Abstract
Strongyloidiasis is a neglected tropical disease caused mainly by Strongyloides stercoralis, a nematode that can persist for decades in the human host with a very low parasitic burden and without specific symptoms. Hence, it is difficult to diagnose and control. Larval concentration and culture methods with fecal samples show higher sensitivity for the diagnosis of Strongyloides-infected individuals; however, these techniques are not routinely used, primarily due to the challenges associated with processing a substantial volume of fecal samples. In the current study, we comparatively evaluated the sensitivity and applicability of modifications made to the Rugai parasitological method for the diagnosis of strongyloidiasis in fecal samples of experimentally infected rats and in 68 individuals from an urban community close to Maceió, Brazil. The presence and quantity of parasite larvae in the feces were comparatively evaluated using different parasitological techniques. In the experimental model, we demonstrated that the modified Rugai technique (RMOD) allowed for significantly higher recovery of larvae than the original Rugai technique (RO). Moreover, the sediment was cleaner and easier to evaluate using optical microscopy. Compared to other parasitological techniques, such as agar-plate culture (A-PC) and spontaneous sedimentation (SS), the RMOD technique showed higher sensitivity in the detection of larvae in all infected groups and presented comparatively better performance, especially in rats with a low parasite burden. In the human population, among the 68 stool samples evaluated, Strongyloides larvae were detected in the feces of six individuals with an estimated prevalence of 8.82%. However, the performance of each parasitological method was remarkably different. SS identified Strongyloides larvae in only two individuals and A-PC in three, whereas RMOD was able to identify six infected individuals, resulting in sensitivities of 33.3%, 50%, and 100%, respectively. In conclusion, the modifications introduced to the Rugai technique resulted in improved sensitivity for the detection of Strongyloides spp. infections, especially in stool samples with a low parasite burden, in comparison with other routinely used parasitological techniques.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Strongyloidiasis is a parasitic disease caused mainly by Strongyloides stercoralis and is found more frequently in tropical and subtropical regions with precarious sanitary conditions, low incomes, and environmental factors favorable for parasite development (Olsen et al. 2009; Requena-Méndez et al. 2013; Page and Speare 2016). Recent estimates indicate that 600 million people would be infected with this nematode worldwide, primarily in areas located in Southeast Asia, Africa, the Western Pacific, and Latin America, including Brazil (Buonfrate et al. 2020; WHO 2022). Nonetheless, significant challenges persist in accurately gauging the real impact of strongyloidiasis on human health. This is attributed to the complexities inherent to the biological development of this parasite, the absence of specific symptoms of this disease in most infected people, and the low sensitivity of the available laboratory diagnostic methods (Krolewiecki and Nutman 2019).
During the parasitic phase of S. stercoralis development, only female worms parasitize the mucosal surfaces of the small intestine. These worms reproduce via parthenogenesis and produce a small number of larvae that are eliminated sporadically and intermittently in the feces of the infected host (Toledo et al. 2015; Viney and Lok 2015). In human infection, some larvae that reach the infective stage while still in the intestinal tract can reinfect the host even in the absence of new exposure to contaminated soil, leading to internal autoinfection, a process that is responsible for the long-lasting persistence of the infection (Grove 1996). In addition, most individuals infected with S. stercoralis are asymptomatic or present nonspecific symptoms and have a low parasite burden (Vadlamudi et al. 2006; Marcos et al. 2008), leading to difficulties in the diagnosis and control of strongyloidiasis. Moreover, in immunocompromised individuals, strongyloidiasis would become a life-threatening disease with the possibility of hyperinfection and parasite dissemination, which can be fatal in up to 85% of the cases (Viney and Lok 2007; Mejia and Nutman 2012; Schar et al. 2013; Toledo et al. 2015).
Hence, it is imperative to develop highly sensitive diagnostic methodologies capable of promptly identifying infections, including those in individuals harboring exceedingly low parasite loads. This is crucial for averting further parasite dissemination and mitigating the potential for more severe clinical manifestations.
The definitive diagnosis of strongyloidiasis is based on the observation of parasite larvae, especially in stool samples. However, no reliable reference test is available that can be considered the “gold standard” for the diagnosis of this infection (Siddiqui and Berk 2001; Arifin et al. 2019). The parasitological techniques used in routine diagnosis, such as direct smears, spontaneous fecal sedimentation, formalin-ether concentration, and the Kato-Katz method, show low sensitivity for the detection of Strongyloides larvae (Siddiqui and Berk 2001) because of the small number of eggs and larvae produced by parthenogenetic parasitic females (Viney and Lok 2015; Toledo et al. 2015). Therefore, parasitological diagnostic methods based on larval concentrations, such as the Baermann-Moraes and Rugai techniques, have been recommended (Requena-Mendez et al. 2013). Both concentration techniques are based on larval positive hydrotropism and thermotropism and show similar efficacy in the coprological diagnosis of strongyloidiasis (Siddiqui and Berk 2001; Requena-Mendez et al. 2013). However, the Rugai technique is simpler and easier to apply to a large number of samples (Rugai et al. 1954). Stool culture methods, such as the Harada-Mori and agar-plate culture techniques, are also used to improve the sensitivity in cases of low parasite burden. However, these techniques also require a more specific laboratory infrastructure and are more time-consuming (Anamnart et al. 2010; Ketzis 2017).
Although concentration techniques show better sensitivity in the diagnosis of S. stercoralis infection (Campo Polanco et al. 2014), they are still not used as routine diagnostic methods by most healthcare services in endemic countries because of the logistical difficulties in working with a large number of samples (Buonfrate et al. 2018; Krolewiecki and Nutman 2019; Hailu et al. 2021). Therefore, there is an urgent need to develop a simple, economical, rapid, logistically applicable, and sensitive diagnostic method for use in epidemiological studies and clinical trials. Here, we aimed to introduce modifications to the Rugai technique to improve its sensitivity and facilitate its application in large-scale field studies.
Material and methods
Ethical considerations
In the present work, the parasitological diagnostic tests for the diagnosis of Strongyloides larvae, including the modifications made to the Rugai technique, were comparatively tested using stool samples derived from rats experimentally infected with S. venezuelensis and from fecal samples from a human population living in area where soil-transmitted helminth infections were prevalent (located in Maceió, Alagoas, Brazil).
All experimental procedures performed in rats were approved by the Ethics Committee for Animal Use (CEUA/UFMG), under protocol number 129/2020. The human study was approved by the local Ethics Committee for Human Research (COEP) and registered on the Brazilian Platform for Research with Human Subjects (Plataforma Brasil) under the number CAAE#55239522.3.0000.5149. Before data collection, a free and informed consent form was read and signed by all participants or by the parents and legal guardians of the participating children. Infected individuals were treated with praziquantel (40–60 mg/kg) for schistosomiasis, ivermectin (200 mg/kg) for strongyloidiasis, albendazole (400 mg as a single dose) for other intestinal helminth infections, and metronidazole (250 mg twice for five days) for parasitic protozoa.
Experimental procedures in rats
Male specific-pathogen-free (SPF) Wistar rats, aged 4–6 weeks (weight ~ 120 g), were purchased from the Animal Facility of the Federal University of Minas Gerais (UFMG, Brazil) and maintained at the animal facility for infected animals of the Department of Parasitology (ICB, UFMG, Brazil) during the experimental procedure. Rats were fed standard chow (Presence, Piracicaba, Brazil) diet and provided ad libitum access to tap water.
For experimentally induced infections, S. venezuelensis filiform larvae (L3) were obtained from the stool cultures of infected rats and collected using the Baermann-Moraes technique (Moraes 1948). The recovered L3 larvae were washed three to four times in phosphate-buffered saline (PBS), quantified under a stereomicroscope, and used for infection (Negrão-Corrêa et al. 2004, 2006).
To better evaluate larval elimination during strongyloidiasis, we used rats as experimental models, and each animal was inoculated subcutaneously with 100 μL of PBS containing 10 (low parasite dose) or 500 (high parasite dose) infective larvae, according to Schilter et al. (2010). Moreover, we evaluated the parasite output in rats that were infected and treated with ivermectin, an anthelmintic used to treat strongyloidiasis (Henriquez-Camacho et al. 2016). Finally, the rats were randomly distributed into four experimental groups containing seven animals each, which are described as follows: (1) a group infected with a low burden of S. venezuelensis (10L3), (2) a group infected with a high burden of S. venezuelensis (500L3), (3) a group infected with a low burden of S. venezuelensis and treated with an anthelmintic (10L3 + IVC), and (4) a group infected with a high burden of S. venezuelensis and treated with an anthelmintic (500L3 + IVC). For anthelmintic treatment, a dose of 200 μg/kg/day of ivermectin (Ivermec 1%—Chemitac®, Ipiranga, SP, Brazil) was administered orally on days 15 and 16 post-infection (dpi) (Henriquez-Camacho et al. 2016). At 5, 10, 15, 20, 25, 30, 35, 40, and 45 dpi, feces from each rat in all experimental groups were collected and processed for parasitological analysis (Fig. 1). For stool collection, the infected rats were maintained individually in polypropylene cages (40 × 33 × 16 cm) containing humidified filter paper (adapted from Chaves et al. 2015). Fecal samples were collected, homogenized, and separated into subsamples of 1 g, which were used to perform the following parasitological diagnostic methods: spontaneous sedimentation (SS), agar-plate culture (A-PC), original Rugai (RO), and modified Rugai (RMOD), as described below.
Experimental design. Male Wistar rats were subcutaneously infected with 10 (low burden) or 500 (high burden) infective S. venezuelensis L3 larvae on day 0. On day 15, subgroups of infected rats with low and high parasite burdens received a dose of 200 μg/kg/day of ivermectin (Chemitac®, Ipiranga, SP, Brazil) orally for 2 consecutive days (10L3+ IVC or 500L3 + IVC groups). Another infected group was kept untreated (10L3 or 500L3 groups). A total of seven rats were used in each experimental group. Parasitological evaluations were performed in fecal samples collected at different timepoints over 45 days post-infection
Human population: study population and parasitological assessment
The current study was carried out among residents from the Vergel do Lago community in the Municipality of Maceió, State of Alagoas, located in Northeastern Brazil (9° 39′ 4″ S 35° 46′ 0″ W). The participants were residents registered at the local community center (Centro Comunidade Espírita Nosso Lar) who agreed to participate in a research project that aimed to evaluate the prevalence of schistosomiasis and other helminthiases. Of the 81 registered individuals who agreed to participate in the study, 68 individuals (both sexes, aged 9–84 years) provided sufficient fecal samples for the proposed analyses and were included in the current study.
The stool sample provided by each participant was homogenized and processed to perform the following parasitological diagnostic techniques: spontaneous sedimentation (SS), Helmintex®, agar-plate culture (A-PC), and modified Rugai (RMOD), as detailed below. The fecal material processed by each parasitological test was examined under an optical microscope (× 100 magnification) for the presence of Strongyloides sp. larvae and eggs of any other intestinal helminth species, and the data were used to create a “Consolidated Reference Standard” (CRS). Individuals who presented larvae with a rhabditiform esophagus occupying the anterior third of the body, short mouth cavity, and the presence of genital primordium (Schad 1989) in any of the parasitological tests were considered to be infected by S. stercoralis.
Parasitological techniques
Spontaneous sedimentation (SS)
The SS technique, a parasitological method commonly used for stool examination, was performed as described by Hoffman et al. (1934). To allow a quantitative comparison with other parasitological diagnostic methods, a defined amount of feces was used. Briefly, 1 g of feces obtained from S. venezuelensis-infected rats were homogenized in 5 mL of PBS containing 10% formalin for fixation. The fecal suspension was filtered through gauze and collected in a sedimentation cone for spontaneous sedimentation. After 2 h, two aliquots of 100 µL obtained from the bottom of each sample were mixed with a Lugol solution and examined under an optical microscope (Nikon Eclipse E200, New York, USA). The number of S. venezuelensis eggs found on each slide was counted and expressed as the number of eggs per gram of feces. For human samples, 3–5 g of feces was homogenized in filtered water containing 10% formalin, filtered through gauze, and transferred to a sedimentation cone. After 2 h of decantation, three sediment samples were examined using light microscopy (× 100) for the presence of Strongyloides sp. larvae. For the human samples, the results of the SS technique were qualitatively evaluated and expressed as positive or negative for the presence of the parasite.
Helmintex
The Helmintex® technique, which is used for the detection of infection in individuals infected with a low parasite burden of Schistosoma mansoni, was performed according to the protocol by Favero et al. (2017). For this purpose, 30 g of feces were suspended in 70% ethanol and treated with detergent (Tween-20), followed by repetitive filtration and sedimentation steps. Thereafter, a solution containing magnetic particles was added to promote the separation of S. mansoni eggs from fecal debris. Finally, the free suspension was discarded, and the attached particles, which formed the final sediment, were mixed with a 3% ninhydrin solution and transferred to microscope slides to search for S. mansoni eggs.
Agar-plate culture (A-PC)
A-PC was performed according to previously described protocols (Arakaki et al. 1988; Koga et al. 1991). Briefly, the agar medium was prepared with 15 g of Difco™ Nutrient Agar, BD (Sparks, MD21152 USA) in 1 L of distilled water, followed by autoclaving the medium (120 °C for 20 min). Next, 10 mL of the agar medium were plated in sterile Petri dishes (140 × 15 mm) and left at room temperature to allow solidification. Subsequently, the plates were packaged and stored at 4 °C until further use. For the parasitological assay, 1 g of each fecal samples derived from infected rats or 3 g of human feces were spread on the central part of the agar plates and incubated at 37 °C for 48 h. After incubation, tracks of larval migration were observed in the medium to confirm the presence of live larvae in the stool samples. Then, the fecal material was removed, and the plates were washed with 15 mL of 70% ethyl alcohol. This suspension was collected from the agar surface and centrifuged at 3000 rpm for 3 min. The sediment was concentrated in 2 mL of PBS containing 10% formalin for material fixation and stained with Lugol solution. Furthermore, aliquots of each sample (100 µL each) were analyzed under an optical microscope (Nikon) to verify the presence and count Strongyloides larvae. The average number of larvae per aliquot of feces was transformed into larvae per gram of feces.
Original Rugai method (RO)
The Rugai parasitological method was performed based on the original description (Rugai et al. 1954), using a defined amount of feces. It is noteworthy that unlike S. stercoralis, which directly eliminates larvae in the feces, the species S. venezuelensis used in the experimental study eliminates eggs in the feces, which quickly hatch under adequate environmental conditions (Takamure 1995; Toledo et al. 2015). Therefore, for a comparative analysis of the Rugai concentration methods (original or modified), the fecal samples of S. venezuelensis-infected rats were kept in contact with heated water for 24 h to allow larval development and migration, and the sediment was evaluated afterwards. Briefly, 1 g of stool sample from infected rats was homogenized and wrapped in folded gauze. Then, these samples were transferred to the surface of a sedimentation cone and maintained in contact with water at 40-42 °C. After 24 h, the sediment at the bottom of the sedimentation glass was collected and stained with Lugol’s solution, and the volume was adjusted to 2 mL. Two 100-µL aliquots of each sample were examined under an optical microscope (Nikon), and the parasite larvae were counted. The mean number of larvae per fecal sample was transformed into the number of larvae per gram of fecal sample.
Modified Rugai method (RMOD)
In the current study, some modifications were made to the Rugai technique to improve the number of larvae recovered from fecal samples and obtain cleaner, easy-to-analyze sediments. It is important to mention that among the larval concentration methods applied to fecal samples, the Rugai technique is easier to perform under field conditions, allowing for the evaluation of a large number of samples (Rugai et al. 1954). Briefly, 1 g of stool samples from infected rats or 10 g of human feces were homogenized with filtered water to obtain a pasty consistency. The homogenized fecal samples were mixed with medium-expanded vermiculite (or granulated charcoal) at a ratio of 1:2 (w/w, feces/vermiculite). This fecal mixture was then wrapped in layers of surgical gauze (Gaze Type Cheese 11F, 15 × 15 cm), covered with an external layer of multi-purpose cleaning cloth (nonwoven, viscose, and latex synthetic fabric, 40G Smoot, 20 × 20 cm), and placed inside a sieve on top of a water-filled plastic sedimentation cone, allowing contact between the fecal mixture and the warm water (40–42 °C). As mentioned previously, the fecal mixture prepared with feces from S. venezuelensis-infected rats was kept in contact with warm water for 24 h (the period necessary for the hatching and migration of S. venezuelensis larvae), whereas the fecal mixture with human feces was kept in contact with warm water for 2 h. After this period, a 9-mL sample was collected from the bottom of the sedimentation cone, and 1 mL of formalin (Formaldehyde 37% PA-ACS, Labsynth®, Diadema, SP, Brazil) was immediately added. The mixture was homogenized and centrifuged at 400 g for 5 min. Subsequently, 8 mL of the supernatant were carefully discarded, leaving 2 mL of the sedimented material. Two aliquots of each sample (100 µL each) were mixed with Lugol solution and analyzed under the light microscope (Nikon), and the number of larvae per aliquot was used to calculate the number of larvae per gram of feces.
Statistical analysis
Statistical analyses were performed using Open Epi version 3.01 (Atlanta, USA), GraphPad Prism version 8.02 (San Diego, CA, USA), and Stata 16.0 (College Station, TX, USA). The normal distribution of the data was verified using the Kolmogorov–Smirnov test. Two-way ANOVA was performed followed by the Bonferroni post-test to compare the means of parametric data between more than two groups. Student’s t-test was used when only two groups were compared. The medians obtained from the two experimental groups with nonparametric distributions were compared using the Mann–Whitney U test. The chi-square test was used to compare the frequency (%) of categorical data between groups. Differences with a p value ≤ 0.05 were considered significant. In order to evaluate the performance of the different parasitological diagnostic tests for strongyloidiasis in the human population, a CRS was established, which included all individuals with the presence of characteristic larvae in feces evaluated by any of the parasitological methods used (SS, A-PC, RMOD, and Helmintex). The overall prevalence of Strongyloides infection in the endemic area was calculated as the number of positive individuals identified by CRS diagnostic tests divided by the total number of participants (negative + positive). The diagnostic accuracy of each parasitological test was compared with that of CRS by calculating the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and concordance (kappa statistics). To assess the degree of agreement between the different techniques, the kappa index (κ) was calculated, which varied from 0 to 1.0 (Landis and Koch 1997).
Results
Comparative evaluation of the RO and modified Rugai technique (RMOD) for diagnosis of strongyloidiasis
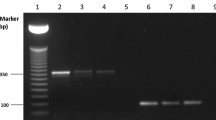
Table 1 shows the number of S. venezuelensis larvae recovered from the fecal samples of experimentally infected rats (500 L3 larvae/rat) that were evaluated using the RO and the RMOD. Compared to the RO method, the RMOD technique recovered a significantly higher number of parasite larvae in all positive fecal samples evaluated (Table 1). The average larval recovery by the RMOD technique during all experimental protocols was 4.6-fold higher than that by the RO technique. This difference was increased up to 10 times when a very low number of larvae were eliminated in feces (Table 1). In addition, it is important to highlight that using the RMOD technique, we were able to detect larval elimination over a prolonged period. Specifically, at 35 dpi, when most of the adult worms were already eliminated (Baek et al. 2003), the frequency of the detection of animals positive for the presence of eggs/larvae by RO was only 28.6%, whereas RMOD revealed that 85.7% of the experimentally infected rats still presented eggs/larvae in their feces (Table 1). These data indicate improved sensitivity of the RMOD technique in identifying a small number of larvae in stool examinations. Additionally, the RMOD technique allowed us to obtain cleaner final sediments, rendering it easier to find and count the eliminated larvae (Fig. 2).
Representative condition of the final sediment obtained from the original (RO) and modified (RMOD) Rugai techniques. Rats were infected on day 0 with 500 L3 of S. venezuelensis, and the parasitological examinations were performed with RO (A) and RMOD (B) techniques using 1 g of fecal samples collected from the same experimentally infected rat at 15 days post-infection. Aliquots of 100 µL of each sample were analyzed under a light microscope (Nikon). Note the larvae (indicated by arrows) in B are cleaner and easier to identify. Scale bars = 100 µm
Diagnostic efficacy of the RMOD compared with that of other parasitological tests
We also compared the effectiveness of the RMOD technique with that of the SS and A-PC to identify and quantify S. venezuelensis larvae in rats experimentally infected with different parasite burdens (Fig. 3). In rats with a high parasite burden (500 L3/rat, Fig. 3A), the RMOD technique recovered a significantly higher number of parasite larvae from stool samples than the SS technique between 5 and 35 dpi. Moreover, the RMOD technique recovered significantly more parasitic larvae than the A-PC technique between 10 and 25 dpi.
Evaluation of the effectiveness of modified Rugai (RMOD), agar-plate culture (A-PC), and spontaneous sedimentation (SS) techniques in the recovery of larvae and/or eggs of S. venezuelensis in feces of rats infected with 500 L3 or 10 L3, treated or not with an anthelmintic. A, B Rats were infected with 500 L3/rat (high parasite burden). C, D Rats infected with 10 L3/rat (low parasite burden). B, D All infected rats were orally treated with 200 μg/kg of ivermectin (Chemitac®, Ipiranga, SP, Brazil) on days 15 and 16 p.i. One gram of fecal sample was individually collected per animal and comparatively evaluated by SS, A-PC, and RMOD at 0, 5, 10, 15, 20, 25, 30, 35, 40, and 45 days post-infection. Data are presented as mean egg/larval counts ± standard error of the mean (SEM) and were analyzed by two-way ANOVA followed by Bonferroni post-test. n = 7 rats/group. * represents statistically different data for RMOD compared with SS and # represents data statistically different bewteen RMOD and A-PC techniques. # or *p < 0.05; ## or **p < 0.01; ### or ***p < 0.001; #### or ****p < 0.0001
In fecal samples from rats with a low parasite burden (10 L3/rat, Fig. 3C), the number of S. venezuelensis larvae recovered by SS was significantly lower than that recovered by the A-PC and RMOD techniques. Moreover, the RMOD technique enabled us to recover a significantly higher number of larvae at 10 and 15 dpi than the A-PC method (Fig. 3C). On the 40th dpi, when the infected rats spontaneously eliminated most of the parasite infection and the number of larvae in the feces decreased further, the RMOD technique was the only parasitological method capable of detecting the presence of Strongyloides larvae (Fig. 3C).
Rats infected with a low dose of S. venezuelensis (10 L3/rat) showed a sharp reduction in the number of eliminated larvae in the feces after treatment with ivermectin, and no more larvae were found in stool samples from 20 dpi onwards, regardless of the parasitological test results (Fig. 3D). However, in rats infected with a high dose (500 L3/rat), a delay was noted in parasite elimination after ivermectin treatment, with eggs/larvae detected until day 20 after infection when RMOD or A-PC techniques were used for fecal examination (Fig. 3B).
Parasitological profile of the human population
As shown in Table 2, the parasitological study of human population included 68 individuals, of whom 72.1% (n = 49) were female. The age of the participants ranged from 9 to 84 years, with a median age of 47.5 years (interquartile range, 34–59 years). Taking into consideration the results of all the applied parasitological methods (CRS), including RMOD, A-PC, SS, and Helmintex, 6 of 68 individuals evaluated demonstrated Strongyloides sp. larvae in their feces, which corresponded to an estimated prevalence of 8.8%. The parasitological analyses also detected 16 (23.5%) individuals infected with S. mansoni, six (8.8%) infected with Ascaris sp., one (1.5%) case of hookworm infection, and one (1.5%) individual infected with Taenia sp. The fecal examination also revealed intestinal protozoan infection in the study population: 23 individuals (33.8%) had Giardia lamblia cysts in their feces, 10 (14.7%) had Entamoeba coli cysts, and 6 (8.8%) had E. histolytica/dispar. Among the six individuals infected with Strongyloides sp., three were co-infected with other parasites: one presented eggs of S. mansoni and Ascaris sp., one showed only S. mansoni eggs, and the other presented Giardia lamblia cysts. No statistically significant differences were observed in the prevalence of strongyloidiasis with respect to sex and age groups in the study population (Table 2).
Performance of RMOD technique for the diagnosis of Strongyloides stercoralis in naturally infected individuals
As determined by CRS, the overall prevalence of S. stercoralis infection in the study population was 8.82% (6/68). The A-PC and SS techniques showed a sensitivity of 50% (three of the six infected individuals) and 33.3% (two of the six infected individuals), respectively. However, using RMOD, all infected individuals could be diagnosed, thus demonstrating 100% sensitivity among the evaluated individuals. The specific diagnostic of Strongyloides sp. infection was based on morphological features of the larvae found in fecal samples (Schad 1989). This was possible using any of the three parasitological techniques applied in the current study, justifying the high specificity of all parasitological tests. However, it is important to mention that the fecal material obtained after the RMOD procedure was cleaner and much easier to observe under a microscope. Based on the concordance analysis (kappa), a higher probability of detection of strongyloidiasis by the RMOD technique (1.0) than that by A-PC (0.64) and SS (0.48) techniques was noted (Table 3).
As verified in the rat experimental model, the comparative evaluation carried out in the human population showed that the RMOD technique was capable of recovering a higher number of Strongyloides larvae than A-PC from fecal samples of infected individuals. Moreover, all four infected individuals that eliminated less than 1 larvae/g of feces were identified by RMOD, but only one of them was diagnosed using the A-PC method (Fig. 4). In humans, SS was used as a qualitative test to identify Strongyloides larvae and only two of the infected individuals showed positive results, both of them with a higher parasite burden.
Number of larvae of Strongyloides sp. quantified by Rugai modified (RMOD) and agar-plate culture (A-PC) techniques in feces of infected individuals from the community of Vergel do Lago, city of Maceió, Alagoas, Brazil. The number of Strongyloides larvae found in fecal sample of the six infected individual after the analysis by RMOD or A-PC was estimated and plotted as larvae per gram of feces. ND = nondetected
Discussion
The prevalence of strongyloidiasis has been increasing in recent years, both in endemic and nonendemic areas, owing to diagnostic problems, unsatisfactory sanitary measures, and a lack of knowledge about the disease in the population (Puthiyakunnon et al. 2014; Page and Speare 2016). In addition, this infection remains the most neglected among tropical diseases that affect the human population (Olsen et al. 2009; Schär et al. 2013), especially because of the limitations and problems associated with correct diagnosis (Puthiyakunnon et al. 2014; Gelaye et al. 2021). This allows for the persistence of infection and the development of severe cases of strongyloidiasis. Hence, the World Health Organization has recently updated its goals to prioritize control efforts against strongyloidiasis by 2030, implying the development of rapid, sensitive, and easy-to-use diagnostic methods for the mapping and surveillance of this parasitosis (WHO 2020).
For the diagnosis of strongyloidiasis, concentration methods used for detecting Strongyloides larvae in stool samples showed better sensitivity than other parasitological tests. Among these, the Baermann technique is the most commonly used in epidemiological studies and clinical trials (Gelaye et al. 2021). However, this method is laborious and not routinely applied in most clinical laboratories (Requena-Méndez et al. 2013). Based on the principles of the Baermann technique, Rugai et al. (1954) developed a simple method with similar sensitivity to detect strongyloidiasis. The Rugai method uses only a conical cup, gauze, and pipette, which renders its employment easier under field conditions. In our study, we modified some steps of the Rugai technique to improve larval recovery and clean the remaining fecal sediment, thereby increasing the sensitivity of the diagnostic tests. Our data demonstrated that the modifications applied to the RO technique significantly improved the detection of larvae of Strongyloides sp. in fecal samples derived from both experimentally infected rats and naturally infected human individuals. Moreover, the recovered sediment obtained using the RMOD technique was cleaner and easier to evaluate under a light microscope.
The first modification applied to the original Rugai technique included the incorporation of medium-expanded vermiculite into the stool samples, allowing for a more porous fecal mixture, which may facilitate larval migration towards warm water. The feces-vermiculite mixture was not compact, which allowed the evaluation of a large amount of feces, further increasing the sensitivity of this parasitological test. Moreover, the RMOD technique allowed us to qualitatively evaluate diarrheic fecal samples. This addressed a limitation inherent in the original Rugai and Baermann-Moraes tests (Krolewiecki and Nutman 2019), as the expanded vermiculite or granulated charcoal absorbs most of the liquid in diarrheic samples. Another important modification introduced to the original test was an additional filter prepared using a multi-purpose cleaning cloth, a cheap material that allows the migration of parasite larvae while retaining most fecal debris, yielding a less dense sample and favoring the visualization and identification of the larvae. In the current study, a comparative evaluation of the RO and RMOD techniques using the same stool samples from experimentally infected rats demonstrated that the RMOD test recovered a significantly higher number of larvae in a clean, easy-to-analyze sediment.
After confirming that RMOD improved larval recovery and facilitated the analysis of fecal samples from infected rats, we compared the performances of RMOD, A-PC, and SS in the detection and quantification of S. venezuelensis infection in rats experimentally infected with low or high parasite burdens. We also examined the performance of these different parasitological tests as alternatives to evaluate the cure for this parasitic infection after ivermectin treatment. Once again, the experimental data demonstrated a better performance of the RMOD method in the detection and recovery of parasite larvae in all evaluated experimental groups, especially in the infected groups with a low parasite burden.
SS is the most commonly used parasitological diagnostic method in routine laboratories and epidemiological studies due to its low cost, ease of handling, and ability to detect protozoa and helminths in formed, pasty, and semi-pasty samples (Carvalho et al. 2012). However, for using this methodology, the stool sample obtained for analysis is a sediment with a large amount of fecal debris, which hinders proper microscopic examination. Moreover, since the SS technique has no further concentration steps for larvae, this diagnostic test shows low sensitivity for detecting Strongyloides spp. infection, especially because this parasite produces a very low number of larvae (Campo-Polanco et al. 2014). These results were confirmed in our experimental study, especially in rats with a low parasite burden or immediately after anthelmintic treatment.
The A-PC technique is currently considered the most sensitive test for the diagnosis of S. stercoralis, as it allows for the development of the parasite by simulating natural climatic and physicochemical requirements and better visualization of the larvae during analysis (Kaewrat et al. 2020). Despite being used in standard laboratories for the screening of strongyloidiasis cases in endemic countries (Kristanti et al. 2018; Kaewrat et al. 2020), this parasitological method is expensive, requires a long time to obtain results, and is often unable to detect infections with very low parasite burden (Toledo et al. 2015; Ketzis 2017). The present findings, derived from experimental rat infections, indicate that the RMOD approach demonstrated comparable or potentially superior efficacy in detecting Strongyloides sp. larvae when compared to A-PC. Moreover, it offers the advantage of being a more straightforward method in terms of execution and analysis.
Finally, we comparatively evaluated the performance of the parasitological techniques in naturally infected individuals. Apart from the elevated prevalence of intestinal schistosomiasis in the study population, other intestinal parasites were also present, most likely as a consequence of the precarious socioeconomic and sanitary conditions in the study area, favoring the transmission of different parasitic infections (Tamano et al. 2015). As previously discussed, despite allowing the identification of a wide range of parasites present in feces (Carvalho et al. 2012), the SS technique has low sensitivity for the detection of S. stercoralis infection. The Helmintex technique only detected individuals infected with S. mansoni, and the Rugai and A-PC larval concentration methods detected only parasitic larvae in human fecal samples, as previously reported (Campo Polanco et al. 2014; Menezes et al. 2023).
In the current study, the estimated prevalence of 8.8% of strongyloidiasis confirms the results obtained in previous surveys carried out in the State of Alagoas (Paula and Costa-Cruz 2011; Chamone et al. 2020). Additionally, we demonstrated that RMOD presented the best sensitivity for detecting Strongyloides larvae in human fecal samples, followed by A-PC and SS. These findings were in line with our experimental data obtained using S. venezuelensis-infected rats. A previous study in a human population demonstrated that the Baermann and A-PC techniques showed 81% and 58% sensitivity in detecting S. stercoralis larvae, respectively (Krolewiecki et al. 2010). Although the Rugai technique was not performed in that study, the authors confirmed that concentration methods based on hydro- and thermotropism, such as the Baermann and Rugai methods, were more effective in detecting Strongyloides spp. infections. In contrast, another study demonstrated that the A-PC technique was more sensitive to S. stercoralis infection (87.9%), followed by the RO technique (60.6%) and SS (45.4%) (Sitta et al. 2014). However, for both experimental and natural infections, we showed that our modifications to the Rugai technique considerably increased its performance and improved the recovery and detection of Strongyloides larvae.
Although we were able to demonstrate the excellent performance of the RMOD technique in the recovery and detection of Strongyloides larvae compared to other techniques, our study had some inherent limitations, such as the small number of analyzed human stool samples. Another important limitation was the examination of a single fecal sample per resident, which was considered insufficient to exclude S. stercoralis infection because of the sporadic and intermittent elimination of larvae in feces (Siddiqui and Berk 2001). Despite these limitations, the observed prevalence of S. stercoralis infection in the study area corroborates the data in the literature (Paula and Costa-Cruz 2011; Chamone et al. 2020). Moreover, we intend to increase our sampling effort in subsequent studies to further assess the performance of the RMOD method in different human populations.
In conclusion, our results demonstrated that the RMOD technique showed better sensitivity for Strongyloides spp. infections in both experimental models and human populations than other parasitological diagnostic methods. In addition, RMOD is considerably easier to implement in a laboratory setting or under field conditions than the other evaluated methods. The implemented alterations, designed to enhance larval migration and achieve cleaner fecal sediment, are both viable and cost-effective. Furthermore, the RMOD parasitological method can process a large volume of feces (up to 10 g) and requires less time to obtain results than any culture method, such as A-PC. Therefore, the presented data and modifications introduced to the parasitological method of Rugai resulted in better performance and increased the diagnostic sensitivity of the test, which, in our opinion, would allow its use in epidemiological studies and large-scale clinical trials.
Data availability
All the data has been included in the manuscript.
References
Anamnart W, Pattanawongsa A, Intapan PM, Maleewong W (2010) Factors affecting recovery of Strongyloides stercoralis larvae: an approach to a newly modified formalin-ether concentration technique for diagnosis of strongyloidiasis. J Clin Microbiol 48:97–100. https://doi.org/10.1128/jcm.01613-09
Arakaki T, Hasegawa H, Asato R, Ikeshiro T, Kinjo F, Saito A, Iwanaga M (1988) A new method to detect Strongyloides stercoralis from human stool. Jpn J Trop Med Hyg 16:11–17. https://doi.org/10.2149/tmh1973.16.11
Arifin N, Hanafiah KM, Ahmad H, Noordin R (2019) Serodiagnosis and early detection of Strongyloides stercoralis infection. J Microbiol Immunol Infect 52:371–378. https://doi.org/10.1016/j.jmii.2018.10.001
Baek BK, Islam MK, Kim BS, Lim CW, Hur J, Oluoch AO, Kim CH, Kakoma I (2003) Characterization of the protective response against a homologous challenge infection with Strongyloides venezuelensis in rats. Vet Parasitol 113:217–227. https://doi.org/10.1016/s0304-4017(03)00085-2
Buonfrate D, Requena-Mendez A, Angheben A, Cinquini M, Cruciani M, Fittipaldo A, Giorli G, Gobbi F, Piubelli C, Bisoffi Z (2018) Accuracy of molecular biology techniques for the diagnosis of Strongyloides stercoralis infection-a systematic review and meta-analysis. PLoS Negl Trop Dis 12:e0006229. https://doi.org/10.1371/journal.pntd.0006229
Buonfrate D, Bisanzio D, Giorli G, Odermatt P, Fürst T, Greenaway C, French M, Reithinger R, Gobbi F, Montresor A, Bisoffi Z (2020) The global prevalence of Strongyloides stercoralis infection. Pathogens 9:468. https://doi.org/10.3390/pathogens9060468
Campo Polanco L, Gutiérrez LA, Cardona Arias J (2014) Infección por Strongyloides stercoralis: metanálisis sobre evaluación de métodos diagnósticos convencionales (1980–2013). Rev Esp Salud Publica 88:581–600. https://doi.org/10.4321/S1135-57272014000500004
Carvalho GL, Moreira LE, Pena JL, Marinho CC, Bahia MT, Machado-Coelho GL (2012) A comparative study of the TF-Test®, Kato-Katz, Hoffman-Pons-Janer, Willis and Baermann-Moraes coprologic methods for the detection of human parasitosis. Mem Inst Oswaldo Cruz 107:80–84. https://doi.org/10.1590/s0074-02762012000100011
Chamone M, Atuncar G, De Melo A (2020) The prevalence of Schistosoma mansoni is affected by Taenia spp. and soil-transmitted helminths. Int J Res Stud Biosci 8:7–12. https://doi.org/10.20431/2349-0365.0805002
Chaves LA, Gonçalves AL, Paula FM, Silva NM, Silva CV, Costa-Cruz JM, Freitas MA (2015) Comparison of parasitological, immunological and molecular methods for evaluation of fecal samples of immunosuppressed rats experimentally infected with Strongyloides venezuelensis. Parasitology 142:1715–1721. https://doi.org/10.1017/S0031182015001298
Favero V, Frasca Candido RR, De Marco VC, Jones MK, St Pierre TG, Lindholz CG, Da Silva VD, Morassutti AL, Graeff-Teixeira C (2017) Optimization of the Helmintex method for schistosomiasis diagnosis. Exp Parasitol 177:28–34. https://doi.org/10.1016/j.exppara.2017.04.001
Gelaye W, Williams NA, Kepha S, Junior AM, Fleitas PE, Marti-Soler H, Damtie D, Menkir S, Krolewiecki AJ, van Lieshout L, Enbiale W (2021) Performance evaluation of Baermann techniques: the quest for developing a microscopy reference standard for the diagnosis of Strongyloides stercoralis. PLoS Negl Trop Dis 15:e0009076. https://doi.org/10.1371/journal.pntd.0009076
Grove DI (1996) Human strongyloidiasis. Adv Parasitol 38:251–309. https://doi.org/10.1016/s0065-308x(08)60036-6
Hailu T, Nibret E, Amor A, Munshea A (2021) Strongyloides Stercoralis infection in ethiopia: systematic review and meta-analysis on prevalence and diagnostic methods. Helminthologia 58:17–27. https://doi.org/10.2478/helm-2021-0010
Henriquez-Camacho C, Gotuzzo E, Echevarria J, White AC Jr, Terashima A, Samalvides F, Pérez-Molina JA, Plana MN (2016) Ivermectin versus albendazole or thiabendazole for Strongyloides stercoralis infection. Cochrane Database Syst Rev 2016:CD007745. https://doi.org/10.1002/14651858.CD007745.pub3
Hoffman WA, Pons JA, Janer JL (1934) The sedimentation-concentration method in Schistostomiasis mansoni. P R Health Sci J 9:283–291
Kaewrat W, Sengthong C, Yingklang M, Intuyod K, Haonon O, Onsurathum S, Dangtakot R, Saisud P, Sangka A, Anutrakulchai S, Pinlaor S, Cha’on U, Pinlaor P (2020) Improved agar plate culture conditions for diagnosis of Strongyloides stercoralis. Acta Trop 203:105291. https://doi.org/10.1016/j.actatropica.2019.105291
Ketzis JK (2017) Limitations to the adoption of a standardized Strongyloides stercoralis diagnostic method: case study in the Caribbean. Acta Trop 170:178–183. https://doi.org/10.1016/j.actatropica.2017.03.003
Koga K, Kasuya S, Khamboonruang C, Sukhavat K, Ieda M, Takatsuka N, Kita K, Ohtomo H (1991) A modified agar plate method for detection of Strongyloides stercoralis. Am J Trop Med Hyg 45:518–521. https://doi.org/10.4269/ajtmh.1991.45.518
Kristanti H, Meyanti F, Wijayanti MA, Mahendradhata Y, Polman K, Chappuis F, Utzinger J, Becker SL, Murhandarwati EEH (2018) Diagnostic comparison of Baermann funnel, Koga agar plate culture and polymerase chain reaction for detection of human Strongyloides stercoralis infection in Maluku, Indonesia. Parasitol Res 117:3229–3235. https://doi.org/10.1007/s00436-018-6021-5
Krolewiecki A, Nutman TB (2019) Strongyloidiasis: a neglected tropical disease. Infect Dis Clin North Am 33:135–151. https://doi.org/10.1016/j.idc.2018.10.006
Krolewiecki AJ, Ramanathan R, Fink V, McAuliffe I, Cajal SP, Won K, Juarez M, Di Paolo A, Tapia L, Acosta N, Lee R, Lammie P, Abraham D, Nutman TB (2010) Improved diagnosis of Strongyloides stercoralis using recombinant antigen-based serologies in a community-wide study in northern Argentina. Clin Vaccine Immunol 17:1624–1630. https://doi.org/10.1128/CVI.00259-10
Landis JR, Koch GG (1997) An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 33:363–374
Marcos LA, Terashima A, Dupont HL, Gotuzzo E (2008) Strongyloides hyperinfection syndrome: an emerging global infectious disease. Trans R Soc Trop Med Hyg 102:314–318. https://doi.org/10.1016/j.trstmh.2008.01.020
Mejia R, Nutman TB (2012) Screening, prevention, and treatment for hyperinfection syndrome and disseminated infections caused by Strongyloides stercoralis. Curr Opin Infect Dis 25:458–463. https://doi.org/10.1097/QCO.0b013e3283551dbd
Menezes DL, Santos CTJ, Oliveira YLDC, Campos VTC, Negrão-Corrêa DA, Geiger SM, Silva JRS, Jain S, Oliveira LM, Fujiwara RT, Graeff-Teixeira C, Dolabella SS (2023) Accuracy study of Kato-Katz and Helmintex methods for diagnosis of Schistosomiasis mansoni in a moderate endemicity area in Sergipe. Northeast Braz Diagn 13:527. https://doi.org/10.3390/diagnostics13030527
Moraes RG (1948) Contribuição para o estudo do Strongyloides stercoralis e da estrongiloidíase no Brasil. Rev Serv Espec Saude Publica 1:507–624
Negrão-Corrêa D, Souza DG, Pinho V, Barsante MM, Souza AL, Teixeira MM (2004) Platelet-activating factor receptor deficiency delays elimination of adult worms but reduces fecundity in Strongyloides venezuelensis-infected mice. Infect Immun 72:1135–1142. https://doi.org/10.1128/iai.72.2.1135-1142.2004
Negrão-Corrêa D, Pinho V, Souza DG, Pereira AT, Fernandes A, Scheuermann K, Souza AL, Teixeira MM (2006) Expression of IL-4 receptor on non-bone marrow-derived cells is necessary for the timely elimination of Strongyloides venezuelensis in mice, but not for intestinal IL-4 production. Int J Parasitol 36:1185–1195. https://doi.org/10.1016/j.ijpara.2006.05.005
Olsen A, van Lieshout L, Marti H, Polderman T, Polman K, Steinmann P, Stothard R, Thybo S, Verweij JJ, Magnussen P (2009) Strongyloidiasis–the most neglected of the neglected tropical diseases? Trans R Soc Trop Med Hyg 103:967–972. https://doi.org/10.1016/j.trstmh.2009.02.013
Page W, Speare R (2016) Chronic strongyloidiasis - don’t look and you won’t find. Aust Fam Physician 45:40–44
Paula FM, Costa-Cruz JM (2011) Epidemiological aspects of strongyloidiasis in Brazil. Parasitology 138:1331–1340. https://doi.org/10.1017/s003118201100120x
Puthiyakunnon S, Boddu S, Li Y, Zhou X, Wang C, Li J, Chen X (2014) Strongyloidiasis–an insight into its global prevalence and management. PLoS Negl Trop Dis 8:e3018. https://doi.org/10.1371/journal.pntd.0003018
Requena-Méndez A, Chiodini P, Bisoffi Z, Buonfrate D, Gotuzzo E, Muñoz J (2013) The laboratory diagnosis and follow up of strongyloidiasis: a systematic review. PLoS Negl Trop Dis 7:e2002. https://doi.org/10.1371/journal.pntd.0002002
Rugai E, Mattos T, Brisola AP (1954) Nova técnica para isolar larvas de nematóides das fezes: modificações do método de Baermann. Rev Adolfo Lutz 14:5–8
Schad GA (1989) Morphology and life history of Strongyloides stercoralis. In: Grove I (ed) Strongyloidiasis: a major roundworm infection of man. Taylor and Francis Ltd, London, pp 85–104
Schär F, Trostdorf U, Giardina F, Khieu V, Muth S, Marti H, Vounatsou P, Odermatt P (2013) Strongyloides stercoralis: global distribution and risk factors. PLoS Negl Trop Dis 7:e2288. https://doi.org/10.1371/journal.pntd.0002288
Schilter HC, Pereira AT, Eschenazi PD, Fernandes A, Shim D, Sousa AL, Teixeira MM, Negrão-Corrêa D (2010) Regulation of immune responses to Strongyloides venezuelensis challenge after primary infection with different larvae doses. Parasite Immunol 32:184–192. https://doi.org/10.1111/j.1365-3024.2009.01176.x
Siddiqui AA, Berk SL (2001) Diagnosis of Strongyloides stercoralis infection. Clin Infect Dis 33:1040–1047. https://doi.org/10.1086/322707
Sitta RB, Malta FM, Pinho JR, Chieffi PP, Gryschek RC, Paula FM (2014) Conventional PCR for molecular diagnosis of human strongyloidiasis. Parasitology 141:716–721. https://doi.org/10.1017/S0031182013002035
Takamure A (1995) Migration route of Strongyloides venezuelensis in rodents. Int J Parasitol 25:907–911. https://doi.org/10.1016/0020-7519(95)00014-s
Tamano LTO, Araujo DM, Lima BBC, Silva FNF, Silva J (2015) Socioeconomia e saúde dos pescadores de Mytella falcata da Lagoa Mundaú, Maceió-AL. Bol Mus Para Emílio Goeldi Cienc Hum 10:699–710. https://doi.org/10.1590/1981-81222015000300011
Toledo R, Muñoz-Antoli C, Esteban JG (2015) Strongyloidiasis with emphasis on human infections and its different clinical forms. Adv Parasitol 88:165–241. https://doi.org/10.1016/bs.apar.2015.02.005
Vadlamudi RS, Chi DS, Krishnaswamy G (2006) Intestinal strongyloidiasis and hyperinfection syndrome. Clin Mol Allergy 4:8. https://doi.org/10.1186/1476-7961-4-8
Viney ME, Lok JB (2007) Strongyloides spp. WormBook 23:1–15. https://doi.org/10.1895/wormbook.1.141.1
Viney ME, Lok JB (2015) The biology of Strongyloides spp. WormBook 16:1–17. https://doi.org/10.1895/wormbook.1.141.2
WHO (World Health Organization) (2020) Ending the neglect to attain the Sustainable Development Goals: a road map for neglected tropical diseases 2021–2030: overview. WHO, Geneva, Switzerland. https://apps.who.int/iris/handle/10665/332094. Liense: CC BY-NC-SA 3.0 IGO. Accessed 22 May 2022
WHO (World Health Organization) (2022) Soil-transmitted helminth infections. WHO, Geneva, Switzerland. https://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections. Accessed 30 Jan 2022
Acknowledgements
We are grateful for the assistance of José Carlos and Elizabeth De Lacorte for the technical support provided.
Funding
The experimental work received financial support from the “Fundação de Amparo à Pesquisa do Estado de Alagoas, PPSUS”: Edital Saúde/Decit-SCTIE-MS/CNPq/FAPEAL/SESAU-AL process # EFP_00023144, and “Conselho Nacional de Desenvolvimeto Científico e Tecnológico—CNPq” for research in neglected tropical diseases, Edital CNPq/MS-SCTIE-DECIT process CNPq #442994/2019–2. DN-C is recipient of CNPq-Research Fellowship.
Author information
Authors and Affiliations
Contributions
JGMR and DAN-C: conceptualization. JGMR, GSM, GMAC, VFR, JKAOS, CBGG, and DAN-C: performed experiments. JGMR, WJNP, and FSW: field collection. JGMR, GSM, GMAC, VRF, JKAOS, CBGG, WJNP, FSW, SMG, and DAN-C: data analysis. JGMR and DAN-C: supervision and project administration. JGMR, GSM, GMAC, WJNP, FSW, SMG, and DAN-C: writing and editing the original draft. All the authors reviewed and approved the final version of this manuscript.
Corresponding author
Ethics declarations
Ethics approval
All experimental procedures performed in rats were approved by the Ethics Committee for Animal Use (CEUA/UFMG), under protocol number 129/2020. The human study protocol was approved by the local Ethics Committee for Human Research (COEP) and registered on the Brazilian Platform for Research with Human Subjects (Plataforma Brasil) under the number CAAE#55239522.3.0000.5149.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Disclaimer
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional information
Section Editor: David Bruce Conn
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rodrigues, J.G.M., Miranda, G.S., Camelo, G.M.A. et al. Modifications to the parasitological technique of Rugai increase the diagnostic sensitivity for strongyloidiasis. Parasitol Res 123, 101 (2024). https://doi.org/10.1007/s00436-023-08111-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00436-023-08111-y