Abstract
Deglutition complaints are frequent after thyroidectomy. The purpose of this study was to follow-up on patients with thyroidectomy indication to compare the videoendoscopic evaluation of swallowing on the seventh day (early postoperative, EPO) and on the 60th day after thyroidectomy, (late postoperative, LPO) and to compare patients that evolved with normal laryngeal mobility (NLM) and abnormal laryngeal mobility (ALM). Nasofibroscopic evaluation was performed preoperatively (PRE), on the EPO and LPO. Two groups were compared: ALM and NLM. The majority of people were women, age bracket 46–65, who underwent total thyroidectomy and with high frequency of carcinoma. 30 out of the 54 patients in the study had change in swallowing (55 %). Dysphagia occurred in 87 % (13/15) of patients with ALM in the EPO and remained in 67 % of them in the LPO. In the NLM group, dysphagia occurred in 44 % (17/39) in EPO and 25 % in LPO. There was a statistical difference between PRE and EPO, and PRE and LPO (P < 0,001). In the ALM group, liquid penetration and aspiration were identified in 33 % of the cases during EPO (P = 0,014); retention of food occurred in 87 % in EPO and in 60 % in LPO (P < 0,001). Dysphagia occurs in patients after thyroid surgery (regardless of larynx mobility alteration) and characterized by stasis of food in the oro and hypopharynx, which is also noticed in LPO, though more frequently in EPO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroidectomy is a largely performed procedure [1]. Dysphonia and dysphagia are common after thyroidectomy and can cause huge impact on the patient’s quality of life [2, 3]. Voice and swallowing complaints occur between 15 and 90 days after surgery [4–6]. Though spontaneous complaints of swallowing are not common, it has been observed that when questioned about this specific aspect, the frequency of complaints is similar to that for voice. [6]. However, published studies indicate that the incidence of dysphagia in thyroid disease affects around 58 % of patients undergoing lobectomy or complete thyroidectomy for malignant or benign tumor [1, 7]. Scerrino et al. indicate that regarding treatment of benign tumor after thyroidectomy, 20 % of patients had dysphagia when evaluated by Swallowing Impairment Score (SIS). [8].
These changes can derive from several factors, including surgical manipulation, palpation of the thyroid gland, scar retraction, and the possibility of injury to the external branch of the recurrent laryngeal nerve (RLN) and superior laryngeal nerve (SLN) [9–11]. Factors such as endotracheal intubation, neural plexus injury, and changes in vascular supply and pain reaction also deserve attention [4, 10, 12, 13]. There may be interconnection among these symptoms, since the presence of pain and discomfort can be the result of manipulation of perithyroidean muscles as well as of the intubation and the scar itself, which may lead to a feeling of tightness and difficulty in swallowing [4, 10, 13, 14]. This assumption is in line with the study of Lee et al. comparing thyroidectomy surgical techniques in the conventional model versus robotic surgeries. Patients who underwent robotic surgery had lower rates of dysphagia than those submitted to the conventional method [15], suggesting that surgical manipulation can be a differentiating factor for the emergence of these symptoms in the postoperative period.
The impact of surgical approaches to cervical swallowing disorders was assessed by surface electromyography and videofluoroscopy and the results reveal that there is stasis of food in the valleculae and pyriform sinus, even in patients without changes in laryngeal mobility [16].
The investigation of swallowing symptoms and signs is essential [4–6], as well as the remarkable differences between patients with normal laryngeal mobility (NLM) and abnormal laryngeal mobility (ALM) [6].
When investigating dysphagia, there is a great emphasis on symptom analysis, but few studies have been conducted that take into account clinical and instrumental analysis of swallowing [17]. Researches usually focus more extensively on severe dysphagia related to ALM [18], but complaints also occur in individuals with NLM [6], which makes the objective analysis of swallowing provided by imaging and functional evaluation essential. Clinical and instrumental analyses of swallowing (both functional evaluation and by imaging), in patients with NLM or ALM after thyroidectomy, are prospectively provided in this study.
Lombardi et al. [17, 19] present prospective studies that reinforce the presence of swallowing difficulties in patients without laryngeal nerve injury (superior or inferior) diagnosed by deep electromyography, however, these studies do not include clinical or instrumental analyses of swallowing.
There are impacts in swallowing caused by the cervical access used in the traditional thyroidectomy [16, 20, 21]. Jung et al. [20] have identified these impacts by videofluoroscopy analysis in a prospective study. Despite the videofluoroscopy being considered as the gold standard in the evaluation of biodynamic swallowing, nasal endoscopy allows you to view the vocal folds mobility and laryngeal function [22, 23], which is more compatible with the analysis of the complaints reported in postoperative thyroidectomy, such as discomfort in swallowing, choking, coughing, throat clearing, and the “blocked throat” feeling [6].
The purpose of this prospective study was to follow-up on hospitalized patients with thyroidectomy indication to compare the videoendoscopic evaluation of swallowing on the seventh day (early postoperative, EPO) vis-à-vis an evaluation on the 60th day after thyroidectomy, (late postoperative, LPO). The objective of the procedure was to compare patients that evolved with normal laryngeal mobility (NLM) and abnormal laryngeal mobility (ALM).
The hypothesis of this study is that patients with NLM or ALM after thyroidectomy have swallowing disorders. Patients with ALM after thyroidectomy have penetration and aspiration in EPO and retention of bolus in the EPO and LPO. Patients with NLM after thyroidectomy also have swallowing disorders, but without penetration and aspiration in the EPO and LPO periods. They have retention of bolus during the EPO and will maintain this until the LPO.
Methods
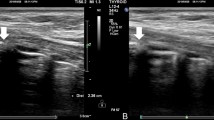
A comparative prospective study was performed. Data collection occurred through the 10 month-period of study. Ninety seven (97) patients with thyroid disease admitted to the infirmary in the Department of Head and Neck Surgery (DHNS), at the Clinical Hospital of the University of São Paulo—USP (Fig. 1).
Inclusion criteria were adult patients (both genders) admitted to the infirmary of DHNS, indicated to thyroidectomy by classical technique or MIVAT (minimally invasive video-assisted thyroidectomy). Exclusion criteria were patients over age 65 (age can be a confounding factor). Patients with prior or simultaneous operations in the region of the head and neck, with the exception of any kind of simultaneous neck dissection (central compartment—level VI or lateral compartment, unilateral or bilateral). Patients with intra or postoperative complications characterized either by hemorrhage, infection, hematoma, seroma, or in need of tracheostomy. If there are any changes in the laryngeal mobility before surgery or in case of laryngeal lesion identified by direct laryngoscopy (without strobe light). Difficulty in understanding simple instructions and previously diagnosed neurological disorders.
For the nasofibroscopy swallowing four consistencies were offered: liquid, thickened liquid, pasty, and solid. The product, quantity, and the utensils used were: 5 ml of water (liquid consistence) offered in a coffee cup, 5 ml of grape juice (thickened liquid) offered in a teaspoon, 5 ml of grape juice (pasty) offered in a teaspoon, and half a biscuit (solid) offered in the hand of the patient, asking them to completely swallow. Foods were colored with aniline blue from the Mix Coralin® brand (manufactured in Taboão da Serra, São Paulo/SP-Brazil). Although not being the amount offered to patients, to achieve each consistencies, we have used the following recipes (ratios between thickened and liquid): to test the thickened liquid (as nectar) it was used one recipe of 100 ml of water and 4.5 g of thickener (Thick & Easy® brand, from Fresenius Kabi company manufactured in Runcorn, Cheshire—WA7 1NT—United Kingdom). To test the pasty consistence (as honey), it was used 100 ml of water and 6 g of the same thickener based on a report by Santoro et al. [23].
The evaluation of swallowing involved four items: early spill of food, penetration, aspiration, and retention. Regarding retention, evaluations were in the base of tongue, vallecula, and posterior wall of the pharynx and hypopharynx. The evaluations followed part of the protocol suggested by the Office of the University of Dysphagia Pittsburgh—UP specific about nasofibroscopic evaluation and excluded oroscopy and oral function mobility (2004) version updated by the service itself and originally based on the book [22]. An analysis followed each offer, either after the first or after the second spontaneous swallow.
The examination was conducted by the Endoscopy Sector of DHNS team through the fiberoptic endoscopic (brand Welch-Allym—manufactured in Runcorn Skaneateles Falls, NY 13153, USA) directly into the computer and recorded in digital version for later analysis by judges. Judges were part of the study and the identity of the patients were unknown to them, once the analyses were blind. The judges received separate and shuffled recordings of the tests, without any identifying information or patient characteristics. Analyses by the judges were independent and blinded.
To facilitate the entry of the nasal fiber, 2 jets of lidocaine (10 %) spray Cristalia Xylestesin were used in the nasal cavity on the side chosen for the introduction of the tool. Testing for laryngeal mobility consisted in asking the patient to say the vowel sound “A” and the vowel sound “I” in a high note, as well as by normal and forced inspiration and coughing. The classification of the laryngeal mobility was either present, restricted, or absent mobility [24]. There is no evidence that the amount of lidocaine used in our sample can affect the function of swallowing [25], hence that was the amount used to enhance patient comfort and make the assessment easier.
All patients underwent thyroidectomy based on the description of the classic surgical technique proposed by Zollinger and Zollinger [26]. At DHNS, identification of the recurrent laryngeal nerve (RLN) and the superior laryngeal nerve (SLN) were part of the routine, although the use of nerve intraoperative monitoring (NIM) was not routinely performed during the period of this sample capture. The surgical team carefully identifies the lower and upper laryngeal nerves and whenever possible tries to preserve them. Anastomosis is performed if the nerve is sacrificed.
Statistical Analysis
Initially, a univariate descriptive analysis of characteristics was conducted in which qualitative variables were ranked by frequency and by percentage and quantitative variables by median and percentiles. This was followed by a bivariate analysis that compared categorical variables using the Chi-square test or Fisher test as appropriate. Odds ratios (OR) were calculated with the respective 95 % confidence intervals (CI). Logistic regression analysis was conducted to explore the association between dependent variables (modified swallow 7 days/60 days) and factors such as gender, age, smokers, group ALM or NLM, MIVAT, thyroid disease, retention, resection, and volume as independent variables. Variables with P < 0.20 in bivariate analysis were selected to be included in multivariate analysis. These variables were then introduced into the regression model using a stepwise forward procedure. All statistical analyses were performed with the use of PASW Statistics 19.0 software, and P values <0.05 were considered statistically significant. Ethical approval for this study was obtained from the Ethics Committee of University of São Paulo—(USP), number 817/06.
Results
From 97 patients 54 were eligible to be part of this sample (Fig. 1), characteristics are summarized in Table 1. The incidence of dysphagia (regardless of time of assessment) was 87 % in patients with ALM (13/15) and 44 % in patients (NLM 17/39). In general, among the 54 patients in the study, 30 had change in swallowing (30/54, 55 %).
The ALM group was composed by 15 patients with unilateral change of laryngeal mobility. In the EPO (7 days), 10/15 patients (67 %) had absent laryngeal mobility and 5/15 (33 %) had reduced mobility. In the LPO (60 days), there was an improvement in the mobility of vocal fold in part of the ALM group: 7/15 patients (47 %) had laryngeal mobility present, 5/15 (33 %) mobility reduced, and 3/15 (20 %) mobility absent. Dysphagia occurred in 87 % of patients with ALM in the EPO. Despite the improvement of laryngeal mobility in 47 % of these patients, dysphagia remained in 67 % of them in the LPO.
All patients of the ALM group underwent the three evaluation stages (PRE, EPO, and LPO). In the NML group, all 39 patients underwent PRE and EPO, but 11/39 patients (28 %) did not show up for the LPO (Fig. 1).
Regarding the ALM Group, there were penetration and aspiration in 33 % (5/15) of the patients while retention in the oro/hypopharynx was the most frequent finding with 87 % (13/15) (Table 2) characterized by retention of food. Liquid consistency offered higher risks of penetration and aspiration in the EPO and thickened liquid and pasty consistencies presented higher retention incidence in the LPO. There was prevalence of retention in the valleculae and pyriform sinuses and though not expected, retention occurred with liquid consistency as well (Table 3).
In the NLM, dysphagia occurred in 44 % (17/39) in the EPO and 25 % (7/28) in the LPO. Food retention was observed in 44 % (17/39) in the EPO and 18 % (5/28) in the LPO. Incidence of early spill was 21 % (8/39) in the EPO, and remained 7 % (2/28) in the LPO (Table 2). Liquid consistency was associated with the highest risks of early spill in the EPO (15 %; 6/39). Pasty consistence left more retention in the oro/hypopharynx 31 % (12/39) in the EPO and 18 % (5/28) in the LPO.
There are differences between the occurrence of dysphagia between the two groups in the EPO (P = 0.004) and LPO (P = 0.008), the ALM group has a higher incidence of dysphagia at all times of the postoperative period (EPO and LPO). However, the NLM group also shows alteration in EPO and LPO. Dysphagia is most frequent in the EPO in both groups, but more severe in the ALM group. The occurrence of LPO retention is still present in both groups (Table 2).
Discussion
There is a direct relationship between alteration of swallowing and thyroid surgery, regardless of larynx mobility alteration. This study showed that 55 % of the subjects had some deglutition disorder after thyroidectomy. Despite being more frequent in the EPO, some changes persist in LPO. Our findings support some previous findings that demonstrated around 58 % of dysphagia incidence in this kind of patient [1, 7] (Tables 4, 5).
The current guideline used to follow-up patients with surgery indication to treat thyroid disease focuses on the postoperative investigation of voice [27]. Both in manual and in clinical routine, there is no concern to investigate swallowing complaints or even to evaluate this function. However, authors who use specific protocols for raising these complaints show how the airway symptoms related to swallowing difficulties are presented in the EPO and LPO [6, 18]. There is a relationship of these symptoms with the results of the nasofibroscopy performed in the present study.
Analyzing groups regardless of the postoperative period, dysphagia is more frequent in the ALM (87 %), but it was also impaired in patients with NLM (44 %). Evidence of functional changes after thyroidectomy, even with NLM, is a recent discussion in the literature and with an emphasis on postoperative dysphonia [10–17]. In the present study, the frequency of retention in the postoperative period of thyroid surgery, in both groups, is apparent (NLM and ALM). In the ALM group, even those who recovered laryngeal movement in the LPO (47 %) presented dysphagia. This finding may indicate the association between dysphagia with thyroid surgery and/or cervical manipulation. In this study, surface electromyography was not performed, but other authors who used this instrument observe changes in the extrinsic muscles after thyroidectomy [17]. However, they did not investigate these changes in the early 7-day postoperative period. There is a relationship between cervicotomy surgery (that means using the cervical access) and retention in swallowing food.
Manipulation of the extrinsic muscles results both in change of the pharyngeal muscle movements and the laryngeal elevation, thus causing retention [16]. Another study that addresses thyroidectomy without access to cervical (performed by robotic techniques through the armpit) reveals that functional impacts are smaller [28].
Although subjects submitted to MIVAT are expected to have lower risk of laryngeal mobility changes and lower functional sequelae [5], there was no statistical significance in our sample, probably due to the few cases in which they used this technique.
The investigation of esophageal motility provides important data on the relationship between change in pharyngoesophageal peristalsis and thyroid surgery, regardless of the vagus nerve injury. There is a change in esophageal motility after thyroidectomy [8]. In the analyzed group, during the postoperative period, the presence of retention in the valleculae, piriform sinuses and at the base of the tongue may relate to the modification of pharyngoesophageal motility. Occurrence of residues in the vallecular and pyriform sinuses after neck surgery, even with the preservation of evidence of recurrent or superior laryngeal nerve with the use of laryngeal electro myography (LEMG) [16].
Analysis of the presence of sensitivity is essential for investigating the function of swallowing [29]. The study did not assess the laryngeal sensitivity because the institution does not have the equipment (FEESST®) specific to this purpose. However, in cases where there was penetration and aspiration, there was response to a cough reflex protection, suggesting the presence of some sensitivity in such cases.
For the present study, there was no parallel analysis of a control group without thyroid disease to compare the influence of tracheal intubation in function. However, laryngeal changes cited in the study of Aluffi et al. [11] as edema of the vocal folds and asymmetric mucosal wave may suggest that they are sequelae of intubation. It is noteworthy that studies with control of mastectomy or cholecystectomy group noted that individuals with thyroid disease had more vocal changes in relation to others [4, 10, 30] suggesting that intubation would not be the causative reason for functional voice disorders, but there is more evident laryngeal changes in the recent postoperative period [10]. During the thyroidectomy, the neck is heavily manipulated in the presence of the tube in the larynx, which would lead to higher risk of possible functional impact in swallowing, however, few studies in the literature can study this risk factor isolated from other base pathologies.
In this study, we conclude that dysphagia occurs in patients after thyroid surgery and is characterized by stasis of food in the oro and hypopharynx, which is also noticed in LPO, though more frequently in EPO. Stasis, though undervalued for not causing severe dysphagia, is a frequent complaint in the recent and late period after thyroidectomy. It is more severe in individuals with ALM, with the possibility of laryngotracheal penetration and aspiration in the first weeks after surgery. A small sample is not conclusive regarding correlation between swallowing dysfunctions with supraglottic and pharyngeal factors, and relation with tracheal intubation, surgical manipulation of the extrinsic muscles and larynx nerve damage.
Complaints of swallowing after thyroidectomy, especially from the early postoperative period until 2–3 months later go undervalued in the routine clinical follow-up of patients with thyroid disease. This is a period of instability, because at adjusting the thyroid hormone, patients often become more complainants, and severe dysphagia with pulmonary risk is the usual concern of the medical staff. Nonetheless, complaints of difficulty in swallowing food or the feeling of stopped food should be valued.
References
Grover G, Sadler GP, Mihai R. Morbidity after thyroid surgery: patient perspective. Laryngoscope. 2013;123(9):2319–23. doi:10.1002/lary.23850.
Finck C. Laryngeal dysfunction after thyroid surgery : diagnosis, evaluation and treatment. Acta Chir Belg. 2006;106:378–87.
Bicknell PG. Mild hypothyroidism and its effects on the larynx. J Laryngol Otol. 1973;87:123–7.
Pereira JA, Girvent M, Sancho JJ, Parada C, Sitges-Serra A. Prevalence of long-term upper aerodigestive symptoms after uncomplicated bilateral thyroidectomy. Surgery. 2003;133:318–22.
Lombardi CP, Raffaelli M, D’alatri L, De Crea C, Marchese MR, Maccora D, Paludetti G, Bellantone R. Video-assisted thyroidectomy significantly reduces the risk of early postthyroidectomy voice and swallowing symptoms. World J Surg. 2008;32(5):693–700. doi:10.1007/s00268-007-9443-2.
Silva IC, de Netto I, Vartanian JG, Kowalski LP, Carrara-de Angelis E. Prevalence of upper aerodigestive symptoms in patients who underwent thyroidectomy with and without the use of intraoperative laryngeal nerve monitoring. Thyroid. 2012;22(8):814–9. doi:10.1089/thy.2011.0118.
Senise AT, Queija DS, Degani C, Corrêa LAC, Dedivitis RA, Lehn CN, Xavier C, Barros APB. Symptoms and signs of swallowing changes after thyroidectomy. Rev Bras Cir Cabeça Pescoço. 2009;38(2):67–71.
Scerrino G, Inviati A, Di GS, Paladino NC, Di Paola PV, Lo Re G, Almasio PL, Cupido F, Gulotta G, Bonventre S. Esophageal motility changes after thyroidectomy; possible associations with postoperative voice and swallowing disorders: preliminary results. Otolaryngol Head Neck Surg. 2013;148(6):926–32.
Rosato L, Avenia N, Bernante P, De Palma M, Gulino G, Nasi PG, et al. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg. 2004;28(3):271–6.
de Pedro NI, Fae A, Vartanian JG, Barros AP, Correia LM, Toledo RN, et al. Voice and vocal self-assessment after thyroidectomy. Head Neck. 2006;28(12):1106–14.
Aluffi P, Policarpo M, Cherovac C, Olina M, Dosdegani R, Pia F. Post-thyroidectomy superior laryngeal nerve injury. Eur Arch Otorhinolaryngol. 2001;258(9):451–4.
Stojadinovic A, Shaha AR, Orlikoff RF, Nissan A, Kornak MF, Singh B, et al. Prospectivefunctionalvoiceassessment in patientsundergoingthyroidsurgery. Ann Surg. 2002;236(6):823–32.
Lombardi CP, Raffaelli M, D’Alatri L, Marchese MR, Rigante M, Paludetti G, et al. Voice and swallowing changes after thyroidectomy in patients without inferior laryngeal nerve injuries. Surgery. 2006;140(6):1026–32 discussion 1032-4.
GonçalvesFilho J, Kowalski LP. Surgical complications after thyroid surgery performed in a cancer hospital. Otolaryngol Head Neck Surg. 2005;132(3):490–4.
Lee J, Kwon IS, Bae EH, Chung WY. Comparative analysis of oncological outcomes and quality of life after robotic versus conventional open thyroidectomy with modified radical neck dissection in patients with papillary thyroid carcinoma and lateral neck node metastases. J Clin Endocrinol Metab. 2013;98(7):2701–8. doi:10.1210/jc.2013-1583.
Ryu JS, Lee JH, Kang JY, Kim MY, Shin DE, Shin DA. Evaluation of dysphagia after cervical surgery using laryngeal electromyography. Dysphagia. 2012;27(3):318–24. doi:10.1007/s00455-011-9368-7.
Lombardi CP, D’Alatri L, Marchese MR, Maccora D, Monaco ML, De Crea C, Raffaelli M. Prospective electromyographic evaluation of functional postthyroidectomy voice and swallowing symptoms. World J Surg. 2012;36(6):1354–60. doi:10.1007/s00268-012-1481-8.
Leder SB, Sasaki CT, Burrell MI. Fiberoptic endoscopic evaluation of dysphagia to identify silent aspiration. Dysphagia. 1998;13:19–21.
Lombardi CP, Raffaelli M, De Crea C, D’Alatri L, Maccora D, Marchese MR, Paludetti G, Bellantone R. Long-term outcome of functional post-thyroidectomy voice and swallowing symptoms. Surgery. 2009;146(6):1174–81. doi:10.1016/j.surg.2009.09.010.
Jung SP, Kim SH, Bae SY, Lee SK, Kim S, Choi MY, Kim J, Kim M, Kil WH, Choe JH, Kim JH, Nam SJ, Kim JS. A new subfascial approach in open thyroidectomy: efficacy for postoperative voice, sensory, and swallowing symptoms. a randomized controlled study. Ann Surg Oncol. 2013;20(12):3869–76.
Lee J, Chung WY. Robotic thyroidectomy and neck dissection: past, present, and future. Cancer J. 2013;19(2):151–61. doi:10.1097/PPO.0b013e31828aab61.
Murry T, Carrau RL. Functional tests of swallowing. In: Carrau RL, Murry T, editors. Comprehensive management of swallowing disorders. 2nd ed. San Diego: Singular Publishing Group; 1999. p. 75–9.
Santoro PP, Tsuji DH, Lorenzi MC, Ricci F. The role of videoendoscopic swallowing study in the quantitative evaluation of the oral and pharyngeal phases of deglutition in the elderly. Int Arch Otorhinolaryngol. 2003;7:181–7.
Yin S, Qiu WW, Stucker FJ, Batchelor BM. Critical evaluation of neurolaryngological disorders. Ann Otol Rhinol Laryngol. 2000;109:832–8.
Kamarunas EE, McCullough GH, Mennemeier M, Schluterman K. Effects of topical nasal anesthetic on fiberoptic endoscopic examination of swallowing with sensory testing (FEESST). Dysphagia. 2014;29:33–43.
Zollinger RM Jr, Zollinger RM. Atlas de Cirurgia. Rio de Janeiro: Guanabara-Koogan; 2003.
Chandrasekhar SS, Randolph GW, Seidman MD, Rosenfeld RM, Angelos P, Barkmeier-Kraemer J, Benninger MS, Blumin JH, Dennis G, Hanks J, Haymart MR, Kloos RT, Seals B, Schreibstein JM, Thomas MA, Waddington C, Warren B, Robertson PJ. Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol Head Neck. 2013;148(6 Suppl):S1–37. doi:10.1177/0194599813487301.
Tae K, Kim KY, Yun BR, Ji YB, Park CW, Kim DS, Kim TW. Functional voice and swallowing outcomes after robotic thyroidectomy by a gasless unilateral axillo-breast approach: comparison with open thyroidectomy. Surg Endosc. 2012;26(7):1871–7. doi:10.1007/s00464-011-2116-0.
Wasserman JM, Sundaram K, Alfonso AE, Rosenfeld RM, Har-El G. Determination of the function of the internal branch of the superior laryngeal nerve after thyroidectomy. Head Neck. 2008;30(1):21–7.
Kark AE, Kissin MW, Auerbach R, Meikle M. Voice changes after thyroidectomy: role of the external laryngeal nerve. Br J Med. 1984;289:1412–5.
Shah J, Shah A, Pietrobon R. Scientific writing of novice researchers: what difficulties and encouragements do they encounter? Acad Med. 2009;84:511–6.
Pietrobon R, Guller U, Martins H, et al. A suite of web applications to streamline the interdisciplinary collaboration in secondary data analyses. BMC Med Res Methodol. 2004;4:29.
Acknowledgments
Endoscopy Section and TecHealth Brasil for the scientific assistance (Dirce Maria Capobianco and Taís Moreira). Alexandro Duarte for the writing review. “Research on Research” for templates on scientific writing [31] and literature review [32].
Conflict of interest
None of the authors have any conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arakawa-Sugueno, L., Ferraz, A.R., Morandi, J. et al. Videoendoscopic Evaluation of Swallowing After Thyroidectomy: 7 and 60 Days. Dysphagia 30, 496–505 (2015). https://doi.org/10.1007/s00455-015-9628-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-015-9628-z