Abstract
Pathogenic variations in the OTOF gene are a common cause of hearing loss. To refine the natural history and genotype–phenotype correlations of OTOF-related auditory neuropathy spectrum disorders (ANSD), audiograms and distortion product otoacoustic emissions (DPOAEs) were collected from a diverse cohort of individuals diagnosed with OTOF-related ANSD by comprehensive genetic testing and also reported in the literature. Comparative analysis was undertaken to define genotype–phenotype relationships using a Monte Carlo algorithm. 67 audiograms and 25 DPOAEs from 49 unique individuals positive for OTOF-related ANSD were collected. 51 unique OTOF pathogenic variants were identified of which 21 were missense and 30 were loss of function (LoF; nonsense, splice-site, copy number variants, and indels). There was a statistically significant difference in low, middle, and high frequency hearing thresholds between missense/missense and LoF/missense genotypes as compared to LoF/LoF genotypes (average hearing threshold for low, middle and high frequencies 70.9, 76.0, and 73.4 dB vs 88.5, 95.6, and 94.7 dB) via Tukey’s test with age as a co-variate (P = 0.0180, 0.0327, and 0.0347, respectively). Hearing declined during adolescence with missense/missense and LoF/missense genotypes, with an annual mid-frequency threshold deterioration of 0.87 dB/year and 1.87 dB/year, respectively. 8.5% of frequencies measured via DPOAE were lost per year in individuals with serial tests. Audioprofiling of OTOF-related ANSD suggests significantly worse hearing with LoF/LoF genotypes. The unique pattern of variably progressive OTOF-related autosomal recessive ANSD may be amenable to gene therapy in selected clinical scenarios.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Permanent hearing loss is common in children and is most often attributable to a genetic etiology (Smith et al. 2005). Phenotypes range from nonsyndromic hearing loss (NSHL) to deafness in the context of multi-system organ involvement. To date, more than 150 genes and over 8000 variants have been implicated in the pathogenesis of hearing loss (Azaiez et al. 2018). This heterogeneity underscores the need for gene-specific phenotype studies.
OTOF encodes for the protein otoferlin, which is a member of the ferlin family of large transmembrane proteins essential for cell membrane fusion and vesicle formation. Expression of otoferlin has been reported only within the organ of Corti, vestibular hair cells, and central nervous system. Otoferlin is an essential component of Ca2+-dependent inner ear hair cell neurotransmitter exocytosis (Strenzke et al. 2016; Hams et al. 2017; Michalski et al. 2017). Pathogenic variants in OTOF are linked to autosomal recessive nonsyndromic auditory neuropathy spectrum disorders (ANSD) and temperature-sensitive ANSD (Azaiez et al. 2021). Among affected patients with nonsyndromic ANSD, severity of hearing loss ranges from mild-to-moderate (Yildirim-Baylan et al. 2014) to profound (Iwasa et al. 2013).
To date, no relationship between OTOF genotype and the severity of associated hearing loss has been reported. The objective of this paper was to analyze audiograms in a diverse cohort of individuals with OTOF-related ANSD, and to correlate these data with patient age and genotype. As a proxy for outer hair cell function, otoacoustic emission testing was also analyzed. Defining the natural history of OTOF-related deafness is essential for counseling affected individuals and in the design of gene-therapy based clinical trials.
Methods
Data source
Audiograms and DPOAEs were collected from individuals with OTOF-related ANSD after comprehensive genetic testing either in the Molecular Otolaryngology and Renal Research Laboratories (MORL), Iowa City, IA, USA or the Chinese Deafness Genetics Consortium (CDGC), Center for Medical Genetics, Southwest Hospital, Army Medical University, Chongqing, China. To collect additional clinical data, a literature review of OTOF-related deafness was completed and reported audiograms and DPOAEs were included. The literature search was conducted by reviewing the references for all variants annotated as likely pathogenic or pathogenic in the Deafness Variation Database (Azaiez et al. 2018) and in ClinVar. Individuals with temperature-sensitive ANSD or only a single variant in OTOF were excluded. This study was approved by the Institutional Review Boards of both institutions. The data for variant interpretation were reported to the Deafness Variation Database (http://deafnessvariationdatabase.org/).
Audiometry
The standard audiogram was recorded between 250 and 8000 Hz. Depending on age, hearing was tested by behavioral observation audiometry, visual reinforcement audiometry, or conventional audiometry. For inclusion in this study, at least four separate frequencies must have been tested. Only air conduction thresholds were included. Audiograms marked as “poor” reliability were excluded. To generate a single audiogram, the better hearing ear was used at each frequency, as previously described (Taylor et al. 2013). Linear interpolation and extrapolation were used to approximate missing values between 250 and 8000 Hz. Frequency averages were defined as low (250, 500 Hz), middle (1000, 2000 Hz) and high (4000, 8000 Hz). In addition, we collected qualitative descriptions of audiometry for affected individuals reported in the literature. This included severity (e.g., “mild” to “profound”) and shape (e.g., “flat” or “upsloping”). Frequency-specific hearing loss severity was defined as mild (26–40 dB), moderate (41–55 dB), moderately severe (56–70 dB), severe (71–90 dB), or profound (> 90 dB).
Distortion product otoacoustic emissions
The standard DPOAE had an f2 (main test frequency) between 1000 and 8000 Hz. For inclusion in this study, at least four separate frequencies must have been tested in each ear. The raw data were examined to measure signal-to-noise ratio (SNR) at each f2 frequency in both ears. An SNR < 3 dB was considered “absent”, 3–6 dB was considered “borderline”, and > 6 dB was considered “present and normal” when scoring the otoacoustic emission. In accordance with standard newborn hearing screening, at least 75% of the total tested frequencies must have been present and normal for a DPOAE to be considered a “pass”.
Plot generation and statistical analyses
We performed statistical analysis to evaluate the significance of age and genotype versus severity of hearing loss on audiometry. To account for sampling bias due to some affected individuals and siblings having multiple audiograms within the dataset, we utilized a Monte Carlo algorithm (Walls et al. 2020). Low, middle, and high frequency groups were calculated for each audiogram. With the Monte Carlo algorithm, one audiogram was randomly selected from each family included in our cohort, then an analysis of variance (ANOVA) test was performed based on genotype versus frequency group hearing level followed by Tukey’s test, with age as a covariate. This resulted in a single audiogram being included from each unique family for each test iteration (a patient with multiple audiograms was counted as a single “family”). This process was repeated for 10,000 runs for each test, and the median P value of the runs was reported. Audioprofiles were generated for two age bins (0–10 and > 10 years of age) utilizing a Monte Carlo algorithm after sampling a single audiogram from each family for each age bin, repeated for 10,000 iterations. Average hearing thresholds at each frequency between 250 and 8000 Hz were utilized to generate the audioprofiles. To calculate the effect of age on hearing threshold, linear regression analysis was performed at each frequency for each genotype as previously described (Booth et al. 2020); these slopes were averaged to calculate the annual threshold deterioration by frequency group. Statistical analyses with the Monte Carlo algorithm were performed on RStudio v1.3.1093 software (Boston, MA). Data for the audioprofile generation with the Monte Carlo algorithm were generated using Python with the SciPy library (Virtanen et al. 2020). Plot generation was performed using GraphPad Prism v9.0.0 software (San Diego, CA).
Results
67 audiograms with quantitative data were identified from 49 unique individuals with OTOF-related ANSD, ranging from 0 to 23 years of age. Twenty-two of the 67 audiograms were obtained through a review of the literature, while the remaining 45 were obtained by the authors. 26 of 67 (38.8%) audiograms were obtained by conventional pure tone audiometry, 11 (16.4%) were obtained using behavioral observation audiometry, 8 (11.9%) were obtained using visual reinforcement audiometry, and for 22 (32.8%) audiograms, the methodology was not reported. Twenty-five DPOAEs were identified from 21 unique patients, ranging from 0 to 12 years of age. All the DPOAEs were obtained by the authors. Age at time of audiogram or DPOAE is summarized in Table 1. A further 184 cases with OTOF-related deafness were identified in the literature with qualitative descriptions of audiograms. Age at time of audiogram was inconsistently reported in these cases.
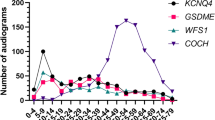
Variants
For individuals with quantitative data available, there were 51 unique genetic variants (41 unique variants in the audiometry group and 35 unique variants in the DPOAE cohort, with 25 variants overlapping). Of these unique variants, 21 were missense, 11 were nonsense, 8 were frameshift deletions, 8 were splice-site mutations, 1 was complex frameshift insertion and deletion, 1 was a 12-base pair in-frame deletion, and 1 was a copy number variant involving an intragenic 5.6 kb deletion. All nonsense, frameshift, splice site, and copy number variants were grouped in a “loss of function” (LoF) category; the 12-base pair in-frame deletion was also included in the LoF group. In the audiometry cohort, 26 audiograms were associated with a missense/missense genotype, 13 were associated with a LoF/missense genotype, and 27 were associated with a LoF/LoF genotype. In the DPOAE cohort, the distribution was 4, 10, and 10, respectively. In one individual in the audiometry and DPOAE cohort, three OTOF variants were identified (1 nonsense, 1 missense and 1 splice-site variant); as this individual did not fit in to the missense/missense, LoF/missense, or LoF/LoF categories, they were excluded from the analysis. Type and location of the variants are listed in Fig. 1. A full list of the variants in the raw audiometry and DPOAE groups are available in Supplemental Table S1.
Map of causative OTOF variants included in this study, based on transcript NM_001287489.2. a Illustration of splice site variants and CNVs. b Illustration of coding variants; variants in red are deletions and/or insertions, variants in green are nonsense mutations, and variants in purple are missense mutations. CNV copy number variant. †This CNV is a deletion with breakpoints of chromosome 2:26,695,190–26,700,779
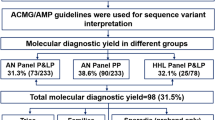
Quantitative audiometry
The mean hearing loss across all frequencies in all 67 audiograms was 82.3 dB (standard deviation (SD) 22.1 dB). Mean low frequency hearing threshold was 78.1 dB (SD 21.2 dB), mean middle frequency hearing threshold was 84.2 dB (SD 22.4 dB), and mean high frequency hearing threshold was 82.3 dB (SD 21.8 dB). Hearing loss at specific frequencies is summarized in Fig. 2. Audiograms and average hearing loss by age are summarized in Table 1. One audiogram was excluded from genotype-specific analysis because the associated individual had three potentially causative OTOF variants. Genotype–phenotype correlations are summarized in Table 2 and Fig. 3. As measured by low, middle, and high frequency groups, 26 audiograms from missense/missense genotypes had a mean hearing loss of 69.6, 73.7, and 72.4 dB (SD 25.1, 25.4, and 23.3 dB), 13 audiograms from LoF/missense genotypes had a mean hearing loss of 73.5, 80.6, and 75.3 dB (SD 22.0, 22.4, 19.9 dB), and 27 audiograms from LoF/LoF genotypes had a mean hearing loss of 88.5, 95.6, and 94.7 dB (SD 11.0, 12.7, and 14.8 dB). These means were statistically significantly different using ANOVA testing with age as a co-variate with a Monte Carlo algorithm for low, middle, and high frequency groups (P = 0.0180, 0.0327, and 0.0347, respectively). Post-hoc analysis using two-sided Tukey’s test with age as a co-variate with a Monte Carlo algorithm showed a statistically significant difference between combined missense/missense and LoF/missense genotypes as compared with LoF/LoF at low, middle, and high frequency hearing thresholds (P = 0.0309, 0.0283, and 0.0296, respectively). Additional comparisons are summarized in Table 2.
Stratified audioprofiles of individuals with OTOF-related hearing loss included in this study. a Audioprofiles based on OTOF genotype (MM, LM, and LL). b Audioprofiles based on individuals with an MM genotype, grouped into age bins. c Audioprofiles based on individuals with an LM genotype, grouped into age bins. d Audioprofiles based on individuals with an LL genotype, grouped into age bins. HL hearing level, MM missense/missense, LM loss of function/missense, LL loss of function/loss of function
Based on linear regression analysis, missense/missense and LoF/missense genotypes had a combined annual threshold deterioration of 1.09 dB/year, 1.25 dB/year and 0.58 dB/year at low, middle, and high frequency groups, respectively; these rates of deterioration were not statistically significant (P = 0.0897, 0.0566, and 0.334, respectively). LoF/LoF genotypes had an annual threshold deterioration of 0.21 dB/year, 0.00 dB/year, and − 0.75 dB/year at low, middle, and high PTAs, respectively; again, these rates of deterioration were not statistically significant (P = 0.522, 0.993, and 0.0833 respectively). These data are summarized in Table 3.
Distortion product otoacoustic emissions
Across all 25 DPOAEs, a median of 12 frequencies were measured in each DPOAE across both ears at an average age of 29.0 months (SD 30.8 months). In total, 294 frequencies were measured; of these, 209 (71.1%) were present and normal, 17 (5.8%) were present and abnormal (borderline), and 68 (23.1%) were absent.
Eight of 25 individuals (32.0%) had at least 75% of frequencies present and normal bilaterally. The average age at time of DPOAE was 21.1 months (SD 15.6 months) for these individuals and 31.3 months (SD 36.0) for those with less than 75% of frequencies present and normal bilaterally. These means were not statistically significantly different by unpaired t test (P = 0.454). Sixteen of 25 individuals (64.0%) had at least 75% of frequencies present in one or both ears. The average age at time of DPOAE was 19.5 months (SD 13.5 months) for these individuals and 45.9 months (SD 44.7 months) for those with less than 75% of frequencies present and normal in at least one ear. These means were statistically significantly different by unpaired t test (P = 0.0365).
Percentage of frequencies present by age group are summarized in Table 1. Genotype–phenotype correlations are summarized in Table 4. Of those patients with biallelic missense or LoF/missense genotypes, two of 14 (14.3%) had at least 75% of frequencies present bilaterally and 8/28 (28.6%) unilaterally, as compared with five of 10 (50.0%) bilaterally and 14 of 20 (70.0%) unilaterally with biallelic LoF genotypes. Likelihood of bilateral “pass” was not statistically significant between these groups, while likelihood of unilateral “pass” was (P = 0.0850 and 0.0078, respectively). There were no statistically significant differences for likelihood of having at least 75% of frequencies present and normal unilaterally or bilaterally between 0–3 and > 3-year-old age groups for any genotype.
Serial DPOAEs were available in 4 patients, with an average of 17.2 months (SD 17.0 months) between the first and second DPOAE. In five of 8 ears (62.5%), there was a decline in frequencies present, while one of 8 (12.5%) showed no change and two of 8 (25.0%) showed an improvement (Fig. 4). The ears that showed improvement were from the same patient, who had biallelic LoF mutations. In aggregate, the change in DPOAEs amounted to a loss of 12.2% of frequencies in all ears, and 8.5% of frequencies per ear per year over the 17.2-month period.
DPOAE results from four individuals with OTOF-related hearing loss with sequential tests. Each individual had two ears tested at each time point; ears from the same individual are represented using the same shape on each graph point. Genotype is listed for each individual. DPOAE results are reported as proportion of frequencies that were present and normal compared with all frequencies tested
Qualitative audiometry
45 articles associated with pathogenic and likely pathogenic OTOF variants from the Deafness Variation Database were reviewed, 18 of which contained qualitative descriptions of audiometry in OTOF-related nonsyndromic hearing loss (Yasunaga et al. 1999, 2000; Adato et al. 2000; Varga et al. 2003, 2006; Rodríguez-Ballesteros et al. 2003, 2008; Rouillon et al. 2006; Choi et al. 2009; Santarelli et al. 2009; Romanos et al. 2009; Zadro et al. 2010; Mahdieh et al. 2012; Matsunaga et al. 2012; Iwasa et al. 2013; Yildirim-Baylan et al. 2014; Jin et al. 2014; Tang et al. 2015). These data comprised 167 unique patients. At least nine of the articles utilized OTOF Sanger sequencing for diagnosis of the hearing loss and required the patients to have at least a severe hearing loss prior to undergoing Sanger sequencing. Of the genotypes for the 167 patients, 43 were missense/missense, 22 were LoF/missense, and 102 were LoF/LoF. Audiograms reported as less than severe (i.e., mild, moderate, or moderately severe) included three of 43 (6.98%) in patients with missense/missense genotypes, one of 22 (4.54%) in patients with LoF/missense genotypes, and one of 102 (0.98%) in patients with LoF/LoF genotypes.
When converting the previously described quantitative audiometry data to qualitative data based on speech/middle frequency PTA, 12 of 26 (46.2%) missense/missense patients were less than severe, four of 13 (30.77%) LoF/missense were less than severe, and two of 27 (7.4%) of the LoF/LoF were less than severe. These data were combined and analyzed by genotype using Fisher’s exact test, which is summarized in Table 5. There was a statistically significant difference between missense/missense and LoF/LoF (P = < 0.0001) as well as LoF/missense and LoF/LoF (P = 0.0117), but not between missense/missense and LoF/missense (P = 0.438).
Discussion
We report the first genotype–phenotype correlations from a large, multi-family dataset for OTOF. Biallelic missense and LoF/missense genotypes were associated with better hearing thresholds than biallelic LoF variants, which is similar to the correlations described for GJB2 genotypes, the most common cause of autosomal recessive hearing loss (Azaiez et al. 2004; Snoeckx et al. 2005). In contrast to GJB2-related deafness, however, there was no statistically significant difference between biallelic missense and LoF/missense genotypes, which may reflect inadequate power as LoF/missense genotypes comprised the lowest number of individuals in this study. We also could not complete a domain specific-analysis, as variants were distributed throughout the entire otoferlin protein with the exception of the C2A domain, which had no pathogenic variants (Fig. 1). In aggregate, we found that biallelic missense variants and LoF/missense genotypes cause severe hearing loss, while biallelic LoF variants cause profound hearing loss.
Audioprofiling of OTOF-related ANSD in this study and in familial studies by others (Chiu et al. 2010; Yildirim-Baylan et al. 2014; Webb et al. 2016) suggests progression of hearing loss with age, though linear regression did not reach statistical significance from our cohort. Our study refines the likelihood of progression—we found that biallelic missense and LoF/missense genotypes show progression of hearing loss, while biallelic LoF variants, which present as profound hearing loss, do not. However, genotype is a stronger driver of outcome than age: in aggregate, individuals over the age of 10 with biallelic missense or LoF/missense genotypes had better hearing thresholds than individuals less than the age of 10 with biallelic LoF genotypes. Nonetheless, there is a wide standard deviation in the degree of hearing loss amongst patients even with similar genotypes suggesting that there may be environmental factors or genetic modifiers that contribute to the observed differences (Walls et al. 2020).
DPOAEs in genetic forms of ANSD, including OTOF, have been reported to decline with age (Kitao et al. 2019). This outcome is hypothesized to reflect loss of outer hair cell function. In our dataset, there did not appear to be a large loss of frequencies with age—loss was limited by the small number of individuals with serial tests and the overall young age of our DPOAE cohort, with the oldest individual being 12-years old. For children who had DPOAEs performed after age 3, over 50% of tested frequencies remained present and normal. Only one child (at the age of 2 years) had complete absence of DPOAEs at all frequencies tested. Amongst patients with serial DPOAEs, an aggregate loss of approximately 8.5% of frequencies per year per ear was noted, which is a more moderate decline than noted by Kitao et al. (2019) in a cohort of DPOAEs in OTOF-related deafness. Our cohort demonstrates a large difference in a theoretical DPOAE screening result by genotype; 14.3% of children with biallelic missense or LoF/missense genotypes would “pass” a standard newborn hearing screening bilaterally (i.e., having at least 75% of tested frequencies present and normal) compared with 50.0% of children with biallelic LoF genotypes. Patients with LoF/missense genotypes were least likely to have a passing result, with zero out of 10 patients having a bilateral “pass”. The reasons for these differences are unclear, as the average hearing loss of all patients with OTOF-related hearing loss are well above the threshold of detection for standard DPOAE testing.
OTOF-related ANSD causes a unique pattern of variably progressive autosomal recessive deafness. A variety of founder mutations have been described in OTOF, including p.Gln829Ter in the Spanish population (Migliosi et al. 2002), p.Val1778Phe in the Ashkenazi Jewish population (Webb et al. 2016), p.Arg1939Gln in the Japanese population (Matsunaga et al. 2012) and p.Glu1700Gln in the Taiwanese population (Chiu et al. 2010). In our cohort, other than p.Glu1700Gln (MAF = 0.67% in the East Asian population in gnomAD), most of the variants are rare with an MAF less than 0.05%. We included 16 audiograms from six individuals from five unique families with biallelic p.Glu1700Gln mutations. Although hearing loss was progressive in all individuals, there was phenotypic variability associated with this genotype. At 1–2 years of age, most individuals had a mild-to-moderate hearing loss, while one had a profound hearing loss. Further studies of intra-familial phenotypic variability for individuals with biallelic OTOF variants will be helpful identify environmental or other factors that contribute to these markedly different outcomes, although compiling large datasets of audiograms from individuals with exactly the same genotype will be considerably more difficult than with autosomal dominant genes.
The current standard of care for patients with OTOF-related ANSD is cochlear implantation. As recently reviewed by Zheng and Liu (2020), patients with OTOF mutations generally have excellent outcomes for sound perception and speech recognition. No relationships between genotype and cochlear implantation response have been noted to date. These individuals in particular benefitted from cochlear implantation before 2 years of age. Abnormal transmission at the auditory synapse caused by genetic mutations, such as in OTOF, are bypassed by cochlear implantation, in contrast to other forms of ANSD that affect primarily the auditory nerve and demonstrate mixed results after cochlear implantation (Teagle et al. 2010; Shearer and Hansen 2019).
Gene therapy for OTOF-related ANSD is an exciting new treatment possibility, with clinical trials set to begin in humans in 2021. Gene therapies for hearing loss may be protective against future decline, or ideally, reverse damage that has already occurred in the cochlea (Omichi et al. 2019). Our data suggest that individuals with at least one missense variant experience a decline in their hearing over time compared to those with biallelic LoF variants, who generally have a profound hearing loss at birth. Those with 0% residual hearing prelingually will have limited efficacy of hearing restoration secondary to inadequate stimulation of the auditory cortex (Butler and Lomber 2013) unless intervention is performed early in life. In contrast, a child born with a moderate-to-severe hearing loss that eventually progresses to a profound hearing loss may be more likely to derive benefit from cochlear implantation or gene therapy later in life due to their matured auditory system, although speech perception is currently the gold standard audiometric parameter to test before intervention. Individuals with biallelic OTOF variants, particularly biallelic LoF variants, must be promptly identified and referred for specialty care to derive the greatest benefit from treatment, including cochlear implantation and gene therapy.
There are several limitations to our study. The audiograms in our cohort were from multiple sources and conducted with different techniques depending on patient age. With qualitative audiograms, authors generally did not describe their cut-offs for degree of hearing loss. Test–retest threshold differences at high frequencies can be greater than ± 10 dB in approximately 1–5% of adults undergoing pure tone audiometry (Valente et al. 1992; Schmuziger et al. 2004), although we believe that the large number of audiograms in our study offsets this variability. Speech discrimination scores were rarely collected in this cohort of patients, many of whom were prelingual. Due to the importance of speech discrimination testing in auditory neuropathy, in future studies, genotype–phenotype correlations involving these tests would be helpful. For mutation type, patients were broadly grouped into missense/missense, LoF/missense, and LoF/LoF; there were insufficient numbers of studies to examine other differences in closer detail, such as comparing domains or splice site mutations versus frameshift mutations. DPOAEs are a valuable tool for assessing the function of outer hair cells but are not specific for outer hair cell function alone. It is possible that other conditions, such as otitis media, external ear anomalies, or congenital ossicular anomalies, led to false negative results in our cohort. These alternatives could not be ruled out without a thorough history and physical examination on each of the included individuals. Finally, a publication bias may exist with regards to raw audiometry in genetic deafness. For patients with a flat, profound hearing loss, researchers may simply describe the audiogram and not publish the raw data. This limitation is reflected in our Supplemental Table S2, in which most of the audiograms are qualitatively described as “profound”. Nonetheless, when these data were combined with the raw audiometry, a statistically significant difference in the qualitative severity remained. As most of our raw audiometry is comprised of patients who were diagnosed via comprehensive massively parallel sequencing without presupposition as to the diagnosis, this bias is minimized.
Conclusion
Audioprofiling of OTOF-related ANSD suggests significantly worse hearing with LoF/LoF genotypes. OTOF-related ANSD causes a unique pattern of variably progressive autosomal recessive deafness that may be amenable to gene therapy in selected clinical scenarios.
Data availability
Data supporting this study’s findings are available within the article and its supplementary materials.
References
Adato A et al (2000) Deafness heterogeneity in a Druze isolate from the Middle East: novel OTOF and PDS mutations, low prevalence of GJB2 35delG mutation and indication for a new DFNB locus. Eur J Hum Genet EJHG 8(6):437–442. https://doi.org/10.1038/sj.ejhg.5200489
Azaiez H et al (2004) GJB2: The spectrum of deafness-causing allele variants and their phenotype. Hum Mutat 24(4):305–311. https://doi.org/10.1002/humu.20084
Azaiez H et al (2018) Genomic landscape and mutational signatures of deafness-associated genes. Am J Hum Genet 103(4):484–497. https://doi.org/10.1016/j.ajhg.2018.08.006
Azaiez H, Thorpe RK, Smith RJ (2021) OTOF-related deafness. In: Adam MP et al (eds) GeneReviews®. University of Washington, Seattle, WA
Booth KT, Azaiez H, Smith RJH (2020) DFNA5 (GSDME) c.991-15_991-13delTTC: founder mutation or mutational hotspot? Int J Mol Sci 21(11):3951. https://doi.org/10.3390/ijms21113951
Butler BE, Lomber SG (2013) Functional and structural changes throughout the auditory system following congenital and early-onset deafness: implications for hearing restoration. Front Syst Neurosci. https://doi.org/10.3389/fnsys.2013.00092
Chiu Y-H et al (2010) Mutations in the OTOF gene in Taiwanese patients with auditory neuropathy. Audiol Neurotol 15(6):364–374. https://doi.org/10.1159/000293992
Choi BY et al (2009) Identities and frequencies of mutations of the otoferlin gene (OTOF) causing DFNB9 deafness in Pakistan. Clin Genet 75(3):237–243. https://doi.org/10.1111/j.1399-0004.2008.01128.x
Hams N et al (2017) Otoferlin is a multivalent calcium-sensitive scaffold linking SNAREs and calcium channels. Proc Natl Acad Sci 114(30):8023–8028. https://doi.org/10.1073/pnas.1703240114
Iwasa Y et al (2013) OTOF mutation screening in Japanese severe to profound recessive hearing loss patients. BMC Med Genet 14:95. https://doi.org/10.1186/1471-2350-14-95
Jin YJ et al (2014) Identification of a novel splice site variant of OTOF in the Korean nonsyndromic hearing loss population with low prevalence of the OTOF mutations. Int J Pediatr Otorhinolaryngol 78(7):1030–1035. https://doi.org/10.1016/j.ijporl.2014.03.033
Karczewski KJ et al (2020) The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 581(7809):434–443. https://doi.org/10.1038/s41586-020-2308-7
Kitao K et al (2019) Deterioration in distortion product otoacoustic emissions in auditory neuropathy patients with distinct clinical and genetic backgrounds. Ear Hear 40(1):184–191. https://doi.org/10.1097/AUD.0000000000000586
Mahdieh N et al (2012) Screening of OTOF mutations in Iran: a novel mutation and review. Int J Pediatr Otorhinolaryngol 76(11):1610–1615. https://doi.org/10.1016/j.ijporl.2012.07.030
Matsunaga T et al (2012) A prevalent founder mutation and genotype-phenotype correlations of OTOF in Japanese patients with auditory neuropathy. Clin Genet 82(5):425–432. https://doi.org/10.1111/j.1399-0004.2012.01897.x
Michalski N et al (2017) Otoferlin acts as a Ca2+ sensor for vesicle fusion and vesicle pool replenishment at auditory hair cell ribbon synapses. eLife 6:e31013. https://doi.org/10.7554/eLife.31013
Migliosi V et al (2002) Q829X, a novel mutation in the gene encoding otoferlin (OTOF), is frequently found in Spanish patients with prelingual non-syndromic hearing loss. J Med Genet 39(7):502–506. https://doi.org/10.1136/jmg.39.7.502
Omichi R et al (2019) Gene therapy for hearing loss. Hum Mol Genet 28(R1):R65–R79. https://doi.org/10.1093/hmg/ddz129
Rodríguez-Ballesteros M et al (2003) Auditory neuropathy in patients carrying mutations in the otoferlin gene (OTOF). Hum Mutat 22(6):451–456. https://doi.org/10.1002/humu.10274
Rodríguez-Ballesteros M et al (2008) A multicenter study on the prevalence and spectrum of mutations in the otoferlin gene (OTOF) in subjects with nonsyndromic hearing impairment and auditory neuropathy. Hum Mutat 29(6):823–831. https://doi.org/10.1002/humu.20708
Romanos J et al (2009) Novel OTOF mutations in Brazilian patients with auditory neuropathy. J Hum Genet 54(7):382–385. https://doi.org/10.1038/jhg.2009.45
Rouillon I et al (2006) Results of cochlear implantation in two children with mutations in the OTOF gene. Int J Pediatr Otorhinolaryngol 70(4):689–696. https://doi.org/10.1016/j.ijporl.2005.09.006
Santarelli R et al (2009) Abnormal cochlear potentials from deaf patients with mutations in the otoferlin gene. J Assoc Res Otolaryngol JARO 10(4):545–556. https://doi.org/10.1007/s10162-009-0181-z
Schmuziger N, Probst R, Smurzynski J (2004) Test-retest reliability of pure-tone thresholds from 0.5 to 16 kHz using sennheiser HDA 200 and etymotic research ER-2 earphones. Ear Hear 25(2):127–132. https://doi.org/10.1097/01.AUD.0000120361.87401.C8
Shearer AE, Hansen MR (2019) Auditory synaptopathy, auditory neuropathy, and cochlear implantation. Laryngosc Investig Otolaryngol 4(4):429–440. https://doi.org/10.1002/lio2.288
Smith RJ, Bale JF, White KR (2005) Sensorineural hearing loss in children. Lancet 365(9462):879–890. https://doi.org/10.1016/S0140-6736(05)71047-3
Snoeckx RL et al (2005) GJB2 Mutations and degree of hearing loss: a multicenter study. Am J Hum Genet 77(6):945–957. https://doi.org/10.1086/497996
Strenzke N et al (2016) Hair cell synaptic dysfunction, auditory fatigue and thermal sensitivity in otoferlin Ile515Thr mutants. EMBO J 35(23):2519–2535. https://doi.org/10.15252/embj.201694564
Tang H-Y et al (2015) DNA sequence analysis and genotype-phenotype assessment in 71 patients with syndromic hearing loss or auditory neuropathy. BMJ Open 5(5):e007506. https://doi.org/10.1136/bmjopen-2014-007506
Taylor KR et al (2013) Audiogene: predicting hearing loss genotypes from phenotypes to guide genetic screening. Hum Mutat 34(4):539–545. https://doi.org/10.1002/humu.22268
Teagle HFB et al (2010) Cochlear implantation in children with auditory neuropathy spectrum disorder. Ear Hear 31(3):325–335. https://doi.org/10.1097/AUD.0b013e3181ce693b
Valente M, Valente M, Goebel J (1992) High-frequency thresholds: circumaural earphone versus insert earphone. J Am Acad Audiol 3(6):410–418
Varga R et al (2003) Non-syndromic recessive auditory neuropathy is the result of mutations in the otoferlin (OTOF) gene. J Med Genet 40(1):45–50. https://doi.org/10.1136/jmg.40.1.45
Varga R et al (2006) OTOF mutations revealed by genetic analysis of hearing loss families including a potential temperature sensitive auditory neuropathy allele. J Med Genet 43(7):576–581. https://doi.org/10.1136/jmg.2005.038612
Virtanen P et al (2020) SciPy 1.0: fundamental algorithms for scientific computing in Python. Nat Methods 17(3):261–272. https://doi.org/10.1038/s41592-019-0686-2
Walls WD et al (2020) A comparative analysis of genetic hearing loss phenotypes in European/American and Japanese populations. Hum Genet 139(10):1315–1323. https://doi.org/10.1007/s00439-020-02174-y
Webb B et al (2016) Identification of a novel pathogenic OTOF variant causative of nonsyndromic hearing loss with high frequency in the Ashkenazi Jewish population. Appl Clin Genet 9:141–146. https://doi.org/10.2147/TACG.S113828
Yasunaga S et al (1999) A mutation in OTOF, encoding otoferlin, a FER-1-like protein, causes DFNB9, a nonsyndromic form of deafness. Nat Genet 21(4):363–369. https://doi.org/10.1038/7693
Yasunaga S et al (2000) OTOF encodes multiple long and short isoforms: genetic evidence that the long ones underlie recessive deafness DFNB9. Am J Hum Genet 67(3):591–600. https://doi.org/10.1086/303049
Yildirim-Baylan M et al (2014) Evidence for genotype-phenotype correlation for OTOF mutations. Int J Pediatr Otorhinolaryngol 78(6):950–953. https://doi.org/10.1016/j.ijporl.2014.03.022
Zadro C et al (2010) Five new OTOF gene mutations and auditory neuropathy. Int J Pediatr Otorhinolaryngol 74(5):494–498. https://doi.org/10.1016/j.ijporl.2010.02.004
Zheng D, Liu X (2020) cochlear implantation outcomes in patients with OTOF mutations. Front Neurosci. https://doi.org/10.3389/fnins.2020.00447
Acknowledgements
This project was supported in part by NIH-NIDCD grant R01′s DC002842, DC012049, and DC017955 (RJHS) and NIH-NIDCD grant 5T32DC000040 (RKT).
Funding
This project was supported in part by NIH-NIDCD grant R01's DC002842, DC012049, and DC017955 (RJHS) and NIH-NIDCD grant 5T32DC000040 (RKT).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethics approval
Clinical data were collected as approved by the University of Iowa Institutional Review Board (IRB), project identification number 201602772.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Thorpe, R.K., Azaiez, H., Wu, P. et al. The natural history of OTOF-related auditory neuropathy spectrum disorders: a multicenter study. Hum Genet 141, 853–863 (2022). https://doi.org/10.1007/s00439-021-02340-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-021-02340-w