Abstract
Background
Interventional endoscopies entail a risk of infection secondary to perforation of the luminal wall. Thereby, bacteria may be introduced into the sterile environment of the peritoneal cavity (PC). Limited data are available regarding the efficacy of prophylactic anti-infective treatments. The aim of the study was to examine the efficacy/safety of anti-infective means in the prevention of infection by interventional endoscopies in a randomized controlled animal trial.
Methods
Forty pigs were randomized to: 1: control; 2: oral lavage; 3: gastric lavage; 4: oral/gastric lavage; 5: i.m. antibiotics. Lavage was performed with Octenisept prior to the operation. After gastric wall perforation, peritoneoscopy was performed. Before the procedure, after closure and prior to autopsy, intraabdominal lavage for bacterial culture was taken using mini-laparoscopy. At autopsy, macroscopic appearance of the PC was scored. Lavage fluids were grown to identify/quantify bacterial load. Concentration of intraperitoneal bacteria at autopsy was defined as main outcome parameter.
Results
No major complications occurred in any of the procedures. Bacterial load of the PC at autopsy was significantly reduced with antibiotics compared to all other groups, whereas it did not differ between the lavage groups and control. Macroscopic scoring of the PC showed significant lower rate of intraabdominal abscesses in the antibiotic group compared to the lavage groups and control (p < 0.01).
Conclusion
Only antibiotic prophylaxis is effective for the prevention of infection after iatrogenic perforation of the gastrointestinal wall. There was no difference between any form of lavage and the control group. Further studies in humans are required to prove these animal data.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Over the last few years, endoscopy has rapidly progressed from diagnosis to therapeutic intervention. Recently, more invasive and riskier applications have been established including endoscopic mucosal resection (EMR), endoscopic submucosal dissection (ESD), peroral endoscopic myotomy (POEM) and even full-thickness wall resection (FWR) [1–5].
All such interventional techniques entail a significant risk of perforation, which is among the most dangerous adverse events in gastrointestinal (GI) endoscopy. In ESD and POEM, the risk of perforation is 3.9 and 57.0 %, respectively [6, 7]. Inadvertent, non-sterile access to the peritoneal cavity (PC) may result in significant infectious complications [8–10].
This is particularly relevant for the more invasive techniques including natural orifice transgastric endoscopic surgery (NOTES) in which a full-thickness GI tract defect is created routinely to access the PC. Although early results of NOTES procedures such as transgastric appendectomy have not seen major infectious complications, data are still limited to case reports and small studies in humans with a reported overall complication rate of up to 17.8 % (5/28) including infectious complications with intraabdominal abscess formation in up to 11 % of cases [11–15].
Infection remains a major concern with more invasive endoluminal and transluminal endoscopic interventions, as spillage of luminal contents into the PC is accompanied by bacterial contamination. Iatrogenic infection is therefore an important topic in interventional endoscopy [16]. The necessity of prophylaxis has been widely discussed but as yet, there is little high-quality data to allow conclusions as to what kind of prophylaxis is best and most effective in avoiding infection once such perforation or access to the PC has occurred [17].
We conducted a randomized controlled animal study to compare the effectiveness of various topic bactericides with antibiotic treatment and untreated controls in a standardized endoscopic procedure with access to the PC.
Materials and methods
Ethics
The study was approved by the local ethics review board and a regional governmental institution (Niedersächsisches Landesamt für Verbraucherschutz und Lebensmittelsicherheit, Oldenburg, Germany; No. 33.9-42502-04-0771354; 10/2008). All experiments were carried out at an approved animal institute (Institute of Farm Animal Genetics, Friedrich Loeffler Institute, Mariensee, Germany) and met the guidelines of the mentioned governmental institution.
Study outline
Forty healthy female large white pigs were randomly allocated to five groups: an untreated control group and four groups in which either topical or intramuscular prophylactic, anti-infective treatment options were applied. The following anti-infective methods were allocated to the different groups:
-
1.
Control group
-
2.
Oral lavage only
-
3.
Gastric lavage only
-
4.
Oral + gastric lavage
-
5.
Antibiotics—intramuscular (i.m.) injection for 3 days post-procedure.
Animals were randomly assigned to the four study groups and the control group using a random number generator (QuickCalc online calculator, GraphPad Software Inc., La Jolla, CA, USA). Within this random generator, each animal was first randomly assigned to a group. Then, the assignment of each subject was swapped with the group assignment of a randomly chosen animal. This entire process was repeated twice to ensure sufficient randomization.
At baseline, bacteriological samples were obtained from the PC in a sterile fashion by mini-laparoscopy and also from mouth (oral swab) and stomach (aspiration of gastric fluid). Prophylaxis was then applied according to the randomization. In the lavage groups (group 2–4), a second oral and gastric sample was collected 5 min after local lavage. In all animals, a transgastric peritoneoscopy was performed for 45 min. This time was deemed as an average time for closing an iatrogenic perforation of the gastrointestinal wall in daily clinical routine. Immediately after closure of the gastric access, a second mini-laparoscopy was performed with fluid sampling from the PC to assess bacterial load before antibiotics were given in group 5. Animals were kept alive for a follow-up period of approximately 3 weeks. Prior to autopsy, a third mini-laparoscopy was undertaken for bacteriological sampling from the PC. At autopsy, the PC was inspected for signs of infection. Figure 1 outlines the different steps of the study protocol.
Anti-infective methods
Mechanical lavage (groups 2–4)
In the oral lavage group, the oral cavities of the animals were disinfected with 100 ml of the topical microbicide Octenisept© (OCT) (0.1 g octenidine dihydrochloride and 0.2 g 2-phenoxyethanol; Octenisept©; Schuelke & Meyer, Norderstedt, Germany). Gastric lavage was performed using 200 ml of the OCT solution being infused into and homogenously distributed within the stomach through the accessory channel of the same endoscope used for the procedure to follow.
Antibiotic prophylaxis (group 5)
Antibiotic prophylaxis consisted of i.m. injection of enrofloxacin 1 mg/kg (Baytril©, Bayer, Leverkusen, Germany) for three consecutive days starting immediately after the operation. I.m. administration is the routine way of application in pigs; plasma levels of i.v. versus i.m. application are comparable (US Patent No. 5,756,506).
Bacteriological sampling
Oral cavity samples
Oral samples were obtained by circular swabbing of the oral cavity using a sterile medical gauze that was then placed in a sterile culture cup with 2 ml sterile 0.9 % saline for further analysis. This procedure was carried out immediately prior and 5 min after oral lavage.
Gastric samples
Prior to and 5 min post-lavage, 2 ml gastric fluid was aspirated using a catheter through the accessory channel of the endoscope. A new catheter was used for aspiration to avoid cross-contamination.
Peritoneal samples
A mini-laparoscopy was performed in a standardized manner as described [18] to collect peritoneal samples under sterile conditions. 200 ml sterile 0.9 % saline was then instilled into the PC via laparoscope. Afterwards, at least 50 ml of the peritoneal fluid was aspirated from the pelvic gutters and transferred to sterile cups. Immediately after the gastric defect was closed, a second peritoneal sample was obtained via mini-laparoscopy to evaluate bacterial contamination during the procedure.
Animal preparation
Animals fasted overnight with free access to water before the surgical procedure was started under general anaesthesia with orotracheal intubation and mechanical ventilation. General anaesthesia was initiated and maintained using isoflurane and fentanyl while hemodynamic parameters (heart rate, blood pressure, O2 saturation, end-tidal CO2 levels) were continuously monitored. Thiopental sodium was injected (6.6–8.8 mg/kg) intravenously through a marginal ear vein.
All animals had the same special diet starting 2 weeks prior to the examinations. After the procedure, the animals resumed their normal diet.
Transgastric peritoneoscopy
Prior to each experiment, the endoscope used was manually reprocessed (rinsing, disinfecting, final rinsing and drying) according to the ESGE guidelines on “Cleaning and disinfection in gastrointestinal endoscopy” [19].
Transgastric passage of the endoscope was performed through the anterior gastric wall using a needle knife (Q441, Olympus Optical, Hamburg, Germany) with electrocautery for a small gastric wall incision followed by insertion of a guide wire (JagWire, 0.035′; Boston Scientific Corp., Natick, MA, USA) into the PC. Subsequently, a 10–12 mm expansion balloon (Boston Scientific Corp., Natick, MA, USA) was passed over the guide wire for dilatation of the gastric wall access up to a diameter of 11 mm to allow passage of a standard gastroscope into the PC. Any bleeding during the access procedure was stopped with argonplasma coagulation (APC) [17]. For standardization, the gastroscope remained in the PC for 45 min. In all animals, only a transgastric peritoneoscopy was performed without manipulating the bowel or any adjacent organs to avoid any additional translocation of gastrointestinal bacteria into the PC. The gastric wall was closed either with an “over the scope clip” (OTSC; OVESCO Endoscopy Inc., Campbell, CA, USA) or an endoscopic suturing system (TAS, Ethicon Endosurgery, Cincinnati, Ohio, USA). The procedure has been described in detail elsewhere [18]. After closure of the wall a leak test was performed by insufflating air into the stomach, a potential air leak would have been recognized by bubbling at the gastrostomy site observed by mini-laparoscopy. A second leak test was performed at autopsy. The stomach was removed, the distal part of the stomach was closed with a suture, and then, 1000 ml of water was instilled into the stomach.
Post-operative observation
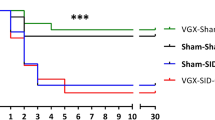
Weight gain was measured every third day during the post-operative observation period and prior to autopsy. Clinical observations of the pigs including behaviour, food intake and body temperature were carried by experienced veterinary personnel (veterinary technician, veterinarian) on a daily basis.
Autopsy
A follow-up of approximately 3 weeks was chosen as an average time of post-operative survival in similar animal studies conducted so far (range between 7 and 28 days) [14–18]. Furthermore, a mean hospital stay of 3 weeks was observed in patients having experienced complicated interventional endoscopic procedures with iatrogenic perforation of the gut wall. At autopsy, close inspection of the PC was performed for any signs of infection or other abnormalities. A macroscopic inflammation score was used. Infection and/or abscess formation was graded between 0 and 3: 0—no infection; 1—mild erythema; 2—marked erythema and occasional (less than 3) small abscesses <1 cm; 3—severe erythema with multiple abscesses, or abscess >1 cm [17]. The macroscopic degree of inflammation was graded independently by two examiners: one member of the surgical team (ME) and one trained pathologist (FS). Both examiners were blinded to the randomization group and did not know about the respective assessment results of their colleague.
Laboratory analysis
All samples were streaked (swab) or plated (fluid) on sheep blood agar plates (BAP) and incubated aerobically for 24–48 h at 37 °C. Then, colonies with a different morphology were picked and subcultured on BAP and Gassner agar plates, a selective medium to differentiate lactose-positive and lactose-negative Enterobacteriaceae. Gram staining was performed for all pure cultures. All Gram-positive cocci were subjected to catalase testing. Based on the colony morphology and the results of the additional tests, the isolates were classified as presumptive Bacillus spp., Enterobacteriaceae, Proteus spp., Pseudomonas spp. Staphylococcus spp. and Streptococcus spp., respectively. Bacterial quantities were expressed as colony-forming units per millilitre (CFU/ml) [18, 20]. Co-workers who performed laboratory analysis were blinded to the randomization and time point of sampling.
Endpoints
The primary outcome of the study was the concentration of intraperitoneal bacteria at the time of autopsy. The changes in bacterial population, presence/absence of gross evidence of intraperitoneal infection and mortality were defined as secondary endpoints.
Statistical analysis
A pilot study conducted by Eickhoff et al. [18] using a quadruple anti-infective treatment achieved a reduction of intraperitoneal bacteria of 99.3 %. Therefore, sample size calculation was based on the assumption that single anti-infective treatment options decrease concentration of intraperitoneal bacteria from 100 to 10 % (90 % reduction) if the peritoneum is accessed with unsterile instrumentation. On this basis, a sample size of at least 8 animals was required in each group to achieve a study power of 95 % and an alpha risk level of 0.05 [21].
Descriptive statistics (median, mean ± SD/SEM, proportions, 95 % confidence intervals) were calculated for qualitative and quantitative data (i.e. infection frequencies, bacterial growth, infection score). The nonparametric Mann–Whitney U test was used to analyse differences of CFU between the control group and the study groups. Cochran–Armitage test was used for categorical data analysis. Statistical significance was reported as p values <0.05. Statistical analysis was carried out using GraphPad Prism, version 6 (GraphPad Software Inc., La Jolla, CA, USA). Statistical consultation was obtained by the Institute of Medical Statistics, University Hospital Schleswig-Holstein, Campus Kiel, Kiel, Germany.
Results
Between June 2012 and August 2013, 40 female pigs were randomly assigned to each of the five study groups (control group; oral lavage; gastric lavage; oral + gastric lavage; antibiotics) with eight animals per group. Post-operative follow-up was 20.1 ± 0.3 days (range 17–23 days). The period did not differ significantly between the control and the treatment groups (p > 0.05).
Procedure
Transgastric perforation, peritoneoscopy and gastric closure were performed within 75.4 ± 0.9 min (range 65.0–88.0 min) without marked complications in all animals except one, in which a bleeding occurred as a side branch of the gastroepiploic artery was hit during the transgastric cutting process. This was stopped using APC as described [16]. At the end of each endoscopic procedure, the stomach was filled with air and leakage of the gastric closure was not seen at mini-laparoscopy. No major or clinically significant complications were observed during the follow-up period. Closure of the gastric wall lasted 18.4 ± 3.7 min using the OTSC device and 19.3 ± 4.8 min using the TAS device. The difference was statistically not significant (p > 0.05).
Clinical characteristics of animals
Body weight
At baseline, the mean body weight of all animals was 32.2 ± 0.6 kg (range 26.0–41.5 kg) and did not differ significantly between the groups (p > 0.05). During follow-up, the weight significantly increased by 31.4 % (42.3 ± 0.9 kg; p < 0.0001, compared to baseline).
Prior to autopsy, animals in the antibiotic group had an approximately 25 % higher body weight when compared to the other study groups and the control group (p < 0.001; weightantibiotics = 50.2 ± 2.5 kg). Between the lavage and the control groups, the final weight did not differ significantly (weightcontrol = 40.3 ± 2.0 kg, weightoral = 40.0 ± 1.1 kg; weightgastric = 40.5 ± 1.3 kg; weightoral/gastric = 40.7 ± 1.7 kg; p > 0.05).
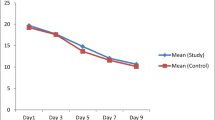
Body temperature
Mean preoperative body temperature at baseline was 35.7 ± 0.1 °C among all animals. Comparison of the different study groups revealed marked post-operative rise in the body temperature in the control group (Temp.control = 37.3 ± 0.5 °C) and the lavage groups (Temp.oral = 37.4 ± 0.4 °C; Temp.gastric = 37.4 ± 0.4 °C; Temp.oral/gastric = 39.2 ± 0.4 °C; p > 0.05). These changes were statistically significant when compared to baseline levels and the antibiotic group (p < 0.0001). The antibiotic group showed no significant changes of body temperature (Temp.antibiotic = 35.9 ± 0.1 °C; p > 0.05) throughout the study period (Tables 1 and 2).
The clinical characteristics of all groups are summarized in Table 2.
Macroscopic inflammation score at autopsy
At autopsy, peritoneal inflammation scores of the control and the 3 lavage groups were classified as “2” or “3” only, while the antibiotic group scored “0” or “1” without any signs of major inflammation or abscess formation (Table 2; Fig. 2). Macroscopic assessment of the degree of inflammation showed accordance in all but one animal (1/40; 2.5 %). This accounts for a kappa coefficient of 0.927 (95 % CI 0.829–1.000), which represents a very good interobserver variability. This one case was reassessed by both examiners simultaneously. Agreement was achieved and recorded for further analysis.
Quantification of bacterial load
Oral cavity and stomach
Oral lavage, either alone or in combination with gastric lavage, resulted in a significant reduction of bacterial growth compared to baseline levels. At baseline, the oral lavage group had a bacterial load of 3799 ± 941/ml (range 582–7424) and the oral/gastric lavage group of 4060 ± 1116/ml (range 364–9287). Bacterial load in the oral cavity was significantly reduced by oral lavage to CFUoral = 157 ± 51/ml (range 28–482; p = 0.002 compared to baseline) in the oral lavage group and to CFUoral/gastric = 123 ± 50/ml (range 36–472; p = 0.003 compared to baseline) in the oral/gastric lavage group.
Gastric lavage alone or gastric/oral lavage resulted in a significant reduction of bacterial load in the gastric juice. Baseline levels of the gastric lavage group were 175.5 ± 55.6/ml (range 56–462) in gastric lavage and 190.8 ± 64.3/ml (range 31–598) in the oral/gastric lavage group. Five min post-lavage, the bacterial load of the gastric juice was reduced to 47.4 ± 19.9/ml (range 31–598) in the gastric lavage group (p = 0.04 compared to baseline) and to 36.5 ± 12.2/ml (range 9–110) in the oral/gastric lavage group (p = 0.03 compared to baseline).
Peritoneal cavity
Baseline While baseline peritoneal samples were sterile in all animals throughout the groups, post-operative samples revealed bacterial growth in each animal.
Post-operative Post-operative bacterial load was 3264 ± 984/ml (range 284–8196) in the control group. Oral/oral-gastric/gastric lavage resulted in a significant reduction of the intraperitoneal bacterial load at the end of the operation when compared to the control group (p < 0.001; post-operation: CFUoral = 116 ± 35/ml (range 14–273); CFUoral/gastric = 92 ± 22/ml (range 14–178); CFUgastric = 884 ± 234/ml; range 51–2082; p = 0.03). No significant changes were observed between the antibiotic and the control group [CFUantibiotic = 2633 ± 856/ml (range 319–7236; p > 0.05)].
Autopsy The control group showed a mean bacterial load in the PC at autopsy of 2527 ± 1095/ml. No significant differences were seen between the control and each of the lavage groups (p > 0.05; CFUoral = 3193 ± 1136/ml; CFUgastric = 3016 ± 1106/ml; CFUoral/gastric = 2131 ± 966/ml). In contrast, only two positive peritoneal cultures occurred in the antibiotic group with a mean bacterial growth of CFU = 38 ± 35/ml. This bacterial concentration was significant lower (p < 0.0001) when compared to the control group and each of the lavage groups (Table 3; Fig. 3).
Comparison of microbiological quantification of colony-forming units (CFU)/ml in the mouth at baseline and after oral and oral/gastric lavage with Octenisept. Asterisks indicate significant differences compared to baseline levels. Data are presented as box plots with median, 0.25/0.75 quartile and minimum and maximum
At follow-up, only two pigs in the antibiotics group showed a peritoneal sample with growth of bacteria, whereas the samples of the other six pigs remained sterile. In contrast, the control group and the lavage groups exhibited positive bacterial cultures in the majority of animals leading to elevated organism concentrations at the time of follow-up (control: 75 %; oral lavage 87.5 %; gastric lavage 87.5 %; oral/gastric lavage 75 %) (Table 3).
Differentiation of bacteria
The most common organisms present in the PC post-operation were presumptive Bacillus spp., Enterobacteriaceae other than Proteus spp., Pseudomonas spp., Staphylococcus spp. and Streptococcus spp. Comparison of groups revealed a shift from predominately Staphylococcus and Streptococcus spp. in the control, gastric lavage and antibiotic group towards Enterobacteriaceae including Proteus spp. after oral lavage.
Bacterial culture of post-operative peritoneal lavages showed identical growth of virtually the same bacteria in 87.5 % (35/40) of animals when compared to baseline cultures cultivated from the mouth swabs. In total, 77.5 % (31/40) of the animals presented with the same bacterial spectrum as before. In the remaining, 22.5 % of the animals mainly Streptococcus and Staphylococcus spp. were cultivated from the samples (Table 4).
Discussion
Until recently, due to its high risk of infection, perforation of the peritoneum has been one of the most dangerous complications in gastrointestinal endoscopy, Over the past few years, interventional endoscopic procedures have shifted towards more invasive treatment methods such as ESD, POEM, FWR and NOTES. All of these bear a significant risk of perforation as a complication or calculated risk of the same while performing NOTES access, but the extent of infection and its consequences are not fully understood, as systematic comparative analysis of the impact on the PC is missing. We therefore evaluated the efficacy and safety of different anti-infective procedures and their impact on infection rates in the PC to identify the best infection prophylaxis in such cases, when there is a high risk of perforation or perforation of the GI wall is part of the procedure.
We demonstrated that, although various topical anti-infectives were able to significantly reduce the post-operative concentration of intraperitoneal bacteria, this had no impact on the bacterial load in the PC weeks later. In addition, the rate of infectious complications was unaltered compared to the control group. Furthermore, no clinical improvement was obtained by combining different means of topical anti-infective treatments. In our study, antibiotic treatment was the only method that reduced the intraperitoneal bacterial load sufficiently well to avoid morbidity and lower the rate of clinical infection.
In a similar study, Eickhoff et al. [18] investigated the effect of a combination of different anti-infective methods on the rate of infections in transgastric NOTES procedures. Eight animals received a quadruple combination treatment including iv. proton pump inhibitors, single shot antibiotic, oral and gastric lavage with chlorhexidine and gastric irrigation with diluted neomycin. In the control group, only gastric cleansing with sterile saline solution was undertaken. Quadruple combination treatment reduced the bacterial load of the PC to nearly nil, resulting in a lower infection rate when compared to the control group. It remains unclear whether it was the combination of all four agents or which of the four agents used caused this beneficial effect described in their study [18].
Similar results were obtained by Giday et al. who investigated transgastric NOTES procedures under sterile and non-sterile conditions in 32 pigs: Sterility was achieved by the use of sterile overtubes, endoscopes and perioperative antibiotics plus antiseptic gastric lavage. In the non-sterile control group (16 pigs), none of these precautions were undertaken. At necropsy after 1 week, all animals (100 %) in the non-sterile group had intraperitoneal infections, whereas neither macroscopic nor microscopic signs of infection were observed in the sterile group [22].
Despite the remarkable outcome of these studies, no conclusions can be drawn regarding the relative importance of any one of the various components of the prophylactic precautions, as they have not been analysed separately. It therefore remains unclear whether the combination of multiple components is necessary. As administration of the various anti-infective means is time-consuming and costly, they are not suitable for implementation in daily practice. Further knowledge of the effect of each of the single components would be valuable.
In our study, oral and gastric lavage (and a combination of both) resulted in a significant reduction of the concentration of bacteria in the oral cavity by ≈96 % and in the stomach by ≈73 %. The concentration of intraperitoneal bacteria was significantly reduced by oral and/or gastric lavage ranging from 73 % (gastric) to 97 % (oral/gastric). However, this did not seem to have any positive effect on the overall result of the autopsy 2 weeks later. This was specifically true for oral lavage (Figs. 3, 4), which initially caused a 96 % reduction in bacteria, but a significant amount of infection was present at autopsy. Topical lavage did not result in a marked difference between the control and the lavage groups’ bacterial load in the PC nor of the actual clinical infection rate and abscess formation at autopsy. The reduction of bacterial load did not seem to have a long-term effect on these complications. It is likely that the sealed environment of the PC is an ideal multiplication place for even small numbers of bacteria remaining, resulting in long-term abscess formation.
Comparison of microbiological quantification of colony-forming units (CFU)/ml in the peritoneal cavity. Data show CFU results at baseline, post-operation and prior to autopsy. Asterisks indicate significant differences compared to the control group. Data are presented logarithmically (log) as box plots with median, 0.25/0.75 quartile and minimum and maximum
Our data further showed that systemic antibiotic treatment was the only effective treatment to prevent any possible infectious complications. It not only reduced the concentration of intraperitoneal bacteria (approximately 38 CFU/ml; p < 0.0001) at the time of autopsy but also significantly reduced the clinical rate of abscess formation.
At the time of autopsy, 77.5 % of the animals presented with the same bacterial spectrum when compared to the baseline cultures of the oral cavity. In the remaining 22.5 % mainly Streptococcus and Staphylococcus spp. were cultivated (Table 4). Of note, in one of these animals a notable infection of the abdominal wall at the laparoscopy incision site was recorded at autopsy as a possible infection site in this case.
The coincidental bacterial species in the oral cavity and PC provided strong evidence that bacterial peritoneal infections are caused by direct translocation of bacteria from the oral cavity to stomach to PC by the endoscope. This spread was not prevented by topical treatment showing translocation of bacteria is the major risk factor for infectious complications in interventional endoscopic procedures with perforation.
As shown by other groups, transgastric NOTES procedures cause a bacterial contamination of the PC, though this contamination did not lead to any septic complications in these animal models [23–25]. It remains unclear whether these data can be directly transferred into humans. The translocation of bacteria by the endoscope into the PC has also been described in studies in humans, but even in this setting the clinical relevance remains controversial. In a retrospective study by Nau et al., the infectious risk of a gastrostomy with and without NOTES procedure was assessed. Fifty patients underwent laparoscopic Roux-en-Y gastric bypass (RYGB), 40 patients received laparoscopic RYGB with concomitant transgastric NOTES peritoneoscopy and ten patients only had a transgastric NOTES peritoneoscopy. NOTES procedures were carried out with disinfected but not sterilized endoscopes without gastric lavage, etc. In this series, gastric to peritoneum cross-contamination (based on peritoneal aspirate cultures) was found in 10 % of laparoscopic RYGB, 21 % of NOTES RYGB and 0 % of NOTES peritoneoscopy. These findings, however, did not correlate with the post-operative clinical outcome of the patient and did not affect the patients’ management. Of note, an antibiotic prophylaxis was administered in all patients supporting the results of our study [26]. Similarly, in a case series of eleven hybrid transgastric NOTES/transabdominal laparoscopic cholecystectomies, Dallemagne et al. [27] confirmed contamination of the peritoneum post-gastrostomy by peritoneal aspirate cultures; these, however, did not result in development of infection or other complications.
These data are in contrast to studies investigating standardized interventional endoscopic procedures. Amongst them, placement of percutaneous endoscopic gastrostomy (PEG) carries a high risk of intraabdominal infection. In a multicenter, retrospective analysis, Lee et al. demonstrated that the use of prophylactic antibiotics was effective in reducing fever without clinically evident infection (p = 0.01). Peristomal infection and peritonitis tended to be less with antibiotic therapy, but the differences failed to reach statistical significance [28].
Though our study is the first one (to our knowledge) that directly compares different anti-infective means to prevent infectious complications after interventional endoscopic procedures, some limitations need to be mentioned. (1) It remains unclear whether these results from an animal model can be directly transferred into humans. But nevertheless, due to ethical concern a similar study design in humans undergoing endoscopic interventions would be impossible. (2) Antibiotics were administered for three consecutive days starting directly after closure of the gastric wall, whereas local bactericides were (of course) only administered once. This fact might entail a pretest likelihood of showing that antibiotics are better than bactericides. Furthermore, an additional treatment arm combining antibiotics with gastric lavage might have been valuable. According to the ESGE consensus on diagnosis and management of iatrogenic endoscopic perforations, antibiotic prophylaxis is recommended when a perforation is observed. But this consensus statement does not delineate how frequently antibiotics should be administered post-interventionally. The studies cited by the ESGE consensus statement applied antibiotics for 1–10 days with a mean of approximately 3 days [29]. Therefore, based on the existing studies and our microbiological data an antibiotic prophylaxis for three consecutive days after iatrogenic perforation seems to be a feasible algorithm. (3) Though all mini-laparoscopies were carried out in a sterile manner, repeated intraperitoneal sampling entails a risk of translocation of additional bacteria, which may have implemented a bias to our data. Since we could not detect any bacteria in the PC at baseline, this potential bias is unlikely or may just play a minor role without any clinical significant effect.
Nevertheless, so far no infective prophylaxis has been recommended in interventional endoscopic procedures [26, 27]. However, when our data are taken into account, one might consider to changing this concept for those patients who have a considerable risk of perforation such as in EMR and ESD and hence have a chance to develop peritonitis [29].
Conclusion
The few available studies with varying settings and outcome make it very difficult to set standards in the prevention of infections related to interventional endoscopic procedures. So far, the variety of studies that exist assessing potential infectious complications of interventional endoscopic procedures all used different definitions for minor and major infections and different prophylactic anti-infective treatments [22–27, 30–32]. Thus, based on the current data no reliable statement can be made regarding post-operative infection rates and the most suitable anti-infective proceeding.
To our knowledge, our study is the first that exactly differentiates and quantifies the bacterial species translocated into the PC after different anti-infective treatments in an animal model with artificial perforation of the gastrointestinal lumen. Oral and gastric lavages induce a significant reduction of the bacterial load in the PC immediately after interventional endoscopic procedures, but in the long term, CFU and clinical signs of infection remain unaltered. Only the periinterventional use of antibiotics results in both a significant reduction of the intraabdominal bacterial load and markedly improves the clinical outcome at the time of follow-up. Therefore, antibiotic prophylaxis could be recommended as the solely prophylactic mean during interventional endoscopic procedures when a perforation is observed. Further studies are needed to determine whether these data can be transferred into routine clinical practice in humans.
References
Park YM, Cho E, Kang HY, Kim JM (2011) The effectiveness and safety of endoscopic submucosal dissection compared with endoscopic mucosal resection for early gastric cancer: a systematic review and meta-analysis. Surg Endosc 25(8):2666–2677
Tanaka S, Terasaki M, Hayashi N, Oka S, Chayama K (2013) Warning for unprincipled colorectal endoscopic submucosal dissection: accurate diagnosis and reasonable treatment strategy. Dig Endosc 25(2):107–116
Bourke MJ (2013) Endoscopic resection in the duodenum: current limitations and future directions. Endoscopy 45(2):127–132
Friedel D, Modayil R, Iqbal S, Grendell JH, Stavropoulos SN (2013) Per-oral endoscopic myotomy for achalasia: an American perspective. World J Gastrointest Endosc 5(9):420–427
Kopelman Y, Siersema PD, Bapaye A, Kopelman D (2012) Endoscopic full-thickness GI wall resection: current status. Gastrointest Endosc 75(1):165–173
Sugimoto T, Okamoto M, Mitsuno Y, Kondo S, Ogura K, Ohmae T, Mizuno H, Yoshida S, Isomura Y, Yamaji Y, Kawabe T, Omata M, Koike K (2012) Endoscopic submucosal dissection is an effective and safe therapy for early gastric neoplasms: a multicenter feasible study. Clin Gastroenterol 46(2):124–129
Von Renteln D, Fuchs KH, Fockens P, Bauerfeind P, Vassiliou MC, Werner YB, Fried G, Breithaupt W, Heinrich H, Bredenoord AJ, Kersten JF, Verlaan T, Trevisonno M, Rösch T (2013) Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology 145(2):309–311.e1–3
Hulagu S, Senturk O, Aygun C, Kocaman O, Celebi A, Konduk T, Koc D, Sirin G, Korkmaz U, Duman AE, Bozkurt N, Dindar G, Attila T, Gurbuz Y, Tarcin O, Kalayci C (2011) Endoscopic submucosal dissection for premalignant lesions and noninvasive early gastrointestinal cancers. World J Gastroenterol 17(13):1701–1709
Li QL, Yao LQ, Zhou PH, Xu MD, Chen SY, Zhong YS, Zhang YQ, Chen WF, Ma LL, Qin WZ (2012) Submucosal tumors of the esophagogastric junction originating from the muscularispropria layer: a large study of endoscopic submucosal dissection (with video). Gastrointest Endosc 75(6):1153–1158
Probst A, Pommer B, Golger D, Anthuber M, Arnholdt H, Messmann H (2010) Endoscopic submucosal dissection in gastric neoplasia—experience from a European center. Endoscopy 42(12):1037–1044
Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, Magee CA, Kantsevoy SV (2004) Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc 60(1):114–117
Meining A, Spaun G, Fernández-Esparrach G, Arezzo A, Wilhelm D, Martinek J, Spicak J, Feussner H, Fuchs KH, Hucl T, Meisner S, Neuhaus HJ (2013) NOTES in Europe: summary of the working group reports of the 2012 EURO-NOTES meeting. Endoscopy 45(3):214–217
Arezzo A, Zornig C, Mofid H, Fuchs KH, Breithaupt W, Noguera J, Kaehler G, Magdeburg R, Perretta S, Dallemagne B, Marescaux J, Copaescu C, Graur F, Szasz A, Forgione A, Pugliese R, Buess G, Bhattacharjee HK, Navarra G, Godina M, Shishin K, Morino M (2013) The EURO-NOTES clinical registry for natural orifice transluminal endoscopic surgery: a 2-year activity report. Surg Endosc 27(9):3073–3084
Rattner D, Kalloo A, ASGE/SAGES Working Group (2006) ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery. October 2005. Surg Endosc 20(2):329–333
Baron TH, Wong Kee Song LM, Zielinski MD, Emura F, Fotoohi M, Kozarek RA (2012) A comprehensive approach to the management of acute endoscopic perforations (with videos). Gastrointest Endosc 76(4):838–859
Fritscher-Ravens A, Ghanbari A, Holland C, Olagbeye F, Hardeler KG, Seehusen F, Jacobsen B, Mannur K (2009) Beyond NOTES: randomized controlled study of different methods of flexible endoscopic hemostasis of artificially induced hemorrhage, via NOTES access to the peritoneal cavity. Endoscopy 41(1):29–35
Fritscher-Ravens A, Ghanbari A, Thompson S, Patel K, Kahle E, Fritscher T, Niemann H, Koehler P, Milla P (2007) Which parameters might predict complications after natural orifice endoluminal surgery (NOTES)? Results from a randomized comparison with open surgical access in pigs. Endoscopy 39(10):888–892
Eickhoff A, Vetter S, von Renteln D, Caca K, Kähler G, Eickhoff JC, Jakobs R, Riemann JF (2010) Effectivity of current sterility methods for transgastric NOTES procedures: results of a randomized porcine study. Endoscopy 42(9):748–752
Beilenhoff U, Neumann CS, Rey JF, Biering H, Blum R, Cimbro M, Kampf B, Rogers M, Schmidt V, ESGE Guidelines Committee, European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates (2008) ESGE-ESGENA guideline: cleaning and disinfection in gastrointestinal endoscopy. Endoscopy 40(11):939–957
Narula VK, Happel LC, Volt K, Bergman S, Roland JC, Dettorre R, Renton DB, Reavis KM, Needleman BJ, Mikami DJ, Ellison EC, Melvin WS, Hazey JW (2009) Transgastric endoscopic peritoneoscopy does not require decontamination of the stomach in humans. Surg Endosc 23(6):1331–1336
Fitzner K, Heckinger E (2010) Sample size calculation and power analysis: a quick review. Diabetes Educ 36:701–707
Giday SA, Dray X, Magno P, Buscaglia JM, Shin EJ, Surti VC, Assumpcao L, Marohn MR, Ruben D, Zhigalin A, Pipitone LJ, Kantsevoy SV (2010) Infection during natural orifice transluminal endoscopic surgery: a randomized, controlled study in a live porcine model. Gastrointest Endosc 71(4):812–816
Azadani A, Jonsson H, Park PO, Bergström M (2012) A randomized trial comparing rates of abdominal contamination and postoperative infection among natural orifice transluminal endoscopic surgery, laparoscopic surgery, and open surgery in pigs. Gastrointest Endosc 75(4):849–855
Guarner-Argente C, Beltrán M, Martínez-Pallí G, Navarro-Ripoll R, Martínez-Zamora MÀ, Córdova H, Comas J, de Miguel CR, Rodríguez-D’Jesús A, Almela M, Hernández-Cera C, Lacy AM, Fernández-Esparrach G (2011) Infection during natural orifice transluminal endoscopic surgery peritoneoscopy: a randomized comparative study in a survival porcine model. J Minim Invasive Gynecol 18(6):741–746
Zheng YZ, Wang D, Gu JJ, Zhou MM, Yu Kong X, Xin Deng S, Ju SuX, Yin J, Gong YF, Wu RP, Li ZS (2011) An experimental study of betadine irrigation for preventing infection during the natural orifice transluminal endoscopic surgery (NOTES) procedure. J Dig Dis 12(3):217–222
Nau P, Ellison EC, Muscarella P Jr, Mikami D, Narula VK, Needleman B, Melvin WS, Hazey JW (2011) A review of 130 humans enrolled in transgastric NOTES protocols at a single institution. Surg Endosc 25(4):1004–1011.6
Dallemagne B, Perretta S, Allemann P, Donatelli G, Asakuma M, Mutter D, Marescaux J (2010) Transgastric cholecystectomy: from the laboratory to clinical implementation. World J Gastrointest Surg 2(6):187–192
Lee C, Im JP, Kim JW, Kim SE, Ryu DY, Cha JM, Kim EY, Kim ER, Chang DK, Small Intestine Research Group of the Korean Association for the Study of Intestinal Disease (KASID) (2013) Risk factors for complications and mortality of percutaneous endoscopic gastrostomy: a multicenter, retrospective study. Surg Endosc 27(10):3806–3815
Paspatis GA, Dumonceau JM, Barthet M, Meisner S, Repici A, Saunders BP, Vezakis A, Gonzalez JM, Turino SY, Tsiamoulos ZP, Fockens P, Hassan C (2014) Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy 46(8):693–711
ASGE TECHNOLOGY COMMITTEE, Kantsevoy SV, Adler DG, Conway JD, Diehl DL, Farraye FA, Kwon R, Mamula P, Rodriguez S, Shah RJ, Wong Kee Song LM, Tierney WM (2008) Endoscopic mucosal resection and endoscopic submucosal dissection. Gastrointest Endosc 68(1):11–18
Fong DG, Pai RD, Thompson CC (2007) Transcolonic endoscopic abdominal exploration: a NOTES survival study in a porcine model. Gastrointest Endosc 65(2):312–318
Raju GS, Pham B, Xiao SY, Brining D, Ahmed I (2005) A pilot study of endoscopic closure of colonic perforations with endoclips in a swine model. Gastrointest Endosc 62(5):791–795
Acknowledgments
We thank Vivian Hensel, Elaine Ibold and Elke Oldigs for excellent technical assistance and Dr. J. Hedderich for statistical advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. M. Ellrichmann received a ESGE EURO-NOTES Olympus research grant for the conduction of this study. K. G. Hadeler and Dres. S. Dhar, F. Seehusen, T. Cuming, A. T. Feßler, H. Niemann, S. Schwarz, A. Fritscher-Ravens have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Ellrichmann, M., Dhar, S., Hadeler, KG. et al. Risk of infection after iatrogenic perforation of the gut wall? Evaluation of preventive strategies in a randomized controlled animal trial. Surg Endosc 30, 3077–3088 (2016). https://doi.org/10.1007/s00464-015-4600-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-015-4600-4