Abstract
Background
Post-prostatectomy urinary incontinence is an adverse event leading to significant distress. Our aim was to evaluate immediate urinary continence (UC) recovery in a single-surgeon prospective randomized comparative study between the traditional robot-assisted laparoscopic radical prostatectomy (TR-RALP) and the Retzius-sparing RALP (RS-RALP), for the treatment of the clinically localized prostate cancer (PCa).
Methods
102 consecutive PCa patients were prospectively randomized to TR-RALP (57) or RS-RALP (45). Postoperative continence was defined as patient-reported absence of leakage or use of 0 pads/day. The immediate continence rate and 95% confidence interval (CI 95%) were calculated for each treatment. Univariable and multivariate logistic regressions were used to assess predictors of immediate continence following RALP. Continence rates from 1 to 6 months were calculated by Kaplan–Meier curves; log-rank test was used for the curve comparison. Two analyses were performed, considering a per-protocol (PP) population regarding all randomized patients that received nerve-sparing RALP and an Intention-To-Treat (ITT) population regarding all randomized patients that received RALP.
Results
In the PP analysis, the rates of immediate continence were 12/40 (30%) (CI 95% 17–47%) for the TR-RALP and 20/39 (51.3%) (CI 95% 35–68%) for the RS-RALP (p = 0.05). In the ITT analysis, the corresponding rates were 12/57 (21%) (CI 95% 11–34%) for the TR-RALP and 23/45 (51%) (CI 95% 36–66%) for the RS-RALP (p = 0.001). Median time to continence was 21 days for the TR-RALP and 1 day for RS-RALP, respectively (p = 0.02). The relative Kaplan–Meier curves regarding continence resulted statistically different when compared with the log rank test (p = 0.02). In the multivariate analysis, lower age and the Retzius-sparing approach were significantly associated to earlier continence recovery.
Conclusions
The Retzius-sparing approach significantly reduces time to continence following RALP. Further studies are required to confirm the reproducibility of our results and investigate the role of the RS-RALP as an additional “protective” factor for postoperative continence in the elderly population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Incontinence is one of the most feared complications of radical prostatectomy. Depending on the value put on urine leakage, the quality of life of patients may be strongly affected [1].
Several continence-sparing techniques have been implemented in the field of traditional RALP (TR-RALP). Bladder neck preservation [2] or intussusception [3], seminal vesicle sparing [4], restoration of the posterior part of the rhabdosphincter [5], puboperineoplasty [6], periurethral suspension stitches to the periosteum of the pubic bone [7], preservation of the lateral prostatic fascia [8], sparing of the pubovesical complex [9], selective ligation of the Santorini plexus [10] are only some of them. These techniques, alone or in combination, may lead to enhanced continence recovery; however, the literature is devoid of high quality of evidence regarding the majority of these techniques. Moreover, the rates of immediate continence (i.e. at the catheter removal) as evaluated in several series of TR-RALP remain low (13.1–38.4%), with a weighted mean of 25.7% [11]. Although the objective evaluation of urinary continence outcomes remains hindered by the lack of standardization of outcome reporting [12], it is evident that the early recovery of continence remains a challenge to be overcome.
Recently, the technique of Retzius-sparing RALP (RS-RALP) has been described [13]; it allows for a complete intrafascial approach avoiding all the Retzius structures involved in continence preservation. The immediate continence was reached in more than 90% of the patients [13], rendering the procedure highly promising.
Aim of the study
To provide a single-surgeon prospective randomized comparative study (RCT) on the immediate continence outcomes between the TR-RALP and the RS-RALP, for the treatment of the clinically localized prostate cancer (PCa). The pathologic (in terms of surgical margin status and pathologic stage/grade) and perioperative outcomes are compared. Patient-related and technical factors are finally assessed regarding their predictive role on immediate postoperative continence.
Patients and methods
Patients
Between November 2011 and October 2014, 102 consecutive male patients with clinically localized PCa underwent RALP, by traditional (trans-Retzius) (57 patients) or Retzius-sparing (45 patients) approach by a single surgeon (F.A) and according to a parallel design. The assignment of each patient to the first or second group of treatment was randomized (computer-generated randomization table). Inclusion criteria were life expectancy > 10 years, clinically organ-confined disease (cT1–cT2), biopsy Gleason score ≤ 7, total serum PSA ≤ 10 ng/ml, normal preoperative continence and normal international prostate symptom score (≤ 7).
Any previous prostatic, urethral, or bladder neck surgery, a positive magnetic resonance imaging for extracapsular extension, preoperative incontinence or neoadjuvant therapy were the exclusion criteria for the study.
Study end-points
The primary end point was to compare the immediate continence rates, i.e. at the catheter removal.
Secondary objectives were the comparisons of perioperative outcomes, complication rates, and oncological results.
Justification of patients’ number
The sample size of our study was able, with an adequate power (1-beta > 0.90), to recognize as significant (at alpha level of 0.05, bilateral) large differences (above 0.30) between incidence proportions of considered outcomes. More precisely, if the true percentages would be 50% in one group and 80% in the other, with the sample size of 39 patients/group or 52 patients/group the study will have power of 80% or 90% respectively to yield a statistically significant result. The sample size was obtained by means of Sample Power software (release 2.0).
Ethics
The study was conducted in accordance with the Ethical Principles for Medical Research Involving Human Subjects (World Medical Association, The Declaration of Helsinki Principles, 2000) and all patients provided written informed consent with guarantees of confidentiality. All patients gave their consent to publish and report their individual clinical data. All the candidates to RALP that respected the inclusion criteria of our study were explained during the informed consent process that the current standard of care for RALP is the anterior approach. The salient features of the posterior approach were then exposed, and they were provided the option for participation in the RCT. Eligible patients gave informed consent preoperatively both for RALP and randomization while actual assignment to the posterior or anterior arm was performed intraoperatively. The surgical team, post-operative caregivers and patients were not blinded to treatment assignment. The study was approved by the local medical ethical committee [ASL Lt/no. 43001/37895/2010].
Surgeon’s experience
The main surgeon has been previously (2006–2007) trained in a high-volume, reference centre in urologic robotic surgery on the TR-RALP. The study compares the cases performed with each technique in the initial experience of the surgeon (i.e. after < 50 cases for each technique).
Main outcome measures
Preoperative continence was evaluated as documented by the International Continence Society male short form questionnaire [14]. Postoperative continence was defined as patient-reported absence of leakage or use of 0 pads/day. It was assessed immediately after the catheter removal and subsequently by telephone interview at 1, 3 and 6 months after surgery.
The prostate specimens were en-bloc formalin fixed and inked to delineate the surgical margins; a step-sectioned transversally at 2–4 mm intervals technique was used to examine the specimen; an apical shaved-section, 2–4 mm thick, was truncated perpendicular to the prostatic urethra and sub-sequentially sectioned as slices parallel to the prostatic urethra. Bladder neck was examined sampling portions of tissue at the junction of the prostatic capsule and bladder neck or by sampling the most proximal portion of the submitted specimen corresponding to the anatomical bladder neck. The TNM 2002 classification was used for the staging.
A positive surgical margin (PSM) was considered when cancer cells were found in contact with the ink-marked resection margin.
All medical and surgical complications occurring both in the inpatient and outpatient setting were recorded.
A research fellow not involved in direct patient care and blinded to the treatment group of each patient performed the interviews and collected the data. The operating surgical team did not have access to the data files.
Principles of surgical technique
The TR-RALP was performed according to the Montsouris technique, through a transperitoneal, antegrade approach, with preservation of the bladder neck/puboprostatic ligaments, selective ligation of the dorsal vascular complex and with the intent of bilateral nerve-sparing inter/intrafascial dissection with high-anterior release of the neurovascular tissue.
The RS-RALP was performed as follows: incision of the peritoneum overlying the rectovesical pouch for about 5 cm, identification of the vas deferens and the seminal vesicle (SV) tip, dissection of the posterior aspect of the SV from the Denonvillier’s fascia, control of the prostatic vascular pedicles at the base of the prostate with 2–4 mm clips (B-Braun Challenger or DS Clips) dissection of the posterior and posterolateral surface of the prostate till the apex and with the intent of bilateral, inter/intrafascial nerve-sparing, dissection of the lateral aspect of the prostate until the anterior attachments of the detrusor apron and the Santorini plexus, incision of the vesico-prostatic muscle, incision of the bladder neck, dissection of the ventral prostatic surface that completely spares the pubovesical complex (PVC) and the dorsal vascular complex, dissection of the apex and urethral transection [15].
The patient steep (25°–30°) Trendelenburg position, the placement of the trocars, the intrabdominal CO2 pressure (obtained with the use of Airseal), the technique of energy and tension-free dissection of the prostatic pedicles/periprostatic neurovascular tissue and the technique for the vesico-urethral anastomosis without posterior Rocco’s reconstruction and with a barbed suture according to Van Velthoven were similar between the two groups.
Postoperative care
The drain was removed after 24–48 h in the absence of any signs of a urinary fistula (output < 100 cc). Patients were regularly discharged in postoperative day 2 or 3 with the Foley catheter still in place, that was removed on an outpatient basis 7–8 days after surgery. All the patients received therapy with PDE5 inhibitors (tadalafil 5 mg, 1 cp per day) for the first 2 months after surgery and after as subjectively needed.
Statistical analysis
The statistical analysis was performed with the STATA 14.1 by an independent, dedicated biostatistician uninvolved in the study and blinded to treatment assignment. The numeric parameters between both groups were compared using Student’s t test or the Mann–Whitney U test where appropriate. Nominal data were compared using the Chi-square or Fisher exact test. The immediate continence rate and 95% confidence interval (CI 95%) were calculated for each treatment. Univariable logistic regressions were used to assess predictors of immediate continence following RALP. Odds ratio (OR) and CI 95% are presented. Variables with association (p value < 0.1) at the univariate analysis were tested in multivariable logistic regression [adjusted OR (adjOR) and CI 95% are presented]. Continence rates at 1, 3and 6 months were calculated by Kaplan–Meier curves; log-rank test was used for the curve comparison. Patients who did not achieve continence at the end of their observation were considered censored. A p value of 0.05 was considered statistically significant. Per-protocol (PP) population included all randomized patients receiving nerve-sparing RALP and with complete postoperative UC data; the Intention-To-Treat (ITT) Population regarded all randomized patients receiving even extrafascial (non nerve-sparing) RALP. In the ITT analysis, for patients who did not have any postoperative UC data the immediate continence was imputed ad failed. The primary endpoint was analysed on both the PP and ITT population while the secondary endpoints were analysed only on PP population.
Results
The flow diagram displaying the progress of all participants through the trial (according to the CONSORT statement [16]) is shown in Fig. 1. A total of 19 patients (13 TR-RALP and 6 RS-RALP) received non nerve-sparing RALP (wide, extrafascial dissection and were included only in the ITT analysis). For four patients of the TR-RALP group without any data on postoperative continence, the immediate continence was imputed ad failed and were included only in the ITT population. Consequently, PP population consisted of a 40 patients for TR-RALP and 39 patients for RS-RALP, submitted to either intra- or inter-fascial bilateral nerve-sparing RALP, while ITT population consisted of 57 patients for TR-RALP and 45 patients for RS-RALP.
Flow diagram displaying the progress of all participants through the trial according to the CONSORT statement. A wide (extrafascial) dissection of the neurovascular tissue was performed in cases of intraoperative adherences between prostate and bundle, macroscopic evidence of extraprostatic extension of the PCa or any doubts about the oncologic radicality of the technique, especially in preoperatively impotent patients or for those not interested in postoperative sexual activity
As shown in Table 1, no statistically significant differences were observed between the two groups in terms of preoperative age, prostate-specific antigen (PSA), biopsy Gleason score and clinical stage. As shown in Table 2, mean operative time, rates of complications and performed lymph-node dissections were also similar. A difference in the rates of unilateral vs. bilateral nerve-sparing was observed between groups (p = 0.032). Table 3 indicates that the two compared approaches were similar in terms of pathologic data (Gleason score, stage). A difference in PSM rates (10% vs. 28.2%, p = 0.05) was observed between groups; a sub-analysis revealed that this difference was due to the higher rate of pT3 (extraprostatic) disease in RS-RALP and not related to the extent of neurovascular tissue dissection (i.e. intra vs. interfascial).
Comparison of continence rates
No patient had a urinary fistula; drain was removed in all cases within 48 h; all the patients were discharged according to the protocol and had their Foley catheter removed at an outpatient basis as planned (at 7–8 days after surgery) and without prior cystogram; no differences in the Foley indwelling time were recorded between groups.
In the ITT analysis, the rates of immediate continence were 12/57 (21%) (CI 95% 11–34%) for the TR-RALP and 23/45 (51%) (CI 95% 36–66%) for the RS-RALP (p = 0.001). In the PP analysis, the corresponding rates were 12/40 (30%) (CI 95% 17–47%) for the TR-RALP and 20/39 (51%) (CI 95% 35–68%) for the RS-RALP (p = 0.05). Median time to continence was 21 days for TR-RALP and 1 day for the RS-RALP respectively (p = 0.02), indicating that the 50% of the patients reaches earlier the primary endpoint in the RS-RALP group.
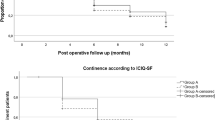
Continence recovery in function of time is depicted for both groups in Figs. 2 and 3, from 0 to 180 days after RALP. The comparison of the two curves yielded statistical significance (log rank test, p = 0.02) at each timepoint and for both ITT and PP population.
ITT analysis (all randomized patients receiving even extrafascial, non nerve-sparing RALP; for patients who did not have any postoperative UC data the immediate continence was imputed ad failed). Urinary continence recovery in patients treated with anterior (traditional-TR) vs. posterior (Retzius-sparing-RS) RALP during 6 months of follow-up, defined as patient-reported absence of leakage or use of 0 pads/day. Numbers along X-axis represent number of men at risk (i.e. those who were still incontinent)
Per protocol analysis (randomized patients receiving nerve-sparing RALP and with complete postoperative UC data). Urinary continence recovery in patients treated with anterior (Montsouris-TR) vs. posterior (Bocciardi-RS) RALP during 6 months of follow-up, defined as patient-reported absence of leakage or use of 0 pads/day. Numbers along X-axis represent number of men at risk (i.e. those who were still incontinent)
Univariate and multivariate analyses for factors predicting immediate continence (Table 4)
At the univariable regression analysis, among the various factors that were evaluated as potential predictors of immediate continence (Age, BMI, PSA, prostate weight, preoperative IPSS, nerve-sparing, pathologic stage, preoperative and pathologic Gleason score, surgical approach to the prostate) only the age and the surgical approach (Retzius-sparing vs. traditional) were significantly associated to continence recovery.
In the multivariate analysis, once adjusted for age, the traditional approach is significantly inferior to the Retzius-Sparing (OR 0.3 CI 95% 0.11–0.83 p = 0.021) concerning early continence recovery, while once adjusted for technique, age is still associated to immediate continence.
Discussion
Urinary incontinence after radical prostatectomy is an adverse event that leads to significant distress. Reported continence rates at 12 months following RALP according to recent series range between 82.1 and 97% [11, 17], depending on the definition of incontinence, severity, bother and the methodology to assess its magnitude [18].
More than long-term UC, early postoperative urinary incontinence still remains a challenge to be overcome with the highest rates of the urinary incontinence-associated bother noted in the first 2–6 mo after surgery [19,20,21]. Time to continence continues to be an issue of significant bother among men undergoing RALP [22].
There are multiple pathophysiologic mechanisms underlying the occurrence of post-prostatectomy incontinence (PPI). Beside to biological factors related to PPI (age, BMI, pre-existing LUTS, prostate size, membranous urethral length etc.), it is the integrity of the external urinary sphincter complex (muscle tissue and innervation), bladder-neck, supporting structures of the membranous urethra as well as the integrity of neural components (pudendal nerve branches and possibly cavernous nerves) to contribute to UC recovery [18].
Several techniques have been consequently developed in order to enhance continence recovery after RALP that can be summarized in three major categories: preservation (bladder neck, neurovascular bundles, puboprostatic ligaments, pubovesical complex, functional urethral length etc.), reconstruction (posterior, anterior, total), and reinforcement (bladder neck plication, sling suspension, suspension of the dorsal vascular complex to the periosteum of the pubic bone etc) [23]. The common denominator of these techniques is to maintain the intactness or to reply the functionality of the periprostatic anatomic structures.
In a recent study, Galfano et al. [13] found that a surgical technique sparing the Retzius structures yielded high early continence rates. The described technique preserves complete anatomic integrity of Aphrodite’s veil, containing the neurovascular bundles. With the standard RALP procedure as well as with intrafascial approaches preserving Aphrodite’s veil, the higher aspect of the veil has to be opened. In contrast, with the Bocciardi approach, the veil does not have to be opened at any point, providing a strong rationale for obtaining better results. Moreover, this approach enables the surgeon to avoid the Santorini plexus, ensuring less blood loss and preserving some small arteries running into the plexus; their role is currently unknown; however, a possible role in the accessorial blood supply of the striated sphincter or the corpora cavernosa cannot be excluded. Finally, pubourethral ligaments and eventual accessory pudendal arteries are avoided completely. The importance of their integrity is still debated, but some role in preservation of continence and potency has been postulated by several authors [24].
Asimakopoulos et al. [9] described the technique of preservation of the pubovesical complex (i.e. detrusor apron and pubovesical ligaments) and reported 80% of completely dry patients and 20% of patients that needed one security pad at the catheter removal following RALP.
Both the aforementioned techniques, that are characterized by the preservation of the structures of the anterior compartment of the Retzius space that are involved in the mechanism of continence, are associated with an enhanced continence recovery.
In the study of Galfano et al. [13], defining continence as 0–1 pad/day, there was reported a 90% of UC, reduced to 76% when there were considered only the cases with 0 pads/day. To our knowledge, this is the group with the largest experience in the world with the RS-RALP. The main limitations of this prospective study were its non-randomized and non-comparative design.
Recently, Dalela et al. [25] published a prospective RCT examining the impact of the Retzius-sparing approach on early urinary continence recovery after RALP. The authors randomized 120 patients with low-intermediate risk PCa to receive either Retzius-sparing or traditional RALP. The primary outcome was urinary continence (defined as 0–1 security liner per day 1 week after catheter removal). According to this study, the RS-RALP resulted in earlier recovery of urinary continence and lower urinary function-related bother compared with standard RALP; in fact, compared with 48% in the TR-RALP, 71% of men undergoing RS-RALP were continent 1 week after catheter removal (p = 0.01). Median time to continence in RS vs. TR-RALP was 2 and 8 days post-catheter removal respectively. When UC was defined as use of 0 pads/day, the rates of immediate continence were 15% in the TR vs. 42% in the RS-RALP.
In our study, in the PP population the rate of immediate continence following the Retzius-sparing approach was 51% while following the traditional was 30% (p = 0.05); the difference in the observed outcomes became clearly statistically significant when the ITT population was considered. Median continence time was 1 vs. 21 days for RS-RALP and TS-RALP, respectively. The comparison of the Kaplan–Meier curves regarding the rates of postoperative continence yielded a statistically significant difference at all time-points after RALP. In both the univariate and multivariate regression analysis, the age and the surgical approach were significantly associated to immediate continence recovery.
Once adjusted for technique, for each extra year of age the possibility of achieving immediate continence is reduced of about 13%, suggesting similar to other studies [26] that older age has a significant adverse effect on recovery of continence. Once adjusted for age, the traditional technique reduces the possibility of immediate continence of about 70% when compared to the Retzius-sparing, rendering the RS-RALP highly promising as an additional “protective” factor for postoperative continence in the elderly population. None of the other evaluated variables were predictors of urinary continence recovery.
The included cases, although performed by the same surgeon, represent his initial personal experience, after < 50 cases previously performed with each technique. Although the surgeon was not previously trained to the Retzius-sparing technique (first described in 2010), in his hands this approach yielded higher continence outcomes.
By using the same definition of UC (0 pads/day) our study yielded higher rates of immediate UC for both arms with respect to Dalela et al. [25]. The difference may be explained by the characteristics of the included populations: in our study mainly low-risk PCa patients were included and our “per-protocol” analysis included only those submitted to nerve-sparing (intra or interfascial) RALP. Our outcomes regarded UC at the catheter removal (while in the study of Dalela UC was evaluated 1 week later). Finally, in both studies, there was a higher PSM rate for the posterior approach that was due to the higher rate of pT3 disease in RS-RALP and not related to the surgical technique or extent of NVT preservation.
The preservation of the periprostatic anatomy is of paramount importance for the maximization of the post-RALP functional outcomes [9]. The Retzius-sparing approach, similarly to the PVC preservation described before [9], achieves a complete sparing of the anatomical structures (detrusor apon and related ligaments) that physiologically support the external urethral sphincter complex and preserve the urethra in its normal place in the pelvic floor, providing the necessary anterior stabilization for its biomechanics. The anterior suspension of the vesico-urethral anastomosis prevents urethral stump recession and probably alleviates downward bladder prolapse on the anastomosis.
Several are the limits of the current study. The study population, although adequately powered, is small. No comparison of the erectile function outcomes or long-term oncologic outcomes has been performed. However, as shown by a recent manuscript [27], there was not a significant difference in erectile function (EF) outcomes (defined as erections sufficient for penetrative intercourse) both at 3 months (36.7% for TR-RALP vs. 43.7% for RS-RALP) and 12 months (69.2% vs. 86.5% respectively, p = 0.5). Biochemical recurrence-free survival (BCRFS) rates at 12 months were 92.7% for TR-RALP vs. 91.4% for RS-RALP. Our trial was powered a priori to assess differences in continence recovery; considering that the reported differences in EF recovery rates and BCRFS are minimal and not of statistical significance, our sample size would be inadequately powered to assess them. No cases of high-risk prostate cancer were finally included and no urinary function-related bother scores were assessed.
Conclusions
While multiple factors are associated with the development of postprostatectomy incontinence, surgical modifications also play a role. In this context, it seems that the Retzius-sparing approach enhances, as an independent factor, early continence recovery. Elder patients may benefit more from the Retzius-sparing approach in RALP. Further studies are required to confirm the reproducibility of our results.
References
Cambio AJ, Evans CP (2006) Minimising postoperative incontinence following radical prostatectomy: considerations and evidence. Eur Urol 50(5):903–913 (discussion 913)
Freire MP, Weinberg AC, Lei Y, Soukup JR, Lipsitz SR, Prasad SM, Korkes F, Lin T, Hu JC (2009) Anatomic bladder neck preservation during robotic-assisted laparoscopic radical prostatectomy: description of technique and outcomes. Eur Urol 56(6):972–980
Tan HJ, Xiong S, Laviana AA, Chuang RJ, Treat E, Walsh PC, Hu JC.. Tan HJ, Xiong S, Laviana AA, Chuang RJ, Treat E, Walsh PC, Hu JC (2016) Technique and outcomes of bladder neck intussusception during robot-assisted laparoscopic prostatectomy: a parallel comparative trial. Urol Oncol 34(12):529.e1–529.e7
John H, Hauri D (2000) Seminal vesicle-sparing radical prostatectomy: a novel concept to restore early urinary continence. Urology 55(6):820–824
Rocco B, Gregori A, Stener S, Santoro L, Bozzola A, Galli S, Knez R, Scieri F, Scaburri A, Gaboardi F (2007) Posterior reconstruction of the rhabdosphincter allows a rapid recovery of continence after transperitoneal videolaparoscopic radical prostatectomy. Eur Urol 51(4):996–1003
Tewari AK, Bigelow K, Rao S, Takenaka A, El-Tabi N, Te A, Vaughan ED (2007) Anatomic restoration technique of continence mechanism and preservation of puboprostatic collar: a novel modification to achieve early urinary continence in men undergoing robotic prostatectomy. Urology 69(4):726–731
Patel VR, Coelho RF, Palmer KJ, Rocco B (2009) Periurethral suspension stitch during robot-assisted laparoscopic radical prostatectomy: description of the technique and continence outcomes. Eur Urol 56(3):472–478
van der Poel HG, de Blok W, Joshi N, van Muilekom E (2009) Preservation of lateral prostatic fascia is associated with urine continence after robotic-assisted prostatectomy. Eur Urol 55(4):892–900
Asimakopoulos AD, Annino F, D’Orazio A, Pereira CF, Mugnier C, Hoepffner JL, Piechaud T, Gaston R (2010) Complete periprostatic anatomy preservation during robot-assisted laparoscopic radical prostatectomy (RALP): the new pubovesical complex-sparing technique. Eur Urol 58(3):407–417
Porpiglia F, Fiori C, Grande S, Morra I, Scarpa RM (2009) Selective versus standard ligature of the deep venous complex during laparoscopic radical prostatectomy: effects on continence, blood loss, and margin status. Eur Urol 55(6):1377–1383
Coelho RF, Chauhan S, Palmer KJ, Rocco B, Patel MB, Patel VR (2009) Robotic-assisted radical prostatectomy: a review of current outcomes. BJU Int 104(10):1428–1435
Krupski TL, Saigal CS, Litwin MS (2003) Variation in continence and potency by definition. J Urol 170(4 Pt 1):1291–1294
Galfano A, Di Trapani D, Sozzi F, Strada E, Petralia G, Bramerio M, Ascione A, Gambacorta M, Bocciardi AM (2013) Beyond the learning curve of the Retzius-sparing approach for robot-assisted laparoscopic radical prostatectomy: oncologic and functional results of the first 200 patients with ≥ 1 year of follow-up. Eur Urol 64(6):974–980
Donovan JL, Peters TJ, Abrams P, Brookes ST, de la Rosette JJ, Schäfer W (2000) Scoring the short form ICSmaleSF questionnaire. J Urol 164:1948–1955
Asimakopoulos AD, Miano R, Galfano A, Bocciardi AM, Vespasiani G, Spera E, Gaston R (2015) Retzius-sparing robot-assisted laparoscopic radical prostatectomy: critical appraisal of the anatomic landmarks for a complete intrafascial approach. Clin Anat 28(7):896–902
Schulz KF, Altman DG, Moher D, for the CONSORT Group. (2010) CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. Ann Int Med 152:726–732
Ficarra V, Novara G, Artibani W, Cestari A, Galfano A, Graefen M, Guazzoni G, Guillonneau B, Menon M, Montorsi F, Patel V, Rassweiler J, Van Poppel H (2009) Retropubic, laparoscopic, and robot-assisted radical prostatectomy: a systematic review and cumulative analysis of comparative studies. Eur Urol 55(5):1037–1063
Heesakkers J, Farag F, Bauer RM, Sandhu J, De Ridder D, Stenzl A (2017) Pathophysiology and contributing factors in postprostatectomy incontinence: a review. Eur Urol 71(6):936–944
Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L, Hembroff L, Lin X, Greenfield TK, Litwin MS, Saigal CS, Mahadevan A, Klein E, Kibel A, Pisters LL, Kuban D, Kaplan I, Wood D, Ciezki J, Shah N, Wei JT (2008) Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med 358(12):1250–1261
Prabhu V, Sivarajan G, Taksler GB, Laze J, Lepor H (2014) Long-term continence outcomes in men undergoing radical prostatectomy for clinically localized prostate cancer. Eur Urol 65(1):52–57
Donovan JL, Hamdy FC, Lane JA, Mason M, Metcalfe C, Walsh E, Blazeby JM, Peters TJ, Holding P, Bonnington S, Lennon T, Bradshaw L, Cooper D, Herbert P, Howson J, Jones A, Lyons N, Salter E, Thompson P, Tidball S, Blaikie J, Gray C, Bollina P, Catto J, Doble A, Doherty A, Gillatt D, Kockelbergh R, Kynaston H, Paul A, Powell P, Prescott S, Rosario DJ, Rowe E, Davis M, Turner EL, Martin RM, Neal DE, ProtecT Study Group* (2016) Patient-reported outcomes after monitoring, surgery, or radiotherapy for prostate cancer. N Engl J Med 375(15):1425–1437
Barry MJ, Gallagher PM, Skinner JS, Fowler FJ Jr (2012) Adverse effects of robotic-assisted laparoscopic versus open retropubic radical prostatectomy among a nationwide random sample of medicare-age men. J Clin Oncol 30(5):513–518
Yanagida T, Koguchi T, Hata J, Yabe M, Sato Y, Akaihata H, Kawashima Y, Kataoka M, Ogawa S, Kumagai S, Kumagai K, Haga N, Kushida N, Ishibashi K, Aikawa K, Kojima Y (2014) Current techniques to improve outcomes for early return of urinary continence following robot-assisted radical prostatectomy. Fukushima J Med Sci 60(1):1–13
Galfano A, Ascione A, Grimaldi S, Petralia G, Strada E, Bocciardi AM (2010) A new anatomic approach for robot-assisted laparoscopic prostatectomy: a feasibility study for completely intrafascial surgery. Eur Urol 58(3):457–461
Dalela D, Jeong W, Prasad MA, Sood A, Abdollah F, Diaz M, Karabon P, Sammon J, Jamil M, Baize B, Simone A, Menon M (2017) A pragmatic randomized controlled trial examining the Impact of the Retzius-sparing approach on early urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol 72(5):677–685
Mandel P, Graefen M, Michl U, Huland H, Tilki D (2015) The effect of age on functional outcomes after radical prostatectomy. Urol Oncol 33(5):203.e11–203.e18
Menon M, Dalela D, Jamil M, Diaz M, Tallman C, Abdollah F, Sood A, Lehtola L, Miller D, Jeong W (2018) Functional recovery, oncologic outcomes and postoperative complications after robot-assisted radical prostatectomy: an evidence-based analysis comparing the Retzius sparing and standard approaches. J Urol 199(5):1210–1217
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr Asimakopoulos Anastasios, Dr Topazio Luca, Dr De Angelis Michele, Dr Finazzi Agrò Enrico, Dr Antonio Lugi Pastore, Dr Andrea Fuschi and Dr Annino Filippo have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Asimakopoulos, A.D., Topazio, L., De Angelis, M. et al. Retzius-sparing versus standard robot-assisted radical prostatectomy: a prospective randomized comparison on immediate continence rates. Surg Endosc 33, 2187–2196 (2019). https://doi.org/10.1007/s00464-018-6499-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6499-z