiguous segments [6]. For all procedures, tissue dissection and hemostasis were performed using the Thunderbeat® ultrasonic dissector (Olympus Co, Tokyo, Japan); bipolar forceps (MicroFrance CEV134, Medtronic, Minneapolis, MN) provided retraction and rescue hemostasis.
Postoperative outcomes
Post-hepatectomy morbidity and mortality were assessed at 90 days after surgery using Clavien–Dindo classification [12]. Severe postoperative complications were defined as Clavien–Dindo grade > 2. Postoperative hepatocellular insufficiency was diagnosed using the “50–50” criteria on postoperative day 5 [13]. Bile leakage was defined as bilirubin concentration in the drain fluid at least 3 times the serum bilirubin concentration on or after postoperative day 3 or as the need for radiologic or operative intervention resulting from biliary collections or bile peritonitis, according to the International Study Group of Liver Surgery [14]. Ascites was defined as abdominal drainage output of more than 10 ml per kg per day after the third postoperative day [15].
Statistical analysis
Baseline characteristics of the studied population, intraoperative and pathological characteristics as well as postoperative outcome were analyzed. Categorical variables were compared using the χ2 test or Fischer’s exact test when appropriate. A p value of < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS version 20.0 (SPSS Inc., Chicago, IL), and statistical significance was accepted at the 0.05 level.
Results
Preoperative patient characteristics and surgical procedure
A total of 35 patients were included in this study: 10 with GBC, 14 with ICC, and 11 with PHC. There were 16 (46%) men, and median age was 71 years (range 41 to 86 years). Preoperative base characteristics were similar between the three groups. Patients with PHC were significantly more likely to have undergone preoperative biliary drainage procedures, to have major hepatectomy with caudate lobe resection and to require vascular resection and biliary reconstruction compared with patients who presented with ICC or GBC. Preoperative and intraoperative characteristics are detailed in Table 1.
Surgical details and perioperative outcomes
Median operative time was 240 min; it was significantly longer in PHC group (355 min) compared with ICC (205 min) and GBC (180 min) groups (p = 0.016). Median estimated blood loss was 200 ml, and 5 (14%) patients had more than 500 ml blood loss. Five (14%) patients required blood transfusion with no significant difference between groups (Table 1).
Conversion to an open procedure was more common in patients with PHC (45% versus 7% for ICC and 0% for GBC) (p= 0.010). A total of 6 patients were converted to open surgery: one patient with ICC was converted to control bleeding from the inferior vena cava and suture a bile leak in the posterior pedicle and 5 patients with PHC due to unclear anatomy (n = 1), unclear resectability status (n = 2), and revision of a biliary anastomosis (n = 2). None of the patients with GBC required conversion to open surgery. Median tumor diameter was 68 mm, and PHC lesions were significantly smaller in size compared to ICC and GBC lesions (p < 0.039). Median retrieved lymph nodes in GBC, ICC, and PHC groups were 6, 3, and 9, respectively (p = 0.467). The number of lymph nodes retrieved was not significantly different between groups, nor was AJCC stage. R0 resection was achieved in 10 (100%), 12 (86%), and 8 (73%) patients in GBC, ICC, and PHC groups, respectively with no significant difference among all groups (p = 0.204).
As detailed in Table 2, 19 (54%) patients presented with postoperative complications of whom 12 (34%) developed minor complications (Clavien-Dindo grade ≤ 2) within the 90 postoperative days. Patients with GBC presented with less postoperative complications compared with ICC and PHC patients (p = 0.022). Bile leak, liver failure, and kidney injury rates were similar between groups (p > 0.05). Postoperative mortality rate was 11% (n = 4); one (7%) patient in GBC group died due to pulmonary embolism, one (7%) patient in ICC group due to sepsis and multi-organ failure, and two (18%) patients in PHC due to liver failure (n = 1) and biliary peritonitis (n = 1), with no significant difference between the 3 groups (p = 0.681). Median hospital stay was 11 days, and it was significantly longer for patients with PHC (21 days) compared with GBC patients (8 days) and ICC group (10 days) (p = 0.028).
Discussion
Biliary tract cancers are rare tumors arising from the lining epithelium of bile ducts and include gallbladder cancer, intra-hepatic cholangiocarcinoma, peri-hilar cholangiocarcinoma and distal cholangiocarcinoma [16]. All these different types of biliary cancers share the same poor prognosis, and surgical resection offers the best chance for potential cure. However, only 5–10% of patients are surgical candidates as these tumors tend to metastasize to lymph nodes, invade vascular structures, and present with distant metastases at the time of diagnosis [16].
While surgical procedures are well standardized via the open approach, published data about the minimally invasive approach for biliary cancer are limited to few reports with a restricted number of patients. The present series provides an update on our experience with LLR for extra-pancreatic cholangiocarcinoma. This study analyzes the postoperative outcomes after LLR in 10, 14, and 11 patients with GBC, ICC, and PHC, respectively. The present series shows satisfactory results in terms of blood loss, blood transfusion, and operative time in addition to acceptable morbidity and mortality rates.
GBC is a rare tumor and most often discovered incidentally after cholecystectomy performed for supposedly benign etiology [3]. For stages T1b or higher GBC, radical cholecystectomy including wedge resection or 4b-5 bi-segmentectomy with loco-regional lymphadenectomy is the only potential curative option for early disease [2]. Until recently, the minimally invasive approach was not recommended due to the reported port site recurrence in patients with incidental GBC after laparoscopic cholecystectomy [17, 18]. Interestingly, the present study did not observe any port-site recurrence and we think that surgical manipulation and gallbladder perforation probably contributed to the large number of port site recurrences previously seen. The current results are in accordance with those reported by the largest series to date, published by Agarwal et al. [2]. In this series, 24 patients who had LLR for GBC were compared to 46 patients who underwent open radical cholecystectomy after matching. The 24 patients had successful R0 resection with median blood loss of 200 ml, median lymph node yield of 10 nodes, 12.5% complications rate and none of the patients developed recurrence at port sites. In another report, Castro et al. [3], described 18 patients with GBC who had LLR with median blood loss of 125 ml, no conversion to open surgery and all patients had R0 resection, median lymph node yield of 6 with a complication rate of 11% and no port site recurrence.. In the present series, 10 patients with GBC underwent successful LLR without conversion to open surgery. Median blood loss was 110 ml; all patients had an R0 resection with a median lymph node yield of 10, minor complications in two patients, and postoperative mortality in one patient.
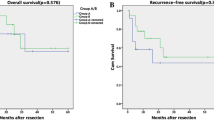
Intra-hepatic cholangiocarcinoma generally requires major liver resection with formal lymphadenectomy, and in some cases vascular or biliary reconstructions, which explains the limited diffusion of laparoscopic approach [6]. A recently published review article [19] of LLR for ICC showed that only 101 (5.5%) patients with ICC were treated with laparoscopic approach out of 1882 patients in 11 studies. Therefore, scarce information is available about outcome of LLR in ICC. One of the largest series [20] included 20 patients who were treated by laparoscopy, and these patients were matched to 60 patients who had open surgery. In LLR group, R0 resection was achieved in all patients, 19 patients were managed by laparoscopy and only one patient (5%) was converted to open surgery with less blood loss compared to open surgery. The complication rate was 15%, and most of these complications were minor with no postoperative mortality. The second largest study on LLR for ICC was published by Lee et al. [21] and compared 14 patients who underwent LLR to 23 patients who had open surgery. Patients in LLR group had less blood loss and shorter hospital stay. The authors did not observe any difference between both groups regarding complications, tumor recurrence and patient survival. In our cohort, 14 patients with ICC were managed by laparoscopy with median blood loss of 200 ml, and only one patient (7%) was converted to open surgery. R0 resection was achieved in 86% of cases, and major liver resections and formal lymphadenectomy were performed in 71% of cases. Again, half of these patients had minor complications and one (7%) patient died postoperatively due to sepsis and multi-organ failure. In terms of postoperative morbidity, the current results show a higher rate of postoperative complications compared with other published reports. In particular, in the study published by Ratti et al. [20] major liver resection was performed in 85% of cases and lymphadenectomy was done in only half of patients and in the study published by Lee et al. [21] half of patients had minor resections and formal lymphadenectomy was done in 36% of cases.
Peri-hilar cholangiocarcinoma or Klatskin tumor was the last to be considered for the laparoscopic approach due to the complexity of the procedure. Curative-intent surgery requires major hepatectomy, including the caudate lobe, radical lymphadenectomy, bile duct resection/reconstruction, and in some cases vascular resection. In the literature, there are 8 studies with a total of 32 cases (including our previous report) of PHC that were managed laparoscopically [8]. The largest study [22] includes 14 patients diagnosed with PHC, and in that study most of the patients underwent local hilar resection and biliary reconstruction only, without performing the standard management as described above.
To the best of our knowledge, this cohort of 11 patients who had LLR for PHC represents the largest series from a single institution to date. Most patients had major hepatectomy with biliary reconstruction; vascular and pancreatic resections were performed due to tumor extension in 6 cases with a median blood loss of 250 ml and 5 patients required conversion to open surgery. R0 resection was achieved in 73% of cases, and postoperative morbidity rate was 64% (n = 7 patients) mostly including minor complications. Postoperative mortality rate was 18% (n = 2 patients). Despite high postoperative mortality rate observed in the present series, this rate in literature ranges from 4 to 18% after open surgery for PHC [23,24,25]. Short-term outcomes seem similar to those reported following an open approach, although postoperative mortality rate (18%) should be carefully interpreted considering the small number of patients included. There are no large series of LLR in PHC to compare to our results. Large series of open approach for PHC have reported surgical resectability ranging between 50 and 80%, R0 resection achieved in 70–80% of patients [26]. Analysis of current results shows that LLR in PHC is promising, yet it is challenging and still in its developing phase. Main challenges are due to the complexity of surgical technique and overall scarceness of patients. Despite the absence of own experience in robotic assisted surgery, we do believe that robotic approach in liver resection for cholangiocarcinoma appears promising and technically achievable in selected patients specially when there is a need for vascular/biliary reconstructions.
There are clear limitations to this study, including its single center nature and the limited number of patients. Although small, this series represents the largest number of patients surgically treated for extra-pancreatic cholangiocarcinoma in a single institution through a minimally invasive approach.
Despite the complexity of biliary cancer surgical management, the present series suggests that LLR is feasible in patients presenting with early-stage gallbladder cancer and intra-hepatic cholangiocarcinoma. Regarding LLR in patients presenting with PHC, although results seem promising, more evidence is required and the procedure should still be considered in its early developing stages and reserved for highly specialized centers.
Abbreviations
- LLR:
-
Laparoscopic liver resection
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- CT:
-
Computed tomography
References
Aldrighetti L, Belli G, Boni L, Cillo U, Ettorre G, De Carlis L, Pinna A, Casciola L, Calise F, Italian Group of Minimally Invasive Liver S (2015) Italian experience in minimally invasive liver surgery: a national survey. Updates Surg 67:129–140. https://doi.org/10.1007/s13304-015-0307-2
Agarwal AK, Javed A, Kalayarasan R, Sakhuja P (2015) Minimally invasive versus the conventional open surgical approach of a radical cholecystectomy for gallbladder cancer: a retrospective comparative study. HPB 17:536–541. https://doi.org/10.1111/hpb.12406
Castro CM, Santibanez SP, Rivas TC, Cassis NJ (2018) Totally laparoscopic radical resection of gallbladder cancer: technical aspects and long-term results. World J Surg. https://doi.org/10.1007/s00268-018-4490-4
Gumbs AA, Jarufe N, Gayet B (2013) Minimally invasive approaches to extrapancreatic cholangiocarcinoma. Surg Endosc 27:406–414. https://doi.org/10.1007/s00464-012-2489-8
Gumbs AA, Hoffman JP (2010) Laparoscopic radical cholecystectomy and Roux-en-Y choledochojejunostomy for gallbladder cancer. Surg Endosc 24:1766–1768. https://doi.org/10.1007/s00464-009-0840-5
Dagher I, Gayet B, Tzanis D, Tranchart H, Fuks D, Soubrane O, Han HS, Kim KH, Cherqui D, O’Rourke N, Troisi RI, Aldrighetti L, Bjorn E, Abu Hilal M, Belli G, Kaneko H, Jarnagin WR, Lin C, Pekolj J, Buell JF, Wakabayashi G (2014) International experience for laparoscopic major liver resection. J Hepat Biliary Pancreat Sci 21:732–736. https://doi.org/10.1002/jhbp.140
Nomi T, Fuks D, Govindasamy M, Mal F, Nakajima Y, Gayet B (2015) Risk factors for complications after laparoscopic major hepatectomy. Br J Surg 102:254–260. https://doi.org/10.1002/bjs.9726
Hu HJ, Wu ZR, Jin YW, Ma WJ, Yang Q, Wang JK, Liu F, Li FY (2018) Minimally invasive surgery for hilar cholangiocarcinoma: state of art and future perspectives. ANZ J Surg. https://doi.org/10.1111/ans.14765
Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz BJ, Youssef BM, Klimstra D, Blumgart LH (2001) Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg 234:507–517 (Discussion 517–509)
Nomi T, Fuks D, Kawaguchi Y, Mal F, Nakajima Y, Gayet B (2015) Learning curve for laparoscopic major hepatectomy. Br J Surg 102:796–804. https://doi.org/10.1002/bjs.9798
Ishizawa T, Gumbs AA, Kokudo N, Gayet B (2012) Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg 256:959–964. https://doi.org/10.1097/SLA.0b013e31825ffed3
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Balzan S, Belghiti J, Farges O, Ogata S, Sauvanet A, Delefosse D, Durand F (2005) The “50–50 criteria” on postoperative day 5: an accurate predictor of liver failure and death after hepatectomy. Ann Surg 242:824–828 (Discussion 828–829)
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M, Christophi C, Banting S, Brooke-Smith M, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Nimura Y, Figueras J, DeMatteo RP, Buchler MW, Weitz J (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149:680–688. https://doi.org/10.1016/j.surg.2010.12.002
Ishizawa T, Hasegawa K, Kokudo N, Sano K, Imamura H, Beck Y, Sugawara Y, Makuuchi M (2009) Risk factors and management of ascites after liver resection to treat hepatocellular carcinoma. Arch Surg 144:46–51. https://doi.org/10.1001/archsurg.2008.511
Hezel AF, Zhu AX (2008) Systemic therapy for biliary tract cancers. The Oncologist 13:415–423. https://doi.org/10.1634/theoncologist.2007-0252
Han HS, Yoon YS, Agarwal AK, Belli G, Itano O, Gumbs AA, Yoon DS, Kang CM, Lee SE, Wakai T, Troisi RI (2019) Laparoscopic surgery for gallbladder cancer: an expert consensus statement. Dig Surg 36:1–6. https://doi.org/10.1159/000486207
Yoon YS, Han HS, Agarwal A, Belli G, Itano O, Gumbs AA, Yoon DS, Kang CM, Lee SE, Wakai T, Troisi RI (2019) Survey Results of the expert meeting on laparoscopic surgery for gallbladder cancer and a review of relevant literature. Dig Surg 36:7–12; https://doi.org/10.1159/000486208
Fiorentini G, Ratti F, Cipriani F, Palombo D, Catena M, Paganelli M, Aldrighetti L (2017) Minimally invasive approach to intrahepatic cholangiocarcinoma: technical notes for a safe hepatectomy and lymphadenectomy. Ann Laparosc Endosc Surg. https://doi.org/10.21037/ales.2017.03.05
Ratti F, Cipriani F, Ariotti R, Gagliano A, Paganelli M, Catena M, Aldrighetti L (2016) Safety and feasibility of laparoscopic liver resection with associated lymphadenectomy for intrahepatic cholangiocarcinoma: a propensity score-based case-matched analysis from a single institution. Surg Endosc 30:1999–2010. https://doi.org/10.1007/s00464-015-4430-4
Lee W, Park JH, Kim JY, Kwag SJ, Park T, Jeong SH, Ju YT, Jung EJ, Lee YJ, Hong SC, Choi SK, Jeong CY (2016) Comparison of perioperative and oncologic outcomes between open and laparoscopic liver resection for intrahepatic cholangiocarcinoma. Surg Endosc 30:4835–4840. https://doi.org/10.1007/s00464-016-4817-x
Yu H, Wu SD, Chen DX, Zhu G (2011) Laparoscopic resection of Bismuth type I and II hilar cholangiocarcinoma: an audit of 14 cases from two institutions. Dig Surg 28:44–49. https://doi.org/10.1159/000322398
Zhang W, Yan LN (2014) Perihilar cholangiocarcinoma: current therapy. World J Gastrointest Pathophysiol 5:344–354. https://doi.org/10.4291/wjgp.v5.i3.344
Launois B, Terblanche J, Lakehal M, Catheline JM, Bardaxoglou E, Landen S, Campion JP, Sutherland F, Meunier B (1999) Proximal bile duct cancer: high resectability rate and 5-year survival. Ann Surg 230:266–275
Capobianco I, Rolinger J, Nadalin S (2018) Resection for Klatskin tumors: technical complexities and results. Transl Gastroenterol Hepatol 3:69 https://doi.org/10.21037/tgh.2018.09.01
Mansour JC, Aloia TA, Crane CH, Heimbach JK, Nagino M, Vauthey JN (2015) Hilar cholangiocarcinoma: expert consensus statement. HPB 17:691–699. https://doi.org/10.1111/hpb.12450
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Walid Elmoghazy, Jane Cowan, Nicolas Tabchouri, Pascale Tinguely, Mostefa Bennamoun, Candice Tubbax, Anthony Sarran, Marine Lefevre, Christian Lamer, Brice Gayet, and David Fuks have no conflict of interests or financial ties to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elmoghazy, W., Cowan, J., Tabchouri, N. et al. Liver resection for extra-pancreatic biliary cancer: what is the role of laparoscopic approach?. Surg Endosc 33, 3711–3717 (2019). https://doi.org/10.1007/s00464-019-06664-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06664-7