Abstract
Trichomonas vaginalis (T. vaginalis) is the most prevalent sexually transmitted infection (STI) globally. Metronidazole is the drug of choice for treating T. vaginalis infections although metronidazole-resistant T. vaginalis has been reported in clinical isolates. The purpose of this study was to determine the presence of mutations in nitroreductase genes associated with metronidazole resistance in vaginal swabs testing positive for T. vaginalis. This study included 385 human immunodeficiency virus (HIV)-positive pregnant women. Vaginal swabs were collected from consenting pregnant women and used for the detection of T. vaginalis using the TaqMan assay. From the vaginal swabs, nitroreductase genes ntr4 and ntr6 containing mutations associated with metronidazole resistance were amplified using a quantitative polymerase chain reaction (PCR) assay. To validate the PCR assay, T. vaginalis cultured isolates with known metronidazole resistance profiles were used as controls in the mutation detection assays. The prevalence of T. vaginalis in the study population was 12.2% (47/385). Mutations associated with resistance to metronidazole were detected in more than 40% of the samples tested, i.e. 21/47 (45%) and 24/47 (51%) for ntr4 and ntr6, respectively. A total of 19 samples (40%) carried mutations for both ntr4 and ntr6 genes associated with metronidazole resistance. The validation assays showed a positive correlation between phenotypic and genotypic resistance profiles. This study found a high prevalence of mutations associated with metronidazole resistance. This is concerning since metronidazole is currently used in the syndromic management of STIs in South Africa. Molecular-based assays for monitoring metronidazole resistance profiles using nitroreductase genes may serve as a feasible method for antimicrobial surveillance studies for T. vaginalis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trichomonas vaginalis is the parasitic protozoan causing the sexually transmitted infection (STI) trichomoniasis and is the most common and prevalent non-viral STI worldwide (Kissinger 2015a). The World Health Organization (WHO) estimated 142 million cases of T. vaginalis among adults (16–45 years of age) globally in 2016, with sub-Saharan Africa (SSA) having the highest incidence (Organization 2016). The last estimated annual incidence of T. vaginalis worldwide exceeds that of chlamydia, gonorrhoea, and syphilis combined (Kissinger 2015b; Organization 2018). However, T. vaginalis is currently not a reportable disease and the true estimation of disease prevalence is not currently known (Van Der Pol et al. 2021).
In South Africa, the prevalence of T. vaginalis infection among pregnant women ranges between 4.8 and 59.6% (Dessai et al. 2020; Green and Taleghani 2020; Joseph Davey et al. 2018, 2019; Mabaso et al. 2020; Medina-Marino et al. 2020; Moodley et al. 2015; Morikawa et al. 2018; Mudau et al. 2018; Nyemba et al. 2021; Peters et al. 2021; Price et al. 2018; Smullin et al. 2020). Asymptomatic T. vaginalis infections are well documented; approximately 50 to 60% of infected women do not show clinical signs (Bouchemal et al. 2017; Mudau et al. 2018; Vallely et al. 2017). Among women, common sites of infection include the vagina, urethra, and endocervix (Kissinger 2015a). Furthermore, symptomatic women are more likely to experience clinical manifestations, including green or yellow vaginal discharge, vaginal odour, dysuria, vulvar irritation, itching, lower abdominal pain, strawberry cervix, and inflammation (Bosserman et al. 2011; Kissinger 2015a).
T. vaginalis has been reported be associated with several health complications including pelvic inflammatory disease (PID), poor pregnancy outcomes, cervical cancer, prostatitis, and infertility (Akbari and Matini 2017; Masha et al. 2019; Price et al. 2018; Silver et al. 2014). Poor pregnancy outcomes include premature rupture of membranes, low birthweight, preterm delivery, and neonatal death (Kissinger 2015b; Mudau et al. 2018; von Glehn et al. 2017). Furthermore, T. vaginalis can also be transmitted to new-born babies during delivery via the birth canal (Akbari and Matini 2017; Kissinger 2015b). Coinfection of T. vaginalis with other STIs has been previously reported (Ginocchio et al. 2012; Joseph Davey et al. 2018). T. vaginalis infection has also been shown to increase the risk of acquisition and transmission of human immunodeficiency virus (HIV) by 50% via several mechanisms, including damage to the vaginal epithelial membrane by the protozoa (Joseph Davey et al. 2019; Kissinger 2015b; Masha et al. 2019). T. vaginalis have been reported to be associated with several risk factors such as older age, sexual behaviour, intravenous drug use, trading sex for goods, commercial sex work, smoking cigarettes, use of oral contraceptives, socioeconomic status, and phase of menstrual cycle (Kissinger 2015a). In women from Africa, older age, marital status, multiple sex partners, a greater number of lifetime sexual partners, poor hygiene, and socioeconomic status have been shown to be risk factors associated with T. vaginalis infection (Joseph Davey et al. 2018; Naidoo et al. 2014).
Resistance to metronidazole in the sexually transmitted parasite T. vaginalis is a public health concern (Kissinger et al. 2018; Marques-Silva et al. 2021). The WHO and the US Centers for Disease Control and Prevention (CDC) recommend a single 2-g dose of oral metronidazole or tinidazole as first-line treatment and a 7-day dose of oral metronidazole (400 mg or 500 mg twice daily for 7 days) as second-line treatment for T. vaginalis infections (Kissinger 2015b; Workowski 2015). However, since metronidazole is generic and affordable, it is primarily used to treat T. vaginalis infections in many settings (das Neves et al. 2020; Marques-Silva et al. 2021). Currently, the management and diagnosis of T. vaginalis infection in South Africa are based on WHO guidance, using a syndromic approach (Health and Africa, 2015; Organization, 2016). According to South African guidelines, trichomoniasis is characterised by abnormal vaginal discharge, which is treated with a 2 g stat of metronidazole (which is safe to be used in all trimesters of pregnancy) (Health and Africa, 2015). Moreover, emerging nitroimidazole-resistant trichomoniasis is concerning, since few alternatives to standard therapy exist (Alessio and Nyirjesy 2019; Ghosh et al. 2018).
To date, the exact mechanisms of metronidazole resistance in T. vaginalis remain unknown and little is known about its molecular basis (Kissinger 2015a). However, it is assumed that it may be due to several mutations in selected targets (Paulish-Miller et al. 2014).
Several studies have reported various factors that modulate metronidazole resistance in T. vaginalis such as downregulation of pyruvate-ferredoxin oxidoreductase (PFOR) enzyme activity in anaerobic resistance (Kulda 1999; Land et al. 2001); transcription of ferredoxin enzyme activity reduction in resistant T. vaginalis strains in aerobic resistance (Bradic et al. 2017; Yarlett et al. 1986); decreased expressions of flavin reductase; and the downregulation of nitroreductase genes (ntr4 and ntr6) (Bradic et al. 2017; Leitsch et al. 2014). The purpose of this study was to determine the presence of mutations in nitroreductase genes associated with metronidazole resistance in T. vaginalis without the need to culture.
Methods
Ethical statement
Ethics approval for this study (BREC/00001382/2020) was obtained from the Biomedical Research Ethics Committee (BREC), University of KwaZulu-Natal.
Study setting and population
The study was a cross-sectional study of pregnant women attending the antenatal clinic (ANC) at the King Edward VIII Hospital in Durban, South Africa. At the clinic, women were educated on the consequences of STIs during pregnancy and provided with information on risk reduction for STIs. The clinic attends to 80 to 100 women on a daily basis, and the recruitment for this study took place between October 2020 and April 2021. Women were enrolled in this study if they were HIV positive, 18 years and older, willing to provide written informed consent, vaginal swab samples, and socio-demographic, behavioural, and clinical data. The swab samples were self-collected, and the women were provided with instructions on proper sample collection. Each enrolled woman provided self-collected vaginal swabs (dry swabs) for detection of vaginal infections. The consenting women had also completed a questionnaire on socio-demographic, behavioural, and clinical factors.
Laboratory procedures
Sample processing
After collection, the dry swabs were placed in 2 ml of phosphate buffered saline (PBS). The solution was vortexed to dislodge the cells from the swabs, and the swab was discarded. The suspension was stored at − 20 °C for further molecular analysis.
DNA extraction
DNA extraction was performed on the vaginal swab suspension using the PureLink Microbiome Kit (ThermoFisher Scientific, USA), according to the manufacturer’s instructions. Briefly, 2 ml of the vaginal fluid samples was centrifuged for 30 min at 14,000 × g. The supernatant was discarded and 800 µl of S1 lysis buffer was added to the pellet and pipetted up and down to mix the sample. The sample was then transferred to the bead tube and 100 µl of S2 lysis enhancer was added to the bead tube, capped, and vortexed briefly. This was incubated at 95 °C for 10 min, followed by vortexing at a maximum speed for 7 min, and further centrifuged at 14,000 × g for 1 min. Thereafter, 500 µl of the supernatant was transferred to a clean microcentrifuge tube, avoiding the bead pellet and any cell debris.
To bind DNA to the column, 900 µl of binding buffer was added and vortexed briefly. Following this, 700 µl of the sample mixture was loaded onto a spin column-tube and centrifuged at 14,000 × g for 1 min. The flow through was discarded and the spin column was centrifuged at 14,000 × g for 30 s. The spin column was placed in a clean tube and 50 µl of elution buffer was added, and the tube was incubated at room temperature for 1 min. After 1 min, the spin column was centrifuged at 14,000 × g for 1 min. The concentration of the extracted DNA was determined using the Nanodrop Spectrophotometer (ThermoFisher Scientific, USA). DNA samples were stored at − 20 °C until further molecular analysis. The molecular assays were conducted at the School of Clinical Medicine Research Laboratory at the University of KwaZulu-Natal.
Detection of T. vaginalis from vaginal swab DNA extracts
T. vaginalis was detected using the TaqMan Real-time PCR (sensitivity) assay (ThermoFisher Scientific, USA) using commercially available primers and probes specific for T. vaginalis (Pr04646256_S1). The assay targets the alpha tubulin 1 gene of from this pathogen. Each PCR reaction was performed in a final volume of 20 µl comprising 1 µl FAM-labelled probe/primer mix, 5 µl Fast Start 4 × probe master mix (ThermoFisher, Part No. 4444434), 2 µl template DNA, and 12 µl nuclease-free water. PCR amplification was performed on the Quant Studio 5 real-time PCR detection system (ThermoFisher Scientific, USA), in a 96-well microtiter reaction plate. Amplification was performed at 95 °C for 30 s followed by 45 cycles comprising of denaturation at 95 °C for 3 s and annealing at 60 °C for 30 s. Detection of amplified fluorescent products was carried out at the end of the annealing phase. The raw fluorescent data that included the CT mean values were automatically generated by the Quant Studio 5 Real-time PCR system software.
Molecular detection of genes associated with metronidazole resistance
Genes (ntr4 and ntr6) associated with resistance to metronidazole were amplified by quantitative PCR, using specific primers described by Paulish-Miller et al. (2014) (Table 1) on the extracted vaginal swab DNA. The primer and probe sequences which contain the mutations associated with resistance to metronidazole are listed in Table 1. Each PCR reaction was performed in a final volume of 10 µl comprising 5ul Taqman master mix (ThermoFisher Scientific, USA), 10 µM (0.5 µl each) of forward and reserve primer, 0.5 µl probe FAM (wild type) and VIC (mutant), 1 µl template DNA, and 2 µl nuclease-free water. PCR amplification was performed on the Quant Studio 5 real-time PCR detection system (ThermoFisher Scientific, USA), in a 96-well microtiter reaction plate. The cycling conditions comprised of a UDG activation stage for 2 min at 50 °C, initial denaturation for 2 min at 95 °C, followed by 40 cycles consisting of denaturation for 15 s at 95 °C, annealing 15 s at 60 °C with extension for 1 min at 72 °C. To assess any contamination of the PCR, a negative control was included in all PCR runs. Detection of amplified fluorescent products was carried out at the end of the extension phase. The raw fluorescent data that included the Ct mean values were automatically generated by the Quant Studio 5 Real-time PCR system software. The wild-type probes were labelled with FAM and the mutant probes were label with VIC.
Control assays
Sub-culture of stored T. vaginalis clinical isolates
T. vaginalis isolates which were stored at − 80 °C were sub-cultured and metronidazole susceptibility assays were performed on the isolates. Sub-culture was performed by transferring 500 μl of the culture into 5-ml fresh Diamond’s TYM medium supplemented with amikacin, amphotericin B, ampicillin, chloramphenicol, ciprofloxacin, and vancomycin at 48-h intervals until non- contaminated axenic cultures were obtained. Once axenic cultures were obtained, metronidazole susceptibility assays and DNA extraction were performed.
Metronidazole susceptibility assay
Metronidazole susceptibility was performed in 96-well flat-bottomed microtiter plates under anaerobic incubation conditions. Twofold serial dilutions of metronidazole were performed in Diamond’s TYM medium. The resulting concentrations ranged from 0.25 to 16 μg/ml. T. vaginalis cultures were then standardised to an inoculum of 1.5 × 104 trichomonads/well. Each T. vaginalis isolate inoculum was then added into each well excluding the ATCC control wells. The T. vaginalis ATCC 50,148 strain was used as a control strain and untreated cultures of the respective isolates were used as growth controls. Plates were incubated in air-tight anaerobic jars containing Oxoid™ AnaeroGen™ 2.5-L gas pack (ThermoFisher Scientific, USA) and Oxoid™ Resazurin Anaerobic indicator strip (ThermoFisher Scientific, USA) at 37 °C for 48 h. T. vaginalis motility and growth were assessed using the inverted microscope at × 400 magnification.
T. vaginalis growth and motility were scored according to the scoring criteria described by Upcroft (Upcroft and Upcroft 2001). Trophozoite numbers were scored 1 + (0–10 motile parasites; not more than 20% coverage of well surface and significantly less active), 2 + (20 to 50% coverage of the well surface and some trophozoite motility), 3 + (more than 50% coverage of the well surface, almost confluent growth with much motility), and 4 + (confluent growth with full motility) (Upcroft and Upcroft 2001). The minimum inhibitory concentration (MIC) was defined as the lowest concentration of metronidazole in which a score of 1 + was observed after 48 h of incubation. Breakpoints suggested by Upcroft were used (Upcroft and Upcroft 2001). MIC ≤ 1 μg/ml was considered susceptible, MIC = 2 μg/ml was considered intermediate (low-level resistance), and MIC ≥ 4 μg/ml was considered resistant (Upcroft and Upcroft 2001). All experiments were performed in triplicate for each T. vaginalis isolate.
DNA extraction from T. vaginalis isolates
DNA was extracted from the T. vaginalis isolates using the phenol–chloroform method (Shaio et al. 1997). Briefly, T. vaginalis cells were washed twice in phosphate-buffered saline (pH 7.4) by centrifugation at 1500 × g for 10 min. DNA was extracted from the cell pellets by adding 500 μl of lysis buffer and incubated at 65 °C for 30 min. The lysis buffer was prepared from concentrated stock solutions to obtain final concentrations of 100 μg of proteinase K, 450 mM NaCl, 15 mM sodium citrate, and 0.2% sodium dodecyl sulphate (SDS) per ml. The extracted DNA was then purified twice by adding an equal volume of phenol–chloroform (1:1; vol/vol) and centrifuged at 1500 × g for 10 min. DNA was then purified once with chloroform only. DNA extracts were then precipitated with 2 volumes of 95% ethanol (vol/vol) and 0.1 volume of 3 M sodium acetate (pH 5.2). The DNA pellets were then washed with 70% (vol/vol) ethanol, air-dried at room temperature, and dissolved in 50 μl of TE buffer. The concentration and purity of the extracted DNA was measured using the NanoDrop Spectrophotometer (ThermoFisher Scientific, USA).
Detection of nitroreductase genes from T. vaginalis cultured isolates
Nitroreductase genes (ntr4 and ntr6) associated with resistance to metronidazole were amplified by quantitative PCR, using specific primers described by Paulish-Miller et al. (2014) (Table 1) on the extracted cultured genomic DNA. Each PCR reaction was performed in a final volume of 10 µl comprising 5ul Taqman master mix (ThermoFisher Scientific, USA), 10 µM (0.5 µl each) of forward and reserve primer, 0.5 µl probe, 1 µl template DNA, and 2 µl nuclease-free water. PCR amplification was performed on the Quant Studio 5 real-time PCR detection system (ThermoFisher Scientific, USA), in a 96-well microtiter reaction plate. The cycling conditions comprised of a UDG activation stage for 2 min at 50 °C, initial denaturation for 2 min at 95 °C, denaturation for 15 s at 95 °C, annealing 15 s at 60 °C with extension for 1 min at 72 °C. To assess any contamination of the PCR, a negative control was included in all PCR runs. Detection of amplified fluorescent products was carried out at the end of the extension phase. The raw fluorescent data that included the Ct mean values were automatically generated by the Quant Studio 5 Real-time PCR system software. The wild-type probes were labelled with FAM and the mutant probes were label with VIC.
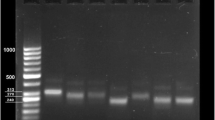
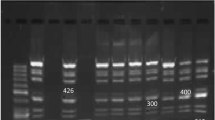
To confirm the identity of the PCR products, conventional PCR was performed on the samples using the ntr4 and ntr6 PCR primers only. The amplification reactions were performed in PCR with a total volume of 25 µl. The reaction contained 12.5 µl DreamTaq master mix (ThermoFisher Scientific, MA, USA), 9.5 µl distilled water, 0.5 µl of each primer (reverse and forward), and 2 µl of template DNA was used. The negative control contained 23 µl of PCR mixture and 2 µl of distilled water. Thereafter, the PCR tubes were placed into the thermal cycler and the following conditions were performed, for gene amplification initial denaturation at 95 °C for 5 min, thereafter 35 cycles: of 95 °C 30 s, annealing 60 °C for 1 min, elongation 72 °C for 1 min, and final elongation at 72 °C for 5 min.
The amplicons were sequenced in one direction using the Sanger approach. The sequencing was performed on an ABI3500XL genetic analyser at Inqaba Biotechnical Industries (Hatfield, Pretoria, South Africa). The ABI sequencing files were edited on CHROMAS (Technelysium, Queensland, Australia).
Data analysis
The statistical data analysis was conducted in a freely available Statistical Computing Environment, R software, version 3.6.3 using the RStudio platform. The population characteristics were described using frequency distribution. All the tests were conducted at 5% level of significance.
Results
Detection of T. vaginalis from vaginal swab samples
Of the 385 samples tested in this study, 47 samples were positive for T. vaginalis.
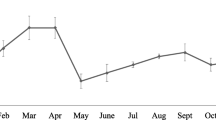
The prevalence of T. vaginalis among the HIV-positive women was 12.2% (47/385). The Ct values of the amplified samples are shown in supplementary Table 1. According to the Ct values, using a cut-off value of 25 for distinguishing low and high positives (< 25 high positives, > 25 low positives), 16 samples were high positives (Ct: < 25), and 31 samples were low positives (Ct: > 25).
Characteristics of the study women who tested positive for T. vaginalis
Educational level was significantly associated with being T. vaginalis positive (p < 0.001), most women reported attending high school, 85.1% when compared to 14.9% who attended college. Other characteristics significantly associated with testing positive for T. vaginalis included employment status, marital status, having a regular sex partner, age of first sex, lifetime sex partners, partner having other partners, condom use, partner having symptoms of STIs, trimester of pregnancy, previously treated for STIs, intravaginal practices, and risk of contracting STIs. Of the women who tested T. vaginalis positive, 78.7% of the women were unemployed when compared to 21.3% who reported being employed, p < 0.001. A higher proportion of positive women, 91.5% were unmarried when compared to 8.5% who reported being married, p < 0.001. Most women (93.6.0%) reported having a regular sex partner, compared to 6.4% who reported not having a regular sex partner, p < 0.001. The majority of the positive women had experienced their first sex between the ages of 15 and 20 years of age (63.8%) when compared to 34.0% of the women who had their first sex at older than 21 years of age, and 2.1% of the women had their first sex younger than 15 years of age, p < 0.001. The majority of the positive women reported having 2–4 lifetime sex partners (55.3%) when compared to 25.5% of the women who reported having greater than 4 lifetime sex partners, and 19.1% of the women reported having 1 lifetime sex partner, p = 0.005. The majority of the positive women reported not knowing if their partners had other partners (57.4%) when compared to 23.4% of the women who reported that their partners did not have other partners, and 19.2% of the women reported that their partners had other partners, p = 0.002. In addition, 72.3% of the women had reported not using condoms during sex when compared to 22.7% who used condoms during sex, p = 0.002. The majority of women reported that their partners did not have symptoms of STIs, 83.0% when compared to 17.0% who reported that their partners had symptoms of STIs, p < 0.001. The majority of the positive women were in their third trimester of pregnancy (73.9%) when compared to 23.9% of the women who were in their second trimester of pregnancy, and 2.2% of the women who were in their first trimester of pregnancy, p < 0.001. Most women who tested positive for T. vaginalis reported not being previously treated for STIs (66.0%) when compared to 34.0% who reported being previously treated for STIs, p = 0.029. Most women who tested positive for T. vaginalis reported not engaging in intravaginal practices such as douching, 97.9% when compared to 2.1% who reported such practices, p < 0.001. The majority of positive women reported being at risk of contracting STIs (68.1%) when compared to 31.9% who reported not being at risk of contracting STIs, p = 0.013 (Table 2).
Detection of mutations associated with metronidazole resistance in control isolates
The control assays were used as validation assays before proceeding to the detection of mutations associated with resistance in the uncultured swabs. The sequencing of the ntr4 and ntr6 PCR amplicons showed a 99% identity with T. vaginalis G3 nitroreductase family protein (Sequence ID: XM_001307905).
The susceptibility assays which were performed on the stored isolates revealed the presence of two drug-resistant isolates (Table 3). To confirm the presence of mutations associated with the resistant phenotype, metronidazole susceptible (n = 2) and resistant isolates (n = 2) were subjected to the amplification assays. According to the analysis, the presence of mutations in the ntr4 and ntr6 genes associated with resistance was detected in the resistant isolates and no amplification was observed in the susceptible isolates. This showed a link between phenotypic and genotypic resistance profiles (Table 3).
Detection of mutations associated metronidazole resistance
The Ct values of the samples testing positive for mutations and wild types associated with metronidazole resistance and metronidazole susceptible respectively are shown in Supplementary Table 2. The ntr4 gene carrying the C213G mutation associated with metronidazole resistance was shown to be present in 21/47 samples (45%). The ntr6 gene with the A238T mutation associated with metronidazole resistance was shown to be in 24/47 (51%) of the samples. A total of 19 samples (40%) carried mutations for both ntr4 and ntr6 (Table 4).
The ntr4 gene lacking the C213G mutation (wild type) was shown to be present in 27/47 samples (57%) and the ntr6 gene lacking the A238T mutation was shown to be in 25/47 (53%) samples. Since the study was aimed at detecting resistance profiles from the primary vaginal swab, certain clinical samples contained both mutant and resistant genotypes and this was expected.
Clinical factors associated with metronidazole resistance mutations compared with no metronidazole resistance mutations in any genes
Table 5 provides an overview of clinical factors associated with samples that had metronidazole resistance mutations in both genes compared to samples that had no metronidazole resistance mutations in any of the genes. Of the women who displayed resistance mutations for both genes, 54% reported not having current symptoms of STIs such as discharge, vaginal odour, vaginal itching, genital sore/ulcers, genital warts, and pain during urination and 46% reported having symptoms of STIs. Of the women who displayed no resistance mutations in any genes, 62% reported not having current symptoms of STIs when compared to 38% who reported having STI symptoms.
Of the women who displayed resistance mutations in both genes, 88% reported that their sexual partners did not have symptoms of STIs such as testicular pain, pain during urination, and discharge from the penis and 12% reported that their sexual partners did have symptoms of STIs. For the women who displayed no resistance mutations in any genes, a higher proportion (76%) reported that their sexual partners did not have symptoms of STIs whilst 24% reported that their sexual partners did have symptoms of STIs.
Of the women with resistance mutations in both genes, 77% reported had not been previously treated for STIs when compared to 23% who reported having been previously treated for STIs. For the women who displayed no resistance mutations in any genes, 52% had not been previously treated for a STI when compared to 48% who were treated in the past.
With respect to gestational age, of the women with resistance mutations in both genes, 4% and 15% were on their 1st and 2nd trimesters of pregnancy and 81% of women were in their 3rd trimesters of pregnancy. For the women who displayed no resistance mutations in any genes, 33% and 67% of the women were in their 2nd and 3rd trimesters of pregnancy.
Discussion
Metronidazole is the first line of treatment for T. vaginalis infections globally (Kissinger, 2015a). However, growing metronidazole resistance in T. vaginalis infections has emerged as a public health concern with long-term health consequences (Bouchemal et al. 2017; Kissinger 2015a; Marques-Silva et al. 2021). In South Africa, metronidazole is used in the syndromic management for the treatment of vaginal discharge syndrome for both the general population and pregnant women (Health and Africa, 2015). This is especially concerning for pregnant women since resistant T. vaginalis infections can have serious consequences for reproductive health, such as an increased risk of HIV and other STIs, as well as perinatal morbidity. Recent metronidazole resistance research studies conducted in South Africa have focused primarily on culture-based approaches rather than molecular-based methods for detecting metronidazole resistance profiles in T. vaginalis (Mabaso and Abbai 2021; Rukasha et al. 2013). Additionally, to our best knowledge, this is the first study in our setting to investigate mutations in nitroreductase genes associated with metronidazole resistance using molecular-based methods on uncultured vaginal swabs in HIV-positive pregnant women.
In this study, the prevalence of T. vaginalis among the HIV-positive women was 12.2%. This prevalence is in accordance with other studies that have been conducted in South Africa among HIV-positive pregnant women (Joseph Davey et al. 2018, 2019; Nyemba et al. 2021). The prevalence of T. vaginalis is diverse and depends on various factors. Herein, the factors that were significantly associated with the prevalent infection included attending high school only, being unemployed, being unmarried, not having a regular sex partner, age of first sex between 15 and 20 years of age, having 2–4 lifetime sex partners, partner having other partners, not using a condom, partner having symptoms of STIs, trimester of pregnancy, being previously treated for STIs, intravaginal practices, and risk of contracting STIs. Similar findings have been reported elsewhere (Joseph Davey et al. 2018; Kissinger 2015a).
Nitroreductase genes have been reported to be associated with metronidazole resistance (Ozcelik et al. 2018; Paulish-Miller et al. 2014). According to Ozcelik et al. (2018), the presence of ntr4 and ntr6 was associated with metronidazole resistance in T. vaginalis and categorised as low (MLC, 50 to 100 μg/ml), moderate (MLC, 200 μg/ml), or high (MLC, ≥ 400 μg/ml) (Ozcelik et al. 2018). In the current study, MIC ≤ 1 μg/ml was considered susceptible, MIC = 2 μg/ml was considered intermediate (low-level resistance), and MIC ≥ 4 μg/ml was considered resistant. In addition, the current study included a mini-validation assay in which the presence and absence of mutations were linked to susceptibility patterns of metronidazole. For the mini-validation assay, TaqMan primers and probes specific for the SNPs associated with the mutations were used. For the susceptible isolates, TV171 and TV184, there was no amplification observed for the presence of ntr4 or ntr6. However, for the resistant isolates, TV253 and TV270, amplification for both ntr4 and ntr6 was observed (Table 3). The validation assays performed in this study showed a positive correlation between phenotypic and genotypic resistance profiles. Therefore, our findings are similar to that of Ozcelik et al. (2018). After having performed the validation assays, the presence of the mutations was determined in the clinical samples. In this study, mutations in ntr4 associated with resistance to metronidazole were detected in 45% of the samples and mutations in ntr6 were detected in 51% of the samples. In addition, 40% of the samples carried mutations for both ntr4 and ntr6 genes.
A study conducted among women attending gynaecology services in Turkey reported a prevalence of 33% for metronidazole-resistant T. vaginalis samples (Ozcelik et al. 2018). That study employed both conventional and molecular approaches to detect metronidazole resistance. A second Turkish study reported a prevalence of 7.5% for metronidazole-resistant T. vaginalis (Ertabaklar et al. 2016). Similarly, a study conducted in South Africa in T. vaginalis isolates obtained from HIV-positive women reported a low prevalence 6% of T. vaginalis metronidazole resistance by culture methods (Rukasha et al. 2013). In addition, Matini et al.(2016) and Ghosh et al. (2018) reported a low prevalence of metronidazole resistance, 2% (1/50) and 8% (8/100) in clinical isolates of T. vaginalis respectively (Ghosh et al. 2018; Matini et al. 2016). The prevalence estimates of metronidazole-resistant T. vaginalis in the USA ranged from 4.3 to 66% (Bosserman et al. 2011; Kirkcaldy et al. 2012; Krashin et al. 2010; Schwebke and Barrientes 2006). A study conducted in Egypt by Abdel-Magied et al. (2017a, b) among symptomatic and asymptomatic women showed a 8.2% prevalence for metronidazole resistance (Abdel-Magied et al. 2017a). Furthermore, Abdel-Magied et al. (2017a, b) assessed in vitro resistance among 30 Egyptian T. vaginalis-positive cases between March 2014 and February 2016 with treatment failure and reported that all isolates, 100% were resistant to metronidazole (Abdel-Magied et al. 2017b). Another two studies that have been conducted in Egypt reported metronidazole resistance prevalence of 0% and 7.7%, respectively (Hussien et al. 2004; Mohamed et al. 2019). All of the studies described above have investigated metronidazole resistance using culture. There is a lack of studies that have determined metronidazole resistance profiles from the molecular level using non-culture methods. The data presented in the current study now reports novel information.
In the current study, the link between clinical factors and metronidazole resistance mutations was determined. According to the findings, most women who carried metronidazole resistance mutations did not present with symptoms of genital infections at enrollment, i.e. they were asymptomatic and would have not been managed by the syndromic approach. The lack of management may lead to the infected women transmitting the infection to their unborn baby or sex partner. A low proportion of women who carried metronidazole resistance mutations had been previously treated for STIs in the past by syndromic management. The lack of diagnosis before treatment initiation using this approach could have contributed to the observed metronidazole resistance mutations. The high proportion of the women who carried metronidazole resistance mutations were in their last trimester of pregnancy. If these infections persist, they can be passed onto their unborn child and have severe neonatal consequences. This study reinforces the need for laboratory diagnosis in order to identify the causative pathogens and antimicrobial surveillance of the pathogens.
Conclusion
The majority of studies that have been conducted focus on the detection of metronidazole resistance using culture-based methods, which explains a huge difference in the frequency of metronidazole resistance among these studies (Kissinger 2015a; Matini et al. 2016; Rukasha et al. 2013). Moreover, these studies focus mainly on general population of women; however, HIV-positive pregnant women are also at higher risk of being infected with T. vaginalis and developing resistance to metronidazole (Matini et al. 2016; Rukasha et al. 2013; Schwebke and Barrientes 2006). Studies have shown that molecular-based methods can be used for the detection of metronidazole resistance profiles (Ozcelik et al. 2018; Paulish-Miller et al. 2014). However, there is a lack of this data from our setting.
The current study found a high level of metronidazole resistance, which is of concern, since metronidazole is currently used in syndromic management for STIs and the syndromic management does not include antimicrobial surveillance. Molecular-based methods are rapid, have high sensitivity and specificity, and they can quickly detect specific gene mutations simultaneously from clinical isolates (Alessio and Nyirjesy 2019; Bruni et al. 2019). Based on the findings from this study, molecular-based assays for monitoring metronidazole resistance profiles using nitroreductase genes may serve as a feasible method for antimicrobial surveillance studies for T. vaginalis.
Limitations
This study had the following limitations: A small sample size (47) was available for testing despite the small sample size, and most of the samples had gene mutations associated with metronidazole resistance. Furthermore, the study participants were recruited from a single clinic; however, King Edward VIII Hospital is a central tertiary hospital that services the most of Durban’s population. The study was also limited to HIV-positive pregnant women only. Future research should include a more general population in order to provide more data on antimicrobial resistance patterns in T. vaginalis. The study did not investigate all potential genes associated with metronidazole resistance such as pyruvate ferredoxin or flavin reductase. This is now being considered as a future research endeavour.
Data availability
Data will be available upon request.
Code availability
Not applicable.
References
Abdel-Magied AA, El-Kholya E-SI, Abou El-Khair SM, Abdelmegeed ES, Hamoudaa MM, Mohamed SA, El-Tantawy NL (2017) The genetic diversity of metronidazole susceptibility in Trichomonas vaginalis clinical isolates in an Egyptian population. Parasitol Res 116:3125–3130
Abdel-Magied AA, Hammouda MM, Mosbah A, El-Henawy AA (2017) In vitro activity of nitazoxanide against some metronidazole-resistant and susceptible Trichomonas vaginalis isolates. J Infect Chemother 23:230–233
Akbari Z, Matini Mx (2017) The study of trichomoniasis in pregnant women attending Hamadan city health centers in 2015. Avicenna J Clin Microbiol Infect 4
Alessio C, Nyirjesy P (2019) Management of resistant trichomoniasis. Curr Infect Dis Rep 21:1–7
Bosserman EA, Helms DJ, Mosure DJ, Secor WE, Workowski KA (2011) Utility of antimicrobial susceptibility testing in Trichomonas vaginalis–infected women with clinical treatment failure. Sex Transm Dis 38:983–987
Bouchemal K, Bories C, Loiseau PM (2017) Strategies for prevention and treatment of Trichomonas vaginalis infections. Clin Microbiol Rev 30:811–825
Bradic M, Warring SD, Tooley GE, Scheid P, Secor WE, Land KM, Huang PJ, Chen TW, Lee CC, Tang P, Sullivan SA, Carlton JM (2017) Genetic indicators of drug resistance in the highly repetitive genome of Trichomonas vaginalis. Genome Biol Evol 9:1658–1672
Bruni MP, Freitas da Silveira M, Stauffert D, Bicca GLO, Caetano Dos Santos C, da Rosa Farias NA, Golparian D, Unemo M (2019) Aptima Trichomonas vaginalis assay elucidates significant underdiagnosis of trichomoniasis among women in Brazil according to an observational study. Sex Transm Infect 95:129–132
das Neves RN, Sena-Lopes Â, Alves MSD, da Rocha Fonseca B, da Silva CC, Casaril AM, Savegnago L, de Pereira CMP, Ramos DF, Borsuk S (2020) 2′-Hydroxychalcones as an alternative treatment for trichomoniasis in association with metronidazole. Parasitol Res 119, 725-736
Dessai F, Nyirenda M, Sebitloane M, Abbai N (2020) Diagnostic evaluation of the BD Affirm VPIII assay as a point-of-care test for the diagnosis of bacterial vaginosis, trichomoniasis and candidiasis. Int J STD AIDS 31:303–311
Ertabaklar H, Yaman Karadam S, Malatyalı E, Ertuğ S (2016) Investigation of in vitro metronidazole resistance in the clinical isolates of Trichomonas vaginalis. Mikrobiyol Bul 50:552–558
Ghosh AP, Aycock C, Schwebke JR (2018) In vitro study of the susceptibility of clinical isolates of trichomonas vaginalis to metronidazole and secnidazole. Antimicrob Agents Chemother 62(4):e02329-17
Ginocchio C, Chapin K, Smith J, Aslanzadeh J, Snook J, Hill C, Gaydos C (2012) Prevalence of Trichomonas vaginalis and coinfection with Chlamydia trachomatis and Neisseria gonorrhoeae in the United States as determined by the Aptima Trichomonas vaginalis nucleic acid amplification assay. J Clin Microbiol 50:2601–2608
Green H, Taleghani S (2020) Partner notification and treatment for sexually transmitted infections among pregnant women in Cape Town, South Africa. Int J STD AIDS 0. pp 1–9
Health Do, Africa RoS (2015) Sexually transmitted infections management guidelines
Hussien EM, El-Sayed HZ, Shaban MM, Salm AM, Rashwan M (2004) Biological variability of Trichomonas vaginalis clinical isolates from symptomatic and asymptomatic patients. J Egypt Soc Parasitol 34:979–988
Joseph Davey D, Peters RPH, Kojima N, Mudau M, De Vos L, Olivier D, McIntyre JA, Klausner JD, Medina-Marino A (2018) Sexual behaviors of human immunodeficiency virus-infected pregnant women and factors associated with sexually transmitted infection in South Africa. Sex Transm Dis 45:754–761
Joseph Davey DL, Nyemba DC, Gomba Y, Bekker LG, Taleghani S, DiTullio DJ, Shabsovich D, Gorbach PM, Coates TJ, Klausner JD, Myer L (2019) Prevalence and correlates of sexually transmitted infections in pregnancy in HIV-infected and- uninfected women in Cape Town. South Africa Plos One 14:e0218349
Kirkcaldy RD, Augostini P, Asbel LE, Bernstein KT, Kerani RP, Mettenbrink CJ, Pathela P, Schwebke JR, Secor WE, Workowski KA (2012) Trichomonas vaginalis antimicrobial drug resistance in 6 US cities, STD Surveillance Network, 2009–2010. Emerg Infect Dis 18:939
Kissinger P (2015) Epidemiology and treatment of trichomoniasis. Curr Infect Dis Rep 17:31
Kissinger P (2015) Trichomonas vaginalis: a review of epidemiologic, clinical and treatment issues. BMC Infect Dis 15:307
Kissinger P, Muzny CA, Mena L, Lillis RA, Schwebke JR, Beauchamps L, Taylor SN, Schmidt N, Myers L, Augostini P (2018) A randomized trial of metronidazole in a single 2 g dose versus 500 mg twice daily for 7 days for the treatment of trichomoniasis in women. Lancet Infect Dis 18:1251
Krashin JW, Koumans EH, Bradshaw-Sydnor AC, Braxton JR, Secor WE, Sawyer MK, Markowitz LE (2010) Trichomonas vaginalis prevalence, incidence, risk factors and antibiotic-resistance in an adolescent population. Sex Transm Dis 37:440–444
Kulda J (1999) Trichomonads, hydrogenosomes and drug resistance. Int J Parasitol 29:199–212
Land KM, Clemens DL, Johnson PJ (2001) Loss of multiple hydrogenosomal proteins associated with organelle metabolism and high-level drug resistance in trichomonads. Exp Parasitol 97:102–110
Leitsch D, Janssen BD, Kolarich D, Johnson PJ, Duchêne M (2014) T richomonas vaginalis flavin reductase 1 and its role in metronidazole resistance. Mol Microbiol 91:198–208
Mabaso N, Abbai N (2021) Distribution of genotypes in relation to metronidazole susceptibility patterns in Trichomonas vaginalis isolated from South African pregnant women. Parasitol Res 120:2233–2241
Mabaso N, Naicker C, Nyirenda M, Abbai N (2020) Prevalence and risk factors for Trichomonas vaginalis infection in pregnant women in South Africa. Int J STD AIDS 31:351–358
Marques-Silva M, Lisboa C, Gomes N, Rodrigues AG (2021) Trichomonas vaginalis and growing concern over drug resistance: a systematic review. J Eur Acad Dermatol Venereol 35:2007–2021
Masha SC, Cools P, Sanders EJ, Vaneechoutte M, Crucitti T (2019) Trichomonas vaginalis and HIV infection acquisition: a systematic review and meta-analysis. Sex Transm Infect 95:36–42
Matini M, Maghsood A-H, Mohebali M, Rabiee S, Fallah M, Rezaie S, Rezaeian M (2016) In vitro susceptibility of Iranian isolates of Trichomonas vaginalis to metronidazole. Iran J Parasitol 11:46
Medina-Marino A, Mudau M, Kojima N, Peters RP, Feucht UD, Vos LD, Olivier D, Muzny CA, McIntyre JA, Klausner JD (2020) Persistent Chlamydia trachomatis, Neisseria gonorrhoeae or Trichomonas vaginalis positivity after treatment among human immunodeficiency virus-infected pregnant women, South Africa. Int J STD AIDS 31:294–302
Mohamed B, Elleboudy N, Hussein H, Khalifa K, Azab M (2019) Genotyping of Trichomonas vaginalis isolates from Egypt. Parasitologists United Journal 12:209–220
Moodley D, Moodley P, Sebitloane M, Soowamber D, McNaughton-Reyes HL, Groves AK, Maman S (2015) High prevalence and incidence of asymptomatic sexually transmitted infections during pregnancy and postdelivery in KwaZulu Natal, South Africa. Sex Transm Dis 42:43–47
Morikawa E, Mudau M, Olivier D, de Vos L, Joseph Davey D, Price C, McIntyre JA, Peters RP, Klausner JD (2018) Acceptability and feasibility of integrating point-of-care diagnostic testing of sexually transmitted infections into a South African antenatal care program for HIV-infected pregnant women. 2018, 3946862
Mudau M, Peters RP, De Vos L, Olivier DH, Davey JD, Mkwanazi ES, McIntyre JA, Klausner JD, Medina-Marino A (2018) High prevalence of asymptomatic sexually transmitted infections among human immunodeficiency virus-infected pregnant women in a low-income South African community. Int J STD AIDS 29:324–333
Naidoo S, Wand H, Abbai NS, Ramjee G (2014) High prevalence and incidence of sexually transmitted infections among women living in Kwazulu-Natal, South Africa. AIDS Res Ther 11:31–31
Nyemba DC, Medina-Marino A, Peters RPH, Klausner JD, Ngwepe P, Myer L, Johnson LF, Davey DJ (2021) Prevalence, incidence and associated risk factors of STIs during pregnancy in South Africa. Sex Transm Infect 97:375–381
Organization W.H (2016) Global health sector strategy on sexually transmitted infections 2016–2021: toward ending STIs (World Health Organization)
Organization W.H (2018) Report on global sexually transmitted infection surveillance 2018
Ozcelik S, Ozpinar N, Karakus S, Akyildiz F, Karakaya O (2018) Metronidazole resistance in Trichomonas vaginalis determined by molecular and conventional methods. Trop Biomed 35:188–194
Paulish-Miller TE, Augostini P, Schuyler JA, Smith WL, Mordechai E, Adelson ME, Gygax SE, Secor WE, Hilbert DW (2014) Trichomonas vaginalis metronidazole resistance is associated with single nucleotide polymorphisms in the nitroreductase genes ntr4Tv and ntr6Tv. Antimicrob Agents Chemother 58:2938–2943
Peters R, Klausner JD, de Vos L, Feucht UD, Medina-Marino A (2021) Aetiological testing compared with syndromic management for sexually transmitted infections in HIV-infected pregnant women in South Africa: a non-randomised prospective cohort study. BJOG 128:1335–1342
Price CM, Peters RPH, Steyn J, Mudau M, Olivier D, De Vos L, Morikawa E, Kock MM, Medina-Marino A, Klausner JD (2018) Prevalence and detection of Trichomonas vaginalis in HIV-infected pregnant women. Sex Transm Dis 45:332–336
Rukasha I, Ehlers M, Kock M (2013) P5. 099 Metronidazole antimicrobial drug resistance testing of Trichomonas vaginalis collected from women attending an anti-retroviral clinic, Pretoria. S Afr Sex Transm Infect 89:A366–A366
Schwebke JR, Barrientes FJ (2006) Prevalence of Trichomonas vaginalis isolates with resistance to metronidazole and tinidazole. Antimicrob Agents Chemother 50:4209–4210
Shaio M-F, Lin P-R, Liu J-Y (1997) Colorimetric one-tube nested PCR for detection of Trichomonas vaginalis in vaginal discharge. J Clin Microbiol 35:132–138
Silver BJ, Guy RJ, Kaldor JM, Jamil MS, Rumbold AR (2014) Trichomonas vaginalis as a cause of perinatal morbidity: a systematic review and meta-analysis. Sex Transm Dis 41:369–376
Smullin CP, Green H, Peters R, Nyemba D, Qayiya Y, Myer L, Klausner J, Joseph Davey D (2020) Prevalence and incidence of Mycoplasma genitalium in a cohort of HIV-infected and HIV-uninfected pregnant women in Cape Town, South Africa. Sex Transm Infect
Upcroft JA, Upcroft P (2001) Drug susceptibility testing of anaerobic protozoa. Antimicrob Agents Chemother 45:1810–1814
Vallely LM, Toliman P, Ryan C, Rai G, Wapling J, Gabuzzi J, Allen J, Opa C, Munnull G, Kaima PJB.o (2017) Performance of syndromic management for the detection and treatment of genital Chlamydia trachomatis, Neisseria gonorrhoeae and Trichomonas vaginalis among women attending antenatal, well woman and sexual health clinics in Papua New Guinea: a cross-sectional study. 7, e018630
Van Der Pol B, Rao A, Nye MB, Chavoustie S, Ermel A, Kaplan C, Eisenberg D, Chan PA, Mena L, Pacheco S, Waites KB, Xiao L, Krishnamurthy S, Mohan R, Bertuzis R, McGowin CL, Arcenas R, Marlowe EM, Taylor SN (2021) Trichomonas vaginalis detection in urogenital specimens from symptomatic and asymptomatic men and women by use of the cobas TV/MG test. J Clin Microbiol 59:e0026421
von Glehn MdP, Sa LCEF, da Silva HDF, Machada ER (2017) Prevalence of Trichomonas vaginalis in women of reproductive age at a family health clinic. J Infect Dev Ctries 11:269–276
Workowski KA (2015) Centers for Disease Control and Prevention sexually transmitted diseases treatment guidelines. Clin Infect Dis 61:S759–S762
Yarlett N, Yarlett NC, Lloyd D (1986) Metronidazole-resistant clinical isolates of Trichomonas vaginalis have lowered oxygen affinities. Mol Biochem Parasitol 19:111–116
Acknowledgements
The authors would like to thank all the women who participated in this study and the King Edward VIII Hospital Antenatal Clinic.
Funding
This work was supported Prof Abbai’s research funds awarded by the Institut Mérieux.
Author information
Authors and Affiliations
Contributions
NSA designed and funded parts of the study. BN, NM, and NSA recruited the study population. BN performed all the laboratory testing. KSH and RS provided some of the laboratory reagents. PT performed the statistical analysis. BN and NSA wrote the first draft of the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was approved annually by the Biomedical Research Ethics Committee (BREC), University of KwaZulu-Natal as well as KwaZulu-Natal Department of Health.
Informed consent
Written informed consent was obtained from all antenatal women that were enrolled in this study.
Consent of publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Section Editor: Berit Bangoura.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ngobese, B., Singh, R., Han, K.S.S. et al. Detection of metronidazole resistance in Trichomonas vaginalis using uncultured vaginal swabs. Parasitol Res 121, 2421–2432 (2022). https://doi.org/10.1007/s00436-022-07548-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-022-07548-x