Abstract
Blastocystis hominis with worldwide distribution is a human intestinal protozoa found in all countries. There have been differences in the severity of the pathogenesis of various Blastocystis spp. and a concomitant variation in the plasma concentration of the cytokines in patients with irritable bowel syndrome. In the present study, we aimed to demonstrate the contribution of B. hominis subtypes in the development of irritable bowel syndrome. Stool samples were collected from patients with gastrointestinal disorders. All samples were evaluated through native-lugol method. Total DNA was extracted. A PCR protocol was developed to amplify a specific region of the SSU ribosomal DNA (rDNA) gene. Serum levels of IL-6 and TNF-α were determined by immunoassay methods. The ClustalW algorithm was applied to align and blast the nucleotide sequences of the amplified region of the SSU rDNA gene. To evaluate the phylogenetic and molecular evolutionary of the nucleotide sequences, we used the MEGA software. In this study, we found 26 haplotypes of B. hominis in the studied samples which were collectively belong to five subtypes (ST1, ST2 in patients without irritable bowel syndrome vs. ST3 and two unknown subtypes in patients with irritable bowel syndrome). Result of ELISA showed a high level of IL-6 and TNF-α in the serum of patients with irritable bowel syndrome. The genetic heterogeneity of B. hominis and the existence of different subtypes of the protozoan in patients with IBS may shed light to the fact that some subtypes of parasites may involve in the pathogenesis of IBS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Blastocystis hominis (B. hominis) with worldwide distribution is a human intestinal protozoa found with high frequency in all countries (Tan 2004). Involvement of the protozoan in a wide range of animals has also been corroborated. Its infection rate varies from developed to developing countries (10 to 50 %, respectively) (Shawky et al. 2011), and in Iran, these figures vary from 4.6 to 51.4 % (Heidari and Rokni 2003; Motazedian et al. 2008).
Taxonomic status of this species was unknown until molecular methods developed. Consequently, genome of this parasite was analyzed by Arisue et al. (2002) using combination eight molecules defined this protozoan as a stramenopile (Arisue et al. 2002) that is a branch of the new taxon Chromalveolata (Adl et al. 2005).
Despite numerous studies, there is still a main controversy on the pathogenic role of B. hominis, and it frequently found not only in healthy people but also in person with enteric symptoms but is generally self-limiting (Shawky et al. 2011). However, in many studies, B. hominis have considered responsible for the gastrointestinal symptoms (Pipatsatitpong et al. 2012). The conflicting reports about the pathogenicity of this protozoan may be due to existence of different subspecies that might have varying degrees of pathogenic capabilities (Böhm-Gloning et al. 1997; Vogelberg et al. 2010; Yakoob et al. 2010).
Irritable bowel syndrome (IBS) is the syndrome with numbers symptoms cause gastrointestinal disorder (Singh et al. 2003). Patients with this syndrome defined with some criteria named Rome III: presence of recurrent pain or uncomfortably on abdomen for at least 3 days per month (during the last 3 months) accompanied to the two or more of the following symptoms: (i) comfortable sensation after stool defecation, (ii) alteration in the frequency of stool defecation, (iii) alteration in the form or appearance of stool (Ramirez-Miranda et al. 2010); in addition, depression, anxiety, fatigue, insomnia, bloating, diarrhea or constipation, or both, passing mucus, and feeling that your symptoms are worse after eating (Singh et al. 2003). Physicians diagnose IBS using these symptom-based criteria.
The main cause of the disease remains unknown but it seems is a multi-factorial disease. Infectious origin of IBS has been suspected but has not yet been proven. Many studies showed B. hominis is more frequent in patients with IBS, and there is an association between Blastocystis spp. with irritable bowel syndrome (Longstreth et al. 2006; Coyle et al. 2012; Eida and Eida 2008; Eltayeb et al. 2013; Poirier et al. 2012; Nagel et al. 2014).
As expected, differences in severity among the different cubtypes of Blastocystis were observed (Poirier et al. 2012). At least 10 B. hominis subspecies (genotypes) have been identified. (Eltayeb et al. 2013) Changes in cytokine (interleukin (IL)-6, IL-8, and tumor necrosis factor-α (TNF-α)) secretion have been reported in the plasma and peripheral blood mononuclear cells of IBS patients (Nagel et al. 2014).
Many studies showed pathogenic potential of B. hominis is related to heterogeneity and morphological diversity. Genotyping analysis and in addition diversity in morphology revealed that B. hominis is genetically and antigenically diverse protozoan and suggested that this diversity in morphology and genetic is related to geographical regions and several strains or species of this parasite exist in different areas (Cruz et al. 2003).
Alteration in the immune function caused by microbial-derived mediators has been proposed to play a role in the pathology of IBS (Hughes et al. 2013a, b). In this regard, the cytokines, TNF- α, and IL-6, sensitize colonic afferent and enteric nerves to mechanical stimuli, are potentiating the symptoms of IBS (Liebregts et al. 2007; Ibeakanma and Vanner 2010; O’Malley et al. 2011). Furthermore, higher levels of the cytokines were reported in the serum of patients with IBS in comparison with healthy subjects (Liebregts et al. 2007). Interleukin-6 is predominately produced by T cells and macrophages (Dieh and Rincon 2002). Interestingly, a significantly more number of T cells were found in the gastrointestinal wall of IBS patients compared with control subjects (Hughes et al. 2013a; Liebregts et al. 2007), further highlighting the involvement of IL-6 in the pathology of IBS. Contribution of the mentioned cytokines in the pathology of IBS is unequivocal; however, the primary factor(s) that led to induction of the cytokines in relation to IBS is/are extensively unknown. We hypothesized that some varieties of the parasite B. hominis may somehow provoke production of the cytokines, leading to the development of IBS.
In this study we are looking for find out relationship between B. hominis different subtypes with IBS and inflammatory cytokines secretion.
It is thought that identifying related genotypic varieties among the symptomatic and asymptomatic isolates should assist in determining the pathogenicity of Blastocystis by clearly assigning symptoms to its genotype (Heidari and Rokni 2003). Polymerase chain reaction (PCR) can be currently used to differentiate and stratify various strains, species, and pathogenic forms of B. hominis. Subtype-specific sequence-tagged-site (STS) primers have been designed and used in research setting for determining different genotypes of B. hominis isolates in humans and animals (Shawky et al. 2011).
Material and methods
Samples collection
Stool samples were collected from patients with gastrointestinal disorders referred to health care centers in Ilam city, Iran (west of country). From all of them, medical records were taken. Individuals are diagnosed by gastroenterologist. Patients were classified as follows: (i) patients with gastrointestinal disorders but not IBS and (ii) patients with symptoms IBS: individuals meeting Rome criteria III (Ramirez-Miranda et al. 2010), as formerly mentioned, who attended the gastroenterology clinic at the Ilam city. Eighty fecal samples were collected from patients with IBS (40 samples, female/male 15/25, age 40 ± 4.21) and without IBS (40 samples, female/male 19/21, age 45.4 ± 3.5). Both groups were matched for age and sex.
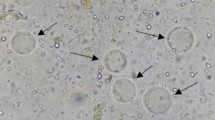
All samples were evaluated through native-lugol method. Stool samples containing other parasites were excluded from our study. Only B. hominis-positive stool samples were stored in −20° C until the DNA was extracted.
Genomic DNA extraction
Total DNA from human stools was extracted using the BIONEER AccuPrep Stool DNA Extraction Kit (Bioneer, South Korea, Lot No. 1301D) according to the manufacturer’s instructions. Briefly, one gram of homogenized stool sample, after thawing and weighting, was suspended thoroughly in lysis buffer. The mixture was warmed to 95 °C to enhance DNA yield, eliminate inhibitors, and improve proteinase K digestion prior DNA eluting in TE buffer.
Blood specimens for inflammatory factor
Five milliliters of peripheral blood was taken from each patient and then sample serum was separated and stored in −20 °C freezer.
PCR amplification
Successful DNA extraction was demonstrated by PCR amplification for ribosomal DNA. Amplification of the specific fragment of the SSU rDNA gene from Blastocystis specimens was accomplished by a developed PCR protocol. The primers are forward Blast 505–532 (5′ GGA GGT AGT GAC AAT AAATC 3′) and reverse Blast 998–1017 (5′ TGC TTT CGC ACT TGT TCATC 3′) previously used by Santín et al. (2011). Each 25 μl PCR mixture contained 1× PCR buffer, 1.5 mM MgCl2, 0.2 mMdNTP, 2.5 U Taq (Qbiogene, Irvine, CA), 2.5 μl BSA (0.1 g/10 ml), and1 μM of each primer. A total of 35 cycles, each consisting of 95° C for 30 s, 54° C for 30 s, and 72° C for 30 s, was performed; an initial pre-heat step at 95° C for 4 min and a final extension step at 72° C for 10 min were also included. The PCR products were separated by electrophoresis on 1.2 % agarose gels containing ethidium bromide and visualized by trans-illumination with ultraviolet light.
Measurements of IL-6and TNF-α
The levels of IL-6 (pg/ml) and TNF-α (pg/ml) were measured using enzyme-linked immunosorbent assays (ELISA). The ABCAM Human IL-6 ELISA Kit (ab46027) and alpha human TNF-α ELISA Kit (a46087) were used to measure IL-6 (human interleukin-6) and TNF-α (Human TNF-α) levels in human serum, respectively. Each kit contains one 96-well strip plate recoated with a human IL-6 and TNF-α capture antibody and sufficient detection antibody, conjugate, buffers, diluents, TMB, and stop buffers, as well as lyophilized human IL-6 and TNF-α standard to analyze several samples.
Molecular analyses
All sequences were subjected to BLAST analysis in GenBank database to verify the isolates under study as Blastocystis spp.. Subtyping definition for Blastocystis was based on the Stensvold et al. (2012) method. For aligning the nucleotide sequences of the study, as well as those genotyping sequences obtained from GenBank (collectively 10 subtypes were identified), the Clustal W algorithm was used. According to the Clustal W algorithm, it would be possible to remove manually the artificial gaps between blasted sequences. MEGA software version 4 was applied for phylogenetic and molecular evolutionary analyses (Tamura et al. 2007). The neighbor-joining (NJ) method of Saitou and Nei (1987) was used for phylogenetic inference. The reliability of phylogenetic branches was evaluated by boot strap analyzing (1000 replicates). Phylogenetic trees were constructed using the neighbor-joining (NJ) method by the help of the software program MEGA version 3.1.
Results
In this study, stool specimens were collected from all of 80 gastrointestinal symptomatic patients, 40 with IBS include 25 males and 15 females, ranging in age from 9 to 60 years, and 40 non-IBS include 21 males and 19 females ranging in age from 5 to 73 years. There were no differences for age and gender between the two groups (P > 0.05).
Stool samples were examined by direct smear, DNA was extracted for each of the isolates, and level IL6 and TNF-α serum samples were tested by standard ELISA. Result of ELISA showed the level of IL6 and TNF-α in patients with IBS is more than patients with no IBS. Serum level of Il-6 was significantly higher in patients relative to the control subjects (23.43 ± 4.23 pg/ml vs. 13.50 ± 3.82 pg/ml, P < 0.0001). Likewise, serum level of TNF-α was significantly elevated in patients compared with the control group (11.06 ± 1.88 pg/ml vs. 6.36 ± 1.94 pg/ml, P < 0.0001). All 80 isolates were successfully amplified by PCR. All samples positive to microscopy were positive on PCR testing with the primers previously used by Santín et al. (2011).
At least 26 B. hominis of SSU ribosomal RNA (rRNA) gene haplotypes have been recognized by alignment analyses and comparing with those sequences presented in GenBank. All the analyses were based on the 500 bp of the SSU rRNA gene B. hominis (without primers). Only 26 out of 80 (32.5 %) PCR products had enough amplified DNA to directly determine their sequences (Table 1). Alignment of these sequences and their homologous from GenBank were revealed to be of diagnostic value for B. hominis spp.. Each of the SSU rDNA gene sequences obtained in this study showed very high similarity (from 98 to 100 %) to homologous sequences of the other Blastocystis isolates reported so far.
The plotted phylogenetic tree revealed five different clades for 26 specimens, detecting ST-1 in three human specimens, ST-2 in four human specimen, ST-3 in eight human specimens, and eleven specimens were located within two independent and different clades obtained from patients with and without IBS (Fig. 1, Table 1). These two clades are not in agreement with those reported in previous studies and are closely related together.
Phylogenetic tree of the SSU-rDNA gene sequences of Blastocystis isolates constructed by the neighbor-joining method using Mega4 software (version4). Isolate or strain names are as provided in Genbank as available, followed by accession numbers in parentheses. Sequences generated in this study named as B. hominis IR/Il. Proteromonas lacerate (accession number AY224080) used as the out-group. Bootstrap values (%) are indicated at the internal nodes (1000 replicates). Bootstrap values of less than 50 % are not shown
All sequences in the present study along with the reference sequences (Table 2) obtained from GenBank were subjected to phylogenetic analysis (Fig. 1)
The 16 sequences from the five isolates have been deposited in the GenBank with these accession numbers (KU168396-KU168411 B. hominis).
Discussion
Blasticystis hominis is a commonly parasitic infection among humans which its infection rate varies from developed (10 %) to developing (50 %) countries (Shawky et al. 2011). In this study, Blastocystis spp. were identified using both direct wet smears and PCR method; moreover, level of inflammatory factors (IL6 & TNF α) were detected by ELISA. Despite a lot of studies, the pathogenicity of B. hominis is still controversial but it is frequently reported in individuals with enteric symptoms and asymptomatic persons (Tan 2008).
It has been accepted that differences in severity among the different subtypes of Blastocystis were observed (Poirier et al. 2012). The first studies made by means of PCR-RFLP of SSU-rDNA by Clark (1997) and Böhm-Gloning et al. (1997) reported the presence of six ribodemes and five subgroups, respectively.
Several studies have been identified at least 10 B. hominis subspecies (genotypes) (Eltayeb et al. 2013). Changes in cytokine (interleukin (IL)-6, IL-8, and tumor necrosis factor-α (TNF-α) secretion have been reported in the plasma and peripheral blood mononuclear cells of IBS patients (Nagel et al. 2014), and many studies showed B. hominis is more frequent in patients with IBS, and there is an association between Blastocystis spp. with irritable bowel syndrome (Longstreth et al. 2006; Coyle et al. 2012; Eida and Eida 2008; Eltayeb et al. 2013; Poirier et al. 2012; Nagel et al. 2014).
Interestingly, in this study, we found 26 haplotypes of B. hominis human-studied samples which belong to five subtypes ST1, ST2, ST3, and two unknown subtype. Haplotypes obtained from non-IBS patients (5,6 9,27,29,31,33) belonging to (ST1, ST2) and haplotypes obtained from IBS) 1,3,7,11,15,19,20,25) belonging to (ST3) and haplotypes including (2,4,8,16,18,22,28,30,34,35) assigned in two unknown and new clades are obtained from patients with and without IBS. It should be noted that, despite specific PCR products being obtained, the subtype(s) of eleven sequenced samples could not be determined. In the previous studies, five subtypes are detected in Iran (I, II, VI, VII, and VIII), and STI was predominated in the asymptomatic and symptomatic persons Motazedian et al. (2008), and ST 3,4, 5,7, and unknown subtype that ST4 was predominant (Khoshnood et al. 2015).
For many years, the genetic heterogeneity of B. hominis has been defined, and existence of different subtypes of these protozoa in IBS and non-IBS patients proves the contribution of subtypes of parasites with IBS syndrome.
The results of this study are in line with the findings of many other studies regarding the presence of genetic diversity of the protozoan (Clark 1997; Böhm-Gloning et al. 1997; Hoevers et al. 2000; Thathaisong et al. 2003; Yoshikawa et al. 2000, 2003). Yan et al. (2006) in Ganzhou (China) found four genotypes of B. hominis that the commonest genotype was ST1. Shawky et al. (2011) detected 110 isolates in stools samples belonging to four different genotypes of B. hominis in patients with and without IBS while the genotype III was the commonest detected genotype.
According to previous studies, distribution of different genotypes of B. hominis is not homogenous in different geographic areas, as ST3 in Bangladesh, Germany, Japan, Pakistan, and UK predominates (Clark 1997; Kaneda et al. 2001; Yoshikawa et al. 2003; Wong et al. 2008), the ST1 and ST4 in China and Thailand (Thathaisong et al. 2003; Yan et al. 2006) and ST4 in the health district of HCUV (Valencia, Spain) are the commonest genotypes.
In present study, ST3 which includes 8/26 (30.7 %) of all isolates was predominant genotype were agree with those reported by Shawky et al. (2011), Abdulsalam et al. (2013), Clark (1997) in London, Kaneda et al. (2001) in Tokyo.
These findings disagree with the results reported by Nourrisson et al.(2014) and Khoshnood et al. (2015) that ST4 was predominant in persons with IBS and Yoshikawa et al. (2004) does not find association between genotype (ST3) and clinical manifestations, but Clark (1997) found significant association between the gastrointestinal symptoms and STI, III. VI.
Although, we found an association between ST3 and its possible pathogenicity, because the sample size was too small to decisively reveal this relation, caution should be regarded for the result. For this reason, further studies with larger sample size are required to verify this issue.
Our finding together with those found by other authors (Clark 1997; Hoevers et al. 2000; Kaneda et al. 2001; Yoshikawa et al. 2000, 2003) revealed the worldwide spreading of different genotypes of B. hominis and that an exclusive genotype could not be limited to a certain geographic area.
The genetic variability of the SSUrDNA gene we found among the different B. hominis isolates in the present study provided robust evidence regarding the highly genetic diversity of the protozoan. Among the three identified subtypes of the organism, the ST3 was predominately associated with IBS syndrome, highlighting the pathogenic potential of the protozoa.
References
Abdulsalam AM, Ithoi I, Al-Mekhlafi HM, Al-Mekhlafi AM, Ahmed A, Surin J (2013) Subtype Distribution of Blastocystis Isolates in Sebha, Libya. PLoS One 8: e84372
Adl S, Simpson A, Farmer M, Andersen R, Anderson O, Barta J, Bowser S, Brugerolle G, Fensome R, Fredericq S, James T, Karpov S, Kugrens P, Krug J, Lane C, Lewis L, Lodge J, Lynn D, Mann D, Mc Court R, Mendoza L, Moestrup O, Mozley-Standridge S, Nerad T, Shearer C, Smirnov A, Spiegel F, Taylor M (2005) The new higher level classification of eukaryotes with emphasis on the taxonomy of protists. J Eukaryot Microbiol 52:399–451
Arisue N, Hashimoto T, Yoshikawa H, Nakamura Y, Nakamura G, Nakamura F, Yano T, Hasegawa M (2002) Phylogenetic position of Blastocystis hominis and of stramenopiles inferred from multiple molecular sequence data. J Eukaryot Microbiol 49:42–53
Awatif MA, Init I, Al-Mekhlafi HM, Al-Mekhlafi AM, Abdulhamid A, Johari S (2013) Subtype distribution of Blastocystis isolates in Sebha, Libya. PLoS One 8:e84372
Böhm-Gloning B, Knobloch J, Walderich B (1997) Five subgroups of Blastocystis hominis isolates from symptomatic and asymptomatic patients revealed by restriction site analysis of PCR-amplified 16S-like rDNA. Trop Med Int Health 2:771–778
Clark CG (1997) Extensive genetic diversity in Blastocystis hominis. Mol Biochem Parasitol 87:79–86
Coyle CM, Varughese J, Weiss LM, Tanowitz HB (2012) Blastocystis: to treat or not to treat. Clin Infect Dis 54:105
Cruz LV, Plancarte CA, Alvarez MC, Valencia RS, Sásnchez RG, Vega FL (2003) Blastocystis hominis among food vendors in xochimilco markets. Rev Latinoam Microbiol 45:12–15
Dieh S, Rincon M (2002) The two faces of IL-6 on Th1/Th2 differentiation. Mol Immunol 39:531–536
Eida AM, Eida MM (2008) Identification of Blastocystis hominis in patients with irritable bowel syndrome using microscopy and culture compared to PCR. Parasitol United J (PUJ) 1:87–92
Eltayeb LB, Brair LS, Aljafari AS (2013) The impact of intestinal protozoan parasites among irritable bowel syndrome patients in Khartoum state. Al Neel Med J 3:47–57
Heidari A, Rokni MB (2003) Prevalence of intestinal parasites among children in day-care centers in Damghan, Iran. Iran J Pub Health 32:31–34
Hoevers J, Holman P, Logan K, Hommel M, Ashford R, Snowden K (2000) Restriction-fragment-length polymorphism analysis of small-subunit rRNA genes of Blastocystis hominis isolates from geographically diverse human hosts. Parasitol Res 86:57–61
Hughes PA, Zola H, Penttila IA, Blackshaw LA, Andrews JM, Krumbiegel D (2013a) Immune activation in irritable bowel syndrome: can neuroimmune interactions explain symptoms? Am J Gasreroentrol 108:1066–1073
Hughes PA, Harrington AM, Castro J, Liebregts T, Adam B, Dallas JG, Isaacs NJ, Maldeniya L, Martin CM, Persson J, Andrews JM, Holtmann G, Blackshaw AL, Brierley SM (2013b) Sensory neuro-immune interactions differ between irritable bowel syndrome subtypes. Gut 62:1456–1465
Ibeakanma C, Vanner S (2010) TNF alpha is a key mediator of the pronociceptive effects of mucosal supernatant from human ulcerative colitis on colonic DRG neurons. Gut 59:612–621
Kaneda Y, Horiki N, Cheng XJ, Fujita Y, Maruyama M, Tachibana H (2001) Ribodemes of Blastocystis hominis isolated in Japan. Am J Trop Med Hyg 65:393–396
Khoshnood S, Rafiei A, Saki J, Alizadeh K (2015) Prevalence and genotype characterization of Blastocystis hominis among the baghmalek people in southwestern Iran in 2013–2014. Jundishapur J Microbiol 8:e23930
Liebregts T, Adam B, Bredack C, Röth A, Heinzel S, Lester S, Downie-Doyle S, Smith E, Drew P, Talley NJ, Holtmann G (2007) Immune activation in patients with irritable bowel syndrome. Gastroenterology 132:913–920
Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F (2006) Functional bowel disorders. Gastroenterology 130:1480–1491
Motazedian H, Gasemi H, Sadjjadi MS (2008) Genomic diversity of Blastocystis hominis from patients in southern Iran. Ann Trop Med Parasitol 102:85–88
Nagel R, Bielefeldt-Ohmann H, Traub R (2014) Clinical pilot study: efficacy of triple antibiotic therapy in Blastocystis positive irritable bowel syndrome patients. Gut Pathogens 6:34
Nourrisson C, Scanzi J, Pereira B, Nkoud Mongo C, Wawrzyniak I, Cian A, Viscogliosi E, Livrelli V, Delbac F, Dapoigny M, Poirier P (2014) Blastocystis is associated with decrease of fecal microbiota protective bacteria: comparative analysis between patients with irritable bowel syndrome and control subjects. PLoS One 9:e111868
O’Malley D, Liston M, Hyland NP, Dinan TG, Cryan JF (2011) Colonic soluble mediators from the maternal separation model of irritable bowel syndrome activate submucosal neurons via an interleukin-6-dependent mechanism. Am J Physiol Gastrointest Liver Physiol 300:G241–G252
Pipatsatitpong D, Rangsin R, Leelayoova S, Naaglor T, Mungthin M (2012) Incidence and risk factors of Blastocystis infection in an orphanage in Bangkok. Parasite Vector 5:37
Poirier P, Wawrzyniak I, Vivare CP, Delbac F, El Alaoui H (2012) New insights into Blastocystis spp.: a potential link with irritable bowel syndrome. PLoS Pathogens 8:e1002545
Ramirez-Miranda ME, Hernandez-Castellanos R, Lopez-Escamilla E, Moncada D, Rodriguez-Magallan A, Pagaza-Melero C, Gonzalez-Angulo A, Flisser A, Kawa-Karasik S, Maravilla P (2010) Parasites in Mexican patients with irritable bowel syndrome: a case-control study. Parasite Vector 3:96
Saitou N, Nei M (1987) The neighbor-joining method: a new method for reconstructing phylogenetic trees. Mol Biol Evol 4:406–425
Santín M, Gómez-Muñoz MT, Solano-Aguilar G, Fayer R (2011) Development of a new PCR protocol to detect and subtype Blastocystis spp. from humans and animals. Parasitol Res (2011) 109:205–212
Shawky A, Fouad A, Maha MA, Basyoni B, Reham A, Fahmy C, Mohamed H, Kobaisi D (2011) The pathogenic role of different Blastocystis hominis genotypes isolated from patients with irritable bowel syndrome. Arab J Gastroenterol 12:194–200
Singh RK, Pandey HP, Singh RH (2003) Irritable bowel syndrome: challenges ahead. Curr Sci 84:25
Stensvold CR, Alfellani M, Clark G (2012) Levels of genetic diversity vary dramatically between Blastocystis subtypes Infection. Gen Evol 12:263–273
Tan KSW (2008) New insights on classification, identification and clinical relevance of Blastocystis spp. Clin Microbiol Rev 21:639–665
Tan KSW (2004) Blastocystis in humans and animals: new insights using modern methodologies. Vet Parasitol 9:121–144
Tamura K, Dudley J, Nei M, Kumar S (2007) MEGA4: Molecular Evolutionary Genetics Analysis (MEGA) software version 4.0. Mol Biol and Evolution 24:1596–1599
Thathaisong U, Worapong J, Mungthin M, Tan-Ariya P, Viputtigul K, Sudatis A, Noonai A, Leelayoova S (2003) Blastocystis isolates from a pig and a horse are closely related to Blastocystis hominis. J Clin Microbiol 41:967–975
Vogelberg C, Stensvold CR, Monecke S, Ditzen A, Stopsack K, Heinrich-Grafe U, Pohlmann C (2010) Blastocystis sp. subtype 2 detection during recurrence of gastrointestinal and urticarial symptoms. Parasitol Int 59:469–471
Wong KH, Ng GC, Lin RT, Yoshikawa H, Taylor MB, Tan KS (2008) Predominance of subtype 3 among Blastocystis isolates from a major hospital in Singapore. Parasitol Res 102:663–670
Yakoob J, Jafri W, AsimBM AZ, NazSh IM, Khan R (2010) Blastocystis hominis and Dientamoeba fragilis in patients fulfilling irritable bowel syndrome criteria. Parasitol Res 107:679–684
Yan Y, Su S, Lai R, Liao H, Ye J, Li X, Luo X, Chen G (2006) Genetic variability of Blastocystis hominis isolates in China. Parasitol Res 99:597–601
Yoshikawa H, Abe N, Wu Z (2003) Genomic polymorphism among Blastocystis isolates and development of PCR-based identification of zoonotic isolates. J Eukaryot Microbiol 50:710–711
Yoshikawa H, Abe N, Iwasawa M, Kitano S, Nagano I, Wu Z, Takahashi Y (2000) Genomic analysis of Blastocystis hominis strains isolated from two long term health care facilities. J Clin Microbiol 38:1324–1330
Yoshikawa H, Wu Z, Kimata I, Iseki M, Ali IK, Hossain MB, Zaman V, Haque R, Takahashi Y (2004) Polymerase chain reaction-based genotype classification among human Blastocystis hominis populations isolated from different countries. Parasitol Res 92:22–29
Acknowledgments
The work was supported by the Ilam University of Medical Scinences, Ilam, Iran, grant 908441 awarded to Dr. Asad Mirzaei. The authors would like to acknowledge the staff of Dr. Asadollahi laboratory for their kind assistance in the sampling.
Authors’ contributions
MA and BGH were involved in designing and supervising the fieldwork and in interpreting the data; AM, was involved in the collection of samples and molecular tests; MA supervised all genetic aspects in this study. MA and BGH wrote the manuscript. All authors have read and approved the final manuscript. MA is the guarantor of the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Ilam University of Medical Sciences Ethics Committee and registered with no: EC/92/H/132.
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Azizian, M., Basati, G., Abangah, G. et al. Contribution of Blastocystishominis subtypes and associated inflammatory factors in development of irritable bowel syndrome. Parasitol Res 115, 2003–2009 (2016). https://doi.org/10.1007/s00436-016-4942-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-016-4942-4