Abstract
Background
Peroral cholangioscopic lithotripsy is a useful procedure in patients with a normal gastrointestinal anatomy who have difficult-to-treat stones. We evaluated the usefulness of peroral direct cholangioscopy (PDCS) using single-balloon enteroscope (SBE) in patients with difficult-to-treat stones who had undergone Roux-en-Y reconstruction.
Methods
Among 118 patients (169 sessions) who underwent SBE-assisted endoscopic retrograde cholangiopancreatography to treat biliary stones after Roux-en-Y reconstruction, patients in whom it was difficult to remove biliary stones via a transpapillary or transanastomotic approach and difficult to switch to ultra-slim endoscope, were retrospectively enrolled. The biliary insertion success rate, procedure success rate, procedure time, and procedural complications were assessed. The SBE was inserted into the bile-duct, first using a free-hand technique, second using a guide wire, and third using the large balloon anchoring and deflation (LBAD) technique.
Results
A total of 11 patients (14 sessions) were enrolled in this study. The biliary insertion success rate was 100%. Bile-duct insertion was performed using a free-hand technique in 4 sessions, a guide wire in 3 sessions (rendezvous technique, 2 sessions), and the LBAD technique in 7 sessions. The procedure success rate was 86% in first session, and 100% in second session. The median procedure time was 81 min (range 49–137). The median procedure time in the bile-duct was 21.5 min (range 6–60). Mild pancreatitis occurred as a complication in one patient. The median follow-up was 528 days (range 282–764). No patient had stone recurrence.
Conclusions
PDCS using SBE is a useful procedure in patients with Roux-en-Y reconstruction. The LBAD technique is an useful technique of inserting SBE into the bile-duct.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The balloon enteroscope has considerably improved the outcome of endoscopic-lithotripsy in patients with Roux-en-Y (R-Y) reconstruction, which was previously considered challenging [1,2,3,4,5,6,7,8].
However, the stone removal remains challenging in some patients. For example, in patients with giant stones that are difficult to grasp, and in patients in whom only a long-type balloon enteroscope can reach the blind end [duodenal papillae or choledochojejunal anastomosis (CJA)].
For giant stones, mother-baby cholangioscopy is useful and has a high success rate with normal gastrointestinal (GI) anatomy [9], but this procedure is difficult to perform with R-Y reconstruction. Treatment using long-type balloon enteroscope cannot be performed similarly to that with normal GI anatomy, because the number of accessories is limited. In patients with gastrectomy, the bile-duct is often dilated even if stones are small, causing more space between accessories and the bile-duct and making stone removal difficult. For these reasons, endoscopic-lithotripsy might be more difficult to perform with R-Y reconstruction rather than with normal GI anatomy.
Peroral direct cholangioscopy (PDCS) [10] is a method that may overcome these difficulties with surgically altered anatomy [11,12,13,14,15,16,17]. In many studies of therapeutic PDCS with surgical altered anatomy, treatment procedures were performed after switching to an ultra-slim endoscope using the overtube-assisted technique (An overtube is left in the intestine, and the scope is exchanged.) [11, 12]. However, this technique has several limitations. Exchange of the scope is often difficult. For example, bowel shortening is precluded by adhesion, the overtube migrates at the time of scope exchange even after bowel shortening, patients with multiple loops, a long afferent loop. In such patients, balloon enteroscope-assisted PDCS may be effective. However, the usefulness of this procedure remains not to be fully defined [11, 13,14,15,16,17].
We report the usefulness of PDCS using single-balloon enteroscope (SBE-PDCS) in patients with R-Y reconstruction in whom it was difficult to remove biliary stones via a transpapillary or transanastomotic approach and difficult to switch to an ultra-slim endoscope.
Methods
Patients
From November 2012 through November 2016, we performed 169 sessions of SBE-assisted endoscopic-lithotripsy in 118 patients with R-Y reconstruction. Data were obtained from the endoscopic database of Kitasato University Hospital. Among 118 patients [169 sessions; R-Y gastrectomy, 126 sessions in 95 patients; R-Y choledochojejunostomy (CJS), 43 sessions in 23 patients], we investigated patients in whom SBE-PDCS was performed (Fig. 1).
A Outcomes of SBE-ERCP for Roux-en-Y gastrectomy. B Outcomes of SBE-ERCP for Roux-en-Y choledochojejunostomy. EUS endoscopic ultrasonography, PDCS peroral direct cholangioscopy, PTBD percutaneous biliary drainage, PTC percutaneous cholangiography, PTCS percutaneous cholangioscopy, R-Y Roux-en-Y, SBE-ERCP single-balloon enteroscope-assisted ERCP. *Including two cases of gastrointestinal perforation. †Including one case of gastrointestinal perforation
All patients provided written informed consent before the procedure. This study was approved by the institutional review board of our hospital.
All examinations were performed in patients who were sedated with pethidine (35 mg) and midazolam (3–10 mg) during intermittent monitoring of vital signs (including percutaneous carbon dioxide monitoring: cutaneous PO2/PCO2 monitor 9100, KOHKEN MEDICAL CO.,LTD. Tokyo, Japan). Antibiotics were given before and after the procedure. Bile-duct stones were diagnosed by abdominal ultrasonography, computed tomography (CT), and magnetic resonance cholangiopancreatography (MRCP).
Indication and contraindication
The indication of SBE-PDCS is patients in whom a transpapillary or choledochojejunal transanastomotic stone removal was difficult, and switching to an ultra-slim endoscope by the overtube-assisted technique was difficult because of multiple loops, a long afferent loop, and bile-duct diameter is more than 12 mm. Difficult-to-treat biliary stones were defined as giant or small stones that could not be grasped with a basket or removed with a stone removal balloon.
The contraindication of SBE-PDCS is patients with severe cholangitis, severe chronic obstructive pulmonary disease, bile-duct diameter less than 12 mm, performance status 4, and patients in whom informed consent was not obtained.
Endoscopic procedure
Endoscope and instruments
We used a short-type SBE (working length; 1520 mm, working channel diameter; 3.2 mm, distal end outer diameter; 9.2 mm, SIF-H290S, SIF-Y0015 series [prototype], Olympus Medical Systems, Tokyo, Japan) and a long-type SBE (working length; 2000 mm, working channel diameter; 2.8 mm, distal end outer diameter; 9.2 mm, SIF-Q260, Olympus Medical Systems). A 12- to 20-mm CRETM Balloon (Boston Scientific, Natick, MA, USA) and a 16- to 18-mm REN Biliary Balloon (Kaneka Medix Corp., Osaka, Japan) was used as a large balloon.
Techniques of bile-duct insertion
SBE was inserted into the bile-duct after dilation with a large balloon in all patients with papillae and with CJA if required. In patients with papillae, balloon dilation was performed until the notch disappeared, without endoscopic sphincterotomy. In patients with CJA, in principle, balloon dilatation was performed until the notch disappeared. However, in patients in whom the notch did not completely disappear even if the balloon was inflated to the target diameter, dilatation was performed for 2–3 min.
In all patients, SBE was inserted first using a free-hand technique. If insertion was difficult, a guide wire was placed in the bile-duct to serve as a landmark; fluoroscopy was performed as required. In patients who had undergone percutaneous transhepatic biliary drainage (PTBD) as pretreatment in another hospital, the PTBD-rendezvous technique was used (i.e., the guide wire was grasped endoscopically by the rendezvous technique and was pulled percutaneously and inserted). In patients in whom insertion was difficult using these methods, the large balloon anchoring and deflation (LBAD) technique was performed. A tip cap was used if necessary.
The LBAD technique was performed as follows (Video 1):
-
1.
The balloon size was determined on the basis of the bile-duct diameter. The duodenal papillae and CJA were dilated. After notch disappeared, the balloon was deflated to confirm the absence of perforation and bleeding.
-
2.
The balloon was re-inflated and was pulled and attached to the enteroscope.
-
3.
The enteroscope was pushed, and the tip of the enteroscope was inserted into the bile-duct.
-
4.
After the enteroscope was slightly inserted into the bile-duct, the balloon was deflated, and the enteroscope was inserted into the bile-duct while removing the balloon catheter.
Bile-duct insufflation
The bile-duct was insufflated with carbon dioxide (CO2), and physiological saline solution was injected through the forceps channel (equipped with a T-tube). To avoid the unwarranted CO2 insufflation, the CO2 insufflator was switched on and off to minimize insufflation. To avoid the elevation of bile-duct pressure, the overtube-balloon was deflated as much as possible during PDCS.
Stone removal
SBE-PDCS was performed on the same day that stone removal, via a transpapillary or transanastomotic approach, was judged to be difficult. Stone removal under PDCS was performed with CO2 insufflation. Electrohydraulic lithotripsy (EHL) was performed after filling the bile-duct with saline. Difficult to grasp small stones, debris, and pieces of crushed stones were washed with saline and removed by aspiration. In patients in whom more than 120 min were required for stone removal after reaching the blind end, a plastic stent was inserted if necessary, and second procedure was performed another day.
Evaluation of outcomes and follow-up
We retrospectively studied the following variables: biliary insertion success rate (reaching the bile-duct required for treatment), first procedure success rate (rate of complete stone removal in first session), final procedure success rate (final rate of complete stone removal in several sessions), procedure time (from insertion to removal of the endoscope), procedure time in bile-duct (from insertion into the bile-duct to removal), the contents of procedures, procedural complications, and stone recurrence rate. The severity of procedural complications was graded according to the system proposed by Cotton et al. [18]. The stone recurrence and residual stones were evaluated with abdominal ultrasonography, CT, and MRCP.
Results
A total of 11 patients (14 sessions; R-Y gastrectomy, 8 sessions in 6 patients; R-Y CJS, 6 sessions in 5 patients) were enrolled in this study. The study group comprised 6 men and 5 women with a median age of 77 years (range 54–86).
Reasons for the difficulty of switching to an ultra-slim endoscope were the long afferent loop requiring the use of long-type SBE in 8 sessions (Fig. 2A) and the difficulty in shortening the intestine because of the multiple loops and adhesion (Fig. 2B) in 6 sessions.
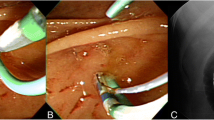
PDCS was indicated for the giant stones that were difficult to grasp in 8 sessions (Fig. 3), the removal of small stones and debris and casts that were difficult to grasp or remove using a balloon in 6 sessions.
The median maximum bile-duct diameter was 19 mm (range 12–29). The median major axis of stone was 18 mm (range 4–30). The median number of stones was 3 (range 1–10). A parapapillary diverticulum was found in 1 session.
The characteristics of the patients are shown in Tables 1 and 2.
The biliary insertion success rate was 100% (14/14). The first procedure success rate was 86% (12/14), the final procedure success rate was 100% (11/11). Stones were completely removed at the first SBE-PDCS in 9 patients. In Case 4 and Case 7, the time required for the first procedure was prolonged. Therefore, second SBE-PDCS was performed 7 and 4 days later, respectively, and the stones were completely removed. In Case 3, stones were completely removed at the first SBE-PDCS (Video 2). However, biliary cast syndrome (caused by bile-duct ulcer) occurred 1 month after the initial treatment, and second SBE-PDCS was performed to remove biliary casts. All biliary casts were completely removed in one session (Video 3).
The median procedure time was 81 min (range 49–137). The median procedure time in the bile-duct was 21.5 min (range 6–60).
The success rate of bile-duct insertion using a free-hand technique was 28.5% (4/14) (R-Y CJS, 4 sessions), using a guide-wire technique was 12.5% (1/8) (R-Y CJS, 1 session), using the PTBD-rendezvous technique was 100% (2/2) (R-Y gastrectomy, 2 sessions), and using the LBAD technique was 100% (7/7) (R-Y gastrectomy, 6 sessions; R-Y CJS, 1 session) (Fig. 4). The median diameter of the balloon used to perform the LBAD technique was 15 mm (range 12–16.5).
EHL was performed in 4 sessions (Video 2) and using a 4-wire basket in 2 sessions, a 5-prong grasping forceps in 6 sessions, and a 5-prong grasping forceps plus a balloon in 2 sessions (Video 4). Lavage and aspiration were performed in 6 sessions. Biliary dilatation was performed in 5 sessions. In addition to the stone removal, the removal of a proximally migrated biliary stent in 1 session (Fig. 5, Video 2), and bile-duct biopsy in 1 session (Video 3).
Bile-duct dilatation was performed to remove stones and casts at liver side of stricture caused by gallstone cholangitis (Cases 7-1, 7-2, 8, 10) and stricture caused by a bile-duct ulcer scar (Case 3-2). Stones and casts were removed under direct vision or fluoroscopy using a 5-prong grasping forceps.
The only procedural complication was mild pancreatitis in 1 session.
The stone recurrence rate was 0%, and the median follow-up was 528 days (range 282–764). We judged Case 3-2 was not procedural complication and recurrence of stone. Because biliary cast syndrome will be one of the natural history of bile-duct ulcer due to impacted stone.
In patients who underwent dilatation of bile-duct strictures (Cases 3-2, 7, 8, 10), the stricture recurrence rate was 25% (1/4 patients), and the median follow-up was 538 days (range 397–698). In Case 3-2, cholangitis caused by restenosis developed 279 days after dilatation, and a stent was placed.
The outcomes and procedural complications are summarized in Tables 2 and 3.
Discussion
We were interested in whether SBE could be successfully inserted into the bile-duct and in determining which method was appropriate. In our study, SBE could be inserted into the bile-duct in all patients, first using a free-hand technique, second using a guide wire and the PTBD-rendezvous technique, and third using the LBAD technique. A free-hand technique and a guide-wire technique succeeded only in patients with R-Y CJS. In patients with a papillae, these techniques were not successful because it was difficult to align the axis of the scope with the bile-duct and to secure a field of vision in the papillary region. On the other hand, in the LBAD technique, the use of a balloon makes it easy to align the scope with the axis of bile-duct, and allows the scope to be inserted while confirming the papillary region and the lower bile-duct through the balloon. A SBE was passively inserted in 4 of 7 patients using the LBAD technique (Video 1), all of whom had a duodenal papillae. The scope may be pulled into the bile-duct by the reaction created when the balloon catheter is deflated and removed. In our experience, we consider that the LBAD technique will be not so difficult to perform and may be more suitable than a free-hand and guide-wire technique in patient with papillae.
However, at the time of scope insertion into the bile-duct, bile-duct injury and papillary perforation can potentially occur as serious procedural complications. Endoscopic-papillary-large-balloon-dilation (EPLBD) has been reported to be effective and safe in patients with surgically altered anatomy [19]. However, bile-duct injury has been reported [20]. Particularly in patients with a papillae, caution should be exercised at the time of biliary insertion of SBE. Because SBE-PDCS was performed after EPLBD, the mechanical stress will be added to the torn and dilated papillae/lower bile-duct. Therefore, when performing the LBAD technique, we recommend that a balloon that can reach the target diameter at a lower pressure should be selected and a balloon larger in diameter than the lower bile-duct should not be selected. About the indication of bile-duct diameter, we consider that SBE-PDCS should not be performed with a bile-duct diameter of less than 12 mm from the viewpoint of complications. In our experience, endoscopic-lithotripsy was successfully performed via a transpapillary or transanastomotic approach with a bile-duct diameter less than 12 mm, and therapeutic procedure might be limited because diameter of SBE is 9.2 mm. In difficult-to-treat patients with a bile-duct diameter of less than 12 mm, other treatments should be considered (PDCS using an ultra-slim endoscope if the scope can be replaced, a transcutaneous treatment, surgical operation etc.).
Intraductal therapeutic procedures were successful in all patients, and easy to perform because conventional devices can be used, expanding the range of treatment options. Intraductal procedures have several advantages, including lavage and aspiration of crushed stones after EHL and high-resolution endoscopic images. In our study, the complete stone removal rate via a transpapillary approach was 90.1% (73/81) with R-Y gastrectomy. Transpapillary stone removal plus therapeutic PDCS increased the complete stone removal rate to 97.6% (79/81) (Fig. 1A). The complete stone removal rate of a transanastomotic approach with R-Y CJS was 77.3% (17/22), and transanastomotic stone removal plus therapeutic PDCS increased the complete stone removal rate to 100% (22/22) (Fig. 1B). Therefore, SBE-PDCS was considered to be an effective procedure and to increase the complete stone removal rate with R-Y reconstruction.
There were no serious procedural complications in our study (mild pancreatitis in one patient). However, complications after biliary insertion include air embolism and bacteremia caused by cholangiovenous reflux. These are serious and fatal complication.
In our study, antibiotics were given before and after treatment, and no patient had infection or infectious symptoms. Prophylactic treatment with antibiotics should be administered before and after procedures because ERCP combined with cholangioscopy has been reported to increase the risk of bacteremia [27].
In previous studies, air embolism was consistently associated with room air [21, 22], and CO2 insufflation has been reported to be safe [10,11,12, 23,24,25]. However, one study reported that fatal systemic gas embolism was caused by CO2 insufflation in patient who underwent YAG laser lithotripsy during overtube-assisted PDCS using an ultra-slim endoscope [26]. Unlike an ultra-slim endoscope, when SBE is inserted into the bile-duct, the scope can easily wedge into the duodenal papillae or the site of CJA, thereby increasing intrabiliary pressure. Therefore, respiratory status should be checked, including CO2 monitoring, and care should be exercised to ensure enough dilation of the duodenal papillae and the CJA and to minimize CO2 insufflation. In the patient described above, treatment was performed in the bile-duct while leaving the balloon attached to the overtube inflated. We have attempted to deflate the balloon as much as possible during PDCS. This step might prevent the elevation of bile-duct pressure. This is because, this step prevents the elevation of intra-intestinal pressure between the blind end and the overtube-balloon, and promotes the flow of CO2 into the anal side of intestine from bile-duct. Although CO2 embolism was reported only in one patient, it is a fatal complication. Therefore, measures to prevent CO2 embolism are essential whenever possible, and our methods of bile-duct insufflation might prevent CO2 embolism. In our study, SBE-PDCS was safe (the only procedural complication was mild pancreatitis in one session). However, our study was a small retrospective and single endoscopic center investigation. The Safety of therapeutic PDCS thus remains to be established.
Therefore, SBE-PDCS should currently be limited to patients with a bile-duct diameter of more than 12 mm in whom a transpapillary or transanastomotic approach is difficult. Further studies of larger numbers of patients are needed to confirm our results.
Conclusions
SBE-PDCS is useful and increases the complete stone removal rate in patients with R-Y anastomosis. The LBAD technique is considered a promising procedure in patients with duodenal papillae.
References
Shimatani M, Matsushita M, Takaoka M et al (2009) Effective “short” double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy 41(10):849–854
Siddiqui AA, Chaaya A, Shelton C et al (2013) Utility of the short double-balloon enteroscope to perform pancreaticobiliary interventions in patients with surgically altered anatomy in a US multicenter study. Dig Dis Sci 58(3):858–864
Yamauchi H, Kida M, Okuwaki K et al (2013) Short-type single balloon enteroscope for endoscopic retrograde cholangiopancreatography with altered gastrointestinal anatomy. World J Gastroenterol 19(11):1728–1735
Ishii K, Itoi T, Tonozuka R et al (2016) Balloon enteroscopy-assisted ERCP in patients with Roux-en-Y gastrectomy and intact papillae (with videos). Gastrointest Endosc 83(2):377–386
Iwai T, Kida M, Yamauchi H et al (2014) Short-type and conventional single-balloon enteroscopes for endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: single-center experience. Dig Endosc 26(Suppl 2):156–163
Skinner M, Popa D, Neumann H et al (2014) ERCP with the overtube-assisted enteroscopy technique: a systematic review. Endoscopy 46(7):560–572
Yamauchi H, Kida M, Imaizumi H et al (2015) Innovations and techniques for balloon-enteroscope-assisted endoscopic retrograde cholangiopancreatography in patients with altered gastrointestinal anatomy. World J Gastroenterol 21(21):6460–6469
Inamdar S, Slattery E, Sejpal DV et al (2015) Systematic review and meta-analysis of single-balloon enteroscopy-assisted ERCP in patients with surgically altered GI anatomy. Gastrointest Endosc 82(1):9–19
Binmoeller KF, Brückner M, Thonke F et al (1993) Treatment of difficult bile duct stones using mechanical, electrohydraulic and extracorporeal shock wave lithotripsy. Endoscopy 25:201–206
Moon JH, Ko BM, Choi HJ et al (2009) Direct per-oral cholangioscopy using an ultra-slim upper endoscope for the treatment of retained bile duct stones. Am J Gastroenterol 104:2729–2733
Itoi T, Sofuni A, Itokawa F et al (2012) Diagnostic and therapeutic peroral direct cholangioscopy in patients with altered GI anatomy (with videos). Gastrointest Endosc 75(2):441–449
Matsumoto K, Tsutsumi K, Kato H et al (2016) Effectiveness of peroral direct cholangioscopy using an ultraslim endoscope for the treatment of hepatolithiasis in patients with hepaticojejunostomy (with video). Surg Endosc 30(3):1249–1254
Okabe Y, Kuwaki K, Kawano H et al (2010) Direct cholangioscopy using a double-balloon enteroscope: choledochojejunostomy with intraductal biliary carcinoma. Dig Endosc 22(4):319–321
Law R, Topazian M, Baron TH (2013) Endoscopic resection of hilar papillomatosis after Whipple procedure for ampullary adenoma. Gastrointest Endosc 78(2):226
Kao KT, Batra B (2014) Single-balloon-assisted ERCP with electrohydraulic lithotripsy for the treatment of a bile duct stone in a patient with a hepaticojejunostomy. Gastrointest Endosc 80(6):1173
Yamauchi H, Kida M, Miyazawa S et al (2015) Electrohydraulic lithotripsy under peroral direct cholangioscopy using short-type single-balloon enteroscope for large common bile duct stone in patients with Roux-en-Y gastrectomy. Endoscopy 47:E240–E241
Hakuta R, Kogure H, Isayama H et al (2015) Electrohydraulic lithotripsy of large bile duct stones under direct cholangioscopy with a double-balloon endoscope. Endoscopy 47:E519–E520
Cotton PB, Eisen GM, Aabakken L et al (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71(3):446–454
Oana S, Shibata S, Matsuda N et al (2015) Efficacy and safety of double-balloon endoscopy-assisted endoscopic papillary large-balloon dilatation for common bile duct stone removal. Dig Liver Dis 47(5):401–404
Lee YS, Moon JH, Ko BM et al (2010) Endoscopic closure of a distal common bile duct perforation caused by papillary dilation with a large-diameter balloon (with video). Gastrointest Endosc 72(3):616–618
Romberg C (2009) Systemic air embolism after ERCP: a case report and review of the literature (with video). Gastrointest Endosc 70(5):1043–1045
van Boxel GI, Hommers CE, Dash I et al (2010) Myocardial and cerebral infarction due to massive air embolism following endoscopic retrograde cholangiopancreatography (ERCP). Endoscopy 42(Suppl 2):E80–E81
Ueki T, Mizuno M, Ota S et al (2010) Carbon dioxide insufflation is useful for obtaining clear images of the bile duct during peroral cholangioscopy (with video). Gastrointest Endosc 71(6):1046–1051
Doi S, Yasuda I, Nakashima M et al (2011) Carbon dioxide insufflation vs. conventional saline irrigation for peroral video cholangioscopy. Endoscopy 43(12):1070–1075
Itoi T, Nageshwar Reddy D et al (2014) Clinical evaluation of a prototype multi-bending peroral direct cholangioscope. Dig Endosc 26(1):100–107
Kondo H, Naitoh I, Nakazawa T et al (2016) Development of fatal systemic gas embolism during direct peroral cholangioscopy under carbon dioxide insufflation. Endoscopy 48(Suppl 1):E215–E216
Thosani N, Zubarik RS, Kochar R et al (2016) Prospective evaluation of bacteremia rates and infectious complications among patients undergoing single-operator choledochoscopy during ERCP. Endoscopy 48(5):424–431
Ackowledgements
The authors thank Olympus Medical Systems (Tokyo, Japan) for providing the prototype instruments used in this study.
Funding
The prototype instruments used in this study were provided by Olympus Medical Systems (Tokyo, Japan).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Hiroshi Yamauchi, Mitsuhiro Kida, Kosuke Okuwaki, Shiro Miyazawa, Takaaki Matsumoto, Kazuho Uehara, Eiji Miyata, Rikiya Hasegawa, Toru Kaneko, Issaree Laopeamthong, Yang Lei, Tomohisa Iwai, Hiroshi Imaizumi, and Wasaburo Koizumi have no conflicts of interest or financial ties to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
LBAD technique The papillae was dilated with a 12-mm large balloon, and the balloon was pulled and attached to the enteroscope. Subsequently, the tip of the enteroscope was inserted into the lower bile-duct by the push technique, and the balloon was then removed while deflating. The enteroscope was passively inserted into the bile-duct. Supplementary material 1 (MP4 9737 kb)
EHL for an impacted bile-duct stone and endoscopic retrieval of a proximally migrated biliary stent (Case 3-1) After cholangiography, EPLBD was performed using a 15 mm balloon. A short-type SBE was inserted into the bile-duct using the LBAD technique and showed a proximally migrated biliary stent (that was placed for treatment of acute obstructive suppurative cholangitis before 7 days), an impacted stone, and a bile-duct ulcer associated with the stone. Electrohydraulic lithotripsy (EHL) (Lithotron EL-21 and EHL probes (A 9411) (both manufactured by Walz Elektronik, Rohrdorf, Germany) was performed to crush the impacted stone. The migrated stent was grasped with a snare and was removed along with the scope. Supplementary material 2 (MP4 25493 kb)
A biopsy of an elevated lesion in the bile-duct and biliary dilatation (Case 3-2) One month after stone removal (Video 2), contrast-enhanced CT showed an elevated lesion in the bile-duct. Cholangiography revealed a stricture in the common hepatic duct, and a defect was seen at liver side of stricture. Intraductal ultrasonography showed thickening of the wall at the site of the narrowed bile-duct. A hyperechoic region suggestive of debris was seen at liver side of stricture. A short-type SBE was inserted into the bile-duct, using the LBAD technique. An elevated lesion was seen in the common hepatic duct. Debris was removed with a grasping forceps and a 5-prong forceps. Endoscopic examination suggested that the elevated lesion was benign. However, a biopsy of the elevated lesion was performed to rule out the presence of malignant disease. The stricture was dilated with a balloon. The biliary cast syndrome was diagnosed by histopathological examination of debris tissue. Supplementary material 3 (MP4 22467 kb)
Biliary dilation and stone removal using a 5-prong grasping forceps (Case 7) MRCP showed multiple stones in the left and right intrahepatic bile-ducts. Because the stones could not be removed from the left hepatic duct, direct cholangioscopy was performed and showed a stricture at the origin of the left hepatic duct. The stricture was dilated with a 12-mm balloon. Stones in the left hepatic duct were removed using a 5-prong grasping forceps. After stone removal, an enteroscope was inserted into the left hepatic duct to wash the bile-duct and to confirm the absence of residual stones. Supplementary material 4 (MP4 14787 kb)
Rights and permissions
About this article
Cite this article
Yamauchi, H., Kida, M., Okuwaki, K. et al. Therapeutic peroral direct cholangioscopy using a single balloon enteroscope in patients with Roux-en-Y anastomosis (with videos). Surg Endosc 32, 498–506 (2018). https://doi.org/10.1007/s00464-017-5742-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-017-5742-3