Abstract
Purpose
NRAS plays a pivotal role in progression of various kinds of somatic malignancies; however, the correlation between NRAS and lung adenocarcinoma is less known. We aim to analyze the prognostic value of NRAS expression in lung adenocarcinoma, and explore the relationship between NRAS and tumor immune microenvironment.
Methods
We obtained the transcriptome profiles and clinical data of LUAD from The Cancer Genome Atlas database and three Genome Expression Omnibus datasets. Specimens from 325 patients with completely resected lung adenocarcinoma were collected for immunohistochemical assays of NRAS, PD-L1, PD-1 and TIM-3. Then, we performed gene set enrichment analysis to investigate cancer-related and immune-related signaling pathways. TIMER algorithms were performed to evaluate tumor immune infiltrating cells and immune-related biomarkers.
Results
Compared with adjacent non-tumor tissue, NRAS expression was significantly upregulated in LUAD tissue. NRAS expression was significantly correlated with more advanced stage and positive lymph nodes. Kaplan–Meier curves and Cox analysis suggested that high NRAS expression led to a poor prognosis, and could be an independent prognostic factor in LUAD patients. Besides, NRAS expression was positively correlated with CD8+ T cells, macrophages, and neutrophils, and negatively correlated with B cells and CD4+ T cells. The expression level of NRAS was positively correlated with PD-L1, PD-1, and TIM-3 both at RNA and protein level.
Conclusions
To conclude, we found NRAS is a novel prognostic biomarker in LUAD. Besides, the expression level of NRAS may influence the prognosis of LUAD via various kinds of cancer-related pathways and remodeling TIM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer remains the leading cause of cancer-related death and has the highest incidence rate worldwide (Bray et al. 2018). Among all the histological subtypes of lung cancer, lung adenocarcinoma (LUAD) is the one which dominant, with an average 5-year survival rate of 15% (Siegel et al. 2017). Over the past decades, advances in high-throughput sequencing techniques have expanded our knowledge about gene expression and genetic alterations at the pan-genomic level in various somatic malignancies. Numerous large-scale studies have demonstrated that different genetic subtypes have distinctive survival rates in malignancies (Liloglou et al. 2014) (Vogelstein et al. 2013). Therefore, identifying genetic biomarkers were in great need to predict prognosis of LUAD.
Neuroblastoma rat sarcoma viral oncogene homolog (NRAS) was originally identified as the third RAS family member following KRAS and HRAS in human neuroblastoma and fibrosarcoma cell lines (Shimizu et al. 1983). Akin to KRAS, NRAS encodes small GTP enzymes which regulate cell cycle, proliferation, maturation and differentiation by transducing signals from membrane-localized receptor tyrosine kinases to the nucleus. The mutation of RAS gene family occurs in nearly 30% of human cancers (Downward 2003). NRAS plays an important role in EGFR mediating RAS/RAF/MEK/ERK and PI3K/AKT/mTOR signaling pathways (Whitwam et al. 2007). The mutation of NRAS leads to continuous activation of Ras-GTP, which promotes tumorigenesis and metastasis. It has been proved that NRAS acts as a negative prognosis predictor in numerous somatic malignancies, such as melanoma, colorectal cancer and hepatocellular carcinoma (Banys-Paluchowski et al. 2020; Bertoli et al. 2019; Dietrich et al. 2019; Hu et al. 2018).
Besides, NRAS, as a proto-oncogene, is also proved to be associated with tumor immune microenvironment (TIM) both in vivo and in vitro. Pérez de Castro et al. (2003) has found that NRAS GTPase is related to T-cell proliferation and immune response. Thomas et al. (2015) indicates that NRAS mutation in advanced melanoma is correlated with increased benefit from immunotherapy. TIM has already been recognized as an essential factor in cancer progression. Its prognostic value has been proven in LUAD (Brambilla et al. 2016; Suzuki et al. 2011). For instance, Brambilla et al. (2016) demonstrate that higher CD4+/CD8+ ratio conferred a better survival of patients suffering from lung cancer. Besides, tumor mutation burden and expression level of PD-L1 have been widely used to predict outcomes in lung cancer patients receiving immunotherapy.
Till now, there is only one multi-institutional study, which has initially explored the relationship between NRAS mutations and lung cancer. This report indicates that LUAD patients with NRAS mutations may have potential sensitivity to MEK inhibitors (Ohashi et al. 2013). Unfortunately, the correlation between NRAS and LUAD is still unclear. Therefore, NRAS seems to be a logic alternative to investigate for potential novel biomarkers in LUAD.
In this study, we analyzed the prognostic value of NRAS in LUAD based on public databases and tumor microarrays of 325 patients with LUAD. In addition, we explored the relationship between NRAS and tumor immune microenvironment both at RNA and protein level, together with potential molecular mechanisms underlying NRAS function in LUAD.
Methods
Tissue samples
LUAD patient datasets, with transcriptome profile and clinical information, were obtained from the public online datasets TCGA LUAD (http://portal.gdc.cancer.gov/), including 497 LUAD tumor tissues and 54 adjacent non-malignant lung tissues. Furthermore, three lung cancer chips GSE50081 (including 181 NSCLC tumor samples, GPL570 [HG-U133_Plus_2] Affymetrix Human Genome U133 Plus 2.0 Array), GSE42127 (176 lung cancer samples, GPL6884 Illumina HumanWG-6 v3.0 expression beadchip), and GSE30219 (293 lung cancer samples and 14 non-tumor lung samples, GPL570 [HG-U133_Plus_2] Affymetrix Human Genome U133 Plus 2.0 Array) were downloaded from Gene Expression Omnibus (GEO) database (https://www.ncbi.nlm.nih.gov/geo/) for a valid confirmation.
The cohort to perform immunohistochemical (IHC) tissue microarray (TMA) consisted of 325 LUAD patients from Fudan University Shanghai Cancer Center (FDUSCC) diagnosed between 2009 and 2015. All these samples were obtained after surgical resection from patients who had never received neoadjuvant therapy.
IHC expression achieved from the Human Protein Atlas
IHC staining images were achieved from the Human Protein Atlas (HPA) (http://www.proteinatlas.org/) to validate the expression of NRAS in LUAD and adjacent non-tumor tissues (Uhlén et al. 2015). Both the tumor tissues and normal tissues were stained by Antibody CAB010157. The staining location was cytoplasmic and membranous. The direct links to these images are as follows:
LUAD tissue: https://www.proteinatlas.org/ENSG00000213281-NRAS/pathology/lung+cancer#img
Normal lung: https://www.proteinatlas.org/ENSG00000213281-NRAS/tissue/lung#img
IHC staining and evaluation of IHC intensity
Formalin-fixed paraffin-embedded primary specimens of patients with LUAD were obtained to construct 4-μm-thick sections. IHC staining was performed as previously described (Fu et al. 2021). Immunostaining analysis was independently evaluated by Yan and Gao who were to the experimental groups using immunoreactive score (IRS). The staining intensity was graded 4 levels (no staining = 0, weak staining = 1, moderate staining = 2, and strong staining = 3) and the staining extent was graded 5 levels (no = 0, < 10% = 1, 10–50% = 2, 51–80% = 3, and > 80% = 4). The scores of the staining intensity and extent were multiplied to give a final staining score of 0–12. The cutoff for IRS of NRAS was 6. Antibodies against the NRAS (ab77392, 1:500, Abcam), PD-L1 (E1L3N, 1:1000, Cell Signaling Technology), TIM-3(D5D5R, 1:1000, Cell Signaling Technology), and PD-1 (DW42J, 1:500, Cell Signaling Technology) were used.
Correlation analysis between NRAS expression and immune cell infiltration in LUAD
Tumor immune estimation resource (TIMER 2.0) (http://timer.cistrome.org/), a useful online tool for comprehensive analysis of tumor-infiltrating immune cells (TIICs) (Li et al. 2020), was used to evaluate the relationship between NRAS expression and TIICs in LUAD. The level of TIICs is an essential indicator reflecting TIM. In addition, we analyze the correlation between immune-related functional molecular and NRAS via TIMER website. The TIIC and immune-related molecular levels of LUAD patients from TCGA datasets were derived from TIMER website.
Gene sets enrichment analysis (GSEA)
A computational method that determines the statistical significance of a priori defined set of genes and the existence of concordant differences between two biological states is known as the GSEA (Subramanian et al. 2007). In this study, GSEA 4.0.3 generated an initial gene list on the classification of the genes according to their correlation with the NRAS expression. For each analysis, we performed 1000 repetitions of gene set permutations. The phenotype label that we put forth was the expression level of NRAS. In addition, to sort the enriched pathways in each phenotype, we utilized the nominal p value and normalized enrichment score (NES) (Subramanian et al. 2005). Gene sets with false-discovery rate (FDR) < 0.25 and nominal p value < 0.05 were considered to be significantly enriched. The gene sets were enriched and analyzed by Hallmark (h.all.v6.2.symbols.gmt) and Go (c5.bp.v6.2.symbols.gmt) Collection.
Statistical analysis
Statistical analysis was performed using R-3.6.1. (R Foundation for Statistical Computing, Vienna, Austria) Group comparison analyses with continuous variables were evaluated by Wilcox T test. The correlation between expression of NRAS and clinical features was performed with logistic analysis. Kaplan–Meier survival curves and log-rank test were applied to compare survival outcomes. Finally, univariate and multivariable Cox analyses were used to identify independent prognostic predictors. A statistical difference was taken as two-sided p value < 0.05.
Results
Demographics of population in TCGA LUAD datasets
Four hundred and ninety-seven LUAD patients with both clinical and transcriptome profiling were downloaded from TCGA LUAD datasets. After excluding those with missing or insufficient data on age, gender or stage, we included 316 patients to further examine the prognostic role by Cox analysis and Logistic regression. We also included 325 LUAD patients from FDUSCC diagnosed between 2009 and 2015 to perform IHC microarrays. The baseline characteristics of these two cohorts are presented in Table 1. Except for one patient with NRAS synonymous mutations, three people have NRAS mutations in TCGA cohort. The genetic status of NRAS for these patients is described in Table S1. As shown in Fig. S1, we found that patients with NRAS mutations expressed higher levels of NRAS than those without NRAS mutations (p = 0.027).
Correlations between the clinical information and NRAS were analyzed by logistic analyses in TCGA cohort. The categorical dependent value is based on the median value NRAS expression. As shown in Table 2, high expression of NRAS in LUAD was significantly associated with advanced stage (stage I vs stage III, OR = 1.90 (1.14–3.21), p = 0.0059) and positive lymph nodes (positive vs negative, OR = 2.00 (1.26–3.20), p = 0.0037).
NRAS expression is upregulated in LUAD specimens
Wilcox T test was performed to estimate the relationship between NRAS expression and disease status of LUAD based on TCGA datasets. As shown in Fig. 1A, the expression of NRAS was significantly upregulated in LUAD samples compared with normal samples (p = 3.85e−04). Meanwhile, we paired the tumor tissue and adjacent tumor tissue of the same patient from TCGA LUAD datasets. The pair analysis shown in Fig. 1B indicated the same results as the former (p = 5.19e−05). 11 LUAD tissue and 3 normal tissue IHC images were obtained from the HPA website. The staining intensity of LUAD tissue was medium-strong (2 of 11 were strong), while that of normal pneumocytes was weak. As shown in Fig. 1C and E (intensity: strong, staining: high, quantity > 75%), the tumor cells were intensely stained. As shown in Fig. 1D and F (Macrophage: intensity: medium, staining: moderate, quantity: > 75%; pneumocyte: intensity: weak, staining: low, quantity: 75–25%), the intensity of macrophage staining is moderate, and that of pneumocytes is weak in normal tissues. This indicates that NRAS acts as a pivotal role in LUAD progression.
Lung adenocarcinoma (LUAD) highly expressing NRAS. A The expression of NRAS was significantly upregulated in LUAD compared with normal cells. B The pair analysis indicated that NRAS expression was significantly upregulated in LUAD. C Representative Immunohistochemical (IHC) staining for NRAS in LUAD tissue was performed. D Representative IHC staining for NRAS in normal tissue was performed. E IHC (200 ×) staining for NRAS in LUAD tissue. F IHC (200 ×) staining for NRAS in normal tissue
NRAS expression predicted survival and could be used as an independent prognostic biomarker in LUAD patients
Patients were divided into high expression group and low expression group according to the median value of NRAS expression. As shown in Fig. 2A, Kaplan–Meier survival analysis shows that high NRAS expression group has a significantly poorer overall survival (OS) compared with low expression group. The univariable analysis shown in Table 3a reveals that NRAS expression correlated significantly with a poor OS. Besides, clinical stage, tumor size and lymph nodes are significantly associated with OS. According to multivariable analysis (Fig. 2B and Table 3b), the expression level of NRAS remains independently associated with OS (p = 0.012). Besides, we verified the prognostic value of NRAS at the protein level. We evaluated the protein level of NRAS in completely resected tissues using TMA. A total of 325 LUAD patients, undergoing surgical resection in Fudan University Shanghai Cancer Center, were enrolled in this study. According to the IRS of IHC staining, we defined 0–6 as weak staining group, and 7–12 as high staining group. The representative IHC images of NRAS are shown in Fig. 2D. As shown in Fig. 2C, higher expression of NRAS is also associated with worse OS at the protein level (p = 0.0072).
NRAS is associated with poor prognosis in LUAD patients at RNA and protein level. A Kaplan–Meier curve to compare the overall survival of LUAD patients between high and low NRAS expression group based on TCGA databases. B Multivariable Cox analysis of NRAS expression and other clinicopathological factors for LUAD patients. C Kaplan–Meier Curve of overall survival according to protein expression of NRAS in patients with LUAD. D Representative images of IHC for strong and weak staining of NRAS in LUAD specimens. The cutoff for the IRS score of NRAS was 6
The prognostic value of NRAS in LUAD was also verified by three GEO datasets GSE50081 (including 181 LUAD samples), GSE42127 (176 LUAD samples), and GSE30219 (293 LUAD samples). Since each dataset used different genetic chips and algorithms, the cutoff value to divide patients into high or low expression group was based on the median value of NRAS expression in each dataset. As shown in Fig. S2 (GSE50081: p = 0.028, GSE42127: p = 0.0078, GSE30219: p = 0.0026), we performed Kaplan–Meier survival analyses as a validation. Hence, NRAS expression level could be an independent prognostic factor for patients with LUAD.
GSEA identified NRAS-related signaling pathways
To further study the signaling pathways that NRAS might be involved in, we performed a GSEA between high and low NRAS expression phenotypes. The gene sets were enriched and analyzed by Hallmark (h.all.v6.2.symbols.gmt) and Go (c5.bp.v6.2.symbols.gmt) Collection.
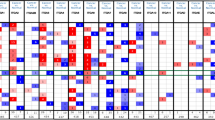
Eleven Hallmark items (Fig. 3A) including G2M checkpoint, E2F targets, DNA repair, P13K AKT MTOR signaling, MTORC1 signaling pathways were significantly enriched in NRAS high expression phenotype. According to the enrichment of Go Collection (Fig. 3B and C), high NRAS expression gene sets were significantly correlated with 12 immune-related signaling pathways such as activation of innate immune response, negative regulation of B-cell proliferation and T-cell regulation signaling pathway. There is no signal pathways with low expression in NRAS enriched in neither GO nor Hallmark Collection based on NES, NOM P value, and FDR q value.
A 11 signaling pathways including G2M checkpoint, E2F targets, MTORC1 signaling, PI3K-AKT-MTOR signaling, MYC Targets V1, and DNA repair were enriched in Hallmark collection. B 12 signaling pathways including activation of innate immune response, negative regulation of B-cell proliferation and T-cell regulation signaling pathway were significantly enriched in GO collection. C A merged enrichment plot from gene set enrichment analysis including enrichment score and gene sets based on GO collection
Correlation analysis between NRAS and TIM in LUAD
We estimated the relationship between the abundance of TIICs and NRAS expression via the TIMER algorithm. The results shown in Fig. 4A indicates that the expression of NRAS was positively correlated with CD8+ T cells (cor = 0.27, p = 1.06e−09), macrophages (cor = 0.331, p = 4.06e−14), and neutrophils (cor = 0.373, p = 8.81e−18), while it was negatively correlated with B cells (cor = − 0.216, p = 1.31e−0.6) and CD4+ T cells (cor = − 0.108, p = 1.65e−02). In addition, we analyzed the correlation between immune-related biomarkers and NRAS expression. As shown in Fig. 4B, NRAS expression was positively correlated with CD274 (rho = 0.333, p = 8.59e−15), HAVCR2 (rho = 0.239, p = 4.01e−08), PDCD1 (rho = 0.101, p = 2.16e−02), CD47 (rho = 0.189, p = 1.64e−05) and CD24 (rho = 0.227, p = 1.82e−07). The results shown in Fig. 4C–E validated the correlation between NRAS and immune-related biomarkers at the protein level via IHC staining of TMAs. Analyzing the IRS score of these immune-related molecules between the NRAS strong staining group and weak staining group, we found that the IRS of PD-L1 (p = 6.24e−3), PD-1 (p = 1.37e−04), and TIM-3 (p = 2.47e−10) were significantly higher in NRAS strong staining group than weak group. The representative stainings are performed in Fig. S3.
NRAS expression is associated with tumor immune microenvironment. A NRAS expression level has significant negative correlations with infiltrating levels of CD8+ T cells (cor = 0.27, p = 1.06e−09), macrophages (cor = 0.331, p = 4.06e−14), and neutrophils (cor = 0.373, p = 8.81e−18), while it was negatively correlated with B cells (cor = -0.216, p = 1.31e−0.6) and CD4+ T cells (cor = -0.108, p = 1.65e−02). B NRAS expression was positively correlated with CD274 (rho = 0.333, p = 8.59e−15), HAVCR2 (rho = 0.239, p = 4.01e−08), PDCD1 (rho = 0.101, p = 2.16e−02), CD47 (rho = 0.189, p = 1.64e−05) and CD24 (rho = 0.227, p = 1.82e− 07). C IRS of PD-L1 was significantly higher in high NRAS expression group at protein level (p = 6.24e−3). D IRS of PD-1 was significantly higher in high NRAS expression group at protein level (p = 1.37e−04). E IRS of TIM-3 was significantly higher in high NRAS expression group at protein level (p = 2.47e−10)
Discussion
NRAS, a gene identified in neuroblastoma and fibrosarcoma cell lines, encodes GTPases involved in cell cycle, proliferation, and differentiation (Shimizu et al. 1983). As a member of the RAS gene family, similar with KRAS, NRAS plays an essential role in tumorigenesis and progression in various kinds of neoplasms. At present, KRAS has been proved strongly as a significant biomarker in the prognosis of NSCLC, (Ma et al. 2020) while the relationship between NRAS and lung cancer remains unclear. Thus far, only one multi-institutional study has initially explored the correlation between NRAS mutation and NSCLC (Ohashi et al. 2013). The potential prognostic value of NRAS for LUAD had not been evaluated due to lack of NRAS-mutated patients. Hence, we performed a first-ever analysis on the NRAS expression in a large cohort of LUAD based on bioinformatics analysis and real world data. We sought to determine the relationship between NRAS and LUAD, especially as a prognostic biomarker in LUAD. Besides, we tried to screen NRAS-related signaling pathways, TIIC levels and immune biomarkers to seek out the potential molecular mechanisms involved in the regulation of LUAD progression and TIM by NRAS.
Based on the transcriptome profiles of TCGA cohort, we found patients with NRAS mutations expressed higher levels of NRAS than those without NRAS mutations. Activated mutation of NRAS might probably upregulate its own expression level. However, there were only three LUAD patients with NRAS non-synonymous mutation in the TCGA cohort. Hence, other independent patient cohorts with larger sample size will still be needed for a further validation in the future. At present, several studies have shown that the NRAS expression level is associated with the progression of lung cancer via in vivo and in vitro experiments. Giannou et al. (2017) performed RNA interference and RNA overexpression to modulate NRAS expression level in LUAD cell lines and mouse models, and found that NRAS expression was closely related to LUAD metastasis. Liu et al. (2018) found targeting NRAS was associated with cisplatin sensitivity in the treatment of lung cancer cell lines. In this study, we provided clinicopathological evidence supporting the role of NRAS expression in development and progression of LUAD. We discovered NRAS expression upregulated in LUAD tissues. High NRAS expression group was positively correlated with advanced clinical stage and positive lymph nodes, and caused a worse prognosis both at RNA level and protein level.
Exploring the molecular mechanisms of NRAS in LUAD is beneficial for further investigation of the novel targeted therapy approach. The enrichment analysis of Hallmark collection showed protein secretion, PI3K/Akt/mTOR signaling, MYC targets, mTORC1 signaling, G2/M checkpoint, E2F targets and DNA repairing pathways were significantly enriched in high expression phenotype. G2/M checkpoint, E2F transcription factor and DNA repairing pathways were closely related to the cell cycle, proliferation and apoptosis. The gene imbalance in these pathways might induce chemotherapy resistance and influence drug sensitivity. Numerous studies reported the potential advantages of cell cycle inhibitors as a group of effective anticancer agents in lung cancer. Whether NRAS could be used as a biomarker for the application of cell cycle inhibitors required more experiments to validate. PI3K/Akt/mTOR, MYC, and mTORC1 signaling pathways were closely related to RAS/RAF cascade. Whitwam et al. (2007) reported that NRAS prevented phosphorylation of MYC through PI3K/AKT/mTOR signaling pathway, leading to enhanced activity of endogenous MYC protein. Song et al. (2017) found that targeting NRAS-regulated MAPK cascade, including RAF, MEK, and ERK, by MEK inhibitors could delay tumor growth and angiogenesis in lung cancer. Thus, the enrichment of cancer-related pathways indicated that NRAS might be a potential target for personalized therapy of LUAD.
According to the enrichment of GO collection, we discovered that NRAS expression is associated with TIM. High expression level of NRAS is significantly correlated with 12 immune-related signaling pathways. To further study the relationship between NRAS expression and TIM, we estimated the abundance of TIIC level via the TIMER algorithm. NRAS expression was negatively correlated with the infiltration level of B cell and CD4+ T cell and positively related that of CD8+ T cell, macrophage and neutrophil in LUAD. The GSEA performed on GO collections indicated that high NRAS expression was enriched in activation of innate immune response, negative regulation of B-cell proliferation and T-cell regulation signaling pathway, which was consistent with the results of TIIC analysis. Brambilla et al. (2016) found lower CD4+/CD8+ ratio conferred a worse survival in non-small cell lung cancer. In addition, multiple studies had proven that CD 20+ B cell was associated with improved survival (Al-Shibli et al. 2008; Pelletier et al. 2001). Prognostic role of tumor-associated macrophages in lung cancer had still been controversial (Chen et al. 2003; Ho et al. 2008; Kim et al. 2008; Zeni et al. 2007). Besides, by comparing the relationship between NRAS and immune-related functional molecules, we found NRAS expression was positively correlated with CD274, HAVCR2, PDCD1, CD47 and CD24. CD274 encodes PD-L1, HAVCR2 encodes TIM-3, and PDCD1 encodes PD-1 (Dong et al. 1999; Ishida et al. 1992; McIntire et al. 2001). We also performed IHC staining in primary LUAD tissues from 325 patients to validate the correlation between NRAS and these immune-related biomarkers. The close relationship between NRAS expression and the immunosuppressive molecules indicated that NRAS might be involved in immune evasion and suppression of immune function in LUAD. Both CD47 and CD24 have been proven as ‘don’t eat me’ signals, which are expressed by tumor-associated macrophages. Cancer cells are expertise in evading clearance by macrophages via the overexpression of such anti-phagocytic molecular as CD47 and CD24 (Barkal et al. 2019; Willingham et al. 2012). Thus, the positive correlation between NRAS and ‘don’t eat me’ signals indicates that NRAS might influence phagocytosis of tumor-associated macrophages. From the above results, we found that the expression level of NRAS might indeed cause a poor prognosis of LUAD patients by remodeling the immune microenvironment of a tumor.
There are still several limitations in our study. First, this study is based on the specimens from one institution and bioinformatic analysis from public RNA-seq databases. By the virtue of its retrospective design, our study has a bias by the virtue of potential heterogeneity. Thus, more prospective large-scale clinical studies are required for us to further study the relationship between NRAS and LUAD. In addition, the clinicopathological information is not intact from public databases. For instance, tumor size, pathological subtype of LUAD and treatment details are not provided from TCGA and GEO databases.
Conclusions
To conclude, we have found NRAS expression as a novel prognostic biomarker in LUAD. Higher expression of NRAS was associated with worse OS at both RNA and protein level. Besides, we have shown that the expression level of NRAS may influence the prognosis of LUAD via a variety of cancer-related pathways and TIM remodeling.
Availability of data and material
Publicly available datasets were analyzed in this study, these can be found in The Cancer Genome Atlas (https://portal.gdc.cancer.gov/), the NCBI Gene Expression Omnibus (GSE30219, GSE42127, and GSE50081), and the Human Protein Atlas (http://www.proteinatlas.org/).
Code availability
Not applicable.
References
Al-Shibli KI, Donnem T, Al-Saad S, Persson M, Bremnes RM, Busund LT (2008) Prognostic effect of epithelial and stromal lymphocyte infiltration in non-small cell lung cancer. Clin Cancer Res 14(16):5220–5227. https://doi.org/10.1158/1078-0432.Ccr-08-0133
Banys-Paluchowski M, Milde-Langosch K, Fehm T, Witzel I, Oliveira-Ferrer L, Schmalfeldt B, Müller V (2020) Clinical relevance of H-RAS, K-RAS, and N-RAS mRNA expression in primary breast cancer patients. Breast Cancer Res Treat 179(2):403–414. https://doi.org/10.1007/s10549-019-05474-8
Barkal AA, Brewer RE, Markovic M, Kowarsky M, Barkal SA, Zaro BW, Weissman IL et al (2019) CD24 signalling through macrophage Siglec-10 is a target for cancer immunotherapy. Nature 572(7769):392–396. https://doi.org/10.1038/s41586-019-1456-0
Bertoli E, Giavarra M, Vitale MG, Minisini AM (2019) Neuroblastoma rat sarcoma mutated melanoma: that’s what we got so far. Pigment Cell Melanoma Res 32(6):744–752. https://doi.org/10.1111/pcmr.12819
Brambilla E, Le Teuff G, Marguet S, Lantuejoul S, Dunant A, Graziano S, Tsao MS et al (2016) Prognostic effect of tumor lymphocytic infiltration in resectable non-small-cell lung cancer. J Clin Oncol 34(11):1223–1230. https://doi.org/10.1200/jco.2015.63.0970
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Chen JJ, Yao PL, Yuan A, Hong TM, Shun CT, Kuo ML, Yang PC et al (2003) Up-regulation of tumor interleukin-8 expression by infiltrating macrophages: its correlation with tumor angiogenesis and patient survival in non-small cell lung cancer. Clin Cancer Res 9(2):729–737
Dietrich P, Gaza A, Wormser L, Fritz V, Hellerbrand C, Bosserhoff AK (2019) Neuroblastoma RAS viral oncogene homolog (NRAS) Is a novel prognostic marker and contributes to sorafenib resistance in hepatocellular carcinoma. Neoplasia 21(3):257–268. https://doi.org/10.1016/j.neo.2018.11.011
Dong H, Zhu G, Tamada K, Chen L (1999) B7–H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nat Med 5(12):1365–1369. https://doi.org/10.1038/70932
Downward J (2003) Targeting RAS signalling pathways in cancer therapy. Nat Rev Cancer 3(1):11–22. https://doi.org/10.1038/nrc969
Fu F, Zhang Y, Gao Z, Zhao Y, Wen Z, Han H, Chen H et al (2021) Combination of CD47 and CD68 expression predicts survival in eastern-Asian patients with non-small cell lung cancer. J Cancer Res Clin Oncol 147(3):739–747. https://doi.org/10.1007/s00432-020-03477-3
Giannou AD, Marazioti A, Kanellakis NI, Giopanou I, Lilis I, Zazara DE, Stathopoulos GT et al (2017) NRAS destines tumor cells to the lungs. EMBO Mol Med 9(5):672–686. https://doi.org/10.15252/emmm.201606978
Ho CC, Liao WY, Wang CY, Lu YH, Huang HY, Chen HY, Yang PC et al (2008) TREM-1 expression in tumor-associated macrophages and clinical outcome in lung cancer. Am J Respir Crit Care Med 177(7):763–770. https://doi.org/10.1164/rccm.200704-641OC
Hu Y, Tao SY, Deng JM, Hou ZK, Liang JQ, Huang QG, Liu H et al (2018) Prognostic value of NRAS gene for survival of colorectal cancer patients: a systematic review and meta-analysis. Asian Pac J Cancer Prev 19(11):3001–3008. https://doi.org/10.31557/apjcp.2018.19.11.3001
Ishida Y, Agata Y, Shibahara K, Honjo T (1992) Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. Embo j 11(11):3887–3895
Kim DW, Min HS, Lee KH, Kim YJ, Oh DY, Jeon YK, Heo DS et al (2008) High tumour islet macrophage infiltration correlates with improved patient survival but not with EGFR mutations, gene copy number or protein expression in resected non-small cell lung cancer. Br J Cancer 98(6):1118–1124. https://doi.org/10.1038/sj.bjc.6604256
Li T, Fu J, Zeng Z, Cohen D, Li J, Chen Q, Liu XS et al (2020) TIMER2.0 for analysis of tumor-infiltrating immune cells. Nucleic Acids Res. https://doi.org/10.1093/nar/gkaa407
Liloglou T, Bediaga NG, Brown BR, Field JK, Davies MP (2014) Epigenetic biomarkers in lung cancer. Cancer Lett 342(2):200–212. https://doi.org/10.1016/j.canlet.2012.04.018
Liu X, Lv X, Yang Q, Jin H, Zhou W, Fan Q (2018) MicroRNA-29a functions as a tumor suppressor and increases cisplatin sensitivity by targeting NRAS in lung cancer. Technol Cancer Res Treat 17:1533033818758905. https://doi.org/10.1177/1533033818758905
Ma Z, Zhang Y, Deng C, Fu F, Deng L, Li Y, Chen H (2020) The prognostic value of Kirsten rat sarcoma viral oncogene homolog mutations in resected lung adenocarcinoma differs according to clinical features. J Thorac Cardiovasc Surg. https://doi.org/10.1016/j.jtcvs.2020.05.097
McIntire JJ, Umetsu SE, Akbari O, Potter M, Kuchroo VK, Barsh GS, DeKruyff RH et al (2001) Identification of Tapr (an airway hyperreactivity regulatory locus) and the linked Tim gene family. Nat Immunol 2(12):1109–1116. https://doi.org/10.1038/ni739
Ohashi K, Sequist LV, Arcila ME, Lovly CM, Chen X, Rudin CM, Pao W et al (2013) Characteristics of lung cancers harboring NRAS mutations. Clin Cancer Res 19(9):2584–2591. https://doi.org/10.1158/1078-0432.Ccr-12-3173
Pelletier MP, Edwardes MD, Michel RP, Halwani F, Morin JE (2001) Prognostic markers in resectable non-small cell lung cancer: a multivariate analysis. Can J Surg 44(3):180–188
Pérez de Castro I, Diaz R, Malumbres M, Hernández MI, Jagirdar J, Jiménez M, Pellicer A et al (2003) Mice deficient for N-ras: impaired antiviral immune response and T-cell function. Cancer Res 63(7):1615–1622
Shimizu K, Goldfarb M, Suard Y, Perucho M, Li Y, Kamata T, Wigler MH et al (1983) Three human transforming genes are related to the viral ras oncogenes. Proc Natl Acad Sci USA 80(8):2112–2116. https://doi.org/10.1073/pnas.80.8.2112
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics, 2017. CA Cancer J Clin 67(1):7–30. https://doi.org/10.3322/caac.21387
Song Z, Liu F, Zhang J (2017) Targeting NRAS(Q61K) mutant delays tumor growth and angiogenesis in non-small cell lung cancer. Am J Cancer Res 7(4):831–844
Subramanian A, Tamayo P, Mootha VK, Mukherjee S, Ebert BL, Gillette MA, Mesirov JP et al (2005) Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci USA 102(43):15545–15550. https://doi.org/10.1073/pnas.0506580102
Subramanian A, Kuehn H, Gould J, Tamayo P, Mesirov JP (2007) GSEA-P: a desktop application for gene set enrichment analysis. Bioinformatics 23(23):3251–3253. https://doi.org/10.1093/bioinformatics/btm369
Suzuki K, Kachala SS, Kadota K, Shen R, Mo Q, Beer DG, Adusumilli PS et al (2011) Prognostic immune markers in non-small cell lung cancer. Clin Cancer Res 17(16):5247–5256. https://doi.org/10.1158/1078-0432.Ccr-10-2805
Thomas NE, Edmiston SN, Alexander A, Groben PA, Parrish E, Kricker A, Conway K et al (2015) Association between NRAS and BRAF mutational status and melanoma-specific survival among patients with higher-risk primary melanoma. JAMA Oncol 1(3):359–368. https://doi.org/10.1001/jamaoncol.2015.0493
Uhlén M, Fagerberg L, Hallström BM, Lindskog C, Oksvold P, Mardinoglu A, Pontén F et al (2015) Proteomics. Tissue-based map of the human proteome. Science 347(6220):1260419. https://doi.org/10.1126/science.1260419
Vogelstein B, Papadopoulos N, Velculescu VE, Zhou S, Diaz LA Jr, Kinzler KW (2013) Cancer genome landscapes. Science 339(6127):1546–1558. https://doi.org/10.1126/science.1235122
Whitwam T, Vanbrocklin MW, Russo ME, Haak PT, Bilgili D, Resau JH, Holmen SL et al (2007) Differential oncogenic potential of activated RAS isoforms in melanocytes. Oncogene 26(31):4563–4570. https://doi.org/10.1038/sj.onc.1210239
Willingham SB, Volkmer JP, Gentles AJ, Sahoo D, Dalerba P, Mitra SS, Weissman IL et al (2012) The CD47-signal regulatory protein alpha (SIRPa) interaction is a therapeutic target for human solid tumors. Proc Natl Acad Sci USA 109(17):6662–6667. https://doi.org/10.1073/pnas.1121623109
Zeni E, Mazzetti L, Miotto D, Lo Cascio N, Maestrelli P, Querzoli P, Boschetto P et al (2007) Macrophage expression of interleukin-10 is a prognostic factor in nonsmall cell lung cancer. Eur Respir J 30(4):627–632. https://doi.org/10.1183/09031936.00129306
Funding
This work was supported by the National Natural Science Foundation of China (Grants 81930073 and 81772466), Shanghai Shenkang Hospital Development Center City Hospital Emerging Cutting-edge Technology Joint Research Project (SHDC12017102) and Shanghai Municipal Health Commission Key Discipline Project (2017ZZ02025 and 2017ZZ01019).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Not applicable.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yan, Y., Gao, Z., Han, H. et al. NRAS expression is associated with prognosis and tumor immune microenvironment in lung adenocarcinoma. J Cancer Res Clin Oncol 148, 565–575 (2022). https://doi.org/10.1007/s00432-021-03842-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-021-03842-w