Abstract
Propose
The use of robotic surgery and neoadjuvant chemoradiation therapy (CRT) for rectal cancer is increasing steadily worldwide. However, there are insufficient data on long-term outcomes of robotic surgery in this clinical setting. The aim of this study was to compare the 5-year oncological outcomes of laparoscopic vs. robotic total mesorectal excision for mid–low rectal cancer after neoadjuvant CRT.
Materials and methods
One hundred thirty-eight patients who underwent robotic (n = 74) or laparoscopic (n = 64) resections between January 2006 and December 2010 for mid and low rectal cancer after neoadjuvant CRT were identified from a prospective database. The long-term oncological outcomes of these patients were analyzed using prospective follow-up data.
Results
The median follow-up period was 56.1 ± 16.6 months (range 11–101). The 5-year overall survival (OS) rate of the laparoscopic and robotic groups was 93.3 and 90.0 %, respectively, (p = 0424). The 5-year disease-free survival (DFS) rate was 76.0 % (laparoscopic) vs. 76.8 % (robotic) (p = 0.834). In a subgroup analysis according to the yp-stage (complete pathologic response, yp-stage I, yp-stage II, or yp-stage III), the between-group oncological outcomes were not significantly different. The local recurrence rate was 6.3 % (laparoscopic, n = 4) vs. 2.7 % (robotic, n = 2) (p = 0.308). The systemic recurrence rate was 15.6 % (laparoscopic, n = 10) vs. 18.9 % (robotic, n = 14) (p = 0.644). All recurrences occurred within less than 36 months in both groups. The median period of recurrence was 14.2 months.
Conclusion
Robotic surgery for rectal cancer after neoadjuvant CRT can be performed safely, with long-term oncological outcomes comparable to those obtained with laparoscopic surgery. More large-scale studies and long-term follow-up data are needed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Laparoscopic total mesorectal excision (TME) is a technically demanding procedure because the surgical space of the rectum is surrounded by a narrow bony pelvis and the laparoscopic instruments have technical limitations. Recently, large randomized trials reported that laparoscopic rectal surgery was nearly equivalent to open surgery with regard to oncological safety [1–3], but some studies reported that the use of laparoscopic resection compared with open resection for rectal cancer failed to meet the criteria for non-inferiority of pathological outcomes, and that there was insufficient evidence to support the routine use of laparoscopic surgery [4, 5].
Neoadjuvant chemoradiation therapy (CRT) is commonly incorporated into the multimodal treatment of locally advanced rectal cancers and is associated with downstaging of the tumor, more sphincter-preserving procedures, and decreased local recurrence [6, 7]. However, CRT can result in slightly more postoperative complications and adds some technical difficulty to the pelvic dissection, because the tissue edema and fibrosis induced by CRT may blur the dissection planes [8].
A robotic surgical system has some advantages that might overcome limitations associated with laparoscopic rectal surgery. It allows the surgeon to work in an ergonomic position and offers improved dexterity. In addition, a robotic system provides seven degrees of freedom, motion scaling to eliminate physiological tremor, a stable camera platform, stereoscopic views, and three-dimensional imaging [9–11]. The use of robotic surgery for rectal cancer is continuing to increase steadily worldwide. Studies of short- and long-term outcomes of robotic surgery for rectal cancer have demonstrated its feasibility and oncologic safety, although there have been no well-designed prospective randomized trials demonstrating the oncologic safety of robotic TME for rectal cancer [12–15].
In a previous study, we reported that 3-year oncological outcomes of robotic and laparoscopic surgery for mid–low rectal cancer after neoadjuvant CRT were comparable [16]. The present follow-up study was based on an analysis of the 5-year oncological outcomes of the same patients. The aim of the present study was to compare the 5-year oncological outcomes of laparoscopic vs. robotic TME for mid–low rectal cancer after neoadjuvant CRT.
Materials and methods
Between January 2006 and December 2010, 138 consecutive patients undergoing robotic (n = 74) and laparoscopic TME (n = 64) for mid and low rectal adenocarcinomas (i.e., 0–12 cm from the anal verge) after neoadjuvant CRT were identified from a prospective database. These patients received long-course neoadjuvant CRT (five cycles of fluorouracil-based chemotherapy and 50.4 Gy) because they were T3 or T4 and/or node positive. Stage IV was excluded from the present study. All of the patients underwent a colonoscopy, biopsy, and staging scan (computed tomography [CT] scan of the chest, abdomen, and pelvis, and magnetic resonance imaging [MRI] of the pelvis). Some patients underwent positron emission tomography (PET) scans and endorectal ultrasound. The operation was to have been performed within 6–8 weeks of the final radiation treatment.
For bowel preparation, colonic lavage was performed the day before the operation, and the patient was given an antibiotic prophylaxis. The laparoscopic and robotic rectal TME techniques have been described in our previous studies [17, 18]. The surgical strategy regarding sphincter-saving procedures was determined based on preoperative MRI staging (corono-axial), and invasion of the levator ani muscle and external sphincter muscle was considered an indication for abdominoperineal resection [19]. The decision of lap vs. robotic was made based on patient’s decision after an explanation about the each procedures such as cost, insurance coverage, and complications and a surgeon’s preference to robotic surgery. For 3 years after surgery, measurement of serum carcinoembryonic antigen (CEA) levels and chest radiography was performed every 2 or 3 months. After 3 years, the follow-up interval was changed to every 6 months. Chest and abdomino-pelvic CT scans were performed annually. The study was approved by the local ethics committee.
Evaluation of TME completeness
The TME quality was scored by surgeons using three grades, as defined by the Dutch TME trial [20]. The following definitions were used to macroscopically assess the quality of the TME completeness: complete, intact mesorectum with minimal irregularities with a depth of less than 5 mm, no coning toward the distal margin of the rectum and a smooth circumferential resection margin; nearly complete, most of the mesorectum has been removed, but with irregularity of the mesorectal surface, and moderate coning of the specimen toward the distal resection margin; and incomplete, little to bulk of the mesorectum remaining with defects extending to the muscularis propria and/or an irregular circumferential resection margin.
Statistical analysis
All of the statistical analyses were performed using SAS version 9.1.3 (SAS Institute Inc., Cary, NC) and SPSS software, version 18.0 (SPSS, Chicago, IL). Categorical variables were analyzed using the Chi-sqaure or Fisher’s exact test, and continuous variables were analyzed using the Student’s t test or Mann–Whitney U rank test. Overall survival (OS) time was defined as the time between the date of diagnosis and the date of death or last follow-up visit, and disease-free survival (DFS) time was defined as the time elapsed between the date of diagnosis and tumor progression. Patients who died from other causes or were alive at the most recent follow-up were treated as censored in the analysis of disease-free survival time. Survival curves and disease-free intervals were obtained using the Kaplan–Meier method. The differences in OS and DFS rate were assessed using the log-rank test.
Results
Patients’ characteristics
There were no significant between-group differences in the age, sex, body mass index (BMI), ASA status, tumor stage, or history of previous abdominal operations (Table 1). The median age of the patients undergoing surgery was 65.4 ± 11.8 years (33–91) according to the last follow-up date (August 2015). The patients in both groups had a low BMI (laparoscopic: 22.7, robotic: 23.4) when the surgery was performed, and they were predominantly male (70 %) and in a low-risk category based on their ASA status.
Sphincter preservation rates were high, and the preservation rates of the laparoscopic and robotic group were not significantly different (95 vs. 98 %, p = 0.444). Although not statistically significant, more patients in the robotic group underwent robotic-assisted coloanal anastomoses and intersphincteric resections (26/74, 33 %) compared to the laparoscopic group (15/64, 23 %).
The operation time was longer in the robotic group. The mean operation time was 311.6 ± 79.8 min in the laparoscopic group vs. 365.2 ± 108.4 min in the robotic group (p = 0.033). The mean tumor location from the anal verge was 6.7 ± 2.6 cm in the laparoscopic group vs. 5.3 ± 2.3 cm in the robotic group (p = 0.495). There were four (6.3 %) conversions in the laparoscopic group and one (1.4 %) conversion in the robotic group (p = 0.182) (Table 1).
Postoperative pathological outcomes
There was no significant difference between the two groups in the yp-TNM stage (complete pathologic response, yp-stage I, yp-stage II, or yp-stage III), ypT, or ypN. The complete pathologic response rate was 12.5 % (n = 8) in the laparoscopic surgery group and 24.3 % (n = 18) in the robotic surgery group (Table 2). The distributions of the response to neoadjuvant CRT (Mandard grade) were similar between the two groups (p = 0.906). The number of harvested lymph nodes, proximal/distal resection margins, and circumferential resection margins was not significantly different between the two groups (Table 2). According to the TME grade, 63 specimens (98.4 %) were classified as complete and one (1.6 %) as nearly complete in the laparoscopic group, and 71 specimens (95.9 %) were classified as complete and three (4.1 %) as nearly complete in the robotic group.
Oncological outcomes
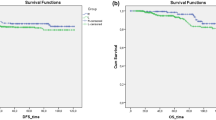
With a mean follow-up of 56.1 ± 16.6 months (range 11–101), the 5-year DFS was comparable between groups: 76.0 % (laparoscopic surgery) vs. 76.8 % (robotic surgery (p = 0.834) (Table 3) (Fig. 1). The 5-year OS rate for the laparoscopic and robotic groups was 93.3 and 90.0 %, respectively (p = 0.424). Compared to the previously reported 3-year DFS10, the 5-year DFS was decreased slightly both in the laparoscopic group (from 78.8 to 76.0 %) and in the robotic group (from 77.7 to 76.8 %). Compared to the 3-year OS10, the 5-year OS was unchanged in the robotic group, whereas the 5-year OS was increased (from 92.1 to 93.3 %) in the laparoscopic group. Although the 5-year OS and DFS were somewhat lower than the 3-year OS and DFS, they were comparable.
According to the subtype of the yp-stage, there was no significant between-group difference. Five-year DFS after laparoscopic and robotic surgery, respectively, was 71.9 and 88.9 % in yp-stage 0 (clinical remission) (p = 0.314), 84.6 and 80.8 % in yp-stage I (p = 0.762), 82.2 and 76.2 % in yp-stage II (p = 0.762), and 65.0 and 61.1 % in yp-stage III (p = 0.845) (Fig. 2). Five-year OS after laparoscopic and robotic surgery, respectively, was 100.0 and 94.4 % in yp-stage 0 (clinical remission) (p = 0.533), 100 and 87.1 % in yp-stage I (p = 0.187), 95.0 and 89.9 % in yp-stage II (p = 0.556), and 84.4 and 88.9 % in yp-stage III (p = 0.841) (Table 3) (Fig. 3).
Recurrence patterns
The local recurrence rate was 6.3 % in the laparoscopic group and 2.7 % in the robotic group (p = 0.308) (Table 4). The site of local recurrence was the pelvic side wall (laparoscopic surgery: n = 3, 4.7 %, robotic surgery: n = 2, 2.7 %) and ureter (laparoscopic surgery: n = 1, 1.6 %). The systemic recurrence rate was 15.6 % in the laparoscopic group and 18.9 % in the robotic group (p = 0.644). The site of systemic recurrence was the lung (laparoscopic surgery: n = 3, 4.7 %, robotic surgery: n = 10, 13.5 %), liver (laparoscopic surgery: n = 10, 13.5 %), para-aortic node (laparoscopic surgery: n = 1, 1.6 %, robotic surgery: n = 1, 1.4 %), and spine (laparoscopic surgery: n = 2, 3.1 %, robotic surgery: n = 0, 0 %) (Table 4). All recurrences occurred in less than 36 months in both groups. The median period of recurrence was 13.1 ± 6.2 months (range 4–27) in the laparoscopic group and 15.3 ± 7.9 months (range 1–30) in the robotic surgery group (Fig. 4).
Discussion
TME is an important surgical concept in treating rectal cancer. The outcome of rectal surgery has improved substantially during the past two decades because of the introduction of total mesorectal excision [21, 22]. The TME procedure must be performed sequentially during the posterior/deep posterior, anterior, posterolateral, and circumferential pelvic dissection, and the surgeon must take care to preserve the pelvic autonomic nerve (superior/bilateral hypogastric nerves, pelvic plexus, and neurovascular bundles) to avoid postoperative sexual and voiding dysfunction after the TME procedure [23].
Since the first laparoscopic TME for rectal cancer was reported, there have been several prospective randomized studies about the efficacy of laparoscopic rectal surgery for rectal cancer [1–3]. However, laparoscopic TME for rectal cancer is regarded as technically demanding, because the rectum is located concavely along the curved sacrum in a narrow and deep pelvic cavity and the complexity of the anatomy in the pelvic cavity makes dissection challenging. Two randomized clinical trials, ACOSOG Z6051 and ALaCaRT, reported that the use of laparoscopic resection compared with open resection for rectal cancer failed to meet the criteria for non-inferiority of pathological outcomes and that there was insufficient evidence for the routine use of laparoscopic surgery [4, 5].
According to the guidelines of the National Comprehensive Cancer Network, neoadjuvant CRT is generally administered to patients with mid–low rectal cancer [24]. The aim of neoadjuvant CRT for rectal cancer is to improve the resectability by downstaging, increasing sphincter-saving rates, and decreasing local recurrence rates [7, 25]. However, neoadjuvant CRT can cause changes in the pelvic tissue (i.e., fibrosis and hydro-dense tissue). As a result, surgeons often find it difficult to locate an appropriate anatomic dissection line for TME. These factors can affect TME quality during laparoscopic resection for rectal cancer.
Robotic surgery aims to overcome limitations associated with laparoscopic surgery for rectal cancer. Robotic TME for rectal cancer has various advantages including a stable platform, camera control, fine scaling of movements, high definition three-dimensional views, elimination of physiological tremors, improved endo-wrist function, and reduced operator fatigue compared to laparoscopic TME. Recently, a robotic interface for rectal cancer has begun to be used for various complex procedures including selective levator excision, lateral pelvic lymph node dissection, pelvic exenteration, single-port surgery, and transanal TME [26–31]. Robotic surgery for rectal cancer could overcome difficulties associated with TME in the “frozen” pelvis after CRT. However, very few studies have exclusively focused upon patients in this setting using a robotic surgical system [16, 32, 33].
There are some studies reporting equivalent oncologic results between laparoscopic and robotic surgery for rectal cancer. Cho et al. [14] reported comparable short- and long-term outcomes between 278 laparoscopic and 278 robotic resections for rectal cancer in their case-matched retrospective study. A 5-year OS rate and DFS rate for laparoscopic versus robotic TME were 93.1 vs. 92.2 % and 79.6 vs. 81.8 %, respectively. Park et al. [34]. reported no significant differences in the 5-year OS, DFS, and local recurrence rates between patients treated with robotic and laparoscopic surgery for rectal cancer (robot, n = 133; laparoscopy, n = 84). In that retrospective single institution study, the 5-year OS, DFS, and local recurrence rates for laparoscopic versus robotic rectal surgery were 93.5 vs. 92.8, 78.7 vs. 81.9 %, and 1.2 vs. 2.3 %, respectively. In the present study, 5-year OS, DFS, and local recurrence rates in the laparoscopic and robotic group were 93.3 vs. 90.0 %, 76.0 vs. 76.8 %, and 6.3 vs. 2.7 %, respectively, during the mean follow-up period of 56 months and our results show comparable oncologic control between the laparoscopic and robotic groups. In previous studies, 8.9–80.5 % of patients underwent neoadjuvant CRT prior to robotic surgery for rectal cancer compared with 5.4–56.0 % of laparoscopic surgery patients [15, 35–38]; however, in the present study, all of the patients underwent neoadjuvant CRT for advanced rectal cancer. Our results show that minimally invasive surgery for mid and low rectal cancer after neoadjuvant long-course chemoradiotherapy (LCRT) can be safe and feasible.
Objective parameters that express the quality of rectal dissection are rate of circumferential resection margins involvement and involvement of the mesorectum. In studies of TME specimens in robotic and laparoscopic surgery, most reported that the positivity rate of the circumferential resection margin in robotic surgery was similar to that obtained in laparoscopic surgery [12, 14]. In this study, the rates of involved circumferential resection margins were not significantly different between the two groups. Regarding to the TME completeness, Baik et al. [39]. reported that macroscopic grading of the TME specimen in the robotic group was complete in 17 cases and nearly complete in one case, and in the laparoscopic group, grading was complete in 13 cases and nearly complete in three cases in their pilot randomized trial where patients were randomly assigned to receive 18 robotic procedures or 16 laparoscopic procedures. In that study, the quality of the mesorectum was scored using three grades (complete, nearly complete, and incomplete) by a pathologist who had no clinical information about the patients. In our study, 63 specimens (98.4 %) were classified as complete and one (1.6 %) as nearly complete in the laparoscopic group, and 71 specimens (95.9 %) were classified as complete and three (4.1 %) as nearly complete in the robotic group, although the quality of TME completeness was evaluated by the operator surgeon in the operating room.
Recently, Baek et al. [40]. classified 182 patients who underwent robotic surgery for rectal cancer into easy, moderate, and difficult groups by MRI-based pelvimetry and there was no difference between the groups in terms of operative and pathologic outcomes, including operation time. They concluded that the surgical robotic system may overcome challenges associated with difficult pelvic anatomy. Although there was no difference between the groups in terms of long-term oncologic outcomes in our study, a randomized prospective comparative study with stricter inclusion criteria such as difficult male pelvis and lower rectum is needed to evaluate the benefit of robotic surgery in these patients in the future.
The current study has several limitations, including its retrospective nature, significant selection biases, small sample size, and lack of data such as urinary and sexual functional outcomes. Although not statistically significant, robotic surgery was performed in patients with lower rectal cancer and more patients in the robotic group underwent robotic-assisted coloanal anastomoses and intersphincteric resections with a significantly higher stoma rate.
In conclusion, robotic surgery for rectal cancer after neoadjuvant CRT can be performed safely, with long-term oncological outcomes comparable to those obtained with laparoscopic surgery in the present study.
References
Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, Choi HS, Kim DW, Chang HJ, Kim DY, Jung KH, Kim TY, Kang GH, Chie EK, Kim SY, Sohn DK, Kim DH, Kim JS, Lee HS, Kim JH, Oh JH (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15(7):767–774
van der Pas MH, Haglind E, Cuesta MA, Furst A, Lacy AM, Hop WC, Bonjer HJ (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14(3):210–218
Bonjer HJ, Deijen CL, Haglind E (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 373(2):194
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M, Peters WR Jr, Maun D, Chang G, Herline A, Fichera A, Mutch M, Wexner S, Whiteford M, Marks J, Birnbaum E, Margolin D, Larson D, Marcello P, Posner M, Read T, Monson J, Wren SM, Pisters PW, Nelson H (2015) Effect of laparoscopic-assisted resection versus open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314(13):1346–1355
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ, Davies L, Wilson K, Hague W, Simes J (2015) Effect of laparoscopic-assisted resection versus open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314(13):1356–1363
Minsky BD, Cohen AM, Kemeny N, Enker WE, Kelsen DP, Saltz L, Frankel J (1993) The efficacy of preoperative 5-fluorouracil, high-dose leucovorin, and sequential radiation therapy for unresectable rectal cancer. Cancer 71(11):3486–3492
van Gijn W, Marijnen CA, Nagtegaal ID, Kranenbarg EM, Putter H, Wiggers T, Rutten HJ, Pahlman L, Glimelius B, van de Velde CJ (2011) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 12(6):575–582
Marijnen CA, Kapiteijn E, van de Velde CJ, Martijn H, Steup WH, Wiggers T, Kranenbarg EK, Leer JW (2002) Acute side effects and complications after short-term preoperative radiotherapy combined with total mesorectal excision in primary rectal cancer: report of a multicenter randomized trial. J Clin Oncol 20(3):817–825
Baik SH, Lee WJ, Rha KH, Kim NK, Sohn SK, Chi HS, Cho CH, Lee SK, Cheon JH, Ahn JB, Kim WH (2008) Robotic total mesorectal excision for rectal cancer using four robotic arms. Surg Endosc 22(3):792–797
Kim NK, Kang J (2010) Optimal total mesorectal excision for rectal cancer: the role of robotic surgery from an expert’s view. J Korean Soc Coloproctol 26(6):377–387
Bae SU, Baek SJ, Hur H, Baik SH, Kim NK, Min BS (2015) Robotic left colon cancer resection: a dual docking technique that maximizes splenic flexure mobilization. Surg Endosc 29(6):1303–1309
Kwak JM, Kim SH, Kim J, Son DN, Baek SJ, Cho JS (2011) Robotic vs laparoscopic resection of rectal cancer: short-term outcomes of a case-control study. Dis Colon Rectum 54(2):151–156
Kuhry E, Schwenk W, Gaupset R, Romild U, Bonjer J (2008) Long-term outcome of laparoscopic surgery for colorectal cancer: a cochrane systematic review of randomised controlled trials. Cancer Treat Rev 34(6):498–504
Cho MS, Baek SJ, Hur H, Min BS, Baik SH, Lee KY, Kim NK (2015) Short and long-term outcomes of robotic versus laparoscopic total mesorectal excision for rectal cancer: a case-matched retrospective study. Medicine (Baltimore) 94(11):e522
Kang J, Yoon KJ, Min BS, Hur H, Baik SH, Kim NK, Lee KY (2013) The impact of robotic surgery for mid and low rectal cancer: a case-matched analysis of a 3-arm comparison–open, laparoscopic, and robotic surgery. Ann Surg 257(1):95–101
Saklani AP, Lim DR, Hur H, Min BS, Baik SH, Lee KY, Kim NK (2013) Robotic versus laparoscopic surgery for mid-low rectal cancer after neoadjuvant chemoradiation therapy: comparison of oncologic outcomes. Int J Colorectal Dis 28(12):1689–1698
Park YA, Kim JM, Kim SA, Min BS, Kim NK, Sohn SK, Lee KY (2010) Totally robotic surgery for rectal cancer: from splenic flexure to pelvic floor in one setup. Surg Endosc 24(3):715–720
Kim JS, Cho SY, Min BS, Kim NK (2009) Risk factors for anastomotic leakage after laparoscopic intracorporeal colorectal anastomosis with a double stapling technique. J Am Coll Surg 209(6):694–701
Saklani AP, Bae SU, Clayton A, Kim NK (2014) Magnetic resonance imaging in rectal cancer: a surgeon’s perspective. World J Gastroenterol 20(8):2030–2041
Nagtegaal ID, van de Velde CJ, van der Worp E, Kapiteijn E, Quirke P, van Krieken JH (2002) Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol 20(7):1729–1734
Heald RJ, Ryall RD (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1(8496):1479–1482
Martling AL, Holm T, Rutqvist LE, Moran BJ, Heald RJ, Cedemark B (2000) Effect of a surgical training programme on outcome of rectal cancer in the County of Stockholm. Stockholm colorectal cancer study group, Basingstoke bowel cancer research project. Lancet 356(9224):93–96
Park S, Kim NK (2015) The role of robotic surgery for rectal cancer: overcoming technical challenges in laparoscopic surgery by advanced techniques. J Korean Med Sci 30(7):837–846
Engstrom PF, Arnoletti JP, Benson AB 3rd, Chen YJ, Choti MA, Cooper HS, Covey A, Dilawari RA, Early DS, Enzinger PC, Fakih MG, Fleshman J Jr, Fuchs C, Grem JL, Kiel K, Knol JA, Leong LA, Lin E, Mulcahy MF, Rao S, Ryan DP, Saltz L, Shibata D, Skibber JM, Sofocleous C, Thomas J, Venook AP, Willett C (2009) NCCN clinical practice guidelines in oncology: rectal cancer. J Natl Compr Canc Netw 7(8):838–881
Kye BH, Cho HM (2014) Overview of radiation therapy for treating rectal cancer. Ann Coloproctol 30(4):165–174
Bae SU, Min BS, Kim NK (2015) Robotic low ligation of the inferior mesenteric artery for rectal cancer using the firefly technique. Yonsei Med J 56(4):1028–1035
Bae SU, Saklani AP, Hur H, Min BS, Baik SH, Kim NK (2014) Robotic interface for transabdominal division of the levators and pelvic floor reconstruction in abdominoperineal resection: a case report and technical description. Int J Med Robot. doi:10.1002/rcs.1624
Bae SU, Saklani AP, Hur H, Min BS, Baik SH, Lee KY, Kim NK (2014) Robotic and laparoscopic pelvic lymph node dissection for rectal cancer: short-term outcomes of 21 consecutive series. Ann Surg Treat Res 86(2):76–82
Shin JW, Kim J, Kwak JM, Hara M, Cheon J, Kang SH, Kang SG, Stevenson AR, Coughlin G, Kim SH (2014) First report: robotic pelvic exenteration for locally advanced rectal cancer. Colorectal Dis 16(1):O9–14
Park JA, Choi GS, Park JS, Park SY (2012) Initial clinical experience with robotic lateral pelvic lymph node dissection for advanced rectal cancer. J Korean Soc Coloproctol 28(5):265–270
Bae SU, Jeong WK, Baek SK (2016) Robotic anterior resection for sigmoid colon cancer using reduced port access. Dis Colon Rectum 59(3):245–246
Huang CW, Yeh YS, Su WC, Tsai HL, Choy TK, Huang MY, Huang CM, Wu IC, Hu HM, Hsu WH, Su YC, Wang JY (2016) Robotic surgery with high dissection and low ligation technique for consecutive patients with rectal cancer following preoperative concurrent chemoradiotherapy. Int J Colorectal Dis 31(6):1169–1177
Serin KR, Gultekin FA, Batman B, Ay S, Kapran Y, Saglam S, Asoglu O (2015) Robotic versus laparoscopic surgery for mid or low rectal cancer in male patients after neoadjuvant chemoradiation therapy: comparison of short-term outcomes. J Robot Surg 9(3):187–194
Park EJ, Cho MS, Baek SJ, Hur H, Min BS, Baik SH, Lee KY, Kim NK (2015) Long-term oncologic outcomes of robotic low anterior resection for rectal cancer: a comparative study with laparoscopic surgery. Ann Surg 261(1):129–137
Park SY, Choi GS, Park JS, Kim HJ, Ryuk JP (2013) Short-term clinical outcome of robot-assisted intersphincteric resection for low rectal cancer: a retrospective comparison with conventional laparoscopy. Surg Endosc 27(1):48–55
Baek JH, Pastor C, Pigazzi A (2011) Robotic and laparoscopic total mesorectal excision for rectal cancer: a case-matched study. Surg Endosc 25(2):521–525
Fernandez R, Anaya DA, Li LT, Orcutt ST, Balentine CJ, Awad SA, Berger DH, Albo DA, Artinyan A (2013) Laparoscopic versus robotic rectal resection for rectal cancer in a veteran population. Am J Surg 206(4):509–517
Bianchi PP, Ceriani C, Locatelli A, Spinoglio G, Zampino MG, Sonzogni A, Crosta C, Andreoni B (2010) Robotic versus laparoscopic total mesorectal excision for rectal cancer: a comparative analysis of oncological safety and short-term outcomes. Surg Endosc 24(11):2888–2894
Baik SH, Kwon HY, Kim JS, Hur H, Sohn SK, Cho CH, Kim H (2009) Robotic versus laparoscopic low anterior resection of rectal cancer: short-term outcome of a prospective comparative study. Ann Surg Oncol 16(6):1480–1487
Baek SJ, Kim CH, Cho MS, Bae SU, Hur H, Min BS, Baik SH, Lee KY, Kim NK (2015) Robotic surgery for rectal cancer can overcome difficulties associated with pelvic anatomy. Surg Endosc 29(6):1419–1424
Acknowledgments
This work was supported by the National Research Foundation of Korea (NRF) Grant funded by the Korea Government (MSIP) (No. 2014R1A5A2010008).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dae Ro Lim, Sung Uk Bae, Hyuk Hur, Byung Soh Min, Seung Hyuk Baik, Kang Young Lee, Nam Kyu Kim declare no potential conflict of interest relevant to this article.
Additional information
Dae Ro Lim and Sung Uk Bae denotes co-first authorship.
Rights and permissions
About this article
Cite this article
Lim, D.R., Bae, S.U., Hur, H. et al. Long-term oncological outcomes of robotic versus laparoscopic total mesorectal excision of mid–low rectal cancer following neoadjuvant chemoradiation therapy. Surg Endosc 31, 1728–1737 (2017). https://doi.org/10.1007/s00464-016-5165-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5165-6