Abstract
Toxoplasmosis is a parasitic infection caused by Toxoplasma gondii protozoon. It is most commonly treated by pyrimethamine (PYR); however, this was intolerable by many patients. The aim of this study was to assess therapeutic effects of Nigella sativa oil (NSO) alone and combined with pyrimethamine (PYR) compared to a previous combination of clindamycin (CLN) and (PYR). One hundred Albino mice were used in the current study and were equally divided into five groups: normal (I), infected untreated control (II); infected, treated with NSO-only (III); infected, treated with NSO + PYR (IV); and infected, treated with CLN + PYR (V). The virulent RH Toxoplasma strain was used in infection survival rates estimation, impression smears from liver and spleen, and histopathological and ultrastructural studies were done. Liver malondialdehyde (MDA) level and total antioxidant capacity (TAC) were determined. Interferon-γ and specific IgM were also measured in sera by ELISA. Results showed that NSO alone has no direct anti-Toxoplasma effect, whereas its combination with PYR produced potent effect that is comparable to CLN + PYR. It significantly increased the survival rate and decreased the parasite density and pathological insult in both liver and spleen. Also, significant increase in interferon-γ level denotes stimulation of cellular immunity. NSO + PYR combination markedly improved the antioxidant capacity of Toxoplasma infected mice compared to the infected untreated ones and to CLN/PYR. In conclusion, although NSO, if administered alone, has significant immunostimulant and antioxidant properties, it failed to decrease tachyzoite counts. Combination of NSO and PYR had synergistic effect in treatment of toxoplasmosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Toxoplasmosis is a worldwide disease caused by the apicomplixan protozoan parasite Toxoplasma gondii. The disease is effectively controlled by the host immune response and remains dormant in the host neural and muscle tissues for the lifetime of the host (Dupont et al. 2012). Although most individuals do not experience any symptoms, individuals with compromised immune system suffer a life-threatening disease. Man acquires the infection through ingestion of tissue cysts in undercooked or raw meat or by accidental ingestion of mature oocysts in contaminated food and drink. Congenital transmission is also another important route of infection that may lead to serious consequences (Ahmed et al. 1996; Pappas et al. 2009).
The standard chemical agents for treatment of toxoplasmosis are dihydrofolate reductase (DHFR) inhibitors as pyrimethamine (PYR). While these drugs have a high degree of binding selectivity for T. gondii DHFR versus mammalian DHFR, they are only active against tachyzoites and not bradyzoites and are not effective when used as single agents. Thus, they are generally used in combination with sulfa drugs (Rosowsky et al. 1998). However, this combined treatment is often associated with bone marrow suppression and kidney problems (Katlama et al. 1996). New agents or combination of agents with better therapeutic efficacy and safety than currently available drugs are urgently needed (Park and Nam 2013).
Interferon-γ (IFN-γ) is an important cytokine for coordinating protective immunity against infection with intracellular parasites. The immunity against T. gondii is mediated by the IFN-γ-dependent Th1-predominant immune response. It mediates its protective effects by triggering the lysosomal activity and modulating metabolic activity of antigen-presenting cells, including dendritic cells and macrophages (Taylor et al. 2004; Sturge et al. 2013).
Nigella sativa oil (NSO) has a potent immunostimulant effect; it increases IFN-γ levels and potentiate T cells in vitro for adoptive T cell therapy against cancer and infectious diseases (Keyhanmanesh et al. 2010; Salem et al. 2011).Therefore, several therapeutic effects have been described for N. sativa including anti-asthma (Suzuki et al. 1988), hypotensive, anti-nociceptive, anti-fertility, anti-diabetic, anti-inflammatory, anti-oxidant, and anti-microbial (Ali and Blunden 2003). Moreover, NSO has been tried for treatment of cancer (Padhye et al. 2008). Also, efficacy of NSO was reported against many helminthic infection as Hydatid cyst (Mahmoudvand et al. 2014), Toxocara (Shalaby and El-Moghazy 2013), and Hymenolepes nana (Ayaz et al. 2007). It was tried also against schistosomiasis and proved prompt hepatoprotective properties (Aboul-Ela 2002). Regarding protozoa, it succeeded as leishmanicidal agent (Mahmoudvand et al. 2015) and in treating Cryptosporidium parvum (Nasir et al. 2013) and Blastocystis hominis (El Wakil 2007). Also, good results were obtained with its experimental treatment of malaria (Okeola et al. 2011).
However, to the best of our knowledge, nothing is known about the efficacy of NSO on the virulent RH strain of T. gondii. Thus, in the present study, we evaluated NSO used alone and in combination with PYR in treatment of mice infected with the virulent RH strain of T. gondii, aiming at development of safe and effective drug or drug combination against toxoplasmosis.
Materials and methods
T. gondii strain
The virulent RH strain of T. gondii was maintained in the Parasitology Department, Faculty of Medicine, Alexandria University by serial intraperitoneal (i.p.) passages of tachyzoites in Swiss albino mice (6–8 weeks old, 20 g weight) every 4–5 days. The tachyzoites were collected from the peritoneal exudates of mice, washed three times, and then diluted with phosphate buffered saline (PBS) pH 7.4 to be used for intraperitoneal infection of mice at a dose of 3.5 × 103 tachyzoites/mouse in 0.1 ml PBS, pH 7.4 (Chan and Luft 1986).
Tested compounds
-
N. sativa oil (NSO) (Pharco-Pharmaceuticals, Alexandria, Egypt)
-
Pyrimethamine (PYR) (Wellcome Pharmaceuticals)
-
Clindamycin (CLN) (Pfizer pharmaceuticals)
Mice and experimental design
This study was carried out on 100 male Swiss albino mice, aged 3 to 5 weeks, weighing between 20 and 25 g. They were housed in well-ventilated cages supplied with standard pellet food and water (El-Fakhry et al. 1998). Mice stools were examined conventionally to exclude the presence of parasites (Giarcia and Bruckner 1977). This study protocol was approved by the Ethics Committee of Faculty of Medicine, Alexandria University, Egypt.
Mice were equally divided into five groups (20 mice each) as follows:
-
Group I:
Normal uninfected mice, included healthy mice injected with 1 ml PBS (pH 7.4) i.p., then received 0.3 ml of 2 % gum acacia orally/day for 5 days.
-
Group II:
Infected untreated mice included infected mice that received 0.3 ml of 2 % gum acacia orally/day for 5 days from day zero post infection.
-
Group III:
NSO-only treated mice, included infected mice that were treated with NSO, in a dose of 5 ml/kg body weight/day emulsified in 0.3 ml gum acacia 2 % orally for 5 days (Mahmoud et al. 2002)
-
Group IV:
NSO + PYR-treated group included infected mice that were treated with a combination of PYR and NSO in doses of 12.5 mg/kg and 5 ml/kg body weight/day, respectively (Romand et al. 1993; Mahmoud et al. 2002 orally suspended and emulsified in 0.3 ml gum acacia 2 % for 5 days.
-
Group V:
CLN + PYR-treated group included infected mice that were treated with a combination of CLN and PYR in doses of 25 mg/Kg (Araujo et al. 1998) and 12.5 mg/Kg (Romand et al. 1993), respectively. The calculated dose of both drugs was suspended in 0.3 ml of gum acacia 2 % and administered orally for 5 days.
Ten mice from each group were observed daily for survival rate calculation, while the other 10 mice were sacrificed on the 5th day post-infection for evaluation of other parameters.
On the 5th day post-infection, mice were fasted for overnight with free access to water. Animals were anesthetized and sacrificed, and blood samples were collected and left to coagulate at 37 °C for 20 min then centrifuged at 3000 rpm for 15 min. Sera were separated, divided into aliquots, and stored at −80 °C until used. The peritoneal fluid containing tachyzoites was collected following sacrifice from all studied groups. Livers and spleens were isolated and used for: estimation of parasite count, histopathological study, and assay of biochemical parameters.
Parasitological evaluation
Survival rate estimation
The number of survived mice was recorded daily until all mice died. The survival rate was calculated in each group according to the following equation:
Number of survived mice/number of mice at the beginning of the experiment × 100 (Eissa et al. 2012)
Parasite load
Impression smears were made from liver and spleen and stained with Giemsa stain. Counting of T. gondii tachyzoites in different tissue smears were carried out using oil immersion objectives (×100) lens. The mean of ten different fields of each mouse and the mean of the 10 mice were calculated (AL-Dakhil and Morsy 1996).
Morphological study
Light microscopy (LM) and scanning electron microscopy (SEM) were used in examination of T. gondii tachyzoites collected on the 5th day PI from each group. The specimens were processed for SEM according to Klainer and Betsch (1970) and examined using a Jeol-JSM-25 SII scanning microscope.
Histopathological evaluation
Specimens from the liver were fixed in 10 % formalin, dehydrated in ascending series of ethyl alcohol, cleared in xylol, and then embedded in paraffin. Serial sections, 5-micron thick, were cut using microtome, and processed for staining using haematoxylin and eosin stain. Sections were put in xylol, passed in descending series of ethyl alcohol, rinsed in water, stained in Harris haematoxylin, washed under running water, and then counter-stained using eosin. They were dehydrated using ascending series of ethyl alcohol and then mounted in Canada balsam (Drury and Wallington 1980).Histopathological examination was performed using standard light microscopy and liver inflammation, and injury was assessed for each study group using the Ishak modification of the Knodell “hepatic activity index” (Theise 2007).
Biochemical evaluation
Parts of the isolated livers were immediately washed with ice-cold saline, blotted dry on filter papers, weighed and homogenized for assessing malondialdehyde (MDA) level (Ohkawa et al. 1979), and total antioxidant capacity (TAC) ( Koracevic et al. 2001) as follows:
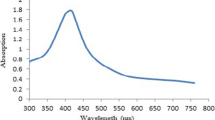
MDA level
This method is based on the reaction of thiobarbituric acid (TBA) with MDA (contained in liver tissue homogenate in 1.15 % KCL) in acidic medium (pH 3.5) at a temperature of 95 °C to form TBA reactive product that yields a pink color which can be measured spectrophotometrically at 532 nm. The values are expressed in nM/gm tissue (Ohkawa et al. 1979)
TAC
Colorimetric determination of TAC is based on the reaction of antioxidants in the sample (supernatant of liver tissue homogenate in 10 mM phosphate buffer pH 7.4) with a defined amount of hydrogen peroxide. The residual is determined colorimetrically by an enzymatic reaction that evolves the conversion of 3,5 dichloro-2-hydroxy benzene sulfonate to a colored product that can be measured at 505 nm. The values are expressed in mM/gm tissue (Koracevic et al. 2001).
Immunological study
IFN-γ (Stoicov et al. 2004) and IgM (Al-Suhaimi 2012) were measured in serum samples using ELISA kit (KOMA Kit, Biotech, Inc.).
Statistical analysis
Data are presented as minimum–maximum, mean ± SD, and median. Data analysis was performed using SPSS version 20 computer software. ANOVA (F) test followed by post hoc test (Scheffe) was performed to compare variables between different studied groups. Significance was set at P < 0.05 (Leslie et al. 1991).
Results
Survival rate
The best survival rate was observed in mice receiving combined treatment (groups IV and V). Eighty percent of animals survived beyond the 10th day PI and all mice died before day 15 PI. These were followed by NSO-only treated mice (group III) in which 30 % of mice survived till day 8 PI. All untreated mice succumbed by day 7 PI. (Fig. 1)
Parasite load
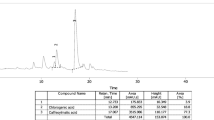
T. gondii tachyzoites were detected clearly in impression smears from liver specimens in all infected groups with extremely variable densities. In the infected untreated mice (group II), the mean tachyzoite count in the liver and spleen was 14.86 ± 1.07 and 8.0 ± 1.81, respectively. Significant reduction was noticed in NSO + PYR-treated mice (group IV) to 2.90 ± 1.03 and 2.67 ± 1.34. Also, in CLN + PYR-treated mice (group V), the mean tachyzoite count significantly reduced to 2.35 ± 0.81 and 2.63 ± 0.92 in liver and spleen, respectively, with no statistically significant difference between them. No significant reduction was observed in NSO-only treated mice (group III) compared to infected untreated mice (group II) (Table 1).
Morphological results
Light microscopic examination of the peritoneal exudates of the different infected groups showed that only in mice received combination treatments NSO + PYR (group IV) and CLN + PYR (group V) tachyzoites showed sluggish of movement with deformed crescent shape. On the other hand, in NSO-only treated mice, the tachyzoites movement was normal without any signs of deformity.
By SEM, tachyzoites in the infected control group (group II) appeared elongated, often crescent-shaped parasite with a rounded pole at one end and a more or less pointed pole at the other. The site of the conoid is evident and resembled a compressed spring, while the cytostome appeared as indentation in the pellicle. However, tachyzoites retrieved from mice receiving combined treatment (groups IV and V) showed deformities (in the form of depressions, protrusions, and irregularities) (Fig. 2).
SEM of tachyzoite of T. gondii (1). Tachyzoites from infected control mice (group II) showing crescent-shaped parasite with smooth surface (×20,000) (2).Tachyzoites from NSO + PYR-treated mice (group IV) showing dimples (arrowhead) and small projections (arrow)and irregular surface with preservation of the crescent shape(×20,000) (3). Tachyzoites from NSO + PYR-treated mice (group IV), showing irregular surface, with deep ridges (arrows) and dimples (arrowheads); their crescent shape is totally lost (×35,000) (4). Tachyzoites from CLN + PYR-treated mice (group V) showing dimples (arrows) and large projections from the terminal ends (arrowheads) (×20,000) (5). Tachyzoites from the same group (V), showing loss of the crescent shape, shrunken, mutilated organism, less tapered ends, multiple deep furrows on the surface (arrows) (×20,000)
Histopathological results
Histopathologic examination of liver
Examination of the liver of the infected untreated group (II) mice revealed disturbance of the hepatic architecture with distortion of the liver cell plates with variable hepatocyte ballooning. Hepatic lobules reveal moderate inflammatory cell infiltrate with frequent drop out (spotty) necrosis (up to 10 foci per ×10 objective) (Fig. 3b) as well as focal confluent necrosis, predominantly within zone 3 (pericentral) (Fig. 3c). Hepatocytes show diffuse ballooning and focal micro-steatosis as well as intrahepatic cholestasis. Hepatic sinusoids are dilated and infiltrated by lymphocytes and histiocytes (Fig. 3d) and fewer eosinophils. Kupffer cell hyperplasia and hypertrophy are notable. Tachyzoites are observed both extracellularly (Fig. 3d) and intracellularly within the cytoplasm of the Kupffer cells, histiocytes as well as hepatocytes. All portal tracts are moderately to markedly infiltrated by a chronic non-specific inflammatory infiltrate composed primarily of lymphocytes, histiocytes, plasma cells, and fewer eosinophils (Fig. 3e).
Histopathological study of the liver (1). Liver section from normal control mice (group I) showing preserved hepatic architecture (H&E, ×100) (2). Liver section from infected, untreated control group (II), showing disturbed architecture with multiple foci of necro-inflammatory activity, predominantly seen in the pericentral location (arrows) (H&E, ×100) (3). Liver section from infected control group (II), showing centrilobular confluent necrosis (compound arrow) as well as tachyzoite collections (single arrow) (4). Liver section from infected control group (II), showing Kupffer cell hyperplasia (single arrows) and a histiocyte within a sinusoid (compound arrow). Extracellular tachyzoites are seen (blue arrows) (H&E, ×1000) (5). Liver section from infected untreated control group (II) showing marked portal inflammatory cellular infiltrate (H&E, ×400) (6). Liver section from NSO-treated group (III) showing moderate portal inflammatory cellular infiltrate (H&E, ×400) (7). Liver section from NSO-treated group (III) showing intrahepatocyte tachyzoites (blue arrow) and centrilobular spotty necrosis (black arrows) (H&E, ×400) (8). A high power view of intra-hepatocyte tachyzoites in liver of NSO-treated group (H&E, ×1000). BD: bile ductule, PV: portal venule
Group III mice (NSO-only) livers exhibited similar changes to the infected group only with notable reduction in the hepatic lobular inflammation with reduced dropout necrosis (Fig. 3g). Intracellular tachyzoites remain to be detected within hepatocytes (Fig. 3h) and Kupffer cells. Portal inflammation remained marked to moderate (Fig. 3f) in all portal tracts with heavy infiltration by lymphocytes and plasma cells.
Group IV mice (NSO + PYR) revealed a marked reduction in the extent and severity of the inflammatory response. Hepatic lobular inflammation and dropout necrosis reduced to 2–4 foci/×10 objective. Kupffer cell hyperplasia and intrasinusoidal histiocytes, as well as tachyzoite collections, were markedly reduced. Portal tract inflammation was observed focally in a few portal tracts.
Group V mice (CLN + PYR) revealed a marked reduction in extent and severity of the hepatic lobular and portal inflammatory response, with reduced inflammatory cell infiltrates as well as tachyzoite collections.
Histopathological examination of the spleen
Examination of the spleen of the infected control group (II) mice revealed marked congestion of the splenic red pulp (Fig. 4a) with hyperplastic Littoral cells as well as sinusoidal engorgement with macrophages, many of which were laden with tachyzoites. A number of extracellular tachyzoite collections, as well as numerous multinucleated giant cells, appeared within the red pulp (Fig. 4b). The white pulp follicles revealed follicular hyperplasia (Fig. 4a).
Histopathological study of the mice spleens (1). Section from infected control group (II) spleen, showing marked red pulp congestion and white pulp follicular hyperplasia. (H&E, ×100) (2) Section from infected control group (II) splenic red pulp, showing intracellular tachyzoites (compound arrow) and numerous multinucleated giant cells (arrows) (H&E, ×400). Inset: a high power view of the intracellular tachyzoites. (H&E, ×1000) (3). Section from NSO-treated group (III) spleen showing red pulp congestion and marked prominence of hyperplastic white pulp follicles. (H&E, ×100) (4). Section from NSO-treated group (III) spleen showing hyperplastic white pulp follicle with reactive germinal center (arrow) (H&E, ×100) (5). Section from NSO-treated group red pulp showing multiple multinuleated giant cells (arrows) (H&E, ×400). Inset: a high power view of multinucleated giant cells (×1000) (6). Section from NSO + PYR-treated group (IV) spleen showing reduced red pulp congestion and white pulp follicular hyperplasia (H&E, ×100)
Group III mice (NSO) spleens revealed a similar changes to the infected group (Fig. 4c) only with notable prominence of white pulp follicular hyperplasia with reactive germinal centers (Fig. 4d), exhibiting frequent mitoses and numerous histiocytes with prominent phagocytosis. Fewer intracellular tachyzoite collections were encountered in the red pulp; however, numerous multinucleated giant cells were identified (Fig. 4e).
Groups IV (NSO + PYR) and V (CLN + PYR) both revealed a reduction in the white pulp follicular hyperplastic changes more pronounced in group V than group IV. The red pulp congestion and sinusoidal histiocytosis were significantly reduced in both groups (Fig. 4f), with a reduction in the number of tachyzoite collections both intra- and extracellularly.
Biochemical results
Hepatic level of MDA was significantly elevated in infected untreated mice (group II) as compared to normal untreated mice (group I). NSO-only treated mice (group III), combined NSO + PYR-treated mice (group IV), and combined CLN + PYR-treated mice (group V) showed statistically significant reductions of MDA level as compared to infected control mice (group II). However, no statistically significant difference was detected between treated mice of group III, group IV, or group V (F = 810.479, P < 0.001).
Regarding TAC, it was significantly increased in NSO-only treated mice (group III) and combined NSO + PYR-treated mice (group IV) as compared to infected untreated control mice (group II). However, combined treatment by CLN + PYR (group V) did not produce a statistically significant change in TAC level as compared to infected control mice (group II). Moreover, the TAC level of group V is statistically lower than those of group III and IV (F = 84.214, P < 0.001) (Table 2).
Immunological results
There was significant increase in the IFN-γ level in infected control mice (group II). However, NSO-only treated mice (group III) showed the highest significant IFN-γ level (295.50 ± 41.22) when both groups compared together. Comparison between the two groups receiving combined treatments (groups IV and V) revealed that NSO + PYR-treated mice (group IV) showed significantly higher level. Similarly, specific anti-Toxoplasma IgM increased significantly in infected untreated control mice (group II) compared to normal mice (group I). Also, in NSO-only treated mice (group III), IgM level increased significantly when compared to infected control mice (group II), whereas in mice receiving NSO + PYR (group IV) IgM decreased when compared to infected untreated control mice (group II) but not to a significant level. In mice receiving CLN + PYR (group V), IgM significantly decreased when compared to other infected groups (groups II, III &IV). (Table 3)
Discussion
Treatment of human infection with T. gondii remains a true challenge. Current therapeutics do not clear latent infection of the parasite and are often not satisfactory to patients. In this respect, the search for alternative drug or drug combinations with novel mechanisms of action should be pursued (Ma et al. 2013).
Since ancient times and until now, herbal medicine is being tried against different parasites (Soonwera 2014; Rivera et al. 2014; Kanojiya et al. 2015). N. sativa seeds have been used as a valuable natural resource of traditional remedies, and its oil extract (NSO) has been used to confer protection and treat several parasites. Thymoquinone (TQ) was found to be the main bioactive constituents of the volatile oil of the black seed (54 %) (Abou Basha et al. 1995). Recently, it has been proven to be a natural larvicidal agent against the fourth instar larvae of Aedes aegypti, Anopheles stephensi, and Culex quinquefasciatus (Raj et al. 2015).
In the present study, we explored the therapeutic effect of NSO alone and in combination with pyrimethamine against the virulent RH T. gondii strain. This was in comparison to the CLN and PYR combination. PYR is one of the most effective drugs against toxoplasmosis; it was used in combination with sulfadiazine (Montoya and Remington 2008). However, sulfa is highly toxic on kidneys and intolerable by most of the patients. CLN is an antimicrobial drug that inhibits protein synthesis of the apicoblasts by binding to rRNA of the large subunit; therefore, clindamycin was chosen in the current research in combination with pyrimethamine to be compared to NSO (Ni Nyoman and Lüder 2013).
Results of the current research showed that, when NSO was given alone to infected mice (group III), no significant difference in survival rate, parasite count in liver and spleen, (Table 1) nor in histopathological studies was observed when compared to infected control mice (group II). However, a significant increase in total antioxidant effect and serum IFN-γ level was observed as compared to the same group (Table 2).This can be attributed to the fact that (NSO) is a potent stimulator to Th-1 immune cells and in turn IFN-γ release, as reported by other authors (Ismael et al. 2003; Salem 2005). Although significant cytokine release, NSO, by itself, was not able to significantly ameliorate the infection and decrease the parasite count. The absence of antiparasitic effect with NSO alone was in agreement with previous studies done by Nasir et al. (2013) and Khan et al. (2013). They reported that N. sativa extracts only had no significant effect to treat balantidiasis and Cryptosporidiosis in animals. Therefore, NSO when combined with a more specific anti-Toxoplasma drug will give better results. Also, Mahmoud et al. (2002) showed promising results of NSO in treatment of schistosomiasis when combined with praziquantel, indicating that NSO potentiates the action of praziquantel.
In the present research, both groups receiving combined treatment whether NSO + PYR or CLN + PYR (group IV or V) showed significantly higher survival rates when compared to infected untreated control mice (group II), with a maximum survival time of 13 days in both groups. A significant increase in the survival rate was also reported by (Eissa et al. 2012) after vaccine trials. Rapid animal death after infection could be explained by rapid and aggressive dissemination of tachyzoites in all animal cells (Sibley et al. 2002). The tachyzoite count reached a mean of 14.86 ± 1.07 and 8.0 ± 1.81 in liver and spleen, respectively, in infected untreated control mice (group II). At the same time, a significant reduction of the tachyzoite counts in both liver and spleen was noticed with combined NSO + PYR and CLN + PYR treatment (groups IV and V) as compared to infected control mice (group II) with no significant difference between them. It is well known that PYR leads to dehydrofolate reductase inhibition and CLN clears the parasite due to inhibition of protein synthesis (Allegra et al. 1987; Martins-Duarte et al. 2013). Furthermore, CLN was proven to trigger apoptosis-like cell death of intracellular parasites (Ni Nyoman and Lüder 2013). Whereas, with NSO, through its strong enhancement of immune cells (T helper 1) counteracts the known strategies employed by Toxoplasma to inhibit T lymphocyte function which in turn leads to T cells unresponsive and exhaustion (Liu et al. 2006; Salem et al. 2011). Therefore, the effect of NSO + PYR combination on survival rate and tachyzoite counts was comparable to that of CLN + PYR (Rodrigues et al. 2014). Consistent with the immunostimulant effect of NSO (Fararh et al. 2004), DNA fragmentation and activation of the mitochondrial-signaling proapoptotic pathway may be another modes of action that were previously reported by Salim et al. (2013) in their trials for treating cancer cells with NSO. Moreover, NSO can inhibit DNA synthesis by inhibiting histone deacetylase (HDAC) enzyme in cancer cells (Vanagas et al. 2012; Zubair et al. 2013), a mode of action that needs further verification with respect to Toxoplasma.
Morphological examination of tachyzoites by light microscopy revealed slight, insignificant change in tachyzoite motility and shape. For further evaluating the effect of NSO on T. gondii tachyzoites, ultrastructural study was done. Tachyzoites obtained from infected mice treated with NSO+ PYR or CLN+ PYR (groups IV and V) showed surface abnormalities in the form of irregularities, depressions, and ridges in comparison to their corresponding infected controls (group II) (Fig. 2). Similar effects were reported by Gaafar et al. (2014) and El-Zawawy et al. (2015). Furthermore, Gaafar et al. (2014) supposed that the changes in the shape of the organisms may be secondary to changes resulting from interference of the drugs with DNA synthesis of the parasite or interference with folic acid cycle.
Histopathological studies in the present work showed that administration of either combination to mice (groups IV and V) had a marked reduction in the pathological changes observed in liver and spleen sections as compared to infected control mice (group II) and NSO-only treated mice (group III). More significant reduction was noticed in the group receiving NSO+ PYR group IV as opposed to those receiving CLN + PYR (group V). Mahmoud et al. (2002) agreed with our results when NSO was administered in combination with PZQ that achieved the most significant effect when compared to that produced by PZQ alone in treatment of schistosomiasis. On the other hand, the heavy infiltration with plasma cells and lymphocytes in NSO-only treated mice (group III) supports the immuno-stimulatory effect of NSO.
In the present study, NSO triggered marked cytokine release as shown by significant increase in IFN-γ level. The highest significant level was observed in NSO-only treated mice (group III) followed by mice receiving NSO+ PYR (group IV) when compared to infected control (group II). Cytokine release may be the key component in NSO efficacy when cell-mediated immunity is required (Salem et al. 2011). In T. gondii cellular immunity develops primarily by local Th-1 host immune responses. Our results were in agreement with Chuang and Yang (2014) who showed that the increase of IFN-γ and IgM after immunization of Toxoplasma-infected mice had the major role in their protection. It prolonged the survival time up to 15 days PI.
Since accurate mechanisms of antimicrobial effects of NSO are not clear, further studies are needed to illuminate these mechanisms.
As regards anti-Toxoplasma-specific IgM antibodies, early appearance on the 5th day post-infection was detected in infected untreated control mice (group II)a finding that is supported by Filisetti and Candolfi (2004). Its significant elevation in mice receiving NSO-only (group III) denotes the immunotherapeutic potentials that was discussed by Salem (2005). This finding coincides with Al-Suhaimi (2012) who proved that NSO increases IgM. Moreover, the decrease in IgM level with NSO + PYR may be attributed to the effective role of PYR in parasite killing guarded by the immunoprotective effect of NSO (Wang et al. 2015).
Our study revealed that hepatic MDA level was significantly elevated, while hepatic TAC level was significantly reduced in the untreated infected mice as compared to the normal healthy mice. Treatment with NSO alone or in combination with PYR (groups III and IV) resulted in a significant reduction in hepatic MDA level and a significant elevation in hepatic TAC level. These findings reflect the oxidative stress induced by T. gondii infection which is in accordance with the findings of Karaman et al. (2008) who reported an increase in MDA level and a decrease in reduced glutathione (GSH) concentration in the serum of T. gondii seropositive patients.
Findings of our study reflect the potent antioxidant effect of NSO which is consistent with the study of Ali and Blunden 2003, who reported that treatment of hyperlipidemic rabbits with NSO significantly reduced the serum lipid peroxidation marker, MDA and increased serum TAC, superoxide dismutase, and glutathione peroxidase activities. This was also confirmed and explained by Salem's study (2005) who provided clear evidence that both the NSO and its active ingredient, thymoquinone, possess reproducible anti-oxidant effects through enhancing the oxidant scavenger system, which, as a consequence, leads to antitoxic effects induced by several insults.
However, our trial revealed that treatment of T. gondii-infected mice with CLN + PYR combination (group V) significantly reduced hepatic MDA level but resulted in a non-significant change in hepatic TAC level as compared to infected untreated mice (group II). The reduction in lipid peroxidation could be attributed to PYR therapy (Sharma and Shukla 2014). On the other hand, the non-significant change in TAC level can be attributed to the pro-oxidant effect of CLN as evidenced by El-Ansary et al. (2013). Thus, from the aforementioned data, it is obvious that the addition of NSO to the therapeutic regimen of toxoplasmosis can ameliorate the accompanying oxidative stress and augment the host antioxidant potential (Mahmoudvand et al. 2014).
In conclusion, our study tried, for the first time, a novel combination therapy for treatment of toxoplasmosis. Being a very potent immunostimulant, NSO was suggested to combine with the DHFR inhibitor, PYR. The new combination succeeded to produce results similar to CLN+ PYR. NSO alone failed to produce any significant anti-Toxoplasma results except in induction of a significantly high level of IFN-γ that alone has no ability to eliminate the parasite. Whereas in combination with PYR, it produced delayed death of infected mice, significant decrease in tachyzoites number in tissues, and improvement of liver and spleen pathology in infected animals. Moreover, strong inmmunostimulant effect of NSO when added to PYR achieved best results in parasite treatment.
Further studies are recommended in order to apply this new combination on immunosuppressed infected mice followed by clinical assessment. Also, dose modification of PYR is required to reach the minimal effective dose with NSO. Moreover, NSO actions as an enzyme inhibitor and as an inducer of apoptosis worth further investigations.
Abbreviations
- T. gondii :
-
Toxoplasma gondii
- NSO:
-
Nigella sativa oil
- IFN-γ:
-
Interferon-γ
- CLN:
-
Clindamycin
- PYR:
-
Pyrimethamine
- TAC:
-
Total antioxidant capacity
References
Abou Basha L, Rashed MS, Aboul-Enein HY (1995) Thin layer chromatographic assay of thymoquinone in black seed oil and identification of dithymoquinone and thymol. J Liq Chromatogr 18:105–115
Aboul-Ela EI (2002) Cytogenetic studies on Nigella sativa seeds extract and thymoquinone on mouse cells infected with schistosomiasis using karyotyping. Mutat Res 516:11–17
Ahmed JH, Safar EH, Omar SH, Khattab HM, el-Kholy HS (1996) Toxoplasma antibodies in clinically suspected cases of toxoplasmosis. J Egypt Soc Parasitol 26:653–659
AL-Dakhil MA, Morsy TA (1996) Natural Toxoplasma infection sought in the Indian grey mongoose trapped in the eastern region, Saudi Arabia. J Egypt Soc Parasitol 26:645–652
Ali BH, Blunden G (2003) Pharmacological and toxicological properties of Nigella sativa. Phytother Res 17:299–305
Allegra CJ, Kovacs JA, Drake JC, Swan JC, Chabner BA, Masur H (1987) Potent in vitro and in vivo anti-Toxoplasma activity of the lipid-soluble antifolate trimetrexate. J Clin Invest 79:478–482
Al-Suhaimi EA (2012) Hepatoprotective and immunological functions of Nigella sativa seed oil against hypervitaminosis A in adult male rats. Int J Vitam Nutr Res 82:288–297. doi:10.1024/0300-9831/a000121
Araujo FG, Khan AA, Bryskier A, Remington JS (1998) Use of ketolides in combination with other drugs to treat experimental toxoplasmosis. J Antimicrob Chemother 42:665–667
Ayaz E, Yilmaz H, Ozbek H, Tas Z, Orunc O (2007) The effect of Nigella sativa oil against Aspiculuris tetraptera and Hymenolepis nana in naturally infected mice. Saudi Med J 28:1654–1657
Chan J, Luft BJ (1986) Activity of roxithromycin (RU 28965), macrolide, against Toxoplasma gondii infections in mice. Antimicrob Agents Chemother 30:323–324
Chuang SC, Yang CD (2014) Sustained release of recombinant surface antigen 2 (rSAG2) from poly (lactide-co-glycolide) microparticles extends protective cell-mediated immunity against Toxoplasma gondii in mice. Parasitology 18:1–10, http://www.ncbi.nlm.nih.gov/pubmed/?term=Sustained+release+of+recombinant+surface+antigen+2+(rSAG2)+from+poly+(lactide-co-glycolide)+microparticles+extends+protective+cell-mediated+immunity+against+Toxoplasma+gondii+in+mice.+Parasitology+18%3A1-10
Drury RAB, Wallington EA (1980) Carleton’s histological technique, 5th edn. Oxford University Press, Oxford, New York, Toronto
Dupont CD, Christian DA, Hunter CA (2012) Immune response and immunopathology during toxoplasmosis. Semin Immunopathol 34:793–813
Eissa MM, El-Azzouni MZ, Mady RF, Fathy FM, Baddour NM (2012) Initial characterization of an autoclaved Toxoplasma vaccine in mice. Exp Parasitol 131:310–316
El Wakil SS (2007) Evaluation of the in vitro effect of Nigella sativa aqueous extract on Blastocystis hominis isolates. J Egypt Soc Parasitol 37:801–813
El-Ansary AK, Al-Daihan S, Ben Bacha A, Shaker GH, Al-Ayadhi LY (2013) Comparative study on the protective effect of carnosine and carnitine against pro-inflammatory/pro-oxidant effects of clindamycin and propionic acid administrations to hamsters. Afr J Microbiol Res 7:103–114
El-Fakhry Y, Achbarou A, Desportes I, Mazier D (1998) Encephalitozoon intestinalis: humoral responses in interferon-y receptor knockout mice infected with a microsporidium pathogenic in AIDS patients. Exp Parasitol 89:113–121
El-Zawawy LA, El-Said D, Mossallam SF, Ramadan HS, Younis SS (2015) Triclosan and triclosan-loaded liposomal nanoparticles in the treatment of acute experimental toxoplasmosis. Exp Parasitol 149:54–64. doi:10.1016/j.exppara.2014.12.007
Fararh KM, Atoji Y, Shimizu Y, Shiina T, Nikami H, Takewaki T (2004) Mechanisms of the hypoglycaemic and immunopotentiating effects of Nigella sativa L. oil in streptozotocin-induced diabetic hamsters. Res Vet Sci 77:123–129
Filisetti D, Candolfi E (2004) Immune response to Toxoplasma gondii. Ann Ist Super Sanita 40:71–80
Gaafar MR, Mady RF, Diab RG, Shalaby TI (2014) Chitosan and silver nanoparticles: promising anti-Toxoplasma agents. Exp Parasitol 143:30–38. doi:10.1016/j.exppara.2014.05.005
Giarcia LS, Bruckner DA (1977) Macroscopic and microscopic examination of fecal specimens. In: Diagnostic medical parasitology, 3rd edn. ASM Press, Washington, DC, pp 608–649
Ismael AB, Sekkai D, Collin C, Bout D, Mévélec MN (2003) The MIC3 gene of Toxoplasma gondii is a novel potent vaccine candidate against toxoplasmosis. Infect Immun 71:6222–6228
Kanojiya D, Shanker D, Sudan V, Jaiswal AK, Parashar R (2015) In vitro and in vivo efficacy of extracts of leaves of Eucalyptus globulus on ovine gastrointestinal nematodes. Parasitol Res 114(1):141–148
Karaman U, Celik T, Kiran TR, Colak C, Daldal NU (2008) Malondialdehyde, glutathione, and nitric oxide levels in Toxoplasma gondii seropositive patients. Korean J Parasitol 46:293–295
Katlama C, Mouthon B, Gourdon D, Lapierre D, Rousseau F (1996) Atovaquone as long-term suppressive therapy for toxoplasmic encephalitis in patients with AIDS and multiple drug intolerance. Atovaquone Expanded Acess Group. AIDS 10(10):1107–1112
Keyhanmanesh R, Boskabady MH, Khamneh S, Doostar Y (2010) Effect of thymoquinone on the lung pathology and cytokine levels of ovalbumin-sensitized guinea pigs. Pharmacol Rep 62:910–916
Khan A, Khan MS, Avais M, Ijaz M, Ali MM, Abbas T (2013) Prevalence, hematology, and treatment of balantidiasis among donkeys in and around Lahore, Pakistan. Vet Parasitol 196:203–205
Klainer AS, Betsch CJ (1970) Scanning beam electron microscopy selected microorganisms. J Infect Dis 121:339–343
Koracevic D, Koracevic G, Djordjevic V, Andrejevic S, Cosic V (2001) Method for the measurement of antioxidant activity in human fluids. J Clin Pathol 54:356–361
Leslie E, Geoffrey J and James M (eds) (1991) Statistical analysis. In: Interpretation and uses of medical statistics (4th ed). Oxford Scientific Publications (pub) 411–416
Liu KY, Zhang DB, Wei QK, Li J, Li GP, Yu JZ (2006) Biological role of surface Toxoplasma gondii antigen in development of vaccine. World J Gastroenterol 12:2363–2368
Ma CI, Diraviyam K, Maier ME, Sept D, Sibley LD (2013) Synthetic chondramide A analogues stabilize filamentous actin and block invasion by Toxoplasma gondii. J Nat Prod 76:1565–1572
Mahmoud MR, El-Abhar HS, Saleh S (2002) The effect of Nigella sativa oil against the liver damage induced by Schistosoma mansoni infection in mice. Ethnopharmacol 79:1–11
Mahmoudvand H, Dezaki ES, Kheirandish F, Ezatpour B, Jahanbakhsh S, Harandi MF (2014) Scolicidal effects of black cumin seed (Nigella Sativa) essential oil on hydatid cysts. Korean J Parasitol 52:653–659. doi:10.3347/kjp.2014.52.6.653
Mahmoudvand H, Tavakoli R, Sharififar F, Minaie K, Ezatpour B, Jahanbakhsh S et al (2015) Leishmanicidal and cytotoxic activities of Nigella sativa and its active principle, thymoquinone. Pharm Biol 53(7):1052–1057
Martins-Duarte ÉS, de Souza W, Vommaro RC (2013) Toxoplasma gondii: the effect of fluconazole combined with sulfadiazine and pyrimethamine against acute toxoplasmosis in murine model. Exp Parasitol 133:294–299. doi:10.1016/j.exppara.2012.12.011, http://www.ncbi.nlm.nih.gov/pubmed/?term=Martins-Duarte+%C3%89S%2C+de+Souza+W%2C+Vommaro+RC+(2013)+Toxoplasma+gondii%3A+the+effect+of+fluconazole+combined+with+sulfadiazine+and+pyrimethamine+against+acute+toxoplasmosis+in+murine+model.+Exp+Parasitol+133%3A294-299.+doi%3A+10.1016
Montoya JG, Remington JS (2008) Management of Toxoplasma gondii infection during pregnancy. Clin Infect Dis 47:554–566
Nasir A, Avais M, Khan MS, Khan JA, Hameed S, Reichel MP (2013) Treating Cryptosporidium parvuminfection in calves. J Parasitol 99:715–717
Ni Nyoman AD, Lüder CG (2013) Apoptosis-like cell death pathways in the unicellular parasite Toxoplasma gondii following treatment with apoptosis inducers and chemotherapeutic agents: a proof-of-concept study. Apoptosis 18:664–680. doi:10.1007/s10495-013-0832-8
Ohkawa H, Ohishi N, Yagi K (1979) Assay of lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
Okeola VO, Adaramoye OA, Nneji CM, Falade CO, Farombi EO, Ademowo OG (2011) Antimalarial and antioxidant activities of methanolic extract of Nigella sativa seeds (black cumin) in mice infected with Plasmodium yoelli nigeriensis. Parasitol Res 108:1507–1512. doi:10.1007/s00436-010-2204-4
Padhye S, Banerjee S, Ahmad A, Mohammad R, Sarkar FH (2008) From here to eternity - the secret of pharaohs: therapeutic potential of black cumin seeds and beyond. Cancer Ther 6:495–510
Pappas G, Roussos N, Falagas ME (2009) Toxoplasmosis snapshots: global status of Toxoplasma gondii seroprevalence and implications for pregnancy and congenital toxoplasmosis. Int J Parasitol 39:1385–1394
Park YH, Nam HW (2013) Clinical features and treatment of ocular toxoplasmosis. Korean J Parasitol 51:393–399
Raj GA, Chandrasekaran M, Krishnamoorthy S, Jayaraman M, Venkatesalu V (2015) Phytochemical profile and larvicidal properties of seed essential oil from Nigella sativa L. (Ranunculaceae), against Aedes aegypti, Anopheles stephensi, and Culex quinquefasciatus (Diptera: Culicidae). Parasitol Res 114(9):3385–3391
Rivera N, López PY, Rojas M, Fortoul TI, Reynada DY, Reyes AJ et al (2014) Antimalarial efficacy, cytotoxicity, and genotoxicity of methanolic stem bark extract from Hintonia latiflora in a Plasmodium yoelii yoelii lethal murine malaria model. Parasitol Res 113(4):1529–1536
Rodrigues V, Cordeiro-da-Silva A, Laforge M, Ouaissi A, Akharid K, Silvestre R et al (2014) Impairment of T cell function in parasitic infections. PLoS Negl Trop Dis 8, e2567. doi:10.1371/journal.pntd.0002567
Romand S, Pudney M, Derouin F (1993) In vitro and in vivo activities of the hydroxyl naphthoquinone atovaquone alone or combined with pyrimethamine, sulfadiazine, clarithromycin, or minocycline against Toxoplasma gondii. Antimicrob Agents Chemother 37:2371–2378
Rosowsky A, Papoulis AT, Queener SF (1998) 2,4-Diamino-67-dihydro-5H-cyclopenta[d]pyrimidine analogues of trimethoprim as inhibitors of Pneumocystis carinii and Toxoplasma gondii dihydrofolate reductase. J Med Chem 41(6):913–918
Salem ML (2005) Immunomodulatory and therapeutic properties of the Nigella sativa L. seed. Int Immunopharmacol 5:1749–1770
Salem ML, Alenzi FQ, Attia WY (2011) Thymoquinone, the active ingredient of Nigella sativa seeds, enhances survival and activity of antigen-specific CD8-positive T cells in vitro. Br J Biomed Sci 68:131–137
Salim LZ, Mohan S, Othman R, Abdelwahab SI, Kamalidehghan B, Sheikh BY et al (2013) Thymoquinone induces mitochondria-mediated apoptosis in acute lymphoblastic leukaemia in vitro. Molecules 18:11219–11240. doi:10.3390/molecules180911219, http://www.ncbi.nlm.nih.gov/pubmed/?term=Salim+LZ%2C+Mohan+S%2C+Othman+R%2C+Abdelwahab+SI%2C+Kamalidehghan+B%2C+Sheikh+BY%2C+et+al+(2013)+Thymoquinone+induces+mitochondria-mediated+apoptosis+in+acute+lymphoblastic+leukaemia+in+vitro
Shalaby HA, El-Moghazy FM (2013) In vitro effect of Nigella sativa oil on adult Toxocara vitulorum. Pak J Biol Sci 16:1557–1562
Sharma L, Shukla G (2014) Treatment of pregnant BALB/c mice with sulphadoxine pyrimethamine or chloroquine abrogates Plasmodium berghei induced placental pathology. Parasitol Int 63:49–56
Sibley LD, Mordue DG, Su C, Robben PM, Howe DK (2002) Genetic approaches to studying virulence and pathogenesis in Toxoplasma gondii. Philos Trans R Soc Lond B Biol Sci 357:81–88
Soonwera M (2014) Efficacy of herbal shampoo base on native plant against head lice (Pediculus humanus capitis De Geer, Pediculidae: Phthiraptera) in vitro and in vivo in Thailand. Parasitol Res 113(9):3241–3250
Stoicov C, Whary M, Rogers AB, Lee FS, Klucevesk K, Li HC et al (2004) Coinfection modulates inflammatory responses and clinical outcome of Helicobacter felis and Toxoplasma gondii infections. J Immunol 173:3329–3336
Sturge CR, Benson A, Raetz M, Wilhelm CL, Mirpuri J, Vitetta ES, Yarovinsky F (2013) TLR-independent neutrophil-derived IFN-γ is important for host resistance to intracellular pathogens. Proc Natl Acad Sci U S A 110(26):10711–10716. doi:10.1073/pnas.1307868110
Suzuki Y, Orellana MA, Schreiber RD, Remington JS (1988) Interferon-gamma: the major mediator of resistance against Toxoplasma gondii. Science 240:516–518
Taylor GA, Feng CG, Sher A (2004) GTPases: regulators of immunity to intracellular pathogens. Nat Rev Immunol 4:100–109
Theise ND (2007) Liver biopsy assessment in chronic viral hepatitis: a personal, practical approach. Mod Pathol 20:3–14
Vanagas L, Jeffers V, Bogado SS, Dalmasso MC, Sullivan WJ Jr, Angel SO (2012) Toxoplasma histone acetylation remodelers as novel drug targets. Expert Rev Anti-Infect Ther 10:1189–1201. doi:10.1586/eri.12.100
Wang S, Hassan IA, Liu X, Xu L, Yan R, Song X et al (2015) Immunological changes induced by Toxoplasma gondii Glutathione-S-Transferase (TgGST) delivered as a DNA vaccine. Res Vet Sci 99:157–164. doi:10.1016/j.rvsc.2014.12.006
Zubair H, Khan HY, Sohail A, Azim S, Ullah MF, Ahmad A et al (2013) Redox cycling of endogenous copper by thymoquinone leads to ROS-mediated DNA breakage and consequent cell death: putative anticancer mechanism of antioxidants. Cell Death Dis 4, e660. doi:10.1038/cddis.2013.172
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mady, R.F., El-Hadidy, W. & Elachy, S. Effect of Nigella sativa oil on experimental toxoplasmosis. Parasitol Res 115, 379–390 (2016). https://doi.org/10.1007/s00436-015-4759-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00436-015-4759-6