Abstract
Introduction
Screening for increased levels of prostate-specific antigen (PSA) has allowed early detection of a large majority of prostate cancer (PCa) cases. However, the relative lack of specificity of PSA has resulted in significant over-diagnosis and unnecessary treatment for indolent tumors. The fusion of the transmembrane protease serine 2 with E26 transformation-specific family genes, particularly ERG, is the most widespread genetic alteration in prostate cancer, and data suggest that it is more specific for neoplastic prostate disease and may be of added prognostic value and point toward molecular subtype of PCa.
Methods
In this review, retrospective studies and clinical trials were analyzed to highlight the recent advances in our understanding of the cellular consequence of ERG rearrangement, describe its interactions with other genetic and molecular pathways, and discuss its potential diagnostic and prognostic value.
Conclusion
ERG over-expression has an emerging role in the diagnosis of PCa pathology, although there is still debate about its prognostic value. Elucidation of the mechanisms of ERG gene rearrangements and expression promises novel therapeutic and diagnostic avenues for prostate cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer is the most common cancer diagnosed in North American men, excluding skin cancers (Siegel et al. 2015). It is estimated that in 2015, approximately 220,800 new cases and 27,540 prostate cancer-related deaths will occur in the USA (Siegel et al. 2015). While the increased use of the relatively nonspecific (PSA) testing and subsequent biopsy has led to an increase in incidence rates, mortality figures have seen much less variation (Ross et al. 2008). The overall high death toll of PCa is mostly due to recurrence of previously treated cases and progression to a largely incurable hormone refractory metastatic disease (Denmeade and Isaacs 2002; Feldman and Feldman 2001). It is becoming obvious that more specific diagnostic and therapeutic modalities are a critical unmet need in prostate cancer research.
ERG was discovered in 2005, to be the most frequently over-expressed proto-oncogene in prostate cancers, by quantitative RT-PCR, with 72 % of cases overexpressing ERG (Petrovics et al. 2005). In the same year, Tomlins et al. (2005) reported a recurrent genomic rearrangement in prostate cancer, resulting in the fusion of the 5′ untranslated region of the androgen-responsive transmembrane serine proteinase TMPRSS2 with E26 transformation-specific (ETS) family genes. While fusion to a number of ETS genes, including ETV1, ETV4 and ETV5, has been reported, the most common gene fusion identified is between TMPRSS2 (21q22.3) and ETS-related gene (ERG) (21q22.2), present in about half of all prostate cancers studied (Kumar-Sinha et al. 2008).
ERG background and discovery
The ETS-related gene (ERG) was first described by Reddy et al. (1987), assigned to the ETS oncogene family (Reddy et al. 1987; Rao et al. 1987), and is located on human chromosome 21, band q22 (Rao et al. 1988). The unique feature of the ETS family, including ERG, is the presence of the highly conserved ETS DNA-binding domain that binds to sequences containing a central GGA motif (Hollenhorst et al. 2011). Genes in the ETS family regulate embryonic development, cell cycle control, cell proliferation, differentiation and migration, apoptosis, and angiogenesis (Sharrocks 2001). It has been reported that ERG is required for hematopoiesis, adult hematopoietic stem cell function, as well as the maintenance of normal peripheral blood platelet numbers (Loughran et al. 2008).
ERG gene rearrangements in human have been found in various malignancies. Chromosomal translocation t (16; 21) (p11; q22), resulting in fusion of TLS/FUS to ERG, was identified in acute myeloid leukemia (Shimizu et al. 1993; Kanazawa et al. 2005) and acute lymphoblastic leukemia (Oh et al. 2010). ERG deletion was also described in a subset of acute lymphoblastic leukemia (Mullighan et al. 2007). Five to ten percent of patients with Ewing’s sarcoma showed t (21; 22) translocation resulting in expression of a hybrid EWS/ERG protein (Sorensen et al. 1994). Moreover, ERG rearrangements have now been well documented in prostate cancer. The landmark study by Tomlins et al. (2005) discovered gene fusion of the 5′ untranslated region of TMPRSS2 (which encodes transmembrane protease, serine 2) to the ETS family members ERG or ETV1 in the majority of the prostate cancer cases studied. These findings have now been independently corroborated by a number of researchers, with increased ERG protein expression thought to be reflective of ERG gene rearrangement in prostate cancer (Chaux et al. 2011; Miettinen et al. 2011; van Leenders et al. 2011; Furusato et al. 2010; Lotan et al. 2011; Park et al. 2010). Of note, the prevalence of Prostate cancer shows a great difference between western and Asian patients (Siegel et al. 2013). It was reported that the incidence of PCa in western countries is 20 times higher than in Asian countries (Ferlay et al. 2013). Furthermore, recent studies have shown lower frequency of TMPRSS2-ERG fusion in Asian countries (21 and 28 % in Korea and Japan, respectively) compared to USA (42–60 %) (Wang et al. 2012). This geographical/ethnic variation might pertain to different molecular mechanisms of prostate tumorogenesis in these populations.
TMPRSS2 is constitutively expressed, downstream of androgen, in prostate tissues (Burdova et al. 2014). In cultured prostate cancer cells, androgen-dependent ERG gene overexpression was noted in the VCaP cell line which is androgen sensitive and harbors the TMPRSS2-ERG gene fusion, but not in LNCaP cells which are also androgen sensitive but do not harbor the TMPRSS2-ERG gene fusion (Tomlins et al. 2005). Similarly, in human prostate cancer xenografts, ERG expression was restricted to samples carrying the TMPRSS2-ERG fusion, but not in the androgen-insensitive samples and fusion-negative samples (Hermans et al. 2006). The focus of recent studies have been related to understanding the functional consequence of these reported gene fusions, in addition to uncovering any potential diagnostic or prognostic value.
Biological and molecular features of ERG gene rearrangements
The TMPRSS2 and ERG genes are located about 3Mbp apart on chromosome 21, and the most common gene rearrangement seen involves the deletion of all or part of the intervening sequence (Iljin et al. 2006; Mertz et al. 2007; Perner et al. 2006). Mani et al. (2009) showed an androgen-mediated fusion mechanism in which androgen not only facilitated the chromosomal proximity between TMPRSS2 and ERG gene partners, but also mediated recombinogenic double-strand breaks (DSBs) to form the gene fusion. The ERG gene belongs to the ETS family (29 members in five subfamilies) and has at least nine reported splice variants (Rao et al. 1987; Owczarek et al. 2004; Duterque-Coquillaud et al. 1993). ERG upregulation is seen in about half of all prostate cancers, and the upregulation is thought to occur as a result of fusion transcripts consisting of the 5′ sequences of the androgen-regulated TMPRSS2 and the 3′ sequence of ERG (Mani et al. 2009).
At least twenty different break points have been identified, However, of the most common variants that exist for TMPRSS fusion with ERG, two encode full-length ERG protein, eight encode N-truncated ERG sequences, and one encodes a TMPRSS2-ERG fusion transcript (Hermans et al. 2008). The most common fusion transcripts involve the fusion of TMPRSS2 exon 1 to ERG exon 4 and TMPRSS2 exon 1 fused to ERG exon 5 (Clark et al. 2007; Svensson et al. 2014). Of note, certain TMPRSS2-ERG fusion isoforms have been implicated as mediators of PCa progression (Wang et al. 2006). For instance, fusion between first two exons of TMPRSS2 and exon 4 of ERG tends to be associated with lethal PCa (Wang et al. 2006). There is increasing evidence showing that TMPRSS2 is involved in metastasis and invasion pathways in the prostate via triggering protease-activated receptor-2 (Wilson et al. 2005). In vivo mice studies showed that either overexpressing of ERG or inducing TMPRSS2-ERG fusions did not develop invasive prostate cancer (Klezovitch et al. 2008). Interestingly, microinvasive cancers were found enriched in ERG mice with PTEN-loss heterozygous background (Carver et al. 2009). These findings raise the possibility that ERG cross talk with other oncogenes or tumor suppressors to develop prostate cancer pathology.
Several studies have correlated whole-genome gene expression profiling with clinical data, obtained from ERG-overexpressing PCa samples, to pinpoint relevant signal transduction pathways. For example, Iljin et al. (2006) demonstrated that the WNT pathway was associated with ERG overexpression in PCa cancer. Another study reported the role of the transforming growth factor β (TGF-β) pathway in ERG-overexpressing PCa pathology (Brase et al. 2011). Although the exact regulating mechanism of ERG-associated genes remains unclear, quite a few studies have reported multiple genes regulated by ERG, either directly or indirectly (Iljin et al. 2006; Brase et al. 2011; Bismar et al. 2014). However, despite the magnitude of information published on this subject in the recent few years, an important question about whether ERG and ETV1 function the same way in PCa pathology remains unanswered. Although ERG and ETV1 belong to the same ETS superfamily and both have common binding sites, they exert opposite effects on AR-mediated gene pathway (Baena et al. 2013). Using expression data from localized PCa samples, ERG and ETV1 downstream genes show differential clustering patterns (Boormans et al. 2010). The exact biological and molecular mechanisms of ETV1 overexpression in PCa remain to be investigated.
ERG-related gene signatures and potential targets
TMPRSS2-ERG fusion has been reported present in about 50 % of surgically treated PCa cohorts (radical prostatectomy series); it is less common in high-grade prostatic intraepithelial neoplasia (HGPIN) averaging about 11 % (Mosquera et al. 2008; Park et al. 2014). Additionally, in mice models, overexpression of TMPRSS2-ERG alone is not sufficient to induce prostate neoplasia, which is accelerated in the presence of PTEN genomic deletions (Carver et al. 2009; King et al. 2009). This has led to the question of whether TMPRSS2-ERG is an early event in PCa pathogenesis and whether it can predict pathways related to HGPIN progression to invasive cancer. Previous studies have focused on identifying genetic signatures related to ERG, i.e., potential associated genes/pathways that may explain how ERG functions in promoting PCa progression. Recently, several groups identified a prognostic gene signature that was able to reflect ERG status and was at some points, considered to be more robust than ERG itself, therefore reflecting downstream targets of ERG overexpression as summarized in Table 1 (Bismar et al. 2014; Barfeld et al. 2014; Gasi Tandefelt et al. 2013; Mochmann et al. 2014; Rajan et al. 2014; Setlur et al. 2008).
Other studies focused on identification of potential targets for ERG, which could act to explain disease progression or be of potential therapeutic targets. For example, TMRSS2-ERG gene fusion, combined with disrupted androgen receptor, induced the epigenetic regulators of transcription polycomb-group protein H3K27 methyltransferase EZH2-mediated repression of gene function to regulate PCa progression (Yu et al. 2010). Additionally, altered DNA methylation landscapes of polycomb-repressed loci were documented to be associated with PCa progression and ERG oncogene expression in PCa (Kron et al. 2013).
Genetic ERG knockdown in TMPRSS2-ERG-expressing PCa cells interfered with cell differentiation by repressing genes implicated in epithelial differentiation (PSA and SLC45A3/Prostein) and induced morphological changes; ERG knockdown also inhibited cancer cell growth in vitro and in mouse xenografts (Sun et al. 2008). Another study, using siRNA-treated cells, provided evidence that the activation of C-MYC oncogene was ERG-mediated (Sun et al. 2008). Reports also show that the N-myc downstream-regulated gene 1 (NDRG1) is fused to ERG in PCa (Pflueger et al. 2009).
The loss of homeodomain-containing transcription factor NKX3.1, a known prostate tumor suppressor, leads to epithelial cell overgrowth (Chen et al. 2002). Studies have established that loss of function of NKX3.1 cooperates with the activation of TMPRSS2-ERG fusions in prostate tumorigenesis (Thangapazham et al. 2014). Defects of NKX3.1, such as allelic loss, haploinsufficiency, attenuated expression, or decreased protein stability, represent established pathways in prostate tumorigenesis that may be related to regulation by TMPRSS2-ERG fusion and ERG gene rearrangement (Chen et al. 2002). Another protein that is linked to ERG gene rearrangement and that represents a clinically relevant subgroup of prostate cancer is cysteine-rich secretory protein 3 (CRISP3) (Ribeiro et al. 2011; Grupp et al. 2013a; Al Bashir et al. 2014). It has been documented that CRISP3 expression was markedly increased in PTEN-deleted, ERG-positive tumors and that the combined status of ERG, PTEN, and CRISP3 may be a strong predictor of PCA tumors with the worst outcome (Ribeiro et al. 2011; Al Bashir et al. 2014).
Recently, Gasi Tandefelt and colleagues reported on a 36-gene expression signature that identifies a subset within the TMPRSS2-ERG class of PCa that had a particularly poor clinical outcome (Gasi Tandefelt et al. 2013). These subsets of patients were characterized by tumor growth factor-β, signaling-dependent genes, leading to enhanced PCa progression. The proposed role of TGF-β in aggressive tumors is in line with other studies showing an important role for stromal cells and fibroblast to myofibroblast differentiation in tumor progression (Franco and Hayward 2012; Hagglof et al. 2014; Tidehag et al. 2014).
ERG linkage to phosphoinositol 3-kinase and AKT signaling
An early event in prostate cancers is the alteration of genes leading to inappropriate activation of the phosphoinositol-3 kinase/protein kinase-B (PI3K/AKT) signaling pathway (Li et al. 1997). This occurs most often through loss of function mutations or deletions of phosphate and tensin homologs on chromosome ten (PTEN), a lipid phosphatase that acts as a negative regulator of the PI3k/AKT signaling pathway (Li et al. 1997). Since PTEN loss is reported in a much larger percentage of HGPIN patients (Bettendorf et al. 2008), Carver and colleagues investigated the cooperative action of PTEN and ERG rearrangements (Carver et al. 2009). In a series of experiments combining human prostate cancer genetic assessment with transgenic mice, they showed that when PTEN loss occurs concomitantly with ERG aberrant expression, the role of ERG on cell migration and invasion rapidly promotes progression of HGPIN to invasive cancer (Carver et al. 2009). Loss of function mutations or rearrangements in the PTEN-associated protein, membrane-associated guanylate kinase inverted (MAGI), is also reported in prostate cancer (Mahdian et al. 2014). MAGI acts as a scaffold protein and augments the ability of PTEN to suppress AKT1 activation, and the loss of this protein would replicate the phenotype seen with PTEN loss. Although ERG has been shown to associate with PTEN genomic deletions, its clinical prognostic value has not been straightforward. An adverse outcome has been reported in tumors with combined PTEN loss and TMPRSS2-ERG rearrangement (Yoshimoto et al. 2008). Other studies suggested slightly better prognosis and documented that only PTEN deletions/decrease expression is of added adverse clinical outcome (Leinonen et al. 2013; Nagle et al. 2013). No matter the potential clinical implication, it is well established that ERG, PTEN, and AR are closely related and may reflect on molecular subtypes of PCa (Bismar et al. 2011; Bismar et al. 2012a).
ERG-related pathways and cellular responses
A clear picture of ERG-regulated genes in prostate cancer has not yet fully been elucidated. ERG overexpression in PCa cells in vitro conveys invasiveness and induces plasminogen activation, as well as matrix metalloproteinase pathways (Tian et al. 2014). Studies have noted that ERG modulates prostaglandin signaling in prostate cancer cells (Mohamed et al. 2011). A role for prostanoid signaling in enabling invasiveness of PCa has been shown, with the regulation of MMP2 and MMP9 proposed as the mechanistic basis for prostanoid regulation of tumor invasiveness (Attiga et al. 2000). These data are in line with the long established observation of prostanoid and eicosanoid signaling being involved in the development of various carcinomas, including those of the prostate (Badawi 2000). In vitro overexpression of ERG is also reported to promote cell migration, a property necessary for tumorigenesis, without affecting proliferation and another member of the MMP family (Carver et al. 2009). A disintegrin and metalloproteinase with thrombospondin motifs 1 (ADAMTS1) (along with CXCR4) was found to be among genes strongly upregulated in the presence of ERG overexpression (Carver et al. 2009). Thus, regulation of the matrix metalloproteinase action in the tumor microenvironment is a likely consequence of ERG gene rearrangement.
Another protease pathway that is important in prostate cancer, but expressed markedly in ERG-negative cancers, is related to the serine peptidase inhibitor, Kazal type 1 (SPINK1). SPINK1 encodes a 6-kDa trypsin inhibitor that is overexpressed in about 10–15 % of ERG-negative prostate cancers (Helgeson et al. 2008) and represents a subgroup of tumors positive for Trefoil3 (TFF3) (Terry et al. 2015). SPINK1 expression is also tightly linked to 6q15- and 5q21-deleted ERG fusion-negative prostate cancers, but was unrelated to PSA recurrence (Grupp et al. 2013b). SPINK1 overexpression was associated with an aggressive subset of prostate cancer cell lines, and the genetic knockdown of SPINK1 attenuated the invasive phenotype and was further shown to mediate its oncogenic effects in part through epidermal growth factor receptor (EGFR) (Helgeson et al. 2008). Therefore, it was hypothesized that therapeutic targeting of either SPINK1 or EGFR with monoclonal antibodies could suppress proliferation and invasion of prostate cancer cells (Ateeq et al. 2011). While previous clinical trials of anti-EGFR monoclonal antibody (cetuximab) in metastatic CRPC were disappointing, subsets of patients did show benefits and were likely a SPINK1-overexpressing patients (Slovin et al. 2009). There is now convincing evidence that SPINK1 may be associated with increased risk of biochemical recurrence, and its inhibition is a promising therapeutic strategy (Terry et al. 2015; Leinonen et al. 2010).
Acetylation and deacetylation of core histones (H2A, H2B, H3 and H4) play a key role in epigenetic repression and are important for transcriptional regulation cell cycle progression and development (Ng and Bird 2000). Histone deacetylase 1 is a protein responsible for deacetylation of lysine residues on the core histones and serves an important role in the regulation of eukaryotic gene expression. Importantly, overexpression of HDAC1 is reported to induce angiogenesis by negatively regulating p53 and von Hippel-Lindau tumor suppressor genes (Kim et al. 2001; Ropero and Esteller 2007). Since HDAC1 is reported to be overexpressed in cancers with ERG rearrangement (Iljin et al. 2006), such regulation of tumor suppressor genes could represent another mechanism by which ERG rearrangements promote prostate cancer. One point in regard to ERG association with other molecular markers, mainly SPINK1, PTEN and CRISP3, is that a combination of two or more markers is likely to affect disease prognosis and may signify subclass of PCa depending on the site where they occur (Fig. 1). Lastly, a study has demonstrated that miR-221 downregulated in TMPRSS2-ERG-positive PCa cells, hence providing an evidence of the cross talk between ERG gene fusion and miRNA expression (Gordanpour et al. 2011). Still, the molecular mechanisms underlying the expression of ERG-regulated genes remain to be investigated.
Molecular classes and association of gene alterations in prostate cancer. Approximately 50 % of all prostate cancers show ERG gene fusion or other ETS gene rearrangement. In patients with positive ERG rearrangement, a concomitant deletion of PTEN and overexpression of CRISP3 lead to poor prognosis. In PCa with no ERG rearrangement, approximately 6 % show overexpression of SPINK1 that promotes metastatic disease. All of the SPINK1-overexpressing cells also showed PTEN deletion. SPINK1 overexpression has been reported in association within the same focus of PTEN homozygous deletions in nonlocalized PCa but not in localized disease
The diagnostic and prognostic value of TMPRSS2-ERG gene fusion
The diagnostic and prognostic value of ERG expression remains to be fully established. Several studies have examined the prognostic value of TMPRSS2-ERG fusion status in PCa. As summarized in Table 2, thirteen studies have shown a significant association between ERG fusion marker and PCa outcome. It is worth noting that although TMPRSS2-ERG has been frequently associated with poorer prognosis and more aggressive tumors, other studies have failed to show such prognostic value (Falzarano et al. 2010; Toubaji et al. 2011; Minner et al. 2011; Hoogland et al. 2012).
Mehra and colleagues identified TMPRSS2-ERG rearrangement to be associated with a high pathological grade in a cohort of 96 surgically treated patients (Mehra et al. 2007). However, Darnel et al. (2009) reported that TMPRSS2-ERG is more frequent in less aggressive tumors with Gleason grade 3. TMPRSS2-ERG gene fusion, ERG expression or composite intensity score was also identified as a prognostic factor of increased rates of biochemical recurrence and cancer-specific mortality in patients that had undergone surgical treatment for primary cancers (Nam et al. 2007a, b; Spencer et al. 2013). In another study, TMPRSS2-ERG gene rearrangement was associated with poor survival of prostate cancer patients with a combination of 5′ ERG deletion and TMPRSS2-ERG (25 % survival at 8 years), compared to patients negative for this rearrangement (90 % survival at 8 years) (Attard et al. 2008). Although, in another study assessing the gene fusion status in a cohort of patients managed expectantly, only 15 % of patients were found to have TMPRSS2-ERG rearrangement, this group of patients showed higher incidence of prostate cancer-specific death (Demichelis et al. 2007). This observation of less frequent ERG gene rearrangements in patients not managed surgically was validated in subsequent cohorts of patients with unsuspected, advanced, and castrate-resistant prostate cancer (CRPC) (Falzarano et al. 2010; Liu et al. 2011). Using ERG protein expression as a surrogate for ERG gene rearrangements in a cohort of men treated with hormonal therapy, we reported that high ERG intensity was associated with lower Gleason score, better response to hormonal therapy, better overall and cancer-specific survival, and longer free progression times to castration-resistant disease (Bismar et al. 2012b). In a revealing recent study, 1590 men with biopsy-diagnosed HGPIN, a precursor lesion of prostate cancer, showed that patients with ERG expression were more likely to develop prostate cancer (Park et al. 2014). While only 11.1 % of the HGPIN patients had ERG rearrangement, over a 3-year follow-up, 53 % of ERG rearrangement-positive patients and 35 % of ERG-negative patients progressed to prostate cancer, highlighting that HGPIN patient with ERG overexpression might need more rigorous clinical monitoring (Park et al. 2014).
However, as noted above, the data on the clinical significance of ERG are not all in agreement. Studies have demonstrated some contrasting results. Teng et al. (2013) showed that although there is significant association between ERG protein levels, extra-prostatic extension, and higher pathological stage, ERG progression is not associated with an adverse clinical outcome and is of limited prognostic value in localized prostate cancer. This was recently confirmed, using gene expression data to predict ERG status, where ERG was noted more often with lower grade Gleason scores and in association with extra-prostatic extension, but with no significant association to biochemical relapse (BCR) (Tomlins et al. 2015a).
Minner et al. (2011) showed no clinical difference between ERG-positive and ERG-negative PCa in the absence of antihormonal therapy. Hoogland et al. (2012) demonstrated that ERG expression by immunohistochemistry had no predictive value for prostate cancer recurrence or progression after radical prostatectomy and that increased ERG levels were associated with the upregulation of androgen receptor expression in clinical specimens. Furthermore, TMPRSS2-ERG fusion was found to be not prognostic for recurrence after radical prostatectomy for clinically localized prostate cancer, although men with ERG gene copy number gain without fusion were twice more likely to recur (Toubaji et al. 2011). When characterizing ERG in early onset PCa, ERG expression was noted to be present at higher rates of close to 60–65 % in two studies (Huang et al. 2014; Steurer et al. 2014). Furthermore, ERG was found to be associated with increased rates of biochemical recurrence postradical prostatectomy in one of those studies (Huang et al. 2014). In light of the contradictory results above, it seems that the significance of ERG expression in PCa is likely dependent on the heterogeneity of studied cohorts, the methods used to detect ERG, and the clinical outcome endpoint being investigated. For example, ERG expression shows a prognostic significance in localized prostate cancer in men below the age of 50 (Huang et al. 2014). Another study shows that ERG may also play a prognostic role in men treated expectantly by hormonal therapy or active surveillance (AS) as it reflects higher stage and higher tumor volume (Teng et al. 2013).
In a cohort of AS, positive ERG at diagnosis was suggested to be used to estimate the risk of progression during AS (Berg et al. 2014). ERG prognostic and diagnostic value in urine samples has been investigated and documented in several studies to provide added value to serum PSA in detecting PCa and high-grade PCa in biopsies (Tomlins et al. 2015b). In summary, it is clearly established that ERG fusion marker is considered a key genomic marker and should be taken into consideration when the prognostic values of other genomic events are investigated.
Clinical utility of TMPRSS2-ERG gene fusion and ERG expression
Although PSA is still widely used to monitor PCa progression, it is too far from ideal to be considered as an early carcinogenic biomarker (Tomlins et al. 2005). It is noteworthy that PSA can early detect merely 23–44 % of PCa pathology (Draisma et al. 2009). Thus, it is mandatory, for the sake of better diagnostic sensitivity, to discover more efficient biomarkers. Consistent with this notion, Leyten et al. (2014) showed that TMPRSS2-ERG fusion, as a urinary biomarker, improves PCa detection and considerably reduces the frequency of unnecessary prostate biopsies. Furthermore, detection of ERG alterations is beneficial to determine the cancer origin and hence differentiate between aggressive PCa variants such as prostate small cell carcinoma from other small cell carcinomas with different origins (e.g., bladder or lung) (Guo et al. 2011). Recent works have introduced invaluable insights on using ERG as a therapeutic target. It has been demonstrated that either genetically knocking down TMPRSS2-ERG fusion or inhibiting its upstream signaling inhibits PCa growth (Wang et al. 2008; Dasgupta et al. 2012). A number of clinical trials are taking the advantage of the ability of TMPRSS2-ERG fusion product to exert tumorigenic activity, via its interaction with PARP1 [Poly (ADPRibose) Polymerase 1], to assess whether modulating this axis would benefit PCa patients (Brenner et al. 2011). Currently, ERG overexpression is considered a valuable tool in the diagnosis of PCa pathology.
Association and significance of ERG in radiation-treated patients
Data are mixed on the issue of ERG and radiosensitivity. An earlier study documented that TMPRSS2-ERG fusion-positive tumors were not more radiosensitive than the fusion-negative tumors and ERG rearrangement is therefore unlikely to be a predictive factor of image-guided radiotherapy response (Dal Pra et al. 2013). However, another study documented that patients with both ERG and PTEN genetic aberrations are at significant adverse BCR following brachytherapy (Fontugne et al. 2014). A previous study has shown the potential of ERG and PTEN to assess the prognostic value in Brachytherapy patients, but these data require further validation (Fontugne et al. 2014). NKX3.1 haploinsufficiency is prognostic for prostate cancer relapse following surgery or image-guided radiotherapy (Locke et al. 2012). A recent study has shown that loss of NKX3.1 promotes TMPRSS2-ERG fusion gene expression (Thangapazham et al. 2014), suggesting that the two molecular events may therefore be related. The full prognostic value in patients treated by radiotherapy still needs full exploration.
ERG and its potential diagnostic value in prostate pathology
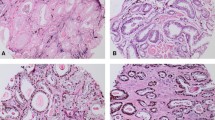
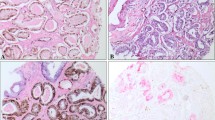
ERG has been investigated in several studies as a diagnostic tool for prostate biopsies in conjunction with basal cell markers and AMACR (Shah et al. 2013; Yaskiv et al. 2011; Lee et al. 2014; Shah 2013). Specifically, it was assessed in atypical glands and suspicious foci (Shah et al. 2013). Overall, ERG is not a useful marker by itself to replace basal cell markers or AMACR, as it is expressed in only half of PCa as compared to AMACR, which is overexpressed in about 90 % of PCa (Yaskiv et al. 2011). ERG is thought to be more specific, but less sensitive as a diagnostic maker for PCa (Lee et al. 2015). The conclusion of these studies is that ERG, in combination with AMACR and basal cell makers, may offer added value in prostate biopsies, but the potential improvement in such a diagnostic test could be limited.
Conclusion
There is tantalizing evidence that ERG overexpression and ERG gene rearrangement is a useful predictive marker of metastatic potential or recurrence of prostate cancer. There is now a fairly good genetic and biological understanding of changes in prostate cancer. A number of clinical efforts to translate this knowledge to better diagnostic modalities and therapeutic strategies are underway. A key target is the rearrangement of the ERG gene and its interaction with other tumor-regulating pathways (Fig. 2). Further work to fully understand the functional consequence of these rearrangements and regulated cell signaling pathways promises exciting new advances in the diagnosis and management of prostate cancer.
Overview of mechanisms underlying ERG regulation in PCA. The most common ERG gene rearrangements involve fusion of exon 1 of TMPRSS2 with exon 4 or 5 of ERG. This leads to ERG becoming an androgen-responsive gene. Cellular function changes reported following such rearrangement include upregulation of MMPs, increased AKT signaling responses, EZH2 suppression of genes, and PGE2 upregulation-dependent PCa progression
References
Al Bashir S, Alshalalfa M, Hegazy SA, Dolph M, Donnelly B, Bismar TA (2014) Cysteine-rich secretory protein 3 (CRISP3), ERG and PTEN define a molecular subtype of prostate cancer with implication to patients’ prognosis. J Hematol Oncol 7:21. doi:10.1186/1756-8722-7-21
Ateeq B, Tomlins SA, Laxman B, Asangani IA, Cao Q, Cao X et al (2011) Therapeutic targeting of SPINK1-positive prostate cancer. Sci Transl Med 3(72):72ra17. doi:10.1126/scitranslmed.3001498
Attard G, Clark J, Ambroisine L, Fisher G, Kovacs G, Flohr P et al (2008) Duplication of the fusion of TMPRSS2 to ERG sequences identifies fatal human prostate cancer. Oncogene 27(3):253–263. doi:10.1038/sj.onc.1210640
Attiga FA, Fernandez PM, Weeraratna AT, Manyak MJ, Patierno SR (2000) Inhibitors of prostaglandin synthesis inhibit human prostate tumor cell invasiveness and reduce the release of matrix metalloproteinases. Cancer Res 60(16):4629–4637
Badawi AF (2000) The role of prostaglandin synthesis in prostate cancer. BJU Int 85(4):451–462
Baena E, Shao Z, Linn DE, Glass K, Hamblen MJ, Fujiwara Y et al (2013) ETV1 directs androgen metabolism and confers aggressive prostate cancer in targeted mice and patients. Genes Dev 27(6):683–698. doi:10.1101/gad.211011.112
Barfeld SJ, East P, Zuber V, Mills IG (2014) Meta-analysis of prostate cancer gene expression data identifies a novel discriminatory signature enriched for glycosylating enzymes. BMC Med Genomics 7(1):513. doi:10.1186/s12920-014-0074-9
Berg KD, Vainer B, Thomsen FB, Roder MA, Gerds TA, Toft BG et al (2014) ERG protein expression in diagnostic specimens is associated with increased risk of progression during active surveillance for prostate cancer. Eur Urol 66(5):851–860. doi:10.1016/j.eururo.2014.02.058
Bettendorf O, Schmidt H, Staebler A, Grobholz R, Heinecke A, Boecker W et al (2008) Chromosomal imbalances, loss of heterozygosity, and immunohistochemical expression of TP53, RB1, and PTEN in intraductal cancer, intraepithelial neoplasia, and invasive adenocarcinoma of the prostate. Genes Chromosomes Cancer 47(7):565–572
Bismar TA, Yoshimoto M, Vollmer RT, Duan Q, Firszt M, Corcos J et al (2011) PTEN genomic deletion is an early event associated with ERG gene rearrangements in prostate cancer. BJU Int 107(3):477–485. doi:10.1111/j.1464-410X.2010.09470.x
Bismar TA, Yoshimoto M, Duan Q, Liu S, Sircar K, Squire JA (2012a) Interactions and relationships of PTEN, ERG, SPINK1 and AR in castration-resistant prostate cancer. Histopathology 60(4):645–652. doi:10.1111/j.1365-2559.2011.04116.x
Bismar TA, Dolph M, Teng LH, Liu S, Donnelly B (2012b) ERG protein expression reflects hormonal treatment response and is associated with Gleason score and prostate cancer specific mortality. Eur J Cancer 48(4):538–546. doi:10.1016/j.ejca.2012.01.001
Bismar TA, Alshalalfa M, Petersen LF, Teng LH, Gerke T, Bakkar A et al (2014) Interrogation of ERG gene rearrangements in prostate cancer identifies a prognostic 10-gene signature with relevant implication to patients’ clinical outcome. BJU Int 113(2):309–319. doi:10.1111/bju.12262
Boormans JL, Hermans KG, Made AC, van Leenders GJ, Wildhagen MF, Collette L et al (2010) Expression of the androgen-regulated fusion gene TMPRSS2-ERG does not predict response to endocrine treatment in hormone-naive, node-positive prostate cancer. Eur Urol 57(5):830–835. doi:10.1016/j.eururo.2009.08.013
Brase JC, Johannes M, Mannsperger H, Falth M, Metzger J, Kacprzyk LA et al (2011) TMPRSS2-ERG-specific transcriptional modulation is associated with prostate cancer biomarkers and TGF-beta signaling. BMC Cancer 11:507. doi:10.1186/1471-2407-11-507
Brenner JC, Ateeq B, Li Y, Yocum AK, Cao Q, Asangani IA et al (2011) Mechanistic rationale for inhibition of poly(ADP-ribose) polymerase in ETS gene fusion-positive prostate cancer. Cancer Cell 19(5):664–678. doi:10.1016/j.ccr.2011.04.010
Burdova A, Bouchal J, Tavandzis S, Kolar Z (2014) TMPRSS2-ERG gene fusion in prostate cancer. Biomed Pap 158(4):502–510. doi:10.5507/bp.2014.065
Carver BS, Tran J, Gopalan A, Chen Z, Shaikh S, Carracedo A et al (2009) Aberrant ERG expression cooperates with loss of PTEN to promote cancer progression in the prostate. Nat Genet 41(5):619–624. doi:10.1038/ng.370
Chaux A, Albadine R, Toubaji A, Hicks J, Meeker A, Platz EA et al (2011) Immunohistochemistry for ERG expression as a surrogate for TMPRSS2-ERG fusion detection in prostatic adenocarcinomas. Am J Surg Pathol 35(7):1014–1020. doi:10.1097/PAS.0b013e31821e8761
Chen H, Nandi AK, Li X, Bieberich CJ (2002) NKX-3.1 interacts with prostate-derived Ets factor and regulates the activity of the PSA promoter. Cancer Res 62(2):338–340
Clark J, Merson S, Jhavar S, Flohr P, Edwards S, Foster CS et al (2007) Diversity of TMPRSS2-ERG fusion transcripts in the human prostate. Oncogene 26(18):2667–2673. doi:10.1038/sj.onc.1210070
Dal Pra A, Lalonde E, Sykes J, Warde F, Ishkanian A, Meng A et al (2013) TMPRSS2-ERG status is not prognostic following prostate cancer radiotherapy: implications for fusion status and DSB repair. Clin Cancer Res 19(18):5202–5209. doi:10.1158/1078-0432.CCR-13-1049
Darnel AD, Lafargue CJ, Vollmer RT, Corcos J, Bismar TA (2009) TMPRSS2-ERG fusion is frequently observed in Gleason pattern 3 prostate cancer in a Canadian cohort. Cancer Biol Ther 8(2):125–130
Dasgupta S, Srinidhi S, Vishwanatha JK (2012) Oncogenic activation in prostate cancer progression and metastasis: molecular insights and future challenges. J Carcinog 11:4. doi:10.4103/1477-3163.93001
Demichelis F, Fall K, Perner S, Andren O, Schmidt F, Setlur SR et al (2007) TMPRSS2: ERG gene fusion associated with lethal prostate cancer in a watchful waiting cohort. Oncogene 26(31):4596–4599. doi:10.1038/sj.onc.1210237
Denmeade SR, Isaacs JT (2002) A history of prostate cancer treatment. Nat Rev Cancer 2(5):389–396. doi:10.1038/nrc801
Draisma G, Etzioni R, Tsodikov A, Mariotto A, Wever E, Gulati R et al (2009) Lead time and overdiagnosis in prostate-specific antigen screening: importance of methods and context. J Natl Cancer Inst 101(6):374–383. doi:10.1093/jnci/djp001
Duterque-Coquillaud M, Niel C, Plaza S, Stehelin D (1993) New human erg isoforms generated by alternative splicing are transcriptional activators. Oncogene 8(7):1865–1873
Falzarano SM, Navas M, Simmerman K, Klein EA, Rubin MA, Zhou M et al (2010) ERG rearrangement is present in a subset of transition zone prostatic tumors. Mod Pathol 23(11):1499–1506. doi:10.1038/modpathol.2010.150
Feldman BJ, Feldman D (2001) The development of androgen-independent prostate cancer. Nat Rev Cancer 1(1):34–45. doi:10.1038/35094009
Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H et al (2013) Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 49(6):1374–1403. doi:10.1016/j.ejca.2012.12.027
Fontugne J, Lee D, Cantaloni C, Barbieri CE, Caffo O, Hanspeter E et al (2014) Recurrent prostate cancer genomic alterations predict response to brachytherapy treatment. Cancer Epidemiol Biomarkers Prev 23(4):594–600. doi:10.1158/1055-9965.EPI-13-1180
Franco OE, Hayward SW (2012) Targeting the tumor stroma as a novel therapeutic approach for prostate cancer. Adv Pharmacol 65:267–313. doi:10.1016/B978-0-12-397927-8.00009-9
Furusato B, Tan SH, Young D, Dobi A, Sun C, Mohamed AA et al (2010) ERG oncoprotein expression in prostate cancer: clonal progression of ERG-positive tumor cells and potential for ERG-based stratification. Prostate Cancer Prostatic Dis 13(3):228–237. doi:10.1038/pcan.2010.23
Gasi Tandefelt D, Boormans JL, van der Korput HA, Jenster GW, Trapman J (2013) A 36-gene signature predicts clinical progression in a subgroup of ERG-positive prostate cancers. Eur Urol 64(6):941–950. doi:10.1016/j.eururo.2013.02.039
Gordanpour A, Stanimirovic A, Nam RK, Moreno CS, Sherman C, Sugar L et al (2011) miR-221 is down-regulated in TMPRSS2: ERG fusion-positive prostate cancer. Anticancer Res 31(2):403–410
Grupp K, Kohl S, Sirma H, Simon R, Steurer S, Becker A et al (2013a) Cysteine-rich secretory protein 3 overexpression is linked to a subset of PTEN-deleted ERG fusion-positive prostate cancers with early biochemical recurrence. Mod Pathol 26(5):733–742. doi:10.1038/modpathol.2012.206
Grupp K, Diebel F, Sirma H, Simon R, Breitmeyer K, Steurer S et al (2013b) SPINK1 expression is tightly linked to 6q15- and 5q21-deleted ERG-fusion negative prostate cancers but unrelated to PSA recurrence. Prostate 73(15):1690–1698. doi:10.1002/pros.22707
Guo CC, Dancer JY, Wang Y, Aparicio A, Navone NM, Troncoso P et al (2011) TMPRSS2-ERG gene fusion in small cell carcinoma of the prostate. Hum Pathol 42(1):11–17. doi:10.1016/j.humpath.2010.05.026
Hagglof C, Hammarsten P, Stromvall K, Egevad L, Josefsson A, Stattin P et al (2014) TMPRSS2-ERG expression predicts prostate cancer survival and associates with stromal biomarkers. PLoS One 9(2):e86824. doi:10.1371/journal.pone.0086824
Helgeson BE, Tomlins SA, Shah N, Laxman B, Cao Q, Prensner JR et al (2008) Characterization of TMPRSS2:ETV5 and SLC45A3: ETV5 gene fusions in prostate cancer. Cancer Res 68(1):73–80
Hermans KG, van Marion R, van Dekken H, Jenster G, van Weerden WM, Trapman J (2006) TMPRSS2: ERG fusion by translocation or interstitial deletion is highly relevant in androgen-dependent prostate cancer, but is bypassed in late-stage androgen receptor-negative prostate cancer. Cancer Res 66(22):10658–10663. doi:10.1158/0008-5472.CAN-06-1871
Hermans KG, van der Korput HA, van Marion R, van de Wijngaart DJ, Ziel-van der Made A, Dits NF et al (2008) Truncated ETV1, fused to novel tissue-specific genes, and full-length ETV1 in prostate cancer. Cancer Res 68(18):7541–7549. doi:10.1158/0008-5472.CAN-07-5930
Hollenhorst PC, McIntosh LP, Graves BJ (2011) Genomic and biochemical insights into the specificity of ETS transcription factors. Annu Rev Biochem 80:437–471. doi:10.1146/annurev.biochem.79.081507.103945
Hoogland AM, Jenster G, van Weerden WM, Trapman J, van der Kwast T, Roobol MJ et al (2012) ERG immunohistochemistry is not predictive for PSA recurrence, local recurrence or overall survival after radical prostatectomy for prostate cancer. Mod Pathol 25(3):471–479. doi:10.1038/modpathol.2011.176
Huang KC, Dolph M, Donnelly B, Bismar TA (2014) ERG expression is associated with increased risk of biochemical relapse following radical prostatectomy in early onset prostate cancer. Clin Transl Oncol 16(11):973–979. doi:10.1007/s12094-014-1182-x
Iljin K, Wolf M, Edgren H, Gupta S, Kilpinen S, Skotheim RI et al (2006) TMPRSS2 fusions with oncogenic ETS factors in prostate cancer involve unbalanced genomic rearrangements and are associated with HDAC1 and epigenetic reprogramming. Cancer Res 66(21):10242–10246
Kanazawa T, Ogawa C, Taketani T, Taki T, Hayashi Y, Morikawa A (2005) TLS/FUS-ERG fusion gene in acute lymphoblastic leukemia with t(16;21)(p11;q22) and monitoring of minimal residual disease. Leuk Lymphoma 46(12):1833–1835. doi:10.1080/10428190500162203
Kim MS, Kwon HJ, Lee YM, Baek JH, Jang JE, Lee SW et al (2001) Histone deacetylases induce angiogenesis by negative regulation of tumor suppressor genes. Nat Med 7(4):437–443. doi:10.1038/86507
King JC, Xu J, Wongvipat J, Hieronymus H, Carver BS, Leung DH et al (2009) Cooperativity of TMPRSS2-ERG with PI3-kinase pathway activation in prostate oncogenesis. Nat Genet 41(5):524–526
Klezovitch O, Risk M, Coleman I, Lucas JM, Null M, True LD et al (2008) A causal role for ERG in neoplastic transformation of prostate epithelium. Proc Natl Acad Sci USA 105(6):2105–2110. doi:10.1073/pnas.0711711105
Kron K, Trudel D, Pethe V, Briollais L, Fleshner N, van der Kwast T et al (2013) Altered DNA methylation landscapes of polycomb-repressed loci are associated with prostate cancer progression and ERG oncogene expression in prostate cancer. Clin Cancer Res 19(13):3450–3461. doi:10.1158/1078-0432.CCR-12-3139
Kumar-Sinha C, Tomlins SA, Chinnaiyan AM (2008) Recurrent gene fusions in prostate cancer. Nat Rev Cancer 8(7):497–511. doi:10.1038/nrc2402
Lee SL, Yu D, Wang C, Saba R, Liu S, Trpkov K et al (2014) ERG expression in prostate needle biopsy: potential diagnostic and prognostic implications. Appl Immunohistochem Mol Morphol. doi:10.1097/PAI.0000000000000119
Lee SL, Yu D, Wang C, Saba R, Liu S, Trpkov K et al (2015) ERG expression in prostate needle biopsy: potential diagnostic and prognostic implications. Appl Immunohistochem Mol Morphol 23(7):499–505. doi:10.1097/PAI.0000000000000119
Leinonen KA, Tolonen TT, Bracken H, Stenman UH, Tammela TL, Saramaki OR et al (2010) Association of SPINK1 expression and TMPRSS2: ERG fusion with prognosis in endocrine-treated prostate cancer. Clin Cancer Res 16(10):2845–2851. doi:10.1158/1078-0432.CCR-09-2505
Leinonen KA, Saramäki OR, Furusato B, Kimura T, Takahashi H, Egawa S et al (2013) Loss of PTEN is associated with aggressive behavior in ERG-positive prostate cancer. Cancer Epidemiol Biomarkers Prev 22(12):2333–2344. doi:10.1158/1055-9965.epi-13-0333-t
Leyten GH, Hessels D, Jannink SA, Smit FP, de Jong H, Cornel EB et al (2014) Prospective multicentre evaluation of PCA3 and TMPRSS2-ERG gene fusions as diagnostic and prognostic urinary biomarkers for prostate cancer. Eur Urol 65(3):534–542. doi:10.1016/j.eururo.2012.11.014
Li J, Yen C, Liaw D, Podsypanina K, Bose S, Wang SI et al (1997) PTEN, a putative protein tyrosine phosphatase gene mutated in human brain, breast, and prostate cancer. Science 275(5308):1943–1947
Liu S, Yoshimoto M, Trpkov K, Duan Q, Firszt M, Corcos J et al (2011) Detection of ERG gene rearrangements and PTEN deletions in unsuspected prostate cancer of the transition zone. Cancer Biol Ther 11(6):562–566
Locke JA, Zafarana G, Ishkanian AS, Milosevic M, Thoms J, Have CL et al (2012) NKX3.1 haploinsufficiency is prognostic for prostate cancer relapse following surgery or image-guided radiotherapy. Clin Cancer Res 18(1):308–316. doi:10.1158/1078-0432.CCR-11-2147
Lotan TL, Gupta NS, Wang W, Toubaji A, Haffner MC, Chaux A et al (2011) ERG gene rearrangements are common in prostatic small cell carcinomas. Mod Pathol 24(6):820–828. doi:10.1038/modpathol.2011.7
Loughran SJ, Kruse EA, Hacking DF, de Graaf CA, Hyland CD, Willson TA et al (2008) The transcription factor Erg is essential for definitive hematopoiesis and the function of adult hematopoietic stem cells. Nat Immunol 9(7):810–819. doi:10.1038/ni.1617
Mahdian R, Nodouzi V, Asgari M, Rezaie M, Alizadeh J, Yousefi B et al (2014) Expression profile of MAGI2 gene as a novel biomarker in combination with major deregulated genes in prostate cancer. Mol Biol Rep 41(9):6125–6131. doi:10.1007/s11033-014-3491-0
Mani RS, Tomlins SA, Callahan K, Ghosh A, Nyati MK, Varambally S et al (2009) Induced chromosomal proximity and gene fusions in prostate cancer. Science 326(5957):1230. doi:10.1126/science.1178124
Mehra R, Tomlins SA, Shen R, Nadeem O, Wang L, Wei JT et al (2007) Comprehensive assessment of TMPRSS2 and ETS family gene aberrations in clinically localized prostate cancer. Mod Pathol 20(5):538–544. doi:10.1038/modpathol.3800769
Mertz KD, Setlur SR, Dhanasekaran SM, Demichelis F, Perner S, Tomlins S et al (2007) Molecular characterization of TMPRSS2-ERG gene fusion in the NCI-H660 prostate cancer cell line: a new perspective for an old model. Neoplasia 9(3):200–206
Miettinen M, Wang ZF, Paetau A, Tan SH, Dobi A, Srivastava S et al (2011) ERG transcription factor as an immunohistochemical marker for vascular endothelial tumors and prostatic carcinoma. Am J Surg Pathol 35(3):432–441. doi:10.1097/PAS.0b013e318206b67b
Minner S, Enodien M, Sirma H, Luebke AM, Krohn A, Mayer PS et al (2011) ERG status is unrelated to PSA recurrence in radically operated prostate cancer in the absence of antihormonal therapy. Clin Cancer Res 17(18):5878–5888. doi:10.1158/1078-0432.CCR-11-1251
Mochmann LH, Neumann M, von der Heide EK, Nowak V, Kuhl AA, Ortiz-Tanchez J et al (2014) ERG induces a mesenchymal-like state associated with chemoresistance in leukemia cells. Oncotarget 5(2):351–362
Mohamed AA, Tan SH, Sun C, Shaheduzzaman S, Hu Y, Petrovics G et al (2011) ERG oncogene modulates prostaglandin signaling in prostate cancer cells. Cancer Biol Ther 11(4):410–417
Mosquera JM, Perner S, Genega EM, Sanda M, Hofer MD, Mertz KD et al (2008) Characterization of TMPRSS2-ERG fusion high-grade prostatic intraepithelial neoplasia and potential clinical implications. Clin Cancer Res 14(11):3380–3385. doi:10.1158/1078-0432.CCR-07-5194
Mullighan CG, Goorha S, Radtke I, Miller CB, Coustan-Smith E, Dalton JD et al (2007) Genome-wide analysis of genetic alterations in acute lymphoblastic leukaemia. Nature 446(7137):758–764. doi:10.1038/nature05690
Nagle RB, Algotar AM, Cortez CC, Smith K, Jones C, Sathyanarayana UG et al (2013) ERG overexpression and PTEN status predict capsular penetration in prostate carcinoma. Prostate 73(11):1233–1240. doi:10.1002/pros.22675
Nam RK, Sugar L, Wang Z, Yang W, Kitching R, Klotz LH et al (2007a) Expression of TMPRSS2: ERG gene fusion in prostate cancer cells is an important prognostic factor for cancer progression. Cancer Biol Ther 6(1):40–45
Nam RK, Sugar L, Yang W, Srivastava S, Klotz LH, Yang LY et al (2007b) Expression of the TMPRSS2: ERG fusion gene predicts cancer recurrence after surgery for localised prostate cancer. Br J Cancer 97(12):1690–1695
Ng HH, Bird A (2000) Histone deacetylases: silencers for hire. Trends Biochem Sci 25(3):121–126
Oh SH, Park TS, Choi JR, Lee S, Cho SY, Kim SY et al (2010) Two childhood cases of acute leukemia with t(16;21)(p11.2;q22): second case report of infantile acute lymphoblastic leukemia with unusual type of FUS-ERG chimeric transcript. Cancer Genet Cytogenet 200(2):180–183. doi:10.1016/j.cancergencyto.2010.04.009
Owczarek CM, Portbury KJ, Hardy MP, O’Leary DA, Kudoh J, Shibuya K et al (2004) Detailed mapping of the ERG–ETS2 interval of human chromosome 21 and comparison with the region of conserved synteny on mouse chromosome 16. Gene 324:65–77
Park K, Tomlins SA, Mudaliar KM, Chiu YL, Esgueva R, Mehra R et al (2010) Antibody-based detection of ERG rearrangement-positive prostate cancer. Neoplasia 12(7):590–598
Park K, Dalton JT, Narayanan R, Barbieri CE, Hancock ML, Bostwick DG et al (2014) TMPRSS2: ERG gene fusion predicts subsequent detection of prostate cancer in patients with high-grade prostatic intraepithelial neoplasia. J Clin Oncol 32(3):206–211. doi:10.1200/JCO.2013.49.8386
Perner S, Demichelis F, Beroukhim R, Schmidt FH, Mosquera JM, Setlur S et al (2006) TMPRSS2: ERG fusion-associated deletions provide insight into the heterogeneity of prostate cancer. Cancer Res 66(17):8337–8341
Petrovics G, Liu A, Shaheduzzaman S, Furusato B, Sun C, Chen Y et al (2005) Frequent overexpression of ETS-related gene-1 (ERG1) in prostate cancer transcriptome. Oncogene 24(23):3847–3852. doi:10.1038/sj.onc.1208518
Pflueger D, Rickman DS, Sboner A, Perner S, LaFargue CJ, Svensson MA et al (2009) N-myc downstream regulated gene 1 (NDRG1) is fused to ERG in prostate cancer. Neoplasia 11(8):804–811
Rajan P, Stockley J, Sudbery IM, Fleming JT, Hedley A, Kalna G et al (2014) Identification of a candidate prognostic gene signature by transcriptome analysis of matched pre- and post-treatment prostatic biopsies from patients with advanced prostate cancer. BMC Cancer 14:977. doi:10.1186/1471-2407-14-977
Rao VN, Papas TS, Reddy ES (1987) erg, a human ets-related gene on chromosome 21: alternative splicing, polyadenylation, and translation. Science 237(4815):635–639
Rao VN, Modi WS, Drabkin HD, Patterson D, O’Brien SJ, Papas TS et al (1988) The human erg gene maps to chromosome 21, band q22: relationship to the 8; 21 translocation of acute myelogenous leukemia. Oncogene 3(5):497–500
Reddy ES, Rao VN, Papas TS (1987) The erg gene: a human gene related to the ets oncogene. Proc Natl Acad Sci U S A 84(17):6131–6135
Ribeiro FR, Paulo P, Costa VL, Barros-Silva JD, Ramalho-Carvalho J, Jeronimo C et al (2011) Cysteine-rich secretory protein-3 (CRISP3) is strongly up-regulated in prostate carcinomas with the TMPRSS2-ERG fusion gene. PLoS One 6(7):e22317. doi:10.1371/journal.pone.0022317
Ropero S, Esteller M (2007) The role of histone deacetylases (HDACs) in human cancer. Mol Oncol 1(1):19–25. doi:10.1016/j.molonc.2007.01.001
Ross LE, Berkowitz Z, Ekwueme DU (2008) Use of the prostate-specific antigen test among U.S. men: findings from the 2005 National Health Interview Survey. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive. Oncology 17(3):636–644. doi:10.1158/1055-9965.EPI-07-2709
Setlur SR, Mertz KD, Hoshida Y, Demichelis F, Lupien M, Perner S et al (2008) Estrogen-dependent signaling in a molecularly distinct subclass of aggressive prostate cancer. J Natl Cancer Inst 100(11):815–825. doi:10.1093/jnci/djn150
Shah RB (2013) Clinical applications of novel ERG immunohistochemistry in prostate cancer diagnosis and management. Adv Anat Pathol 20(2):117–124. doi:10.1097/PAP.0b013e3182862ac5
Shah RB, Tadros Y, Brummell B, Zhou M (2013) The diagnostic use of ERG in resolving an “atypical glands suspicious for cancer” diagnosis in prostate biopsies beyond that provided by basal cell and alpha-methylacyl-CoA-racemase markers. Hum Pathol 44(5):786–794. doi:10.1016/j.humpath.2012.06.024
Sharrocks AD (2001) The ETS-domain transcription factor family. Nat Rev Mol Cell Biol 2(11):827–837. doi:10.1038/35099076
Shimizu K, Ichikawa H, Tojo A, Kaneko Y, Maseki N, Hayashi Y et al (1993) An ets-related gene, ERG, is rearranged in human myeloid leukemia with t(16;21) chromosomal translocation. Proc Natl Acad Sci U S A 90(21):10280–10284
Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63(1):11–30. doi:10.3322/caac.21166
Siegel RL, Miller KD, Jemal A (2015) Cancer statistics, 2015. CA Cancer J Clin 65(1):5–29. doi:10.3322/caac.21254
Slovin SF, Kelly WK, Wilton A, Kattan M, Myskowski P, Mendelsohn J et al (2009) Anti-epidermal growth factor receptor monoclonal antibody cetuximab plus Doxorubicin in the treatment of metastatic castration-resistant prostate cancer. Clin Genitourin Cancer 7(3):E77–E82. doi:10.3816/CGC.2009.n.028
Sorensen PH, Lessnick SL, Lopez-Terrada D, Liu XF, Triche TJ, Denny CT (1994) A second Ewing’s sarcoma translocation, t(21;22), fuses the EWS gene to another ETS-family transcription factor, ERG. Nat Genet 6(2):146–151. doi:10.1038/ng0294-146
Spencer ES, Johnston RB, Gordon RR, Lucas JM, Ussakli CH, Hurtado-Coll A et al (2013) Prognostic value of ERG oncoprotein in prostate cancer recurrence and cause-specific mortality. Prostate 73(9):905–912. doi:10.1002/pros.22636
Steurer S, Mayer PS, Adam M, Krohn A, Koop C, Ospina-Klinck D et al (2014) TMPRSS2-ERG fusions are strongly linked to young patient age in low-grade prostate cancer. Eur Urol 66(6):978–981. doi:10.1016/j.eururo.2014.06.027
Sun C, Dobi A, Mohamed A, Li H, Thangapazham RL, Furusato B et al (2008) TMPRSS2-ERG fusion, a common genomic alteration in prostate cancer activates C-MYC and abrogates prostate epithelial differentiation. Oncogene 27(40):5348–5353. doi:10.1038/onc.2008.183
Svensson MA, Perner S, Ohlson AL, Day JR, Groskopf J, Kirsten R et al (2014) A comparative study of ERG status assessment on DNA, mRNA, and protein levels using unique samples from a Swedish biopsy cohort. Appl Immunohistochem Mol Morphol 22(2):136–141. doi:10.1097/PDM.0b013e31829e0484
Teng LH, Wang C, Dolph M, Donnelly B, Bismar TA (2013) ERG protein expression is of limited prognostic value in men with localized prostate cancer. ISRN Urol 2013:786545. doi:10.1155/2013/786545
Terry S, Nicolaiew N, Basset V, Semprez F, Soyeux P, Maille P et al (2015) Clinical value of ERG, TFF3, and SPINK1 for molecular subtyping of prostate cancer. Cancer. doi:10.1002/cncr.29233
Thangapazham R, Saenz F, Katta S, Mohamed AA, Tan SH, Petrovics G et al (2014) Loss of the NKX3.1 tumorsuppressor promotes the TMPRSS2-ERG fusion gene expression in prostate cancer. BMC Cancer 14:16. doi:10.1186/1471-2407-14-16
Tian TV, Tomavo N, Huot L, Flourens A, Bonnelye E, Flajollet S et al (2014) Identification of novel TMPRSS2: ERG mechanisms in prostate cancer metastasis: involvement of MMP9 and PLXNA2. Oncogene 33(17):2204–2214. doi:10.1038/onc.2013.176
Tidehag V, Hammarsten P, Egevad L, Granfors T, Stattin P, Leanderson T et al (2014) High density of S100A9 positive inflammatory cells in prostate cancer stroma is associated with poor outcome. Eur J Cancer 50(10):1829–1835. doi:10.1016/j.ejca.2014.03.278
Tomlins SA, Rhodes DR, Perner S, Dhanasekaran SM, Mehra R, Sun XW et al (2005) Recurrent fusion of TMPRSS2 and ETS transcription factor genes in prostate cancer. Science 310(5748):644–648
Tomlins SA, Alshalalfa M, Davicioni E, Erho N, Yousefi K, Zhao S et al (2015a) Characterization of 1577 primary prostate cancers reveals novel biological and clinicopathologic insights into molecular subtypes. Eur Urol 68(4):555–567. doi:10.1016/j.eururo.2015.04.033
Tomlins SA, Day JR, Lonigro RJ, Hovelson DH, Siddiqui J, Kunju LP et al (2015b) Urine TMPRSS2: ERG plus PCA3 for individualized prostate cancer risk assessment. Eur Urol. doi:10.1016/j.eururo.2015.04.039
Toubaji A, Albadine R, Meeker AK, Isaacs WB, Lotan T, Haffner MC et al (2011) Increased gene copy number of ERG on chromosome 21 but not TMPRSS2-ERG fusion predicts outcome in prostatic adenocarcinomas. Mod Pathol 24(11):1511–1520. doi:10.1038/modpathol.2011.111
van Leenders GJ, Boormans JL, Vissers CJ, Hoogland AM, Bressers AA, Furusato B et al (2011) Antibody EPR3864 is specific for ERG genomic fusions in prostate cancer: implications for pathological practice. Mod Pathol 24(8):1128–1138. doi:10.1038/modpathol.2011.65
Wang J, Cai Y, Ren C, Ittmann M (2006) Expression of variant TMPRSS2/ERG fusion messenger RNAs is associated with aggressive prostate cancer. Cancer Res 66(17):8347–8351. doi:10.1158/0008-5472.CAN-06-1966
Wang J, Cai Y, Yu W, Ren C, Spencer DM, Ittmann M (2008) Pleiotropic biological activities of alternatively spliced TMPRSS2/ERG fusion gene transcripts. Cancer Res 68(20):8516–8524. doi:10.1158/0008-5472.CAN-08-1147
Wang JJ, Liu YX, Wang W, Yan W, Zheng YP, Qiao LD et al (2012) Fusion between TMPRSS2 and ETS family members (ERG, ETV1, ETV4) in prostate cancers from northern China. Asian Pac J Cancer Prev 13(10):4935–4938
Wilson S, Greer B, Hooper J, Zijlstra A, Walker B, Quigley J et al (2005) The membrane-anchored serine protease, TMPRSS2, activates PAR-2 in prostate cancer cells. Biochem J 388(Pt 3):967–972. doi:10.1042/BJ20041066
Yaskiv O, Zhang X, Simmerman K, Daly T, He H, Falzarano S et al (2011) The utility of ERG/P63 double immunohistochemical staining in the diagnosis of limited cancer in prostate needle biopsies. Am J Surg Pathol 35(7):1062–1068. doi:10.1097/PAS.0b013e318215cc03
Yoshimoto M, Joshua AM, Cunha IW, Coudry RA, Fonseca FP, Ludkovski O et al (2008) Absence of TMPRSS2:ERG fusions and PTEN losses in prostate cancer is associated with a favorable outcome. Mod Pathol 21(12):1451–1460. doi:10.1038/modpathol.2008.96
Yu J, Yu J, Mani RS, Cao Q, Brenner CJ, Cao X et al (2010) An integrated network of androgen receptor, polycomb, and TMPRSS2-ERG gene fusions in prostate cancer progression. Cancer Cell 17(5):443–454. doi:10.1016/j.ccr.2010.03.018
Acknowledgments
LZ and TAB drafted the manuscript. TAB supervised and oversight the manuscript outline.
Funding
This work was supported in part by the Prostate Cancer Foundation Young Investigator Award (T.A.B). This work was also supported by Prostate cancer Canada and is proudly funded by the Movember Foundation, Grant #B2013-01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare in this study.
Ethical approval
NA (review article).
Rights and permissions
About this article
Cite this article
Abou-Ouf, H., Zhao, L. & Bismar, T.A. ERG expression in prostate cancer: biological relevance and clinical implication. J Cancer Res Clin Oncol 142, 1781–1793 (2016). https://doi.org/10.1007/s00432-015-2096-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-015-2096-x