Abstract
Background
Delta-shaped anastomosis is usually applied for an intracorporeal gastrogastrostomy in totally laparoscopic pylorus-preserving gastrectomy (TLPPG). However, the remnant stomach is slightly twisted around the anastomosis because it connects in side-to-side fashion. To realize an intracorporeal end-to-end gastrogastrostomy using an endoscopic linear stapler, we invented a novel method including a unique anastomotic technique.
Materials and methods
In this new approach, we first made small gastrotomies at the greater and lesser curvatures of the transected antrum and then pierced it using an endoscopic linear stapler. After the pierced antrum and the proximal remnant stomach were mechanically connected, the gastrotomies and stapling lines were transected using an endoscopic linear stapler, creating an intracorporeal end-to-end gastrogastrostomy. We have named this technique the “piercing method” because piercing the stomach is essential to its implementation. Between October 2015 and June 2017, 26 patients who had clinically early gastric cancer at the middle third of the stomach without clinical evidence of lymph node metastasis underwent TLPPG involving the novel method.
Results
The 26 patients successfully underwent an intracorporeal mechanical end-to-end gastrogastrostomy by the piercing method. The median operation time of the 26 patients was 272 min (range 209–357 min). With the exception of one gastric stasis, no problems associated with the piercing method were encountered during and after surgery.
Conclusion
The piercing method can safely create an intracorporeal mechanical end-to-end gastrogastrostomy in TLPPG. Piercing the stomach using an endoscopic linear stapler is a new technique for gastrointestinal anastomosis. This method should be considered if the surgical aim is creation of an intracorporeal end-to-end gastrogastrostomy in TLPPG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
As innovation in endosurgical devices and techniques advances, laparoscopic gastrectomy tends toward being performed completely under a laparoscopic view, including reconstruction followed by lymph node dissection, named totally laparoscopic gastrectomy (TLG) [1,2,3]. Pylorus-preserving gastrectomy (PPG), which is intended to avoid dumping syndrome and obtain better nutritional status [4,5,6], is also performed as one type of TLG by many surgeons. In totally laparoscopic PPG (TLPPG), gastrogastrostomy as reconstruction is created mechanically by delta-shaped anastomosis [7, 8] in a manner originally developed for Billroth I reconstruction in totally laparoscopic distal gastrectomy [2].
Although delta-shaped anastomosis for gastrogastrostomy in TLPPG is easy and safe [7, 8], it harbors several problems. The antrum and proximal remnant stomach, which are connected by the delta-shaped anastomosis, are slightly twisted around the anastomosis, and the lesser curvature side of the antral-transected edge is not used for anastomosis as it is side-to-side anastomosis [7, 8]. Moreover, gastric stasis, a distinctive complication of PPG was reported at a rate of 10.0% in TLPPG including delta-shaped anastomosis compared with 6.2% in end-to-end anastomosis by hand stitching in laparoscopy-assisted PPG [8].
Solving the problems concerning delta-shaped anastomosis has required development of a mechanical end-to-end anastomotic method in TLPPG. Therefore, a novel intracorporeal mechanical end-to-end gastrogastrostomy using an endoscopic linear stapler involving an entirely new technique of intestinal anastomosis has been invented and applied for the treatment of several patients. Despite its limited application thus far, this novel anastomotic method has safely created an ideal end-to-end anastomosis after which all patients followed a satisfactory postoperative course. Herein, we present the technique of mechanical end-to-end gastrogastrostomy in TLPPG and an evaluation of its safety.
Materials and methods
Patients
Between October 2015 and June 2017, 26 patients who had clinically early gastric cancer at the middle third of the stomach without clinical evidence of lymph node metastasis underwent TLPPG that included the method of gastrogastrostomy invented by the first author as an operator or instructive assistant at the Cancer Institute Hospital, Tokyo, Japan. The 26 patients comprised 13 men and 13 women of median age 58 years (range 35–79 years). All patients had histologically proven gastric adenocarcinoma or signet ring cell carcinoma. Written informed consent was obtained from all patients prior to surgery.
Basic concept of a novel method
This novel anastomotic method incorporates a unique technique which, to the best of our knowledge, has not previously been applied. Even if the anvil of an endoscopic linear stapler is inserted through a small gastrotomy on the greater curvature of the antrum, an end-to-end anastomosis using the full length of the antral transected edge cannot be created. Constructively, about 1 cm from the tip of the anvil does not receive staples. Additionally, with regard to the limit of anvil insertion due to closed cavity at the lesser curvature side, stapling and cutting does not reach the edge of the lesser curvature, being about 2–3 cm short of the edge (Fig. 1A). However, if a small gastrotomy is also made on the edge of the lesser curvature and the tip of the anvil comes through this gastrotomy, i.e., pierces the antrum, the ending point of stapling and cutting can be made closer to the edge of the lesser curvature (Fig. 1B), which is very accurate and sure, so that almost the full length of the antral transected edge can be used for an end-to-end anastomosis. Finally, stapling and cutting of the stomach wall (Fig. 2A) creates an end-to-end anastomosis using the full length of the antral transected edge (Fig. 2B). Piercing the antrum with the anvil is an essential process of this novel anastomotic method. The technique is named the “piercing method” for this reason.
Usefulness of piercing the stomach in an end-to-end gastrogastrostomy using the full length of the antral-transected line. A Because about 1 cm from the tip of the anvil does not receive staples and anvil insertion is limited due to closed cavity at the lesser curvature side, stapling and cutting reach about 2–3 cm short of the lesser curvature edge if the anvil side is inserted into the antrum through the small gastrotomy of the greater curvature in anastomosis. B If a small gastrotomy is also made at the lesser curvature edge and an endoscopic linear stapler pierces the antrum in anastomosis, stapling and cutting can almost reach the lesser curvature edge
Basic procedure of end-to-end gastrogastrostomy by the piercing method. A The posterior anastomosis is created by the piercing technique. B The common entry hole, the transected edges, the anastomosis between the transected edges, and the small gastrotomy of the lesser curvature (encircled in A) are stapled and cut using an endoscopic linear stapler, after which an end-to-end gastrogastrostomy by the piercing method is completed
Preparation of the antrum
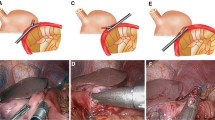
After usual lymph node dissection of PPG [9, 10], using five working ports, one at the umbilicus for a laparoscope and the remaining four at the bilateral hypochondrium and the mid-abdomen for several kinds of forceps, an energy device, and an endoscopic linear stapler, serosal marks on the points 5 cm from the pylorus at both the lesser and greater curvature sides were drawn and connected. A small gastrotomy along the mark at the greater curvature was created and the antrum was incompletely divided with an endoscopic linear stapler (iDrive Ultra Powered Stapling System; Medtronic, Dublin, Ireland) intracorporeally, which was inserted from the greater curvature side (Fig. 3A). The remaining lesser curvature was completely divided using an ultrasonically activated device to create another hole in the antrum. At this point, the antrum had two small gastrotomies located at the edges of both the greater and lesser curvatures (Fig. 3B).
Preparation of the antrum in the piercing method. A After a small gastrotomy is made at the greater curvature (arrowhead), the antrum is transected incompletely using an endoscopic linear stapler with the lesser curvature still connected. B The connection of the lesser curvature is sharply transected with an ultrasonically activated device. The antrum has two small gastrotomies at the greater (black arrowhead) and lesser curvatures (white arrowhead)
Creation of the posterior anastomosis
After the stomach was transected at the proximal side of the lesion and the specimen was taken from the abdominal cavity, a gastrogastrostomy was initiated. A small gastrotomy was made on the edge of the greater curvature at the proximal remnant stomach. An endoscopic linear stapler with a curved-tip cartridge attached (End GIA 60-mm Curved Tip Articulating Medium/Thick Reload with Tri-Staple Technology; Medtronic) was introduced into the abdominal cavity from the left inferior port. A special cartridge with a curved and triangle-shaped tip easily pierced the stomach. The cartridge side was inserted into the proximal remnant stomach through the gastrotomy. Next, the anvil side was inserted into the gastrotomy of the greater curvature at the antrum and the tip of the anvil was pushed to protrude from the gastrotomy at the lesser curvature of the antrum (Fig. 4A). The antrum was pierced with the endoscopic linear stapler, which is an original and essential aspect of this novel anastomotic procedure. The endoscopic linear stapler was fired, keeping the antrum pierced with the endoscopic linear stapler and attaching the transected edges of both the proximal and distal remnant stomach, and an anastomosis of the posterior wall from a common entry hole to the gastrotomy of the lesser curvature at the antrum was made (Fig. 4B). After the anastomosis, checks were made to confirm that there was no bleeding and adequate stapling.
Creation of the posterior anastomosis using an endoscopic linear stapler with a special type of the cartridge attached. A After the cartridge side is inserted into the proximal remnant stomach through the gastrotomy, the anvil side is introduced into the gastrotomy of the greater curvature at the antrum. The curved tip of the anvil protrudes from the gastrotomy at the lesser curvature of the antrum (arrowhead). B Keeping the antrum pierced with the endoscopic linear stapler (arrowhead) and attaching the transected edges of both the proximal and distal remnant stomach, the endoscopic linear stapler is fired and an anastomosis of the posterior wall is made
Creation of the anterior anastomosis
To create the anterior anastomosis, the common entry hole, the entire length of the antral transected edge, the greater curvature side of the transected edge at the proximal remnant stomach, the anastomosis between the transected edges, and the gastrotomy of the lesser curvature at the antrum were stapled and cut using an endoscopic linear stapler with a black cartridge attached (Endo GIATM 60-mm Articulating Extra-Thick Reload with Tri-Staple Technology; Medtronic) inserted from the left inferior port. A black cartridge was selected to create the anterior anastomosis, as it was capable of stapling and cutting the thick overlapping gastric wall of the lesser curvature side. The common entry hole was temporarily closed, and stay sutures were placed on the transected edges of both the antrum and the proximal remnant stomach including the anastomosis between them, as well as on the near and opposite side of the gastrotomy at the lesser curvature of the antrum (Fig. 5A). Moreover, the gastrotomy was colored for easy visual identification. The strings were then pulled upward, and an endoscopic linear stapler with black cartridge was used to staple and cut the lifted stomach wall. The first firing of the stapler closed the common entry hole at the greater curvature side, and the additional stapling created the remaining anastomosis (Fig. 5B). It is very important to absolutely cut the small gastrotomy of the lesser curvature at the antrum. The strings around the gastrotomy and the visual confirmation of the colored one are indispensable for cutting the lifted stomach including the gastrotomy of the lesser curvature at the antrum.
Creation of the anterior wall using an endoscopic linear stapler with black cartridges. A The common entry hole is temporarily closed and stay sutures placed on the transected edges of both the antrum and proximal remnant stomach including the anastomosis between them, as well as around the gastrotomy on the lesser curvature of the antrum. B After the strings are pulled upward, an endoscopic linear stapler with a black cartridge attached staples and cuts the lifted stomach wall, after which an intracorporeal end-to-end gastrogastrostomy by the piercing method is completed
Confirmation of hemostasis and sufficient anastomosis
After the piercing method was completed (Fig. 6), intraoperative gastroendoscopy was carried out to confirm hemostasis, the opening size, and adequacy of the anastomosis (Fig. 7A). If any problem was discovered, an appropriate solution was applied immediately. Even if no problem was discerned under endoscopic view, the edge of the anterior anastomosis on the greater curvature and the crossing part of the stapling on the lesser curvature were buried by seromuscular sutures.
An ideal end-to-end gastrogastrostomy by the piercing method. A No bleeding and anastomotic sufficiency are confirmed by intraoperative gastroendoscopy. The reconstructive remnant stomach expands cylindrically under inflating CO2 (lateral side view). B The piercing method creates a beautiful and fit end-to-end gastrogastrostomy using the full length of the antral transected edge (anterior side view)
The timeline of the anastomotic procedures is presented in the supplemental data (Video 1).
Results
The 26 patients successfully underwent an intracorporeal mechanical end-to-end gastrogastrostomy by the piercing method. The median operation time for the 26 patients was 272 min (range 209–357 min). No problems concerning the piercing method occurred during surgery. Postoperatively, no complications concerning the anastomosis were witnessed except for one episode of gastric stasis. The patient suffering from gastric stasis was 79-year-old woman who also suffered from colitis induced by Clostridium difficile toxin. She required fasting, transfusion, and medication to relieve abdominal distension and diarrhea. Forty-six days after surgery, she was discharged without any symptoms.
One year after surgery, 20 patients underwent gastroendoscopy, which revealed that all anastomoses presented a wide circular shape with the antral cuffs maintained circumferentially (Fig. 7B).
Discussion
The present study showed that a novel intracorporeal anastomotic method involving a unique technique, piercing the stomach with an endoscopic linear stapler, safely creates a mechanical end-to-end gastrogastrostomy in TLPPG. This is the first report of the piercing technique applied for a mechanical intestinal anastomosis that enables an intracorporeal end-to-end gastrogastrostomy in TLPPG.
Piercing the stomach using an endoscopic linear stapler was very useful in realizing an intracorporeal end-to-end gastrogastrostomy. Although the piercing method is equivalent to triangular anastomosis, piercing the stomach with an endoscopic linear stapler eliminates the need for entire opening of the transected edges in both the antrum and the proximal remnant stomach. Three methods to create an end-to-end gastrogastrostomy in TLPPG can be considered if the piercing technique is not applied. First, an anastomosis can be made by a complete hand stitch. Similar to an extracorporeal hand-stitch procedure, the transected edges of the antrum and the proximal remnant stomach are intracorporeally opened and circumferentially sewn in layer-to-layer fashion using laparoscopic sewing instruments. The second method is intracorporeal triangular anastomosis using a linear stapler, such as the extracorporeal approach reported by Nunobe et al. [11] in laparoscopy-assisted PPG. Lastly, the hybrid method combines manual and mechanical stitches. Recently, Koeda et al. [12] reported such a hybrid method whereby the posterior wall of the anastomosis was stapled with an endoscopic linear stapler while the anterior wall was treated by hand stitching. These three methods require complete opening of the transected stomach, which introduces mucosal protrusion, difficult manipulation, and intra-abdominal contamination. Moreover, hand stitching needs expert technical skill and a long operation time. In the piercing method, the remnant stomach is easily handled with only small gastrotomies and scant contamination as the mucosal protrusion is minimal and the anastomosis is fully mechanical, using three cartridges of a linear stapler similar to delta-shaped anastomosis. The piercing method can minimize the potential problems of the conventional approaches of end-to-end anastomosis in TLPPG.
In this small series, the piercing method needed a long operation time. However, both during and after the surgery, no specific problems were encountered in relation to this technique, apart from postoperative gastric stasis in one patient who needed fasting and infusion. One possible reason for the relatively long operation time may be that the piercing method was still under development up to the study period. Piercing the stomach, firing an endoscopic linear stapler to create a posterior anastomosis with both the proximal and distal transected edges of the stomach brought close together, and cutting the anterior walls of the proximal and distal remnant stomach, including the transected edges, to establish the anterior anastomosis are processes specific to the piercing method not required of other anastomotic methods. Both surgeons and assistants needed time to become used to performing these new procedures during the study period. The operation time will be shortened once the procedure is established as a standard maneuver. It is unclear whether gastric stasis in one patient was associated with the piercing method, as colitis induced by C. difficile toxin as an early postoperative event in a relatively elderly woman possibly affected the motility of the whole intestinal tract. Although the incidence of gastric stasis after TLPPG with gastrogastrostomy using the piercing method is expected to be equal to that after hand-stitch gastrogastrostomy, further data from a larger-scale study need to be collected and evaluated.
In the piercing method, the need for a curved tip and a black cartridge, which normally are not used in gastrointestinal surgery, is a limitation. However, these types of cartridges can be purchased easily and are not indispensable in the piercing method. Both the piercing technique and creation of the anterior wall can be performed using a regular cartridge, although a curved tip and a black cartridge help to make the piercing method safer and easier to perform.
In conclusion, the piercing method can safely create an intracorporeal mechanical end-to-end gastrogastrostomy in TLPPG. Piercing the stomach using an endoscopic linear stapler, which is essential to this approach, is an entirely new technique for the creation of gastrointestinal anastomosis, and should be considered a valid option for intracorporeal end-to-end gastrogastrostomy in TLPPG. Further experience and investigation will be required to verify whether the piercing method is a workable solution for patients undergoing TLPPG.
References
Kim JJ, Song KY, Chin HM, Kim W, Jeon HN, Park CH, Park SM (2008) Totally laparoscopic gastrectomy with various types of intracorporeal anastomosis using laparoscopic linear staplers: preliminary experience. Surg Endosc 22:436–442
Uyama I, Sugioka A, Fujita J, Komori Y, Matsui H, Soga R, Wakayama A, Okamamoto K, Ohyama A, Hasumi A (1999) Completely laparoscopic extraperigastric lymph node dissection for gastric malignancies located in the middle or lower third of the stomach. Gastric Cancer 2:186–190
Kanaya S, Gomi T, Momoi H, Momoi H, Tamaki N, Isobe H, Katayama T, Wada Y, Ohtoshi M (2002) Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg 195:284–287
Jiang X, Hiki N, Nunobe S, Fukunaga T, Kumagai K, Nohara K, Sano T, Yamaguchi T (2011) Postoperative outcomes and complications after laparoscopy-assisted pylorus-preserving gastrectomy for early gastric cancer. Ann Surg 253:928–933. https://doi.org/10.1097/SLA.0b013e3182117b24
Nunobe S, Sasako M, Saka M, Fukagawa T, Katai H, SanoT (2007) Symptom evaluation of long-term postoperative outcomes after pylorus-preserving gastrectomy for early gastric cancer. Gastric Cancer 10:167–172
Suh YS, Han DS, Kong SH, Kwon S, Shin CI, Kim WH, Kim HH, Lee HJ, Yang HK (2014) Laparoscopy-assisted pylorus-preserving gastrectomy is better than laparoscopy-assisted distal gastrectomy for middle-third early gastric cancer. Ann Surg 259:485–493. https://doi.org/10.1097/SLA.0b013e318294d142
Lee SW, Bouras G, Nomura E, Yoshikawa R, Tokuhara T, Nitta T, Tsunemi S, Tanigawa N (2010) Intracorporeal stapled anastomosis following laparoscopic segmental gastrectomy for gastric cancer: technical report and surgical outcomes. Surg Endosc 24:1774–1780. https://doi.org/10.1007/s00464-009-0803-x
Kumagai K, Hiki N, Nunobe S, Sekikawa S, Chiba T, Kiyokawa T, Jing X, Tanimura S, Sano T, Yamaguchi T (2015) Totally laparoscopic pylorus-preserving gastrectomy for early gastric cancer in the middle stomach: technical report and surgical outcomes. Gastric Cancer 18:183–187. https://doi.org/10.1007/s10120-014-0337-3
Nunobe S, Hiki N, Fukunaga T, Tokunaga M, Ohyama S, Seto Y, Yamaguchi T (2007) Laparoscopy-assisted pylorus-preserving gastrectomy: preservation of vagus nerve and infrapyloric blood flow induces less stasis. World J Surg 31:2335–2340
Kiyokawa T, Hiki N, Nunobe S, Honda M, Ohashi M, Sano T (2017) Preserving infrapyloric vein reduces postoperative gastric stasis after laparoscopic pylorus-preserving gastrectomy. Langenbecks Arch Surg 402:49–56. https://doi.org/10.1007/s00423-016-1529-6
Nunobe S, Kiyokawa T, Hatao F, Wada I, Shimizu N, Nomura S, Seto (2010) Triangulating stapling technique for anastomosis in laparoscopy-assisted pylorus-preserving gastrectomy. Dig Surg 27:359–363. https://doi.org/10.1159/000315013
Koeda K, Chiba T, Noda H, Nishinari Y, Segawa T, Akiyama Y, Iwaya T, Nishizuka S, Nitta H, Otsuka K, Sasaki A (2016) Intracorporeal reconstruction after pylorus-preserving gastrectomy for middle-third early gastric cancer: a hybrid technique using linear stapler and manual suturing. Langenbecks Arch Surg 401:397–402. https://doi.org/10.1007/s00423-016-1378-3
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Manabu Ohashi, Naoki Hiki, Satoshi Ida, Koshi Kumagai, Souya Nunobe, and Takeshi Sano have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary data Video 1 (WMV 373238 KB)
Rights and permissions
About this article
Cite this article
Ohashi, M., Hiki, N., Ida, S. et al. A novel method of intracorporeal end-to-end gastrogastrostomy in laparoscopic pylorus-preserving gastrectomy for early gastric cancer, including a unique anastomotic technique: piercing the stomach with a linear stapler. Surg Endosc 32, 4337–4343 (2018). https://doi.org/10.1007/s00464-018-6237-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6237-6