Abstract
Post-stroke dysphagia is a prevalent, life threatening condition. Scientists recommended implementing behavioral therapies with new technologies such as transcranial direct current of stimulation (TDCS). Studies showed promising TDCS effects, and scientists suggested the investigation of the effectiveness of different montages. Supramarginal gyrus (SMG) is important in swallowing function. Our study aimed to investigate the effectiveness of stimulating SMG in improving post-stroke dysphagia. Forty-four patients finished the study (a randomized, double-blind one). All of them received behavioral therapy. The real group received anodal (2 mA, 20 min) stimulation on the intact SMG, and the sham group received the same for 30 s (5 sessions). Patients were assessed with Functional Oral Intake Scale (FOIS) and Mann Assessment of Swallowing Ability (MASA) after treatment and at one-month follow-up. The results showed that the difference between groups at baseline was not significant. According to MASA both groups improved significantly during the time (p-value < 0.001). The improvement in the real group was significantly higher than in the sham group after treatment (p-value = 0.002) and after one-month follow-up (p-value < 0.001). According to FOIS, most of the patients in the real group (72.70%) reached level 6 or 7 after one-month follow-up which was significantly higher than the sham group (31.80%, p-value = 0.007). In conclusion, TDCS applied to the scalp's surface associated with SMG localization may improve swallowing function in the stroke patients with dysphagia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Swallowing is a rapid, highly coordinated function [1] that requires the involvement of 26 pairs of muscles, five cranial nerves, and both peripheral nervous system and central nervous system [2]. Although this motor activity is effortless for most people [2], this is not the case for many stroke patients. Studies showed that swallowing difficulty (dysphagia) was very prevalent after stroke, and more than 50% of the patients face dysphagia, especially during the first weeks of stroke [2, 3]. According to the life-threatening complications of dysphagia, such as aspiration pneumonia, malnutrition, dehydration, and decreased quality of life, scientists recommend early management of dysphagia [4, 5].
Speech therapists often administer classic behavioral techniques with a long history of dysphagia management. Scientists classified these approaches into two main categories: compensatory techniques and rehabilitative ones. In compensatory techniques, liquid/ food modifications, positioning and swallowing maneuvers (such as supraglottic maneuver, hard swallow technique, etc.) might be administered. In rehabilitative techniques, sensory and physical stimulations (such as thermal tactile stimulation, sour stimulation, etc.) may be administered [6]. Although these techniques have shown promising results, their cost-effectiveness is still controversial [7,8,9]. Therefore, researchers tried to complement these techniques with new ones, such as non-invasive brain stimulation (NIBS), to promote recovery through enhancing neural plasticity [3, 10].
In recent years, one of the cost-effective NIBS techniques that have received attention for dysphagia management is transcranial direct current stimulation (TDCS) [3]. During TDCS, a direct electric current with an intensity usually between 1–2 mA is passed over the scalp and cranium external to the brain by two large surface electrodes covered in sponges soaked in saline. Due to the large size of the electrodes, the current density is low. This current modulates the activity of sodium and calcium channels as well as NMDA receptors. The change in the polarity and direction of the current flow can enhance (anodal) or depress (cathodal) the excitability of the neurons [3, 11,12,13]. Kumar et al. (2011) investigated the effect of anodal TDCS on the intact sensory-motor cortex, in post-stroke dysphagia for the first time and got promising results [14]. After that, other scientists investigated the impact of TDCS on pharyngeal motor cortex or sensory-motor cortex in post-stroke dysphagia with different methodologies and offered the hope for these patients that TDCS has the potential to enhance and facilitate the swallowing function [14,15,16,17,18].
Although TDCS showed positive outcomes in dysphagia post-stroke trials, there is still a need for more extensive research before it can be viewed as a viable clinical treatment for post-stroke dysphagia [2]. Scientists recommended that different stimulation sites, doses and patients be investigated so that TDCS can be offered differently according to the patients’ characteristics and as an individualized treatment for the patients [2, 19]. Recent MRI studies in stroke patients showed several cortical regions that can play an important role in swallowing. Supramarginal gyrus (SMG) is one of these regions that appears to play a role in the laryngeal vestibule closure and is associated with reduced residue. This region can be important in the safety of swallowing [20]. SMG (area 40 Broadman) is a part of somatosensory-associated cortex that can play a role in proprioception, an essential role in motor control [21]. SMG might have a pivotal role in the coordination of swallowing [20]. To the best of our knowledge, there is no study on the effectiveness of stimulating SMG for dysphagia management. Therefore, our study aimed to investigate the effectiveness of stimulating SMG for post-stroke dysphagia. We hypothesize that stimulating this region effectively promotes dysphagia recovery, and this region can be viewed as a new site for stimulation in NIBS.
Methods
Patients
This is a parallel-group, concealed, double-blinded, randomized clinical trial in which 44 patients finished the study. Stroke patients (> 24 h from their stroke onset) who were admitted between February 2021 and November 2021to the neurology wards and stroke units of Shiraz University of Medical Sciences hospitals and met the inclusion criteria were enrolled in the study. The inclusion criteria were age 18 years or over, presence of ischemic stroke confirmed with brain imaging, and diagnosis of dysphagia according to Northwestern Dysphagia Patient Check Sheet Screening (NDPCS). Exclusion criteria were hemorrhagic or lacunar stroke, previous history of dysphagia, presence of neurological disorders other than stroke or neurodegenerative disorders, auditory and/ or visual condition interfering with speech therapist or assessor or technician’s instruction, history of seizures, those with cardiac pacemaker or metallic implants, previous history of skull surgery or current need of skull surgery, presence of a tracheal cannula, an unstable medical condition which can interfere with the study process (such as hemodynamic instability, decreased level of consciousness, etc.), and inability to stay alert during treatment.
This study was done during the COVID- 19 pandemic. For the safety of both patients and the research group, none of the patients recruited for the study had active SARS- COV- 2 infections or a history of infection in the last 14 days.
Assessment Tools
The Functional Oral Intake Scale (FOIS), our primary outcome measure, is a valid and reliable scale sensitive to changes in functional oral intake. It is an appropriate tool for estimating and documenting the changes in the functional eating abilities of stroke patients over time in 7 levels (level 1: nothing by mouth, level 2: tube- dependent with a minimal attempt of food or liquid, level 3: tube-dependent with consistent oral intake of food or liquid, level 4: oral diet, single consistency, level 5: oral diet, multiple consistencies, requiring special compensation or preparation, level 6: oral diet, multiple consistencies, no special preparation, specific food limitation, and level 7: total oral diet with no restrictions) [22]. In this study we defined 2 levels or more improvement according to FOIS as an acceptable level of improvement. We also reported the prevalence of the patients who reached level 6 and 7 which are the levels with no need for special food preparation.
The Mann Assessment of Swallowing Ability (MASA), our secondary outcome measure, is a valid and reliable tool designed to be administered for stroke subjects aged 18 years or over. It is designed to yield the swallowing abilities of the patients while assessing 24 items. The maximum score of MASA is 200; according to the score obtained, the patients can be grouped into 4 categories of dysphagia severity (nil abnormality detected = 178–200, mild = 168–177, moderate = 139–167, and severe ≤ 138). It also has cutoff score for the severity grouping of aspiration [23].
The National Institute of Health Stroke Scale (NIHSS) is a valid and reliable tool designed to yield the stroke severity of the patients. It has 15 questions with multiple Likert-type scales. The minimum possible score is 0 and the maximum 42. According to the score obtained, the patient can be grouped into 4 categories (minor stroke = 1–4, moderate stroke = 5–15, moderate to severe stroke = 16–20, severe stroke = 21–42) [24, 25]. In this study, NIHSS was used to group the patients according to the severity of their stroke.
Study Process
The speech therapist, a PhD student of neuroscience, screened and interviewed the patients and caregivers provided them with information about the project, collected the demographic data, and administered the behavioral treatment of the patients in 5 sessions. The neuroscientist also trained all the personnel of the team before beginning the study and coordinated the project.
We classified the patients into four groups according to their stroke and dysphagia scores to minimize the clinical differences between the patients. Therefore, the patients were matched based on the NIHSS and MASA scale. The table consisted of 4 groups [group one: (NIHSS = 1–15, MASA = 139–177), group two: (NIHSS = 1–15, MASA ≤ 138), group three: (NIHSS = 16–42, MASA = 139–177), and group four: (NIHSS = 16–42, MASA ≤ 138)] with 12 blocks which enabled a stratified randomization using permuted blocked randomization in each group. This randomly allocated table was prepared using random allocation software before data collection was started. Only the secretary had access to this table during data collection.
All the patients who met the inclusion criteria and signed the informed consent were assessed and allocated into groups. For the patients who could not sign the informed consent due to their clinical conditions signed consent was obtained from their next of kin. The study was approved by the Ethics Committee of Kerman University of Medical Sciences (IR.KMU.REC.1399.366) and registered in the Iranian Registry of Clinical Trials (IRCT20200520047521N1).
After meeting the inclusion criteria and signing the consent form, all the patients were assessed by NIHSS, MASA scale and FOIS. The classification and results of the scales were given to the secretary, who was trained to do the allocation process, and the patients were randomly assigned 1:1 to receive real or sham stimulation. After allocation, the secretary wrote the names of the group of the patients (sham or real) in an envelope and gave it to the TDCS technician. The secretary maintained all the patients’ documents from the screening phase to the last assessment in the follow-up phase.
All the patients and their families, the assessor, the speech therapist, and stroke physicians were blind to allocating the patients to the groups (real or sham). A TDCS technician who was trained and employed to deliver the TDCS performed the procedure. They were independent of the investigators and was unaware of the study’ methodology. The secretary informed her about the group of the patients (real or sham TDCS) in a sealed envelope. Therefore, the only persons who knew the group of the patients (sham or real) were the secretary and the technician of TDCS.
All the patients were assessed by the outcome measures, at the baseline, one day after the last day of the intervention, and after one-month follow-up.
Patients who were discharged from the hospital before finishing the five therapy sessions were referred to Shiraz Medical Sciences outpatient centers to continue their therapy. Every day, the neurologist assessed the patients to detect any potential unintended stimulation effect of TDCS. Also, the speech therapist reported any effects during or after therapy that the patients or their families/caregivers reported, such as itching, pain, burning, warmth/heat, metallic/iron taste, fatigue, and alertness decrease.
Study Interventions
Stimulation was delivered by transcranial electrical stimulation device (Neurostim 2, Medina Teb Gostar Company, Iran) through a pair of carbon pad electrodes in saline-soaked sponges. The Anode electrode (4*4 cm) was placed on the intact supra marginal gyrus (CP5 or CP6 according to 10- 10 international EEG system) [26]. SMG was localized based on the 10–10 EEG system, using an EEG cap with 64 points. We had three sized EEG caps which were selected according to the head circumference of the patients. To localize CP5/CP6, we first measured the distance between the anatomical landmarks nasion, inion, and left/right preauricular points to locate CZ. The CZ location was marked with a cross mark. Afterward, the EEG cap was placed on the head of the participants. SMG was located at CP5/CP6. We marked this point with spot.
The neuroscientist of the team did the localization process, and the TDCS technician and sometimes the secretary helped them control the head position of the patients (especially for those who could not control their heads) for better accuracy. We located the spot in the middle of the anode electrode. For the patients with brainstem ischemic stroke, the electrode was placed on the right hemisphere due to the probability of the right dominance lateralization for swallowing, which was found in recovered brainstem stroke patients [17, 27]. The neurologist determined the side of the Anode placement. The reference electrode (4*6 cm) was placed on the contralateral supraorbital region. The current intensity was 2 mA for 20 min for five days (one session in a day). The current density of the TDCS anodal pad used was 0.125 mA/cm 2. For patients in the sham group, the same montage was performed. The only difference was that the patients received the current only for 30 s at the beginning and the end of the period, which was a sham procedure in producing the transient skin sensation similar to real procedure without producing any sustainable effects. During stimulation, all the patients received behavioral therapy according to their condition. These techniques consisted of different passive and active rehabilitative techniques and swallow maneuvers. After each session, the patients/ caregivers received 10 min consultation with the speech therapist about the food modification (if applicable for the patient), positioning, and the behavioral techniques which were used for the patient.
Calculation of Sample Size
We calculated the sample size on the basis of a previous study that reported real and sham means of the swallowing function as 3.5 ± 0.9 and 4.7 ± 0.9 [18]. The calculation of the sample size was performed by assuming type I error of 0.05 and a power of 80%. Using the sample size formula for two independent means, the number of subjects to be enrolled was found to be 24 per group. It should be noted that to achieve more reliable results, we increase the sample size by decreasing the mean difference between the two groups to d = 0.74.
Statistical Analysis of Data
In this study, descriptive values were presented as mean (SD) or number (percentage). The normality of variables was assessed by Kolmogorov—Smirnov test. Because of the absence of normal distribution, nonparametric testing was performed using Mann–Whitney U and Freedman tests. Dunn-Bonferroni post hoc test was used for pairwise comparisons. Also, The χ2 test or Fishers’ exact test were used to compare the groups in case of categorical data. The significance level was ≤ 0.05.
Results
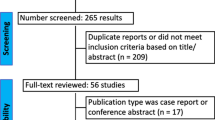
Amongst 132 patients who were screened for eligibility, 48 were randomized into two groups, and 44 patients finished the study (Fig. 1). Most of the patients (65. 90%) in this study were elderly people (≥ 65 years old). The mean age of the participants was 68.00 (16.37), the minimum age was 24 years old, and the maximum was 94 years old. Most of the patients were male (52.30%), and few of them reported a previous history of Corona (18.20%). More than half of the patients (65.90%) were fed by an NG tube at the baseline. The patients’demographic characteristics, stroke characteristics, and outcome measures showed no significant difference between the groups at baseline (Table 1).
According to our outcome measures, both groups revealed significant improvement after five days of therapy and one-month follow-up. The improvement was significantly higher in the real group than in the sham one (Table 2).
According to the FOIS scale, most of the patients in the real group (n = 20, 90.90%) showed two levels or more improvement after treatment which was significantly higher than the sham group (p-value < 0.001). After one-month follow-up, many patients (n = 16, 72.70%) in the sham group reached them and improved for two levels or more (p-value = 0.24) (Table 3).
Also, in the real group, many patients (n = 13, 59.10%) reached level 6 or 7 according to the FOIS scale post-treatment, which was significantly higher in the real group than the sham one (p-value = 0.01). After one-month follow-up, this significant difference in improvement in the real group compared to the sham group existed (p-value = 0.007) (Table 3).
According to the MASA score, both groups showed significant improvement over time (p-value < 0.001). According to the pairwise comparisons of the time of assessments, the sham group showed non-significant improvement from post-treatment to the follow-up. In contrast, the real group significantly improved from post-treatment to the follow-up score (Table 4).
Itching (which was tolerable for patients during treatment) was reported for 3 (13.60%) patients in the real group, but none of the patients in the sham group had such a report or other reports about side effects of TDCS.
Two of the patients in this study suffer from brainstem stroke. Both of them were in the real group, and their swallowing function and ability showed improvement after treatment and at one-month follow-up (Table 5).
Discussion
This study is the first randomized clinical trial study investigating the effect of stimulating supramarginal gyrus with TDCS combined with behavioral therapy in patients with post-stroke dysphagia. Our data showed that anodal stimulation of SMG improved the swallowing ability and function of the patients in the real group significantly compared to the sham group both after five treatment sessions and one-month follow-up.
The supramarginal gyrus, located in the inferior parietal lobe (the rostral part), is amongst the somatosensory association cortex, which plays a role in interpreting tactile sensory information and in the perception of space as well as in internally guided movements (active movements). It is suggested that especially the right SMG is pivotal for central processing of proprioception which is necessary for precise motor control [21]. On the other hand, SMG is among the regions containing mirror neurons. These are “a distinctive class of neurons that discharge both when an individual performs a motor act and observes another individual performing the same or a similar motor act” [28]. Studies showed that SMG contained mirror neurons that would be activated during oral movements related to swallowing acts such as biting [29].
Studies that map the lesion locations of the stroke to physiological swallow impairments showed that SMG might be crucial for coordination of swallowing [20] because SMG deficit was associated with impaired laryngeal vestibular closure and pharyngeal residue and cough response [20, 30]. According to the magnetoencephalography (MEG) studies, in post-stroke dysphagic patients who were improved after swallowing treatments, SMG of the stimulated hemisphere was amongst the regions (such as the primary and secondary sensorimotor cortex, dorsolateral prefrontal cortex, and posterior cingulate) which showed a significant increase of activation in the swallowing network [17]. According to our data, it seems that this region can be viewed as an alternative in swallowing neurorehabilitation field.
Our results are in line with those of the previous studies which stimulated the pharyngeal sensory motor cortex in post-stroke dysphagia or the swallowing motor cortex in the elderly and showed promising results [17, 31]. Studies showed that different montages with placing electrodes on different locations of the cranium had the potential to change the results of TDCS stimulation [32]. It is believed that even a 1 to 1.5 cm shift in electrode location had the potential to significantly change the electrical field’ s distribution [33, 34]. Also, different characteristics of stimulation and physical arrangements of electrodes, such as electrode distance, current intensity, and stimulation duration, are the important factors for the physiological and functional effects of TDCS [35]. Although our results are in line with the previous ones with different montages, there is still unclear which one of these montages is the most effective one for the patients with dysphagia post-stroke. So, there is a need for further investigations comparing the effectiveness of different montages in this group of patients in the future. On the other hand, clinicians should take the individual characteristics of their patients into account when they tend to select between different alternatives of the montages.
According to the FOIS level, more than half of the patients in the real group (59.10%) reached level 6 or 7 after treatment. Most of them (72.70%) showed such an improvement after one-month follow-up significantly higher than the improvement in the sham group. Studies showed that oral intake level correlated positively with the self-confidence, attendance in social events, and quality of life of patients [36, 37]. It seems that complementing behavioral therapy with TDCS has the potential to improve not only the swallowing function and ability of the patients but also their mental health and quality of life. Therefore, there is a need to investigate the effects of such therapies on the patient’s mental health and quality of life after treatment and during the time.
According to the investigation of improvement during time, MASA scores in both real and sham groups improved over time. The improvement from post-treatment to the follow-up was significantly higher in the real group, but there was a non-significant improvement from post-treatment to the follow-up in the sham group (Table 4). This long-lasting effect may be due to the capacity of TDCS stimulation to induce a higher order of neuroplasticity [38,39,40], which is called the meta-plasticity [40,41,42,43,44,45]. This meta-plasticity regulates the synaptic plasticity when the brain stimulation is paired with repeated tasks that induce synaptic plasticity [45, 46]. Dysphagia scientists recommended pairing brain stimulation with the behavioral repeated tasks to improve the effectiveness of these techniques in the literature [11]. The neurophysiological bases of the long-lasting effect of TDCS in dysphagia therapy is an important issue that can help us understand the underlying mechanisms of this effect, and there is a gap in this field. Therefore, we recommend that the necessity of such investigations should be kept in mind for future research.
In this study, we stimulated the intact hemisphere based on previous meta-analysis results. The results of that study showed that stimulating the intact hemisphere in post-stroke dysphagic patients had a moderate significant pooled effect size than stimulating the lesioned side with a moderate non-significant pooled effect size [10]. Although the results of that meta-analysis confirmed that stimulating the unaffected hemisphere can produce a larger magnitude of improvement in dysphagia, we should keep in mind that some variables such as the stimulation duration, lesion type, location, size and stroke type, and other methodological issues have the potential to oppose those outcomes [10]. Therefore, there are still controversies about the effectiveness of the affected versus unaffected hemisphere stimulation. Each of these methodologies has it’ s followers according to their theories. So, there is still a need for further investigations in this area.
In our study, there were only two patients with brainstem stroke as the prevalence of this stroke is too small generally. Both patients’ swallowing function and ability were improved after treatment and at one-month follow-up. The central pattern generator (CPG) of swallowing, which is essential in the pharyngeal phase, is located in the brainstem [47]. Studies showed that patients with brainstem strokes showed different clinical symptoms than the hemispheric strokes [48, 49]. The brainstem stroke patients showed fewer cognitive deficits than the hemispheric ones. On the other hand, studies showed that medullary and cerebellar stroke patients are more likely to aspirate severely [48, 49]. Although these patients showed more severe dysphagia than the hemispheric ones, it seems that they had a better long-term prognosis than the hemispheric stroke patients [50, 51]. Data from our study showed that these patients could benefit from rehabilitation techniques complemented with TDCS. However, the small number of brainstem stroke patients was a barrier to do any subgroup analysis to investigate whether brainstem stroke patients benefit from TDCS equally compared to the hemispheric stroke patients. Therefore, there is a need to conduct a research in the brainstem group of stroke patients to investigate the amount of the benefit they gained from therapies according to their clinical symptoms of dysphagia.
Study Limitations
We located SMG according to 10- 10 international EEG system in this study. However, this localization technique is commonly used in research protocols of TDCS studies in post-stroke dysphagia [14,15,16,17,18] because of its applicability, low cost, and availability [32]. Some studies showed that other techniques, such as function-guided procedures using Transcranial Magnetic Stimulation (TMS) or the Neuronavigation techniques using Magnetic Resonance Imaging (MRI), are more accurate than the 10–20 EEG system [52, 53]. However, the expense and highly specialized requirement of MRI and even TMS make it unfeasible for most clinical settings [32]. Therefore, it deserves further investigation into whether treatment protocols in post-stroke dysphagia with 10- 20 EEG system localization have the same effects as those with TMS or MRI localizations. Also, in this study the sample size was still too small to do subgroup analysis according to the severity of dysphagia. Therefore, we recommend studies with larger sample sizes to analyze the swallowing improvement according to the severity of dysphagia.
Conclusions
In conclusion, TDCS is a portable, easily accessible, and non-invasive device which does not cause any intolerable side effects for the patients and can be viewed as a complementary treatment for dysphagia post-stroke. Our study demonstrated that stimulating SMG could improve the swallowing ability and function of the patients, and there is a need to investigate the effects of different montages on different patients to reach an individualized protocol for the management of dysphagia post-stroke. Although there are promising results of using TDCS protocols, there is still a need for larger sample sizes in different populations of stroke patients. On the other hand, to avoid malpractice of health care providers in working with TDCS, we need guidelines, educational workshops, and courses for this group as improving healthcare providers’ knowledge will positively affect the quality of care for the patients [54]. In this regard, policymakers and industries are amongst the stakeholders who can help improve knowledge about evidence-based practice in post-stroke dysphagia [55].
References
Dziewas R, et al. European stroke organization and European society for swallowing disorders guideline for the diagnosis and treatment of post-stroke dysphagia. Eur Stroke J. 2021. https://doi.org/10.1177/23969873211039721.
Simons A, Hamdy S. The use of brain stimulation in dysphagia management. Dysphagia. 2017;32(2):209–15.
Cheng I, Sasegbon A, Hamdy S. Effects of neurostimulation on poststroke dysphagia: a synthesis of current evidence from randomized controlled trials. Neuromodulation. 2020. https://doi.org/10.1111/ner.13327.
Clavé P, Shaker R. Dysphagia: current reality and scope of the problem. Nat Rev Gastroenterol Hepatol. 2015;12(5):259–70.
Fairfield CA, Smithard DG. Assessment and management of dysphagia in acute stroke: an initial service review of international practice. Geriatrics. 2020;5(1):4.
Bath PM, Lee HS, Everton LF. Swallowing therapy for dysphagia in acute and subacute stroke. Cochrane Database Sys Rev. 2018. https://doi.org/10.1002/14651858.CD000323.pub3.
Geeganage C, et al. Interventions for dysphagia and nutritional support in acute and subacute stroke. Cochrane Database Sys Rev. 2012. https://doi.org/10.1002/14651858.CD000323.pub2.
Speyer R, et al. Effects of therapy in oropharyngeal dysphagia by speech and language therapists: a systematic review. Dysphagia. 2010;25(1):40–65.
Bonilha HS, et al. The one-year attributable cost of post-stroke dysphagia. Dysphagia. 2014;29(5):545–52.
Pisegna JM, et al. Effects of non-invasive brain stimulation on post-stroke dysphagia: a systematic review and meta-analysis of randomized controlled trials. Clin Neurophysiol. 2016;127(1):956–68.
Vasant DH, et al. Transcranial direct current stimulation reverses neurophysiological and behavioural effects of focal inhibition of human pharyngeal motor cortex on swallowing. J Physiol. 2014;592(4):695–709.
Yang SN, et al. Effectiveness of non-invasive brain stimulation in dysphagia subsequent to stroke: a systemic review and meta-analysis. Dysphagia. 2015;30(4):383–91.
Lefaucheur J-P. A comprehensive database of published tDCS clinical trials (2005–2016). Clin Neurophysiol. 2016;46(6):319–98.
Kumar S, et al. Noninvasive brain stimulation may improve stroke-related dysphagia: a pilot study. Stroke. 2011;42(4):1035–40.
Yang EJ, et al. Effects of transcranial direct current stimulation (tDCS) on post-stroke dysphagia. Restor Neurol Neurosci. 2012;30(4):303–11.
Ahn YH, et al. Effect of bihemispheric anodal transcranial direct current stimulation for dysphagia in chronic stroke patients: a randomized clinical trial. J Rehabil Med. 2017;49(1):30–5.
Suntrup-Krueger S, et al. Randomized trial of transcranial direct current stimulation for poststroke dysphagia. Ann Neurol. 2018;83(2):328–40.
Shigematsu T, Fujishima I, Ohno K. Transcranial direct current stimulation improves swallowing function in stroke patients. Neurorehabil Neural Repair. 2013;27(4):363–9.
Michou E, Hamdy S. Neurostimulation as an approach to dysphagia rehabilitation: current evidence. Curr Phys Med Rehabil Rep. 2013;1(4):257–66.
Wilmskoetter J, et al. Mapping acute lesion locations to physiological swallow impairments after stroke. NeuroImage Clin. 2019. https://doi.org/10.1016/j.nicl.2019.101685.
Ben-Shabat E, et al. The right supramarginal gyrus is important for proprioception in healthy and stroke-affected participants: a functional MRI study. Front Neurol. 2015;6:248.
Crary MA, Mann GDC, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86(8):1516–20.
Mann G. MASA: the mann assessment of swallowing ability, vol. 1. Boston: Cengage Learning; 2002.
Fischer U, et al. NIHSS score and arteriographic findings in acute ischemic stroke. Stroke. 2005;36(10):2121–5.
Dehghani R, et al. Validity and reliability of the persian versions of national institute of health stroke scale and modified national institute of health stroke scale in hospitalized patients. Galen Med J. 2019;8:1188.
Koessler L, et al. Automated cortical projection of EEG sensors: anatomical correlation via the international 10–10 system. Neuroimage. 2009;46(1):64–72.
Teismann IK, et al. Cortical swallowing processing in early subacute stroke. BMC Neurol. 2011;11(1):1–13.
Acharya S, Shukla S. Mirror neurons: enigma of the metaphysical modular brain. J Nat Sci Biol Med. 2012;3(2):118.
Buccino G, et al. Neural circuits involved in the recognition of actions performed by nonconspecifics: an fMRI study. J Cogn Neurosci. 2004;16(1):114–26.
Suntrup-Krueger S, et al. The impact of lesion location on dysphagia incidence, pattern and complications in acute stroke. Part 2: oropharyngeal residue, swallow and cough response, and pneumonia. Eur j Neurol. 2017;24(6):867–74.
Cosentino G, et al. Anodal transcranial direct current stimulation and intermittent theta-burst stimulation improve deglutition and swallowing reproducibility in elderly patients with dysphagia. Neurogastroenterol Motil. 2020;32(5):e13791.
Solomons CD, Shanmugasundaram V. Transcranial direct current stimulation: a review of electrode characteristics and materials. Med Eng Phys. 2020;85:63–74.
Woods AJ, Bryant V, Sacchetti D, Gervits F, Hamilton R. Effects of electrode drift in transcranial direct current stimulation. Brain stimul. 2015;8(3):515–9.
ÁguidaFoerster F, LeilaFarnad A, WalterPaulus MA, Nitsche MF. Effects of electrode angle-orientation on the impact of transcranial direct current stimulation on motor cortex excitability. Brain Stimul. 2019;12(2):263–6.
Nasseri P, Nitsche MA, Ekhtiari H. A framework for categorizing electrode montages in transcranial direct current stimulation. Front Hum Neurosci. 2015. https://doi.org/10.3389/fnhum.2015.00054.
Hong DG, Yoo DH. A comparison of the swallowing function and quality of life by oral intake level in stroke patients with dysphagia. J Phys Ther Sci. 2017;29(9):1552–4.
Kim JY, et al. The mediating and moderating effects of meaning in life on the relationship between depression and quality of life in patients with dysphagia. J Clin Nurs. 2019;28(15–16):2782–9.
Nitsche MA, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol. 2000;527(3):633–9.
Nitsche MA, Paulus W. Transcranial direct current stimulation–update 2011. Restor Neurol Neurosci. 2011;29(6):463–92.
Cheng I, Hamdy S. Metaplasticity in the human swallowing system: clinical implications for dysphagia rehabilitation. Neurol Sci. 2021. https://doi.org/10.1007/s10072-021-05654-9.
Cheeran B, et al. A common polymorphism in the brain-derived neurotrophic factor gene (BDNF) modulates human cortical plasticity and the response to rTMS. J Physiol. 2008;586(23):5717–25.
Fritsch B, et al. Direct current stimulation promotes BDNF-dependent synaptic plasticity: potential implications for motor learning. Neuron. 2010;66(2):198–204.
Meinzer M, et al. Transcranial direct current stimulation over multiple days improves learning and maintenance of a novel vocabulary. Cortex. 2014;50:137–47.
Stagg CJ, Nitsche MA. Physiological basis of transcranial direct current stimulation. Neuroscientist. 2011;17(1):37–53.
Costanzo F, et al. Long-lasting improvement following tDCS treatment combined with a training for reading in children and adolescents with dyslexia. Neuropsychologia. 2019;130:38–43.
Hulme SR, et al. Mechanisms of heterosynaptic metaplasticity. Phil Trans R Soc B. 2014;369(1633):20130148.
Bautista TG, Sun Q-J, Pilowsky PM. The generation of pharyngeal phase of swallow and its coordination with breathing: interaction between the swallow and respiratory central pattern generators. Prog Brain Res. 2014;212:253–75.
Teasell RW, McRae MP, Finestone HM. Social issues in the rehabilitation of younger stroke patients. Arch Phys Med Rehabil. 2000;81(2):205–9.
Teasell R, et al. Clinical characteristics of patients with brainstem strokes admitted to a rehabilitation unit. Arch Phys Med Rehabil. 2002;83(7):1013–6.
Turney T, Garraway W, Whisnant J. The natural history of hemispheric and brainstem infarction in Rochester Minnesota. Stroke. 1984;15(5):790–4.
Kjaersgaard A, Pallesen H. First-hand experience of severe dysphagia following brainstem stroke: two qualitative cases. Geriatrics. 2020;5(1):15.
De Witte S, et al. Left prefrontal neuronavigated electrode localization in tDCS: 10–20 EEG system versus MRI-guided neuronavigation. Psychiatry Res Neuroimaging. 2018;274:1–6.
Sparing R, et al. Transcranial magnetic stimulation and the challenge of coil placement: a comparison of conventional and stereotaxic neuronavigational strategies. Hum Brain Mapp. 2008;29(1):82–96.
Farpour S, et al. Dysphagia management in Iran: knowledge, attitude and practice of healthcare providers. Dysphagia. 2019;34(1):105–11.
Farpour S, Farpour HR, Smithard DG. Oropharyngeal dysphagia and its related health problems in Iranian elderly people: a scope of work for the future. Eur J Integr Med. 2018;21:94–100.
Acknowledgements
This manuscript was a part of Sima Farpour's thesis (NO. 99000137) approved by the Medical Ethics Committee of Kerman University of Medical Sciences, Kerman, Iran, with the Reference Number “IR.KMU.REC.1399.366”. The authors would like to thank Kerman Neuroscience Research Center, Kerman University of Medical Sciences, Kerman, Iran, for their funding support. The authors would like to thank the Center for Developing Clinical Research of Nemazee Hospital, Dr. Parisa Chamanpara,Dr. Nasrin Shokrpour, the Research Consultation Center (RCC) of Shiraz University of Medical Sciences, Shiraz, Iran, and Dr. Zahra Bagheri for their statistical and editorial assistance. The authors would also like to thank all the patients and their families/caregivers and head nurses and nurses who helped us to conduct this project.
Funding
The work received support from Kerman Neuroscience Research Center, Institute of Neuropharmacology, Kerman University of Medical Sciences, Kerman, Iran (No. 99000137).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Farpour, S., Asadi-Shekaari, M., Borhani Haghighi, A. et al. Improving Swallowing Function and Ability in Post Stroke Dysphagia: A Randomized Clinical Trial. Dysphagia 38, 330–339 (2023). https://doi.org/10.1007/s00455-022-10470-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-022-10470-0