Abstract
Background
The present study summarizes the 11-year laparoscopic gastric cancer surgery experience of a single institution in South Korea and evaluates the current trends of laparoscopic gastric cancer surgery through our experience.
Methods
A total of 3000 minimally invasive gastric cancer surgeries were performed at Seoul National University Bundang Hospital between May 2003 and January 2014. The types of laparoscopic gastrectomy used, surgical techniques, postoperative morbidities, and long-term oncologic outcomes were analyzed.
Results
The proportion of challenging procedures such as laparoscopic total gastrectomy and laparoscopic gastrectomy for patients with advanced gastric cancer increased during the study period. The frequency of laparoscopic function-preserving gastrectomy for patients with early-stage cancer also increased. The overall rate of complications was 16.7 %; surgical and systemic complication rates were 11.8 and 6.2 %, respectively. There was one case of postoperative mortality due to delayed bleeding after discharge. Male gender, high BMI, long operating times, combined resection of other organs, and total and proximal gastrectomies were independent predictors of surgical morbidities; however, pathologic T-stage was not a predictable factor. Accumulated experience in laparoscopic surgery decreased the surgical complication rates of total and proximal gastrectomies more than it did in distal gastrectomy over time. The 5-year overall survival rates of patients in advanced stages and those who underwent laparoscopic total gastrectomy were comparable to those reported previously.
Conclusions
Our results indicate the trends toward the expansion of laparoscopic approaches to technically demanding procedures and an increased use of laparoscopic function-preserving surgeries for patients with EGC with acceptable outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Since Kitano et al. [1] first reported the use of laparoscopy-assisted gastrectomy for patients with early gastric cancer (EGC) in 1994, the laparoscopic procedure has gained widespread international acceptance as one of the general modalities for the management of EGC. In Korea, 3783 laparoscopic gastrectomies were performed in 2009, accounting for 25.8 % of gastric cancer surgeries [2].
Accumulating experience and technical advances resulted in the emergence of two major trends in laparoscopic gastrectomy [3]. First, laparoscopic procedures are increasingly applied in technically demanding operations, such as laparoscopic gastrectomy for patients with advanced gastric cancer (AGC) or laparoscopic total gastrectomy (TG). Recent studies analyzing morbidities and long-term oncologic outcomes support the use of laparoscopic gastrectomy in patients with AGC [4–6] and laparoscopic TG [7–9]. Second, laparoscopic function-preserving gastrectomy is increasingly being used for the treatment for patients with EGC. Because of recent developments in screening programs in Korea and Japan, the proportion of EGC exceeds 50 % [2, 10], and the low incidence of lymph node metastasis and the favorable prognosis of EGC make it suitable for laparoscopic function-preserving surgery.
Our experience with laparoscopic gastric cancer surgery reflects these current trends in laparoscopic gastrectomy. The aims of the present study were to summarize our experience with laparoscopic surgery for gastric cancer in a single center in Korea over a period of 11 years and evaluate postoperative complication rates, how they have changed, and the long-term outcomes of patients.
Materials and methods
Types of laparoscopic procedures
Between May 2003 and January 2014, 3000 laparoscopic operations for gastric cancer were performed by four surgeons at the Department of Surgery at Seoul National University of Bundang Hospital (Table 1). Although the proportion of laparoscopic operation was 37.5 % of the total cases in 2003, the proportion increased to 89.0 % in 2013 (Fig. 1). Among laparoscopic operations, 2749 (91.7 %) were laparoscopic curative resections, and 98 (3.2 %) were sentinel node navigation surgeries, which were performed after 2010. A total of 147 (4.2 %) operations were performed as non-curative surgeries, of which 67 were laparoscopic peritoneal seeding nodule biopsies, 28 were palliative gastrojejunostomies, 11 were metastatic mass excisions (small bowel metastasis in four, port-site metastasis in one, locoregional lymph node metastasis in three, and distant lymph node metastasis in three), four were jejunostomy or ileostomy formation for seeding ileus, and 37 were palliative gastric resections (21 cases of R1 resection and 16 cases of R2 resection).
All cases were restaged retrospectively according to the 7th American Joint Committee on Cancer/International Union Against Cancer Tumor Node Metastasis staging, and the study protocol was approved by the institutional review board of SNUBH (IRB No. B-1508-312-110).
Operative criteria and strategy for laparoscopic gastrectomy
During the initial 5-year period, the indication for laparoscopic gastrectomy was confined to clinical T1–T2 stage without suspected lymph node metastasis. However, accumulating laparoscopic experience and the building of a competent laparoscopic surgical team resulted in the expansion of the criteria to locally advanced cancer. A prospective phase II clinical trial of our institution (NCT01441336) was initiated in 2008 to evaluate the technical and oncological safety of laparoscopic gastrectomy for patients with AGC, and thereafter, we gradually extended the indications of laparoscopic gastrectomy to clinical T4a (serosa invasion) stage and/or suspected node metastasis. A prospective phase II clinical trial was initiated in 2008 to evaluate the technical and oncological safety of laparoscopic gastrectomy for patients with AGC (NCT01441336). Lymph node dissection was performed as described in the Japanese gastric cancer treatment guidelines [11, 12]. The data on the extent of lymphadenectomy were revised retrospectively according to a recently published version of those guidelines [11]. Patients with gastric cancer clinically limited to the submucosa without evidence of lymph node metastasis underwent D1+ lymph node dissection, while D2 lymph node dissection was routinely performed when the clinical stage of the tumor was advanced (beyond the submucosa) or lymph node metastasis was suspected despite the diagnosis of EGC. D1 dissections were limited to decrease postoperative complications in high-risk patients. Partial omentectomy was performed routinely except in cases of AGC with serosa exposure under laparoscopic view, in which total omentectomy was performed.
Changes in anastomosis techniques
During the initial period, reconstructions (gastroduodenostomy and gastrojejunostomy) after laparoscopic distal gastrectomy (DG) were extracorporeally completed with direct visualization through mini-laparotomies (transverse incisions from 5 to 7 cm in the epigastric area). Intracorporeal gastroduodenostomy (delta-shaped anastomosis using linear stapler) was performed after 2010, and the first intracorporeal gastrojejunostomy was performed in 2011. In totally laparoscopic DG with intracorporeal reconstruction, all anastomoses were performed in the laparoscopic view, and specimens were extracted through vertically extended umbilical trocar sites (3–4 cm).
End-to-side esophagojejunostomy (E–J stomy) using a circular stapler after TG was performed intracorporeally using a laparoscopic purse-string clamp (Lap-Jack, Greenmate Biotech Corp., Seoul, Korea, and Endo-PSI, Hope Electronics, Chiba, Japan) after 2008. Before the use of the laparoscopic purse-string clamp, extracorporeal E–J stomy was performed through a vertical incision in the epigastric area or intracorporeal side-to-side E–J stomy using a linear stapler was performed [13]. End-to-side jejunojejunostomy (J–J stomy), 40 cm below the E–J stomy, was performed using an extracorporeal hand-sewing suture or linear staplers through a minilaparotomy (5–6 cm) with extension of the left 12-mm trocar site.
The first laparoscopic proximal gastrectomy (PG) for upper-third EGC was performed in 2004. Esophagogastrostomy (E–G stomy) was used initially; however, in 2009, the reconstruction method was changed to double tract reconstruction (DTR) because of its lower incidence of late complications such as gastroesophageal reflux and anastomotic stenosis [14]. DTR consists of conventional Roux-en Y E–J stomy and side-to-side gastrojejunostomy between the E–J stomy and J–J stomy. Currently, all reconstructions after PG are performed by DTR.
Patient selection for the analysis of changes in postoperative complication rates
To analyze changes in the rate of complications over time, 192 cases of gastrectomy with concomitant resections were excluded from the 2749 cases of laparoscopic curative gastrectomy. Other organ resections performed simultaneously were classified into two groups: concomitant resections for other pathological conditions (such as cholecystectomy for gallstone, colectomy for synchronous colon cancer, or hepatectomy for hemangioma), and combined resection for cancer invasion or for extended lymphadenectomy (such as distal pancreatectomy for the removal of a directly invaded tumor or splenectomy for resection of lymph node #10) [15]. Most concomitant resections except cholecystectomies were performed by surgeons from other divisions; attributing the postoperative complications to gastrectomy in such cases may be difficult. Therefore, only cases of combined resection were included out of all simultaneous other organ resections.
In addition, 148 operations performed by two surgeons were also excluded because these surgeons performed a small number of surgeries during a short period of time. These cases could be a confounder when analyzing the trend of complication rates over time. Finally, 2409 cases of laparoscopic curative gastrectomy were included in the analysis; postoperative surgical and systemic complications of grade II or higher in the Clavien–Dindo classification [16] were investigated. Complications associated with the surgical technique or the operation field were considered surgical complications. Surgical complications included wound morbidity, leakage (anastomosis and duodenal stump), anastomotic stricture, bleeding (anastomosis site or intra-abdominal), intra-abdominal abscess, pancreatic fistula (drain amylase content greater than 1000 U/L after postoperative days 3–5), pancreatitis (elevated serum amylase >150 U/L with symptoms such as back pain and fever), splenic arterial aneurysm, lymphorrhea, remnant stomach infarction, delayed gastric emptying, reflux esophagitis, and intestinal obstructive morbidity (paralytic ileus during the immediate postoperative period and adhesive ileus occurring after 1 month postoperatively). Systemic complications were defined as complications not associated with the operation field, such as lung morbidity, urinary tract morbidity, cardiovascular morbidity, renal failure, and uncontrolled ascites in patients with liver cirrhosis.
Patient selection for the analysis of 5-year overall survival
The long-term oncologic outcomes of patients who underwent laparoscopic curative distal or total gastrectomy were evaluated. A total of 2308 cases were selected from 2749 cases of laparoscopic curative gastrectomy, and the inclusion criteria were as follows: (1) pathologically proven gastric adenocarcinoma; (2) patients who underwent curative distal or total gastrectomy with D1+/D2 lymphadenectomy as described in the third Japanese gastric cancer treatment guidelines [11]; (3) no history of other therapies for gastric cancer; and (4) no history of other organ malignancy.
Statistical analysis
Continuous values are expressed as the mean and standard deviation. Statistical analyses were performed using the Chi-square test or Fisher’s exact test for categorical variables and a t test for continuous variables when appropriate. To identify the risk factors for morbidity, univariable and multivariable analyses were performed using Chi-square tests and binary logistic regression models. The interactions between surgical complication rates and the operation year were investigated. Kaplan–Meier curves were used to determine the prognosis of each staging system, and survival probabilities were compared using the log-rank test.
Statistical analyses were performed using SPSS version 20.0 software (IBM SPSS Inc., Chicago, IL, USA) and R version 3.1.1 (R Foundation for Statistical Computing, Vienna, Austria). A P value of ≤0.05 was considered statistically significant for all analyses.
Results
Clinicopathological features of patients who underwent laparoscopic curative gastric resection
The clinical and pathologic features of patients who underwent laparoscopic curative gastrectomy for gastric cancer are listed in Table 2. DG (81.2 %) was the most commonly performed procedure, followed by TG (11.9 %), PG (5.5 %), and pylorus-preserving gastrectomy (PPG, 1.0 %). The most common method of reconstruction after DG was Billroth I anastomosis (1340/2231, 60.1 %), followed by uncut Roux-en Y gastrojejunostomy (535/2231, 24.0 %). Simultaneous organ resection was performed in 280 cases; the most commonly resected organ in concomitant resections was the gallbladder (102/192, 53.1 %), whereas that in combined resections was the spleen (71/88, 80.7 %). Most patients underwent D1+ (47.5 %) and D2 (51.3 %) lymph node resection; laparoscopic D2+ lymph node dissection including the para-aortic lymph nodes (PAN) was performed in patients with suspected isolated PAN metastasis after palliative chemotherapy. Of 13 patients who underwent D2+ lymph node dissection, five had pathologically proven stage IV gastric cancer (pathologically positive PAN). The ratio of EGC to AGC diagnosed pathologically was 2025 (73.7 %):721 (26.3 %), and the most common histologic type was moderately differentiated tubular adenocarcinoma (34.7 %) followed by poorly cohesive carcinoma (22.8 %).
Changes in the type of laparoscopic gastrectomy for gastric cancer
The frequency of laparoscopic total gastrectomy has increased at an accelerated pace since 2009 after the establishment of the end-to-side E–J stomy method using a laparoscopic purse-string clamp (Fig. 2). The proportion of function-preserving gastrectomies (PG, PPG, and sentinel lymph node navigation surgery) increased from 0 % (0/29 total EGC cases) in 2003 to 13.8 % (40/250) in 2013, reaching a peak in 2011 at 21.4 % (69/254). The proportion of patients with AGC among those undergoing laparoscopic curative gastrectomy increased gradually after 2003 (Fig. 3). In 2013, 28.8 % of patients who underwent laparoscopic curative gastrectomy for gastric cancer were pathologically diagnosed with AGC, whereas only 6.2 % of all patients had advanced disease in 2003.
Postoperative morbidity and mortality
Postoperative morbidities were evaluated in 2409 cases selected according to the above-described criteria. The rate of complications changed over time; of 29 patients who underwent laparoscopic curative gastrectomy during the first year, nine (31.0 %) had complications, whereas the rate of complications stabilized to approximately 10–20 % after 2003 (Fig. 4). Grade II or higher complications according to the Clavien–Dindo classification are listed in Table 3. The overall complication rate was 16.7 %; the surgical and systemic complications occurred at a rate of 11.8 and 6.2 %, respectively. The most frequent surgical morbidity was pancreatic fistula (2.2 %), followed by wound morbidity (2.1 %). In 33 cases (1.4 %), reoperation was required because of postoperative complications, and the most common cause of repeat surgery was bleeding (8/33, 24.2 %), followed by stricture (7/33, 21.2 %) and internal herniation (2/33, 6.0 %). There was one case of postoperative mortality because of delayed bleeding after discharge in a patient who underwent laparoscopic DG.
Risk factors associated with postoperative morbidity
Risk factors associated with postoperative morbidity were evaluated in the selected 2409 cases. Variables associated with the occurrence of surgical complications in the univariable analysis were as follows: male gender, high BMI, high American Society of Anesthesiology (ASA) score, long operating time, combined resection, type of gastrectomy, large tumor size, and advanced T and N stages; a recent year of operation was a negative predictive factor (Table 4). In the multivariate analysis, male gender, BMI ≥ 27.5 kg/m2, operating time ≥180 min, combined resection of other organs, and total and proximal gastrectomies were independent risk factors for the occurrence of surgical complications, whereas a recent year of operation was an independent negative predictive factor (Table 5).
Old age, male gender, high ASA score, long operation time, combined resection, type of gastrectomy, large tumor size, and advanced T and N stages were factors associated with systemic complications in the univariable analysis (Table 4). Among them, age ≥60 years, male gender, and ASA score ≥3 were identified as independent risk factors associated with systemic complications in the multivariable analysis (Table 6).
Changes in the surgical complication rate over time according to each predictive factor
In the subgroup analysis, we investigated whether the rate of surgical complications changed over time according to each predictive factor. For this purpose, the study period was subdivided into three periods (first period: 2003–2007, second period: 2008–2010, and third period: 2011–2014.1), and the surgical complication rates in each period were analyzed according to each independent predictive factor (Supplementary Table 1). The reduction in the rate of surgical complications from the first to the third period was greater in patients undergoing PG than in those undergoing DG (first to third period: 46.2–11.9 % in PG vs. 10.8–8.9 % in DG, P = 0.009), and in TG compared with DG (from 43.6 to 21.6 % in TG, P = 0.057). When we dichotomize the whole period by merging the second and third periods, the introduction of intracorporeal end-to-side E–J stomy in 2008 resulted in a significant decrease in TG complication rate from 43.6 % in the first period (2003–2007) to 20.0 % in the second and third periods (2008–2014.1) (P = 0.001) (Supplementary Table 2). In particular, anastomosis-related complications, such as leakage (10.3 vs. 2.0 %, P = 0.020) and stenosis (5.1 vs. 0.4 %, P = 0.047), decreased significantly between the two periods.
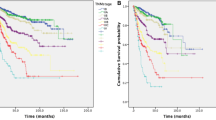
Long-term oncologic outcomes
The median follow-up period for the 2308 cases was 49.6 months (range 2.0–141.1 months). The overall 5-year survival rate was 90.2 %. The 5-year overall survival rates according to TNM stage were 95.1 % for stage IA (n = 1476), 91.5 % for stage IB (n = 284), 90.1 % for stage IIA (n = 167), 82.8 % for stage IIB (n = 117), 82.6 % for stage IIIA (n = 96), 61.9 % for stage IIIB (n = 83), and 36.7 % for stage IIIC patients (n = 81) (Fig. 5). The 5-year overall survival of stage IV patients (n = 4) could not be estimated because of two patient deaths at 4 and 10 months from aggravated alcoholic liver cirrhosis and cancer recurrence, respectively; the remaining patients were referred to other hospitals 2 and 3 years postoperatively. In the subgroup analysis of the DG and TG groups, there were no differences in the 5-year overall survival rates according to tumor stage [stage IA: 95.2 % (n = 1346) vs. 93.4 % (n = 130), P = 0.066; stage IB: 91.4 % (n = 261) vs. 92.3 % (n = 23), P = 0.564; stage IIA: 90.6 % (n = 140) vs. 87.5 % (n = 27), P = 0.306; stage IIB: 82.2 % (n = 100) vs. 86.3 % (n = 17), P = 0.926; stage IIIA: 81.2 % (n = 67) vs. 85.7 % (n = 29), P = 0.580; stage IIIB: 62.4 % (n = 51) vs. 59.3 % (n = 32), P = 0.529; and stage IIIC: 37.5 % (n = 40) vs. 35.1 % (n = 41), P = 0.712].
Discussion
One of the interesting findings of the present study was that the accumulated laparoscopic experience of the hospital was associated with a reduction in the rate of surgical complications. Although surgical complication rates remained stable after the second year of the study, the year of operation was found to be a protective factor for the prevalence of surgical complications in the multivariate analysis because the proportion of TG and combined resection, which were independent predictive factors of surgical complications, increased steadily during the same period. There are several studies in the literature addressing the learning curves of laparoscopic gastrectomy. These studies show that 40–90 cases of laparoscopic DG and 100 cases of laparoscopic TG are required for initial completion of learning [17–20]. Our study showed that the sustained accumulation of experience contributes to the decrease in surgical complications after overcoming the learning curve. The improved surgical outcomes could be attributed to the use of standardized laparoscopic procedures and the establishment of a laparoscopic gastrectomy team that includes experienced scopists and nurses, as well as an increase in the surgeons’ personal laparoscopic techniques and the advance of laparoscopic equipment such as high definition or three-dimensional laparoscopic cameras and more reliable energy devices [21]. Although our hospital is responsible for the education of residents and fellowship trainees as a national tertiary hospital and a large proportion of the operations are performed under supervision, standardized procedures that can be reproduced easily and an experienced supporting staff may have improved the surgical outcomes [22].
During the course of the present study, one of the major trends in laparoscopic gastrectomy in our hospital was an increase in the application of laparoscopic methods to technically demanding operations, such as laparoscopic gastrectomy for patients with AGC and laparoscopic TG. The results regarding morbidity and survival showed the technical feasibility and long-term oncologic safety of laparoscopic gastrectomy for AGC patients. Our data showed that the extent of lymphadenectomy did not affect the occurrence of postoperative complications, whereas a high pathologic (p) T-stage was associated with an increased rate of surgical complications in the univariate analysis. However, the proportion of combined resections of other organs was also significantly higher in patients with pT3 and pT4 stage than in those with pT1 and pT2 stage disease (T1: 0.8 %, T2: 3.4 %, T3: 7.8 %, and T4: 27.4 %, P < 0.001). Consequently, the independent predictive factor for surgical complications was not pT-stage, but rather combined resections in the multivariate analysis. Previous studies reported similar complication rates of laparoscopic gastrectomy in patients with EGC and AGC [6, 7, 23–26], with rates of 10.5–25.4 % for EGC [23–25], and 8.0–24.2 % for AGC [6, 7, 26]. These figures did not differ from those of open gastrectomy for AGC (8.0–28.5 %) [7, 26, 27]. The overall 5-year survival rate in the present study was also acceptable compared with that reported previously [5, 28, 29]. These survival data could provide preliminary evidence supporting the use of laparoscopic gastrectomy in patients with AGC before the results of randomized controlled clinical trials investigating the efficacy of the laparoscopic approach for the treatment for AGC become available.
Although TG was a predictive factor for surgical morbidity in the present study, the mean surgical complication rate of laparoscopic TG during the study period (23.1 %) was comparable to that reported previously [7, 30, 31]. The rate of surgical complications including anastomotic leakage and stenosis after TG decreased sharply between the early (2003–2007) and late (2008–2014.1) periods. The anastomosis technique of intracorporeal end-to-side E–J stomy using the laparoscopic purse-string clamp was introduced in 2008, and accumulated experience in this technique could reduce the rate of anastomosis-related surgical complications. Furthermore, the long-term outcomes did not differ between laparoscopic TG and laparoscopic DG in all tumor stages and were comparable with those reported previously [7, 30, 32].
According to the Nationwide Registries of Gastric Cancer of Korea and Japan [2, 10], the rates of incidence of pathological T1 (mucosal and submucosal) cancer in 2009 and 2008 were 57.6 and 51.2 %, respectively, and quality of life after surgery became an increasingly important factor because of the excellent long-term survival of patients with EGC. Therefore, function-preserving surgery such as PG has become increasingly popular as a patient-specific operation. Proximal gastrectomy for upper EGC is unpopular in Korea because of its well-established late complications such as reflux esophagitis, which occurs regardless of improved nutrition [33, 34]. At our institution, the number of PGs performed has increased steeply since 2011. This increase can be attributed to two factors, namely the establishment of the E–J anastomosis technique and the introduction of DTR as a new reconstruction method after PG. DTR consists of conventional Roux-en-Y reconstruction after TG and additional gastrojejunostomy. Therefore, reduced anastomosis-related complications after laparoscopic TG could reduce the burden of DTR after laparoscopic PG. DTR after PG has been performed since 2009, and the incidence of reflux esophagitis decreased to a level similar to that associated with TG [14]. In the present study, laparoscopic PG was associated with a significantly higher mean rate of surgical complications (19.7 %) than laparoscopic DG (9.5 %); however, this rate decreased from 46.2 % in the first period to 11.9 % in the third period. This drop was significantly greater than that of DG. The two technical factors mentioned above could have contributed to this sharp decrease in the surgical morbidities of PG.
In conclusion, the sustained accumulation of laparoscopic gastrectomy experience may contribute to a continuous decrease in the rate of surgical complications. Challenging laparoscopic procedures, such as laparoscopic TG and laparoscopic surgery for patients with AGC, showed acceptable short-term and long-term outcomes. With the advancement in laparoscopic techniques, laparoscopic PG can be performed safely. The present results indicate the trends toward the expansion of laparoscopic approaches to technically demanding procedures and an increased use of laparoscopic function-preserving surgeries for patients with EGC with acceptable outcomes.
References
Kitano S, Iso Y, Moriyama M, Sugimachi K (1994) Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 4(2):146–148
Jeong O, Park YK (2011) Clinicopathological features and surgical treatment of gastric cancer in South Korea: the results of 2009 nationwide survey on surgically treated gastric cancer patients. J Gastric Cancer 11(2):69–77. doi:10.5230/jgc.2011.11.2.69
Son SY, Kim HH (2014) Minimally invasive surgery in gastric cancer. World J Gastroenterol 20(39):14132–14141. doi:10.3748/wjg.v20.i39.14132
Lee JH, Lee CM, Son SY, Ahn SH, Park DJ, Kim HH (2014) Laparoscopic versus open gastrectomy for gastric cancer: long-term oncologic results. Surgery 155(1):154–164. doi:10.1016/j.surg.2013.06.015
Kim HH, Han SU, Kim MC, Hyung WJ, Kim W, Lee HJ, Ryu SW, Cho GS, Song KY, Ryu SY (2014) Long-term results of laparoscopic gastrectomy for gastric cancer: a large-scale case-control and case-matched korean multicenter study. J Clin Oncol 32(7):627–633. doi:10.1200/JCO.2013.48.8551
Lee JH, Son SY, Lee CM, Ahn SH, Park DJ, Kim HH (2013) Morbidity and mortality after laparoscopic gastrectomy for advanced gastric cancer: results of a phase II clinical trial. Surg Endosc 27(8):2877–2885. doi:10.1007/s00464-013-2848-0
Eom BW, Kim YW, Lee SE, Ryu KW, Lee JH, Yoon HM, Cho SJ, Kook MC, Kim SJ (2012) Survival and surgical outcomes after laparoscopy-assisted total gastrectomy for gastric cancer: case-control study. Surg Endosc 26(11):3273–3281. doi:10.1007/s00464-012-2338-9
Haverkamp L, Weijs TJ, van der Sluis PC, van der Tweel I, Ruurda JP, van Hillegersberg R (2013) Laparoscopic total gastrectomy versus open total gastrectomy for cancer: a systematic review and meta-analysis. Surg Endosc 27(5):1509–1520. doi:10.1007/s00464-012-2661-1
Wang W, Zhang X, Shen C, Zhi X, Wang B, Xu Z (2014) Laparoscopic versus open total gastrectomy for gastric cancer: an updated meta-analysis. PLoS One 9(2):e88753. doi:10.1371/journal.pone.0088753
Isobe Y, Nashimoto A, Akazawa K, Oda I, Hayashi K, Miyashiro I, Katai H, Tsujitani S, Kodera Y, Seto Y, Kaminishi M (2011) Gastric cancer treatment in Japan: 2008 annual report of the JGCA nationwide registry. Gastric Cancer 14(4):301–316. doi:10.1007/s10120-011-0085-6
Japanese Gastric Cancer Association (2011) Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 14(2):113–123. doi:10.1007/s10120-011-0042-4
Nakajima T (2002) Gastric cancer treatment guidelines in Japan. Gastric Cancer 5(1):1–5. doi:10.1007/s101200200000
Noh SY, Lee JH, Ahn SH, Son SY, Lee CM, Park DJ, Kim HH, Lee HJ, Yang HK (2012) Intracorporeal end-to-side esophagojejunostomy using a laparoscopic purse-string clamp during laparoscopic total gastrectomy. J Minim Invasive Surg 15(2):32–37. doi:10.7602/jmis.2012.15.2.32
Ahn SH, Jung DH, Son SY, Lee CM, Park DJ, Kim HH (2014) Laparoscopic double-tract proximal gastrectomy for proximal early gastric cancer. Gastric Cancer 17(3):562–570. doi:10.1007/s10120-013-0303-5
Lee CM, Rao J, Son SY, Ahn SH, Lee JH, Park DJ, Kim HH (2013) Laparoscopic gastrectomy for gastric cancer with simultaneous organ resection. J Laparoendosc Adv Surg Tech A 23(10):861–865. doi:10.1089/lap.2013.0081
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications. Ann Surg 240(2):205–213. doi:10.1097/01.sla.0000133083.54934.ae
Zhang X, Tanigawa N (2009) Learning curve of laparoscopic surgery for gastric cancer, a laparoscopic distal gastrectomy-based analysis. Surg Endosc 23(6):1259–1264. doi:10.1007/s00464-008-0142-3
Kim MC, Jung GJ, Kim HH (2005) Learning curve of laparoscopy-assisted distal gastrectomy with systemic lymphadenectomy for early gastric cancer. World J Gastroenterol 11(47):7508–7511
Jin SH, Kim DY, Kim H, Jeong IH, Kim MW, Cho YK, Han SU (2007) Multidimensional learning curve in laparoscopy-assisted gastrectomy for early gastric cancer. Surg Endosc 21(1):28–33. doi:10.1007/s00464-005-0634-3
Jung DH, Son SY, Park YS, Shin DJ, Ahn HS, Ahn SH, Park DJ, Kim HH (2014) The learning curve associated with laparoscopic total gastrectomy. Gastric Cancer. doi:10.1007/s10120-014-0447-y
Kim MG, Kwon SJ (2014) Comparison of the outcomes for laparoscopic gastrectomy performed by the same surgeon between a low-volume hospital and a high-volume center. Surg Endosc 28(5):1563–1570. doi:10.1007/s00464-013-3352-2
Tokunaga M, Hiki N, Fukunaga T, Miki A, Nunobe S, Ohyama S, Seto Y, Yamaguchi T (2009) Quality control and educational value of laparoscopy-assisted gastrectomy in a high-volume center. Surg Endosc 23(2):289–295. doi:10.1007/s00464-008-9902-3
Kim HH, Hyung WJ, Cho GS, Kim MC, Han SU, Kim W, Ryu SW, Lee HJ, Song KY (2010) Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report—a phase III multicenter, prospective, randomized Trial (KLASS Trial). Ann Surg 251(3):417–420. doi:10.1097/SLA.0b013e3181cc8f6b
Kim MC, Kim W, Kim HH, Ryu SW, Ryu SY, Song KY, Lee HJ, Cho GS, Han SU, Hyung WJ, Korean Laparoscopic Gastrointestinal Surgery Study Group (2008) Risk factors associated with complication following laparoscopy-assisted gastrectomy for gastric cancer: a large-scale korean multicenter study. Ann Surg Oncol 15(10):2692–2700. doi:10.1245/s10434-008-0075-z
Lee JH, Park DJ, Kim HH, Lee HJ, Yang HK (2012) Comparison of complications after laparoscopy-assisted distal gastrectomy and open distal gastrectomy for gastric cancer using the Clavien–Dindo classification. Surg Endosc 26(5):1287–1295. doi:10.1007/s00464-011-2027-0
Shinohara T, Satoh S, Kanaya S, Ishida Y, Taniguchi K, Isogaki J, Inaba K, Yanaga K, Uyama I (2013) Laparoscopic versus open D2 gastrectomy for advanced gastric cancer: a retrospective cohort study. Surg Endosc 27(1):286–294. doi:10.1007/s00464-012-2442-x
Fang C, Hua J, Li J, Zhen J, Wang F, Zhao Q, Shuang J, Du J (2014) Comparison of long-term results between laparoscopy-assisted gastrectomy and open gastrectomy with D2 lymphadenectomy for advanced gastric cancer. Am J Surg. doi:10.1016/j.amjsurg.2013.09.028
Park DJ, Han SU, Hyung WJ, Kim MC, Kim W, Ryu SY, Ryu SW, Song KY, Lee HJ, Cho GS, Kim HH, Korean Laparoscopic Gastrointestinal Surgery Study Group (2012) Long-term outcomes after laparoscopy-assisted gastrectomy for advanced gastric cancer: a large-scale multicenter retrospective study. Surg Endosc 26(6):1548–1553. doi:10.1007/s00464-011-2065-7
Huscher CG, Mingoli A, Sgarzini G, Sansonetti A, Di Paola M, Recher A, Ponzano C (2005) Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: five-year results of a randomized prospective trial. Ann Surg 241(2):232–237
Mochiki E, Toyomasu Y, Ogata K, Andoh H, Ohno T, Aihara R, Asao T, Kuwano H (2008) Laparoscopically assisted total gastrectomy with lymph node dissection for upper and middle gastric cancer. Surg Endosc 22(9):1997–2002. doi:10.1007/s00464-008-0015-9
Topal B, Leys E, Ectors N, Aerts R, Penninckx F (2008) Determinants of complications and adequacy of surgical resection in laparoscopic versus open total gastrectomy for adenocarcinoma. Surg Endosc 22(4):980–984. doi:10.1007/s00464-007-9549-5
Bo T, Peiwu Y, Feng Q, Yongliang Z, Yan S, Yingxue H, Huaxing L (2013) Laparoscopy-assisted vs. open total gastrectomy for advanced gastric cancer: long-term outcomes and technical aspects of a case-control study. J Gastrointest Surg 17(7):1202–1208. doi:10.1007/s11605-013-2218-1
Ahn SH, Lee JH, Park DJ, Kim HH (2013) Comparative study of clinical outcomes between laparoscopy-assisted proximal gastrectomy (LAPG) and laparoscopy-assisted total gastrectomy (LATG) for proximal gastric cancer. Gastric Cancer 16(3):282–289. doi:10.1007/s10120-012-0178-x
Kosuga T, Ichikawa D, Komatsu S, Okamoto K, Konishi H, Shiozaki A, Fujiwara H, Otsuji E (2015) Feasibility and nutritional benefits of laparoscopic proximal gastrectomy for early gastric cancer in the upper stomach. Ann Surg Oncol. doi:10.1245/s10434-015-4590-4
Acknowledgments
The authors thank the Medical Research Collaborating Center at Seoul National University Bundang Hospital for performing analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Young Suk Park, Sang-Yong Son, Aung Myint Oo, Do Hyun Jung, Dong Joon Shin, Sang-Hoon Ahn, Do Joong Park, and Hyung-Ho Kim have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Park, Y.S., Son, SY., Oo, A.M. et al. Eleven-year experience with 3000 cases of laparoscopic gastric cancer surgery in a single institution: analysis of postoperative morbidities and long-term oncologic outcomes. Surg Endosc 30, 3965–3975 (2016). https://doi.org/10.1007/s00464-015-4708-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4708-6