Abstract
Osteoarthritis is a degenerative joint disease caused by excessive death of chondrocytes and loss of the extracellular matrix (ECM) in articular cartilage. We previously reported that reactive oxygen species (ROS) generated by the NADPH oxidase (NOX) isoform NOX-2 are involved in chondrocyte death induced by interleukin-1β (IL-1β). In this study, we investigate the role of NOX-2 in the production and degradation of ECM by chondrocytes. Although IL-1β lowered the mRNA expression of type II collagen (Col2a1) and aggrecan (Acan) in mouse chondrocyte-like ATDC5 cells, RNA silencing of Nox2 did not change the mRNA expression of these major components of the ECM of cartilage. Hence, NOX-2 is not involved in the IL-1β-induced suppression of ECM production. On the other hand, the NOX inhibitor 4-(2-aminoethyl)benzenesulfonyl fluoride (AEBSF), the ROS scavenger N-acetylcysteine and an antisense oligodeoxynucleotide for Nox2 prevented the loss of proteoglycan induced by IL-1β in highly differentiated ATDC5 cells. Furthermore, AEBSF did not affect the expression of hyaluronidase-1 and −2, whereas it suppressed hyaluronidase activity in culture medium. IL-1β-induced intra- and extracellular acidification was also suppressed by AEBSF, as was the antisense oligodeoxynucleotide for Nox2. Since hyaluronidase activity is known to be higher under acidic conditions, NOX-2 probably contributes to ECM loss by the activation of hyaluronidase through acidification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Even though cartilage is an avascular tissue, the functions of the chondrocytes contained therein are influenced by molecular oxygen and its reactive metabolites. Notably, so-called reactive oxygen species (ROS) are reported to play important roles in the regulation of chondrocyte metabolism including matrix degradation in joint diseases, such as rheumatoid arthritis and osteoarthritis (Henrotin et al. 2005; Goldring and Marcu 2009; Zamli and Sharif 2011; Kaku and Yamauchi 2014). The major ROS produced by chondrocytes are superoxide (O2 −), hydrogen peroxide (H2O2), nitric oxide (NO) and peroxynitrite, a reaction product of O2 − and NO (Reiter et al. 2000; Del Carlo and Loeser 2002). Among these ROS, a large amount of NO is known to be produced by the inducible type of NO synthase in response to inflammatory stimuli, whereas the O2 −- and H2O2-generating systems in chondrocytes have not been fully elucidated.
NADPH oxidase (NOX) is a specialized biological system that generates ROS, more specifically, O2 − and H2O2. Among the seven members of the NOX family, NOX-2 is the most-well-characterized and has been shown to be mainly distributed in phagocytes (Sheppard et al. 2005). In addition, attention has recently been given to NOX in non-immune cells, including those in the cardiovascular and central nervous systems (Lambeth 2004). We have previously reported that interleukin-1β (IL-1β) induces the expression of NOX-2 in ATDC5 cells, a mouse chondrocyte-like cell line and in primary mouse and rat chondrocytes and is required for IL-1β-induced death of those cells (Yasuhara et al. 2005; Yoshimura et al. 2011). These previous observations indicate the possible participation of NOX-2 in the induction of chondrocyte death, which might be one of the characteristic changes found in the articular cartilage of osteoarthritic joints (Grogan and D’Lima 2010; Zamli and Sharif 2011).
Loss of the extracellular matrix (ECM) in articular cartilage is another change seen in joints affected by osteoarthritis (Zamli and Sharif 2011; Goldring and Marcu 2009; Kaku and Yamauchi 2014). However, to the best of our knowledge, the role of NOX in this loss has not been fully elucidated. In this study, we have investigate the roles of NOX in the production and degradation of ECM of ATDC5 cells stimulated by IL-1β and find that it has functions in the degradation of hyaluronan and loss of proteoglycan.
Materials and methods
Cell culture
ATDC5 cells (Atsumi et al. 1990) were obtained from Riken BioResource Center (Tsukuba, Japan) and maintained at 37 °C with 5 % CO2 in DMEM/F12 medium (Sigma-Aldrich, St. Louis, Mo., USA) containing antibiotics and 2.5 % fetal bovine serum (FBS; Thermo Fisher Scientific, Waltham, Mass., USA). ATDC5 cells at the differentiation stage with expression of type II collagen (Col2a1) and aggrecan (Acan) mRNAs were used for experiments to investigate the effects of IL-1β (R&D systems, Minneapolis, Minn., USA) on the expression of these genes. ATDC5 cells were pre-cultured for 3 weeks in appropriate culture plates in the above-described medium supplemented with insulin-transferrin-selenium (ITS; 10 μg/ml insulin, 5.5 μg/ml transferrin, 6.7 ng/ml sodium selenite), with the medium being changed every other day and were then used in experiments to evaluate IL-1β-induced degradation of matrix components. Culturing for 3 weeks in the presence of ITS allowed the cells to produce proteoglycans that were visualized in ECM by Alcian blue staining (Shukunami et al. 1996).
Nox2 silencing and NOX inhibition
To investigate the roles of NOX-2 in the expression of mRNAs for Col2a1 and Acan in ATDC5 cells cultured in the presence of IL-1β, 30 pmol mouse Nox2 short interfering RNA (siRNA) or its control siRNA (Stealth RNAi; Thermo Fisher Scientific) was introduced by using LipofectamineTN RNAiMAX (Thermo Fisher Scientific; Yoshimura et al. 2011) into 40-50 % confluent cells grown in 6-well plates, which were then treated with mouse recombinant IL-1β in complete medium containing 2.5 % FBS.
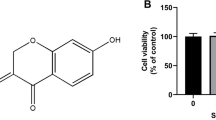
For experiments to assess ECM degradation, we used ATDC5 cells pre-cultured in 96-well plates for 3 weeks in the presence of ITS with the medium being changed every other day. Using these experiments, we assessed the amounts of proteoglycan and hyaluronan accumulated during the 3-week pre-culture period and the degradation of extracellular components within 48 h after addition of IL-1β. An NOX inhibitor, 4-(2-aminoethyl)benzenesulfonyl fluoride hydrochloride (AEBSF; Diatchuk et al. 1997; Calbiochem-Novabiochem, La Jolla, Calif., USA) and an ROS scavenger, N-acetylcysteine (NAC; Sigma-Aldrich), were used to examine the role of NOX in IL-1β-induced ECM degradation. Although the efficiency of introducing Nox2 siRNA into these highly differentiated ATDC5 cells was low, an antisense oligodeoxynucleotide (ODN) for Nox2, with the sequence 5’-AACTGGGCTGTGAATGAGG-3’ (letters in italics denote phosphorothioate-bonded bases) targeting base pairs 7 to 25 downstream of the translation initiation start in the coding sequence of Nox2 mRNA (NM_000397; Wagner et al. 2001), was effective in suppressing Nox2 expression. Nox2 antisense ODN and a scrambled control ODN, with the sequence 5’-CATTGTGGAGTGACAGGAG-3’, were used to confirm the participation of NOX-2 in ECM degradation. The ATDC5 cells used in this experiment were pre-cultured for 3 weeks in 10-cm dishes in ITS-supplemented medium. The cells were detached by digestion with 0.1 % collagenase and 0.2 % dispase (both from Wako Pure Chemicals, Osaka, Japan) in medium containing 2.5 % FBS for 1 h at 37 °C, then washed with phosphate-buffered saline (PBS) and re-suspended in complete medium. A trypan blue dye exclusion method showed that more than 95 % of the cells were viable. These ODNs (2 μmol/l) were then introduced into cells by using Endo-Porter (Gene Tools, LLC, Philomath, Ore., USA). Suppression of NOX-2 expression was evaluated by Western blot analysis with an antibody for mouse NOX-2 (Santa Cruz Biotechnology, Santa Cruz, Calif., USA).
Polymerase chain reaction
Total RNA was extracted from cells by using TRIzol solution (Thermo Fisher Scientific). Reverse transcription (RT) reactions were performed with Superscript III (Thermo Fisher Scientific) and a random hexamer. The primer sequences employed for the polymerase chain reaction (PCR) were as follows: Col2a1, 5’-GCC AAG ACC TGA AAC TCT GC-3’ and 5’-CTT GCC CCA CTT ACC AGT GT-3’; Acan, 5’-CAG GTT TCC CCA CTG TGT CT-3’ and 5’-ACT CCA GAC CCT GGG AAG TT-3’; Nox2, 5’-GAG GGT TTC CAG CCA GCG AAC TTT GGT-3’ and 5’-TGA AGG GGG CCT GTA TGT GG-3’; ActB (β-actin), 5’-TGT TAC CAA CTG GGA CGA GA-3’ and 5’-AAG GAA GGC TGG AAA AGA GC-3’; Cd44, 5’-CGA TTG GAG ACG TCA TTC CT-3’ and 5’-GCT GGA AAG CAA TGC CTA AG-3’; Gapdh (D-glyceraldehyde-3-phosphate dehydrogenase), 5’-ACC ACA GTC CAC GCC ATC AC-3’ and 5’-TCC ACC ACC CTG TTG CTG TA-3’. The PCR products were separated on 1 % agarose gels and stained with ethidium bromide.
Quantitative real-time RT-PCR was performed by using TaqMan Gene Expression Assays (Thermo Fisher Scientific) with a StepOne Real-time PCR System (Thermo Fisher Scientific). The assay numbers of Col2a1, Acan, hyaluronidase 1 (Hyal1), hyaluronidase 2 (Hyal2) and Gapdh were Mm01309563_g1, Mm00545807_m1, Mm00476206_m1, Mm01230688_g1 and Mm03302249_g1, respectively.
Staining and quantitative evaluation of proteoglycan
After being washed with PBS, cells were fixed in 2 % paraformaldehyde in 0.1 mol/l sodium phosphate buffer (pH 7.4). The fixed cells were treated for 5 min with 3 % acetic acid, incubated for 30 min with 1 % Alcian blue dye in 3 % acetic acid and rinsed in tap water. Alcian blue bound to the ECM was solubilized in 6 mol/l guanidine hydrochloride. Solubilized Alcian blue in the lysates was quantified by reading the absorbance at 595 nm.
Hyaluronan staining
Hyaluronan was visualized by using a previously reported method (Tengblad 1979; Asari et al. 1992a, 1992b). Briefly, after fixation in PBS containing 2 % glutaraldehyde and 2 % paraformaldehyde, followed by treatment with 0.05 % trypsin and 0.1 % Triton X-100, cells were incubated overnight at 4 °C with 2 μg/ml biotinylated hyaluronic-acid-binding protein (Seikagaku, Tokyo, Japan) in PBS containing 0.1 % bovine serum albumin (BSA). After being washed with PBS, cells were incubated for 2 h at room temperature with 10 μg/ml Texas-Red-conjugated streptavidin in PBS containing 0.1 % BSA and then further stained with 4’,6-diamidino-2-phenylindole (DAPI). Observation and quantification of fluorescence intensity were performed by using an In Cell Analyzer 1000 (GE Healthcare, Buckinghamshire, UK). For some experiments, cells were cultured in the absence of IL-1β and treated with 100 μg/ml hyaluronidase from Streptomyces hyaluronlyticus (Seikagaku) at pH 6.0.
Hyaluronidase activity assay
A microtiter-plate-based assay of hyaluronidase activity was performed as previously described (Flannery et al. 1998). Briefly, biotinylated hyaluronan (bHA) covalently bound to Covalink-NH microtiter plates (Nunc, Kamstrupvej, Denmark) was incubated for 30 min at 37 °C with culture supernatants or standard hyaluronidase solutions and then residual bHA was quantified in a colorimetrical manner by using avidin-linked alkaline phosphatase and its substrate p-nitrophenylphosphate. In some experiments, hyaluronidase activity in the culture supernatants was determined without pH adjustment, whereas in others, the culture supernatants were diluted in formate buffer (pH 4.5) before the determination of hyaluronidase activity.
Intracellular and extracellular pH determination
The pH levels of culture medium samples were determined as extracellular pH by use of a pH electrode (Horiba, Kyoto, Japan) with a method previously described (Rink et al. 1982). Briefly, cells were detached by collagenase digestion as described above, then washed with PBS, re-suspended in HEPES-buffered saline (pH 7.4) containing 5 mmol/l glucose (HBSG) and incubated for 30 min with 3’-O-acetyl-2’,7’-bis(carboxyethyl)-4 or 5-carbocyfluoresceine (BCECF) diacetoxymethyl ester (BCECF-AM; Dojindo Laboratories, Kumamoto, Japan; 10 μmol/l). The fluorescence intensity of BCECF in the cells was measured by using a fluorescence spectrophotometer (F-400; Hitachi, Tokyo, Japan) with excitation at 455 and 505 nm and emission at 530 nm. Calibration of pH was performed by using cells permeabilized with 10 μmol/l nigericin (Merck, Darmstadt, Germany) in isotonic buffer at various pH levels. For the assessment of endocytosis based on the measurement of endosomal pH, we used pHrodo Green Dextran (Thermo Fisher Scientific) according to the manufacturer’s instructions.
Statistical analysis
Data are expressed as the means ± SD. Student’s t test was used for comparisons of results from two groups and Tukey’s test was used for pairwise comparisons of results from three or more groups, with P <0.05 being considered to indicate significance.
Results
NOX-2-independent decrease in expression of mRNAs for type II collagen and aggrecan induced by IL-1β
Both the reduced synthesis and the increased degradation of ECM components cause the loss of cartilage ECM. In the present study, we initially examined the effects of Nox2 siRNA on expression of the mRNAs for Col2a1 and Acan, the two main components of cartilage ECM, in IL-1β-treated ATDC5 cells. IL-1β lowered the expression of both genes in a concentration-dependent manner (Fig. 1a). On the other hand, Nox2 siRNA did not restore the reduced expression of Co2a1 or Acan (Fig. 1b). Hence, NOX-2 might not play an important role in the suppressed expression of these genes induced by IL-1β.
NADPH oxidase-2 (NOX2)-independent suppression of type II collagen (Col2a1) and aggrecan (Acan) expression induced by interleukin-1β (IL-1β). a ATDC5 cells received Nox2 short interfering RNA (siRNA) or control siRNA and were treated for 48 h with various concentrations of IL-1β. Expression of mRNAs for Col2a1, Acan, Nox2 and ActB (β-actin gene) was examined by reverse transcription plus polymerase chain reaction (RT-PCR). b ATDC5 cells received Nox2 siRNA or control siRNA and then were treated for 48 h with IL-1β (10 ng/ml). Expression of mRNAs for Col2a1 and Acan was examined by real-time RT-PCR (n = 6). Amplification signals from these genes were normalized against that of Gapdh (D-glyceraldehyde-3-phosphate dehydrogenase). *P < 0.05
NOX-dependent reductions in proteoglycan and hyaluronan after IL-1β treatment
The amount of proteoglycan was evaluated by examining Alcian blue bound to the ECM of ATDC5 cells pre-cultured for 3 weeks in the presence of ITS. The level of proteoglycan was lowered after treatment with IL-1β for 2 days, whereas AEBSF and NAC suppressed the IL-1β-dependent reduction in extracellular proteoglycan shown by Alcian blue binding (Fig. 2a), indicating that NOX and ROS were involved in loss of proteoglycan induced by IL-1β. To assess the release of aggrecan from the ECM, we measured aggrecan in samples of culture medium. Although the difference was not significant, aggrecan in culture medium tended to increase in the presence of IL-1β (Supplementary Fig.S1A).
Effects of 4-(2-aminoethyl)benzenesulfonyl fluoride (AEBSF) and N-acetylcysteine (NAC) on IL-1β-induced decrease in aggrecan and hyaluronic acid. Differentiated ATDC5 cells were incubated for 48 h with IL-1β (10 ng/ml) in the presence or absence of AEBSF (0.3 mmol/l) and/or NAC (5 mmol/l). a Extracellular proteoglycan amounts were evaluated by determining the binding of Alcian blue to cells in cultures (n = 4). Filled and unfilled columns indicate results obtained from cells cultured without and with IL-1β, respectively. *Significantly different (P <0.05) from control group (leftmost filled column). †Significantly different (P <0.05) from IL-1β group (unfilled column second from left). b Texas Red was used to stain hyaluronic-acid-binding protein (HA, red, top row) and DAPI was used for nuclear staining (bottom row). c Fluorescence intensity of HA was then quantified (n = 3). Image far right in b shows culture treated with hyaluronidase from Streptomyces hyaluronlyticus (Hyal). *Significantly different (P <0.05) from control group (leftmost filled column). †Significantly different (P <0.05) from IL-1β group (unfilled column second from left). ‡Significantly different (P <0.05) from AEBSF group (filled column third from left)
Hyaluronan, which maintains the localization of aggrecan in cartilage ECM, is anchored to chondrocytes via CD44, a hyaluronan receptor, resulting in a large number of aggrecan molecules bound to hyaluronan (Knudson and Knudson 2001; Wilusz et al. 2014). Hence, we examined the effects of the combination of IL-1β with AEBSF and NAC on the amount of hyaluronan in ATDC5 cultures. Cultures growing in the presence of IL-1β showed lower levels of staining of fluorescence-labeled hyaluronan-binding protein as compared with cultures without the cytokine (Fig. 2b). In the presence of AEBSF or NAC, no significant difference was seen between the levels of fluorescence based on the amount of hyaluronan in cultures with and without IL-1β (Fig. 2c). The mechanism by which AEBSF and NAC reduces the amount of hyaluronic acid remains to be clarified.
Increased hyaluronidase activity in culture medium after IL-1β treatment
To elucidate the mechanism of the IL-1β-dependent decrease in hyaluronan and its suppression by AEBSF, we examined the effects of IL-1β and AEBSF on the mRNA expression of the hyaluronan receptor CD44 in ATDC5 cells (Fig. 3a). ATDC5 cells constitutively expressed Cd44, irrespective of being treated with either IL-1β or AEBSF. Next, we determined the expression levels of mRNAs for hyaluronidase 1 and 2 (major mammalian hyaluronidases; Harada and Takahashi 2007) in ATDC5 cells (Fig. 3b). A slight increase in Hyal1 mRNA expression was observed in cells treated with IL-1β, whereas AEBSF had no effect on the expression of the Hyal1 gene and the expression of Hyal2 mRNA was not affected by either IL-1β or AEBSF (Fig. 3c).
Suppression of IL-1β-induced increase in hyaluronidase activity by NOX inhibitor. a Expression of mRNAs for CD44, hyaluronan receptor (Cd44) and GAPDH (Gapdh) in differentiated ATDC5 cells cultured for 48 h in the presence and absence of IL-1β (10 ng/ml) and/or AEBSF (0.3 mmol/l) as assessed by RT-PCR. b, c Expression of mRNAs for Hyal1 (b) and Hyal2 (c) as assessed by real-time RT-PCR and normalized to that of Gapdh (n = 3). d Hyaluronidase (Hydase) activity in culture supernatants of differentiated ATDC5 cells determined without pH adjustment after incubation for the indicated periods in the absence (filled triangles) or presence (filled squares) of IL-1β (10 ng/ml) or of IL-1β and AEBSF (0.3 mmol/l; filled circles). e Hydase activity in culture supernatants of differentiated ATDC5 cells determined at pH 4.5 after incubation for 48 h in the presence (+) and absence (−) of IL-1β (10 ng/ml) and/or AEBSF (0.3 mmol/l). *P <0.05 (NS not significant)
Next, hyaluronidase activity in the culture medium of differentiated ATDC5 cells was determined after incubation in the absence and presence of IL-1β (10 ng/ml) or of IL-1β and AEBSF (0.3 mmol/l) without adjustment of pH (Fig. 3d). Total hyaluronidase activity in culture medium was shown to increase from 24 to 48 h after addition of IL-1β but was suppressed by co-incubation with AEBSF. On the other hand, the optimal pH of hyaluronidase is known to be in the acidic range, namely, pH 3.5-6.0 (Lv et al. 2015). AEBSF did not have an effect on hyaluronidase activity in culture medium when enzyme activity was assessed at pH 4.5 (Fig. 3e).
Lowering of intracellular and extracellular pH by IL-1β
Intra- and extracellular acidification was observed in differentiated ATDC5 cell cultures after treatment for 48 h with IL-1β. AEBSF suppressed the acidification caused by IL-1β in both intra- and extracellular spaces (Fig. 4a, a’, b, b’). Secreted hyaluronidase-1 is reported to be incorporated by cells via endocytosis and degrades some hyaluronic acid intracellularly (Harada and Takahashi 2007); thus, we also assessed endocytosis in ATDC5 cells after treatment with IL-1β and AEBSF by detecting any fluorescence from a pH-sensitive fluorescence probe, pHrodo-dextran, in the acidic milieu (Flores et al. 2014). Observation with fluorescence microscopy (Fig. 4c, c’, c’’, c’’’) and measurement of fluorescence intensity (Fig. 4d) indicated that IL-1β promoted endocytosis in ATDC5 cells. In contrast, in the presence of AEBSF, no increase in fluorescence was observed in cultures with IL-1β (Fig. 4d). These results suggested that NOX-dependent acidification of the culture medium contributed to the apparent increase in hyaluronidase activity. Whereas BCECF-AM is used as an indicator of cytosolic pH, the dye has been reported to be distributed in endosomes (Slayman et al. 1994). Hence, a possibility exists that increased endocytosis contributes to the intracellular acidification detected in cells receiving BCECF-AM (Fig. 4b).
Suppression of IL-1β-induced acidification by NOX inhibitor. a, a’ Differentiated ATDC5 cells were cultured for the indicated periods in the presence (filled squares) and absence (filled circles) of IL-1β (10 ng/ml) and then the intracellular (a) and extracellular (a’) pH levels were determined. b, b’ Differentiated ATDC5 cells were cultured for 48 h in the presence (+) and absence (−) of IL-1β (10 ng/ml) and/or AEBSF (0.3 mmol/l) and then intracellular (b) and extracellular (b’) pH levels were determined (n = 3). c–c’’’ Endocytic activity of ATDC5 cells incubated for 48 h with (c, c’) or without (c’’, c’’’) IL-1β (10 ng/ml) in the absence (c, c’’) or presence (c’, c’’’) of AEBSF (0.3 mmol/l) detected as fluorescence from pHrodo-dextran in an acidic environment. Bars 100 μm. d Endocytic activity in the cells was assessed by measuring fluorescence intensity (n = 3). e Differentiated ATDC5 cells were cultured in medium with pH adjusted to 7.6 (filled columns) or 6.8 (unfilled columns) for 48 h in the presence (+) or absence (−) of IL-1β (10 ng/ml) and then extracellular proteoglycan was evaluated by Alcian blue binding (n = 3). *P <0.05
To elucidate the biological significance of IL-1β-dependent acidification, Alcian blue staining of proteoglycan was performed on ATDC5 cells cultured in medium with the pH adjusted to 6.8 (Fig. 4e). IL-1β reduced the amount of cell-associated Alcian blue to half of that bound to control cells when cultured in medium with a normal pH level (pH 7.6; Supplementary Fig. S1A, B). On the other hand, when the cells were cultured in the absence of IL-1β in medium with the pH adjusted to 6.8, Alcian blue binding was diminished to half of that observed in cells cultured without IL-1β in normal medium (Fig. 4e). Although IL-1β treatment reduced the amount of proteoglycan, even at pH 6.8, the reduction was less than that observed in cells cultured in normal medium (pH 7.6). On the other hand, acidification of the culture medium to pH 6.8 did not have a significant effect on the mRNA expression of Acan, Col2a1, Hyal1 and Hyal2 in ATDC5 cells (Supplementary Fig. S2), indicating that the reduced binding of Alcian blue to the ECM of cells cultured at pH 6.8 (Fig. 4e) was attributable to an increase in hyaluronidase activity under acidic conditions.
Inhibition of Nox2 expression suppressed acidification and loss of proteoglycan
To confirm the suppressive effects of AEBSF and NAC on acidification and proteoglycan loss induced by IL-1β in differentiated ATDC5 cells, a phosphorothioate bond-containing antisense ODN for Nox2 was introduced into these cells (Fig. 5a). Intra- and extracellular acidification and an increased hyaluronidase activity and a decrease in Alcian blue binding to ECM induced by IL-1β were suppressed by the Nox2 antisense ODN (Fig. 5b-d). Although a significant difference was not observed, Nox2 antisense ODN tended to lower the amount of aggrecan in the culture supernatants after incubation with IL-1β (Supplementary Fig. S1B). These results indicate that NOX-2 plays an important role in IL-1β-induced acidification and degradation of ECM.
Contribution of NOX-2 to intra- and extracellular acidification and the proteoglycan loss induced by 48-h treatment with IL-1β. Differentiated ATDC5 cells were transfected with antisense oligodeoxynucleotide for Nox2 and its scrambled control ODN (SRC). a NOX-2 and β-actin were detected by Western blotting. Expression levels of NOX-2 after normalization to that of β-actin are indicated under the photographs as the relative value to that obtained with SRC-treated cells. b Intra- and extracellular pH values were determined after 48 h of treatment with 10 ng/ml IL-1β (n = 3). c Hyaluronidase (Hydase) activity in culture medium was determined (n = 5). d Amount of Alcian blue bound to the ECM was determined by using a spectrophotometric technique (n = 4). *P < 0.05.
Discussion
Characteristic changes observed in articular cartilage obtained from osteoarthritic joints include the loss of the ECM and chondrocyte death. Previous reports have shown that inflammatory cytokines, such as tumor necrosis factor-α and IL-1β, participate in the induction of these degenerative changes in osteoarthritic joints (Yasuhara et al. 2005; Goldring and Marcu 2009; Grogan and D’Lima 2010; Yoshimura et al. 2011; Zamli and Sharif 2011; Chen et al. 2015). In addition, our previous studies revealed that IL-1β induces the expression of NOX-2, a phagocyte-type NOX, in chondrocytes (Yasuhara et al. 2005; Yoshimura et al. 2011). NOX is a membrane-bound enzyme that produces O2 − and H2O2. We have also reported that peroxynitrite formed by the reaction of NO and O2 − induces mitochondrial dysfunction and cell death in ATDC5 cells and in primary rat chondrocytes treated with IL-1β (Yasuhara et al. 2005). On the other hand, the roles of NOX in the loss of cartilage ECM have not been fully elucidated.
Cartilage ECM is maintained by a balance between the production and degradation of matrix components including type II collagen and aggrecan. Under the present experimental conditions, Nox2 siRNA slightly but significantly suppresses the expression of Col2a1 mRNA without any effect on that of Acan mRNA (Fig. 1). ROS produced by NOX-2 and NOX-4 have previously been reported to be required for chondrogenesis in the early stage (Kim et al. 2010). Hence, ROS derived from NOX-2 can be said to play a role in promoting ECM production, whereas NOX-2 does not seem to cause reduced production of ECM.
On the other hand, our results show that the intra- and extracellular spaces are acidified in an NOX activity-dependent manner; this increases hyaluronidase activity in cultures of ATDC5 cells. Since hyaluronan in cartilage ECM is known to hold aggrecan, the most abundant proteoglycan secreted by chondrocytes (Knudson and Knudson 2001; Wilusz et al. 2014), its degradation might result in the release of aggrecan from the ECM. In addition, increased endocytic activity has been observed in ATDC5 cells after IL-1β treatment (Fig. 4c, c’’, d). Hence, the degradation of hyaluronic acid and proteoglycans in endosomes might have also contributed to their decrease in the cultures.
As is well known, the pH level of the synovial fluid in osteoarthritis patients is lower than that in healthy individuals (Nagaya et al. 1999), indicating the possibility that ROS produced by NOX in chondrocytes contribute to this acidification. The intracellular pH of chondrocytes has also been reported to be regulated by the Na+/H+-exchanger and vacuolar H+-ATPase (Browning and Wilkins 2004), carbonic anhydrases (Yocum et al. 1995) and monocarboxylate transporters (Meredith et al. 2002). More recently, experiments with chondrocytes have demonstrated that mitochondrial ROS increase acid efflux to lower the level of extracellular pH (Milner et al. 2007). In the present experimental setting, intra- and extracellular pH change in reversed directions at 12 h after IL-1β treatment, i.e., alkalinization of the intracellular space and acidification of culture medium occur (Fig. 4a, a’). Acid efflux from cells into the culture medium or other mechanisms might have induced these changes. However, they are likely to be independent of NOX-2 activity, since no expression of NOX-2 was observed at 12 h, whereas it was observed at 36 h after addition of IL-1β in our previous study (Yoshimura et al. 2011). On the other hand, in that same study, we found that excess lactic acid (2 mmol/l) had accumulated in the culture medium of ATDC5 cells treated for 24 h with IL-1β as compared with those without IL-1β; this might lead to extracellular acidification prior to the expression of NOX-2.
In the present study, we found that both intra- and extracellular spaces became acidified from 24 to 48 h after IL-1β treatment (Fig. 4a, a’). The suppression of acidification by AEBSF and antisense ODN for Nox2 (Figs. 4, 5) indicates the possibility that NOX-2 is involved in this process. Several reports concerning the role of NOX-2 in the suppression of lysosomal acidification via the inhibition of vacuolar H+-ATPase by ROS have been presented (Sheppard et al. 2005; Savina et al. 2006; Lamb et al. 2009). One possible explanation for simultaneous acidification of the intra- and extracellular spaces is that the inhibition of vacuolar H+-ATPase contributes to cytosolic acidification, while it secondarily causes extracellular acidification by extrusion of H+. However, IL-1β-promoted endocytosis was detected by a probe that emits fluorescence under acidic conditions (Fig. 4c, c’’, d). Hence, IL-1β is unlikely to suppress lysosomal/endosomal acidification. On the other hand, we have previously reported that the expression of NOX-2 induces the necrotic cell death of ATDC5 cells (Yasuhara et al. 2005; Yoshimura et al. 2011). Hence, another possibility is that the lysosomal fluid released from the necrotic cells acidifies the extracellular space. Nevertheless, the precise mechanism of NOX-2 activity-dependent acidification remains to be clarified.
In summary, the results obtained in this and our previous studies indicate that the suppression of NOX-2 activity and ROS production are probably important for the regulation of osteoarthritis progression, namely, the suppression of chondrocyte death and ECM loss.
References
Asari A, Miyauchi S, Miyazaki K, Hamai A, Horie K, Takahashi T, Sekiguchi T, Machida A, Kohno K, Uchiyama Y (1992a) Intra- and extracellular localization of hyaluronic acid and proteoglycan constituents (chondroitin sulfate, keratan sulfate, and protein core) in articular cartilage of rabbit tibia. J Histochem Cytochem 40:1693–1704
Asari A, Miyauchi S, Takahashi T, Kohno K, Uchiyama Y (1992b) Localization of hyaluronic acid, chondroitin sulfate, and CD44 in rabbit cornea. Arch Histol Cytol 55:503–511
Atsumi T, Miwa Y, Kimata K, Ikawa Y (1990) A chondrogenic cell line derived from a differentiating culture of AT805 teratocarcinoma cells. Cell Differ Dev 30:109–116
Browning JA, Wilkins RJ (2004) Mechanisms contributing to intracellular pH homeostasis in an immortalised human chondrocyte cell line. Comp Biochem Physiol A Mol Integr Physiol 137:409–418
Chen C, Xie J, Rajappa R, Deng L, Fredberg J, Yang L (2015) Interleukin-1β and tumor necrosis factor-α increase stiffness and impair contractile function of articular chondrocytes. Acta Biochim Biophys Sin Shanghai 47:21–29
Del Carlo M, Loeser RF (2002) Nitric oxide-mediated chondrocyte cell death requires the generation of additional reactive oxygen species. Arthritis Rheum 46:394–403
Diatchuk V, Lotan O, Koshkin V, Wikstroem P, Pick E (1997) Inhibition of NADPH oxidase activation by 4-(2-aminoethyl)-benzenesulfonyl fluoride and related compounds. J Biol Chem 272:13292–13301
Flannery CR, Little CB, Hughes CE, Caterson B (1998) Expression and activity of articular cartilage hyaluronidases. Biochem Biophys Res Commun 251:824–829
Flores JA, Balseiro-Gomez S, Cabeza JM, Acosta J, Ramirez-Ponce P, Ales E (2014) A new role of myosin II in vesicle fission. PLoS ONE 9:e100757
Goldring MB, Marcu KB (2009) Cartilage homeostasis in health and rheumatic diseases. Arthritis Res Ther 11:224
Grogan SP, D’Lima DD (2010) Joint aging and chondrocyte cell death. Int J Clin Rheumatol 5:199–214
Harada H, Takahashi M (2007) CD44-dependent intracellular and extracellular catabolism of hyaluronic acid by hyaluronidase-1 and −2. J Biol Chem 282:5597–5607
Henrotin Y, Kurz B, Aigner T (2005) Oxygen and reactive oxygen species in cartilage degradation: friends or foes? Osteoarthr Cartil 13:643–654
Kaku M, Yamauchi M (2014) Mechano-regulation of collagen biosynthesis in periodontal ligament. J Prosthodont Res 58:193–207
Kim KS, Choi HW, Yoon HE, Kim IY (2010) Reactive oxygen species generated by NADPH oxidase 2 and 4 are required for chondrogenic differentiation. J Biol Chem 285:40294–40302
Knudson CB, Knudson W (2001) Cartilage proteoglycans. Semin Cell Dev Biol 12:69–78
Lamb FS, Moreland JG, Miller FJ Jr (2009) Electrophysiology of reactive oxygen production in signaling endosomes. Antioxid Redox Signal 11:1335–1347
Lambeth JD (2004) NOX enzymes and the biology of reactive oxygen. Nat Rev Immunol 4:181–189
Lv S-H, Rong S-F, Cai B-G, Guan S-M, Li Q-Q (2015) Property and current clinical applications of mammal hyaluronidase. Eur Rev Med Pharmacol Sci 19:3968–3976
Meredith D, Bell P, McClure B, Wilkins R (2002) Functional and molecular characterisation of lactic acid transport in bovine articular chondrocytes. Cell Physiol Biochem 12:227–234
Milner PI, Wilkins RJ, Gibson JS (2007) The role of mitochondrial reactive oxygen species in pH regulation in articular chondrocytes. Osteoarthritis Cartilage 15:735–742
Nagaya H, Ymagata T, Ymagata S, Iyoda K, Ito H, Hasegawa Y, Iwata H (1999) Examination of synovial fluid and serum hyaluronidase activity as a joint marker in rheumatoid arthritis and osteoarthritis patients (by zymography). Ann Rheum Dis 58:186–188
Reiter CD, Teng RJ, Beckman JS (2000) Superoxide reacts with nitric oxide to nitrate tyrosine at physiological pH via peroxynitrite. J Biol Chem 275:32460–32466
Rink TJ, Tsien RY, Pozzan T (1982) Cytoplasmic pH and free Mg2+ in lymphocytes. J Cell Biol 95:189–196
Savina A, Jancic C, Hugues S, Guermonprez P, Vargas P, Moura IC, Lennon-Dumenil AM, Seabra MC, Raposo G, Amigorena S (2006) NOX2 controls phagosomal pH to regulate antigen processing during crosspresentation by dendritic cells. Cell 126:205–218
Sheppard FR, Kelher MR, Moore EE, McLaughlin NJ, Banerjee A, Silliman CC (2005) Structural organization of the neutrophil NADPH oxidase: phosphorylation and translocation during priming and activation. J Leukoc Biol 78:1025–1042
Shukunami C, Shigeno C, Atsumi T, Ishizeki K, Suzuki F, Hiraki Y (1996) Chondrogenic differentiation of clonal mouse embryonic cell line ATDC5 in vitro: differentiation-dependent gene expression of parathyroid hormone (PTH)/PTH-related peptide receptor. J Cell Biol 133:457–468
Slayman CL, Moussatos VV, Webb WW (1994) Endosomal accumulation of pH indicator dyes delivered as acetoxymethyl esters. J Exp Biol 196:419–438
Tengblad A (1979) Affinity chromatography on immobilized hyaluronate and its application to the isolation of hyaluronate binding properties from cartilage. Biochim Biophys Acta 578:281–289
Wagner AH, Schroeter MR, Hecker M (2001) 17β-Estradiol inhibition of NADPH oxidase expression in human endothelial cells. FASEB J 15:2121–2130
Wilusz RE, Sanchez-Adams J, Guilak F (2014) The structure and function of the pericellular matrix of articular cartilage. Matrix Biol 39:25–32
Yasuhara R, Miyamoto Y, Akaike T, Akuta T, Nakamura M, Takami M, Morimura N, Yasu K, Kamijo R (2005) Interleukin-1β induces death in chondrocyte-like ATDC5 cells through mitochondrial dysfunction and energy depletion in a reactive nitrogen and oxygen species-dependent manner. Biochem J 389:315–323
Yocum SA, Lopresti-Morrow LL, Gabel CA, Milici AJ, Mitchell PG (1995) Bafilomycin A1 inhibits IL-1-stimulated proteoglycan degradation by chondrocytes without affecting stromelysin synthesis. Arch Biochem Biophys 316:827–835
Yoshimura K, Miyamoto Y, Yasuhara R, Maruyama T, Akiyama T, Yamada A, Takami M, Suzawa T, Tsunawaki S, Tachikawa T, Baba K, Kamijo R (2011) Monocarboxylate transporter-1 is required for cell death in mouse chondrocytic ATDC5 cells exposed to interleukin-1β via late phase activation of nuclear factor κB and expression of phagocyte-type NADPH oxidase. J Biol Chem 286:14744–14752
Zamli Z, Sharif M (2011) Chondrocyte apoptosis: a cause or consequence of osteoarthritis? Int J Rheum Dis 14:159–166
Acknowledgements
This work was supported in part by grants from the MEXT-Supported Program for the Strategic Research Foundation at Private Universities from the Ministry of Education, Culture, Sports, Science, and Technology, Japan and Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to declare in regard to this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Fig. S1
Effect of NOX inhibition on aggrecan release in culture supernatants. A ATDC5 cells were pre-cultured for 3 weeks with ITS (insulin-transferrin-selenium) supplementation and then further incubated for 48 h with or without IL-1β (10 ng/ml) and AEBSF (0.3 mmol/l); n = 3. B Nox2 antisense oligodeoxynucleotide or its scrambled control ODN (SRC) were introduced to ATDC5 cells pre-cultured for 3 weeks with ITS supplementation and then the cells were cultured for 48 h in the presence of IL-1β (10 ng/ml). Aggrecan in culture supernatants was determined by using a mouse aggrecan enzyme-linked immunosorbent assay (MyBioSource, San Diego, Calif., USA); n = 3. (EPS 844 kb)
Fig. S2
Effects of pH of culture medium on expressions of aggrecan (Acan), type II collagen (Col2a1), hyaluronidase 1 (Hyal1) and hyaluronidase 2 (Hyal2). ATDC5 cells were cultured for 48 h in medium with pH adjusted to 6.8 or 7.4. Expression of mRNAs for Acan (A), Col2a1 (B), Hyal1 (C) and Hyal2 (D) were evaluated by real-time RT-PCR. The expression level of each gene was normalized to that of Gapdh and is indicated as relative to that obtained in cells cultured at pH 7.4; n = 3. (EPS 977 kb)
Rights and permissions
About this article
Cite this article
Funato, S., Yasuhara, R., Yoshimura, K. et al. Extracellular matrix loss in chondrocytes after exposure to interleukin-1β in NADPH oxidase-dependent manner. Cell Tissue Res 368, 135–144 (2017). https://doi.org/10.1007/s00441-016-2551-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00441-016-2551-2