Abstract
Purpose
Metastasis-associated in colon cancer-1 (MACC1) is a newly identified gene that plays an important role in cancer progression and metastasis. MACC1 has important functions in the differentiation, invasion, and metastasis of nonsmall cell lung cancer (NSCLC). However, the value of circulating MACC1 as a potential diagnostic and prognostic biomarker for NSCLC remains unknown.
Methods
Plasma MACC1 mRNA levels were examined in 272 patients with NSCLC, 61 with benign lung disease, and 80 healthy volunteers using reverse transcription quantitative real-time polymerase chain reaction.
Results
MACC1 was more highly expressed in NSCLC patients than in patients with benign disease (P < 0.001) or in healthy volunteers (P < 0.001). High MACC1 expression was significantly associated with NSCLC stage (P = 0.013) and lymph node metastasis (P = 0.016). The area under the receiver operating characteristic curve was 0.766, and the optimal cutoff value was 0.105, providing a sensitivity of 71.4 % and a specificity of 89.1 %. The diagnostic capability of circulating MACC1 mRNA was higher than that of carcinoembryonic antigen (P = 0.025) or cytokeratin-19 (P = 0.010). Furthermore, high MACC1 expression was associated with poor overall survival (OS) and disease-free survival (DFS) and predicted poor survival in NSCLC patients. Consequently, MACC1 mRNA was an independent prognostic factor of OS and DFS.
Conclusion
We concluded that circulating MACC1 mRNA represents a potential noninvasive, diagnostic and prognostic marker for NSCLC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer, largely nonsmall cell lung cancer (NSCLC), is becoming the major cause of cancer and cancer-related mortality worldwide, with a five-year survival rate below 15 % after the initial diagnosis (Jemal et al. 2011; Siegel et al. 2011). This poor prognosis of NSCLC is largely associated with late-stage diagnosis, when a potential cure is unlikely. Moreover, a lack of effective treatments contributes to the poor survival of patients with early-stage lung cancer. Novel biomarkers with high sensitivity and specificity are therefore urgently needed to allow the early diagnosis of NSCLC and to encourage the development of new treatments (Alberg et al. 2007).
Some biomarkers have already been identified, including mutations in the KRAS, epidermal growth factor receptor, TP53 genes, and changes in the expression levels of carcinoembryonic antigen (CEA), cytokeratin-19 fragment (CK19), cancer antigen-125 (CA125), and neuron-specific enolase (NSE) (Arya and Bhansali 2011; Cabrera-Alarcon et al. 2011; Gridelli et al. 2011). However, the low sensitivities, specificities, and reproducibilities of these markers have limited their clinical value (Cho and Sung 2009; Huang et al. 2013a).
Studies on circulating mRNA have increased since the first detection of plasma RNA in nasopharyngeal carcinoma and melanoma (Kopreski et al. 1999; Lo et al. 1999). Numerous circulating RNAs have been found in different types of carcinomas (Gahan 2010). Furthermore, many highly expressed circulating RNAs have been shown to correlate with tumor diagnosis and prognosis (Gahan 2010; Holdenrieder et al. 2010). Detection of circulating RNA thus represents a promising noninvasive strategy for tumor diagnosis and prognosis, and for monitoring antitumor therapies.
Metastasis-associated in colon cancer-1 (MACC1) is a novel gene that was initially detected in colon cancer (Stein et al. 2009). MACC1 is located on human chromosome 7p 21.1 and encodes a protein containing four domains: ZU5, SH3, and two C-terminal death domains related to signal transduction and cell apoptosis (Kokoszynska et al. 2009). MACC1 has been identified in relation to the proliferation and invasion of colon cancer, both in vivo and in vitro (Stein et al. 2009). Moreover, recent studies have shown that MACC1 is overexpressed in epithelial ovarian cancer (Zhang et al. 2011), hepatocellular carcinoma (Qiu et al. 2011; Xie et al. 2013), rectal cancer (Kawamura et al. 2012), pancreatic cancer (Wang et al. 2012), lung cancer (Chundong et al. 2011; Hu et al. 2012; Shimokawa et al. 2011; Wang et al. 2014), nasopharyngeal carcinoma (Meng et al. 2013), breast cancer (Huang et al. 2013b), osteosarcoma (Zhang et al. 2013b), glioma (Hagemann et al. 2013; Yang et al. 2013), esophageal cancer (Zhu et al. 2013), and gastric cancer (Guo et al. 2013; Wang et al. 2013), where it has been associated with tumor metastasis, progression, and prognosis.
In order to allow repeated, noninvasive measurements, the detection of MACC1 by blood-based assays needs to be considered. Circulating MACC1 mRNA was first detected in colorectal cancer by Stein (Stein et al. 2012) and represents a promising diagnostic and prognostic biomarker of metastasis and survival, and for monitoring therapeutic responses in cancer patients. However, the value of circulating MACC1 for the diagnosis and prognosis of NSCLC remains unknown. We therefore retrospectively examined the expression status of plasma MACC1 mRNA in NSCLC patients and healthy volunteers to assess its value as a biomarker for NSCLC.
Materials and methods
Patients
This study was authorized by the Ethics Committee of the Affiliated Hospital of Jiangnan University. All plasma specimens and clinical materials were obtained and used with prior written informed consent from the patients and the Affiliated Hospital of Jiangnan University.
This study analyzed data for consecutive patients with NSCLC from the Department of Cardiothoracic Surgery at the Affiliated Hospital of Jiangnan University between January 2007 and December 2007. A total of 272 eligible patients were finally enrolled, including 149 with squamous carcinoma and 123 with adenocarcinoma. Tumors were classified according to the TNM cancer staging system (2009) set by the Union of International Cancer Control, and the patients were divided into stage I (n = 35), stage II (n = 68), stage III (n = 74), and stage IV (n = 95). Of the 272 patients (142 male, 130 female), 140 underwent radical surgery. The control group included 61 patients (34 male, 27 female) with benign lung diseases such as hamartoma, pneumonia, and phthisis, and 80 healthy volunteers (45 male, 35 female). None of the control patients had formerly been diagnosed with any malignancy. Blood samples were taken from patients on the day of diagnosis, prior to any surgery and therapy.
Patients were followed up every 1–3 months for the first year, and every 3–6 months thereafter for at least 5 years, by telephone, correspondence, or clinical assessments. The study was censored on April 30, 2013. The median follow-up time was 23 months (range 3–75 months). The study end point was death. Patients underwent routine physical examinations, blood tests, abdominal ultrasonography, bone scintigraphy, and imaging studies. For patients who underwent surgery, the overall survival time (OS) was calculated from the date of diagnosis to death (or last follow-up), and disease-free survival (DFS) was defined as the period from diagnosis to first locoregional or distant recurrence.
Plasma preparation and RNA extraction
Plasma was separated as described previously (Stein et al. 2011, 2012; Fleischhacker et al. 2001). A volume of 5 ml of EDTA-anticoagulated blood was obtained from each patient and healthy volunteer. Plasma separation was carried out using cooled EDTA-blood on the same day, within 7 h of blood collection. The 5 ml of cooled EDTA-anticoagulated blood was separated by centrifugation at 1,600g for 10 min at 4 °C followed by a second centrifugation at 16,000g for 10 min at 4 °C to eliminate any cell debris. Finally, plasma samples were stored at −80 °C until use. All samples were blinded to the manipulators, and neither clinical nor pathological data were disclosed during detection.
RNA was extracted from 3 ml of plasma using TRIzol LS reagent (Invitrogen, Life Technologies, Paisley, UK), as described previously (Zhang et al. 2012). The procedure was carried out according to manufacturer’s instructions, with minor modifications, as follows. A concentrator was used to concentrate each plasma sample at 4 °C, followed by separation into six aliquots. TRIzol LS reagent (Invitrogen) (750 μl) was mixed with each aliquot and incubated at room temperature for 5 min, followed by the addition of 200 μl chloroform and shaking for 15 s. The mixture was incubated at room temperature for another 10 min followed by centrifugation at 12,000g at 4 °C for 15 min. The supernatant was obtained and mixed with 0.5 ml isopropyl alcohol. The mixture was then precipitated at −20 °C for 16 h, centrifuged at 12,000g at 4 °C for 15 min, followed by washing with 1 ml 75 % ethanol. Finally, the RNA pellet was dehydrated at room temperature for 5–10 min and dissolved in 20 μl Rnase-free water at 60 °C. All aliquots were pooled, and the RNA concentration was detected by spectrophotometric analysis. The final RNA concentration ranged from 2.54–11.27 ng/μl.
Reverse transcription quantitative real-time polymerase chain reaction
All plasma samples were evaluated by reverse transcription quantitative real-time polymerase chain reaction (RT-qPCR) as described previously (Qiu et al. 2011; Zhang et al. 2012). The procedure was conducted in a blinded manner, with no knowledge of the clinical or follow-up data. cDNA was generated by reverse transcription of 100 ng RNA from each sample in triplicate, using PrimeScript RT (Takara, Dalian, China), according to the manufacturer’s instructions. The resulting cDNA was pooled and amplified by PCR. RT-qPCR was performed using a SYBR green I Master Mix kit (Invitrogen). The primers (GenScript, NanJing, China) were 5′-GGATGCGTGCATTTATCAGA-3′ (forward) and 5′-GTTGATAGGGCAGACGTTCG-3′ (reverse) for 18 s rRNA; and 5′-TTCTTTTGATTCCTCCGGTGA-3′ (forward) and 5′-ACTCTGATGGGCATGTGCTG-3′ (reverse) for MACC1. RT-qPCR was carried out using an ABI Prism7900 HT Sequence Detection System (Applied Biosystems, Foster, CA, USA). 18 s rRNA was also analyzed for normalization of the RT-qPCR results. Lung cancer A549 cells were used as a positive control for each run of amplification, and samples lacking cDNA were used as a negative control. The ratio between MACC1 and 18 s rRNA was calculated as the normalized expression level of MACC1 in each sample.
Plasma CEA and CK-19 assays
CK19 and CEA are the most frequently investigated NSCLC biomarkers (Holdenrieder et al. 2010). CEA is considered to be a more valuable indicator for adenocarcinoma, while CK19 is used for squamous cell carcinomas (Cabrera-Alarcon et al. 2011). We compared the diagnostic values of plasma MACC1 mRNA, and plasma CEA and CK19 by enzyme-linked immunosorbent assay using an ARCHITECT i2000 SR system (Abbott Laboratories, Chicago, USA), according to the manufacturer’s protocol. The immunoassay kits were from Cusabio (Wuhan, China). According to the manufacturers, upper limits of 5–4 ng/ml were used to define the normal ranges for CEA and CK-19, respectively. Results were compared with standard curves, and all measurements were done in triplicate.
Statistical analysis
All statistical analyses were carried out using SPSS 19.0 (SPSS, Chicago, IL, USA). The data were characterized by median values and interquartile ranges. The Kolmogorov–Smirnov test was used to analyze the distribution of samples in each group. Mann–Whitney U and Kruskal–Wallis tests were performed to assess the differences between nonparametric distributed variables. Subjects with or without NSCLC were discriminated by receiver operating characteristic curve (ROC) analysis. The optimal cutoff value of circulating MACC1 mRNA was determined by the Youden index (sensitivity + specificity − 1). The Kaplan–Meier method was used to depict survival curves, and comparisons were made using log-rank tests. A forward stepwise Cox proportional hazards regression model analysis was used to estimate the independent prognostic factors for OS and DFS.
Results
Plasma MACC1 expression in patients with NSCLC, benign lung disease, and healthy volunteers
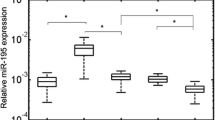
We analyzed MACC1 mRNA levels in 272 patients with NSCLC, 61 with benign lung disease, and 80 healthy volunteers. The dissociation curve showed a single peak for MACC1 mRNA. RT-qPCR indicated MACC1 mRNA expression in all samples, but with higher levels in patients with NSCLC than in those with benign disease (P < 0.001) or in healthy volunteers (P < 0.001) (Fig. 1a). CEA and CK19 levels were also higher in patients with NSCLC than in nontumor groups. Table 1 shows the relative levels of circulating MACC1 mRNA in each group.
Correlations between MACC1 mRNA expression and clinical parameters
We analyzed the correlation between MACC1 mRNA levels and various NSCLC clinical parameters (Table 2). Circulating MACC1 mRNA levels were significantly positively correlated with clinical stage (P = 0.013) (Fig. 1b) and regional lymph node metastasis (P = 0.016). There were no significant correlations between age, sex, tumor size, histological type, or cell differentiation and MACC1 levels (all P > 0.05). Regarding tumor stage, MACC1 mRNA levels were higher in patients with stage Ι NSCLC than in healthy controls (P = 0.027) and were similar to levels in patients with stage II and III NSCLC (P = 0.224), but lower than in those with stage IV NSCLC (P < 0.001) (Fig. 1b).
Diagnostic performance of circulating MACC1 mRNA for NSCLC
To evaluate the diagnostic value of circulating MACC1 mRNA, we compared its levels with those of the conventional tumor markers, CEA and CK19, using ROC analysis (Fig. 2a–e). The optimal cutoff point for MACC1 mRNA in NSCLC patients was 0.105, providing a sensitivity of 71.4 % and a specificity of 89.1 %. However, the optimal cutoff points were 7.46 (sensitivity of 65.4 % and specificity of 87.2 %) for CEA in NSCLC patients and 4.05 for CK19 (sensitivity of 68.6 % and specificity of 83.1 %). The area under the ROC curve (AUC) for circulating MACC1 mRNA for the detection of NSCLC was 0.766, which was significantly higher than that for CEA (0.713) or CK19 (0.705) alone, but lower than that for the combination of CEA and CK19 (0.785), indicating that circulating MACC1 mRNA might be a more reliable marker than conventional tumor markers for discriminating between NSCLC and nontumor cases. Meanwhile, ROC analysis gave an AUC for the combination of circulating MACC1 mRNA, CEA, and CK19 of 0.812 (Fig. 2e), which was significantly higher than that for circulating MACC1 mRNA alone (P = 0.014). Regarding its diagnostic ability for early NSCLC, MACC1 revealed a sensitivity of 63.5 % and specificity of 77.4 % with an AUC of 0.663 for distinguishing between stage Ι NSCLC and nontumor groups (Fig. 2f).
Correlation between MACC1 mRNA expression and prognostic survival
Patients with NSCLC were divided into two groups according to MACC1 expression levels: patients with values below the median (0.184) of all NSCLC patients (low-level group; n = 136), and the remainder (high-expression group; n = 136).
Kaplan–Meier survival curves demonstrated that high MACC1 mRNA expression was significantly associated with reduced OS (P = 0.004, Fig. 3a) and DFS (P = 0.006, Fig. 3b). Univariate Cox proportional hazards regression model analysis (Table 3) showed that OS was associated with MACC1 mRNA level (P = 0.008), tumor size (P = 0.031), clinical stage (P < 0.001), lymph node metastasis (P = 0.023), and cell differentiation (P = 0.034). MACC1 mRNA level (P = 0.014), clinical stage (P = 0.040), and lymph node metastasis (P = 0.006) were significantly correlated with DFS. Parameters significantly correlated with survival in univariate analysis were brought into multivariate analysis to identify the independent prognostic factors. MACC1 mRNA level and lymph node metastasis were independent prognostic factors for DFS (P = 0.036 and P = 0.009, respectively), whereas MACC1 mRNA level and clinical stage were independently related to OS (P = 0.012 and P = 0.001, respectively).
Discussion
MACC1 has been identified overexpressed in many tumors and been associated with tumor metastasis, progression, and prognosis, but the molecular mechanisms remain unclear. However, previous studies showed that MACC1 may activate and regulate the hepatocyte growth factor (HGF)/c-Met signaling pathway in colon cancer via transcriptional activation of c-Met by binding Sp1 (Kokoszynska et al. 2009; Stein et al. 2009). The signaling pathway was shown to lead to colon cancer cell proliferation, invasion, and migration in vitro (Stein et al. 2010), as well as to colon cancer metastasis and recurrence in vivo (Arlt and Stein 2009; Boardman 2009). MACC1 and c-Met have also been shown to be consistently overexpressed in hepatocellular carcinoma (Qiu et al. 2011), rectal cancer (Kawamura et al. 2012), NSCLC (Hu et al. 2012), epithelial ovarian cancer (Hu et al. 2012), colorectal cancer (Isella et al. 2013), and gastric cancer (Guo et al. 2013). The consistent overexpression of MACC1 and c-Met suggests that MACC1 may play a key role in tumor development, progression, and metastasis via the c-Met signaling pathway. Moreover, studies have also reported that MACC1, combined with c-Met and HGF, may activate downstream signaling pathways, including the Akt/ß-catenin (Meng et al. 2013; Zhang et al. 2013a), Ras/ERK (Wang et al. 2012) and EMT (Wang et al. 2013) signaling pathways, and that this could be inhibited by MACC1 siRNA (Stein et al. 2009; Wang et al. 2012). In addition, bioinformatic analyses indicated that MACC1 was associated with apoptosis in MET signaling (Kokoszynska et al. 2009).
We investigated the diagnostic and prognostic values of plasma MACC1 mRNA for NSCLC, measured using a quantitative, noninvasive assay suitable for the routine clinical monitoring of tumor patients. Plasma MACC1 mRNA levels were significantly higher in patients with NSCLC, compared with patients with benign lung diseases or healthy volunteers. Moreover, circulating MACC1 mRNA was more suitable for detecting NSCLC than the traditional NSCLC diagnostic markers, CEA and CK19. Importantly, survival analysis showed that high plasma MACC mRNA predicted poor OS and DFS in NSCLC, and plasma MACC1 mRNA was identified as an independent prognostic factor of NSCLC.
In previous studies, tumor progression, metastasis, and survival have been associated with expression level of MACC1. This was confirmed in our study that circulating MACC1 mRNA was significantly increased in patients with NSCLC, consistent with the results that found in NSCLC tissues (Chundong et al. 2011; Hu et al. 2012; Shimokawa et al. 2011; Wang et al. 2014). The results of this study showed that high plasma MACC1 mRNA levels were associated with advanced NSCLC stage and positive lymph node metastasis. This can be explained by the entry of increasing numbers of circulating tumor cells into the peripheral blood as the tumor progresses (Muinelo-Romay et al. 2014; Sun et al. 2011), thus increasing the levels of circulating MACC1 mRNA. Plasma MACC1 mRNA was also identified as an independent prognostic marker for NSCLC; patients with high MACC1 mRNA levels had poorer OS and DFS than those with lower levels. Similar results were demonstrated in colon cancer patients, where patients with higher circulating MACC1 mRNA levels showed shorter OS and DFS (Stein et al. 2012). These results suggest that circulating MACC1 mRNA may be serving as a predictor of high or low risk for NSCLC.
Many circulating biomarkers can be used to help diagnose NSCLC, of which the most widely used are CEA and CK19 (Holdenrieder et al. 2010). However, their low sensitivities and specificities limit their clinical application, especially for the diagnosis of early NSCLC. The results of the current study suggest that circulating MACC1 mRNA may represent a useful biomarker for NSCLC, with a sensitivity of 71.4 %, a specificity of 89.1 %, and an AUC of 0.766. Regarding its ability to identify early NSCLC, plasma MACC1 mRNA was higher in stage Ι NSCLC than in nontumor groups, with a sensitivity of 63.5 %, specificity of 77.4 %, and an AUC of 0.663 for distinguishing between stage Ι and nontumor patients. We therefore conclude that plasma MACC1 mRNA represents a useful diagnostic biomarker for early stage, as well as later-stage NSCLC.
The results of this study suggest that MACC1 might be a more suitable plasma biomarker than CEA or CK19 for distinguishing between NSCLC and nontumor cases. The AUC for MACC1 was higher than that for CEA or CK19, indicating that circulating MACC1 mRNA had a higher diagnostic value than CEA or CK19 for NSCLC. Furthermore, the combination of circulating MACC1 mRNA, CEA, and CK19 had a significantly larger AUC than that of MACC1 alone, suggesting that this combination might further improve the diagnosis of NSCLC.
This study had certain limitations. Firstly, circulating MACC1 mRNA is expressed in healthy individuals and in patients with different types of tumors and is not specific for NSCLC. Secondly, the number of patients involved in the study was small, and further studies with larger numbers of patients are needed to validate the results. In addition, the patients in this study all came from one hospital and the study results may differ according to the techniques used. Multicenter studies are therefore required to confirm the value of MACC1 mRNA as a diagnostic and prognostic marker.
In conclusion, plasma MACC1 mRNA levels were significantly higher in patients with NSCLC compared with healthy volunteers, suggesting that MACC1 might represent a useful biomarker for distinguishing between early NSCLC patients and nontumor individuals. Blood levels of MACC1 show promise as a diagnostic and prognostic biomarker in patients with NSCLC. Further prospective studies with larger cohorts are required to clarify the value of plasma MACC1 mRNA as a useful marker for screening response to chemotherapy and detecting tumor recurrence in NSCLC, and the mechanisms responsible for the role of MACC1 in cancer should also need to be clarified.
References
Alberg AJ, Ford JG, Samet JM, American College of Chest P (2007) Epidemiology of lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 132:29S–55S. doi:10.1378/chest.07-1347
Arlt F, Stein U (2009) Colon cancer metastasis: MACC1 and Met as metastatic pacemakers. Int J Biochem Cell Biol 41:2356–2359. doi:10.1016/j.biocel.2009.08.001
Arya SK, Bhansali S (2011) Lung cancer and its early detection using biomarker-based biosensors. Chem Rev 111:6783–6809. doi:10.1021/cr100420s
Boardman LA (2009) Overexpression of MACC1 leads to downstream activation of HGF/MET and potentiates metastasis and recurrence of colorectal cancer. Genome Med 1:36. doi:10.1186/gm36
Cabrera-Alarcon JL, Carrillo-Vico A, Santotoribio JD, Leon-Justel A, Sanchez-Gil R, Gonzalez-Castro A, Guerrero JM (2011) CYFRA 21-1 as a tool for distant metastasis detection in lung cancer. Clin Lab 57:1011–1014
Cho JY, Sung HJ (2009) Proteomic approaches in lung cancer biomarker development. Expert Rev Proteomics 6:27–42. doi:10.1586/14789450.6.1.27
Chundong G et al (2011) Molecular diagnosis of MACC1 status in lung adenocarcinoma by immunohistochemical analysis. Anticancer Res 31:1141–1145
Fleischhacker M, Beinert T, Ermitsch M, Seferi D, Possinger K, Engelmann C, Jandrig B (2001) Detection of amplifiable messenger RNA in the serum of patients with lung cancer. Ann N Y Acad Sci 945:179–188
Gahan PB (2010) Circulating nucleic acids in plasma and serum: diagnosis and prognosis in cancer. EPMA J 1:503–512. doi:10.1007/s13167-010-0021-6
Gridelli C, Rossi A, Maione P (2011) 2010 Consensus on lung cancer, new clinical recommendations and current status of biomarker assessment—first-line therapy. Eur J Cancer 47(Suppl 3):s248–s257. doi:10.1016/S0959-8049(11)70171-X
Guo T, Yang J, Yao J, Zhang Y, Da M, Duan Y (2013) Expression of MACC1 and c-Met in human gastric cancer and its clinical significance. Cancer Cell Int 13:121. doi:10.1186/1475-2867-13-121
Hagemann C et al (2013) Impact of MACC1 on human malignant glioma progression and patients’ unfavorable prognosis. Neurooncol 15:1696–1709. doi:10.1093/neuonc/not136
Holdenrieder S, Nagel D, Stieber P (2010) Estimation of prognosis by circulating biomarkers in patients with non-small cell lung cancer. Cancer Biomark 6:179–190. doi:10.3233/CBM-2009-0128
Hu X, Fu X, Wen S, Zou X, Liu Y (2012) Prognostic value of MACC1 and c-met expressions in non-small cell lung cancer. Chin J Lung Cancer 15:399–403. doi:10.3779/j.issn.1009-3419.2012.07.02
Huang J, Wang K, Xu J, Huang J, Zhang T (2013a) Prognostic significance of circulating tumor cells in non-small-cell lung cancer patients: a meta-analysis. PloS One 8:e78070. doi:10.1371/journal.pone.0078070
Huang Y et al (2013b) Overexpression of MACC1 and its significance in human. Breast Cancer Progress Cell Biosci 3:16. doi:10.1186/2045-3701-3-16
Isella C et al (2013) MACC1 mRNA levels predict cancer recurrence after resection of colorectal cancer liver metastases. Ann Surg 257:1089–1095. doi:10.1097/SLA.0b013e31828f96bc
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61:69–90. doi:10.3322/caac.20107
Kawamura M et al (2012) Correlation of MACC1 and MET expression in rectal cancer after neoadjuvant chemoradiotherapy. Anticancer Res 32:1527–1531
Kokoszynska K, Krynski J, Rychlewski L, Wyrwicz LS (2009) Unexpected domain composition of MACC1 links MET signaling and apoptosis. Acta Biochim Pol 56:317–323
Kopreski MS, Benko FA, Kwak LW, Gocke CD (1999) Detection of tumor messenger RNA in the serum of patients with malignant melanoma. Clin Cancer Res 5:1961–1965
Lo KW et al (1999) Analysis of cell-free Epstein-barr virus associated RNA in the plasma of patients with nasopharyngeal carcinoma. Clin Chem 45:1292–1294
Meng F et al (2013) MACC1 down-regulation inhibits proliferation and tumourigenicity of nasopharyngeal carcinoma cells through Akt/beta-catenin signaling pathway. PLoS One 8:e60821. doi:10.1371/journal.pone.0060821
Muinelo-Romay L et al (2014) Evaluation of circulating tumor cells and related events as prognostic factors and surrogate biomarkers in advanced NSCLC patients receiving first-line systemic treatment. Cancers 6:153–165. doi:10.3390/cancers6010153
Qiu J et al (2011) Identification of MACC1 as a novel prognostic marker in hepatocellular carcinoma. J Transl Med 9:166. doi:10.1186/1479-5876-9-166
Shimokawa H, Uramoto H, Onitsuka T, Chundong G, Hanagiri T, Oyama T, Yasumoto K (2011) Overexpression of MACC1 mRNA in lung adenocarcinoma is associated with postoperative recurrence. J Thorac Cardiovasc Surg 141:895–898. doi:10.1016/j.jtcvs.2010.09.044
Siegel R, Ward E, Brawley O, Jemal A (2011) Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin 61:212–236. doi:10.3322/caac.20121
Stein U et al (2009) MACC1, a newly identified key regulator of HGF-MET signaling, predicts colon cancer metastasis. Nat Med 15:59–67. doi:10.1038/nm.1889
Stein U, Dahlmann M, Walther W (2010) MACC1—more than metastasis? Facts and predictions about a novel gene. J Mol Med 88:11–18. doi:10.1007/s00109-009-0537-1
Stein U, Burock S, Herrmann P, Wendler I, Niederstrasser M, Wernecke KD, Schlag PM (2011) Diagnostic and prognostic value of metastasis inducer S100A4 transcripts in plasma of colon, rectal, and gastric cancer patients. J Mol Diagn 13:189–198. doi:10.1016/j.jmoldx.2010.10.002
Stein U, Burock S, Herrmann P, Wendler I, Niederstrasser M, Wernecke KD, Schlag PM (2012) Circulating MACC1 transcripts in colorectal cancer patient plasma predict metastasis and prognosis. PLoS One 7:e49249. doi:10.1371/journal.pone.0049249
Sun YF, Yang XR, Zhou J, Qiu SJ, Fan J, Xu Y (2011) Circulating tumor cells: advances in detection methods, biological issues, and clinical relevance. J Cancer Res Clin Oncol 137:1151–1173. doi:10.1007/s00432-011-0988-y
Wang G, Kang MX, Lu WJ, Chen Y, Zhang B, Wu YL (2012) MACC1: a potential molecule associated with pancreatic cancer metastasis and chemoresistance. Oncol Lett 4:783–791. doi:10.3892/ol.2012.784
Wang L et al (2013) Metastasis-associated in colon cancer-1 upregulation predicts a poor prognosis of gastric cancer, and promotes tumor cell proliferation and invasion. Int J Cancer 133:1419–1430. doi:10.1002/ijc.28140
Wang Z et al (2014) MACC1 overexpression predicts a poor prognosis for non-small cell lung cancer. Med Oncol 31:790. doi:10.1007/s12032-013-0790-6
Xie C et al (2013) MACC1 as a prognostic biomarker for early-stage and AFP-normal hepatocellular carcinoma. PLoS One 8:e64235. doi:10.1371/journal.pone.0064235
Yang T et al (2013) Overexpression of MACC1 protein and its clinical implications in patients with glioma. Tumour Biol. doi:10.1007/s13277-013-1112-5
Zhang RT, Shi HR, Huang HL, Chen ZM, Liu HN, Yuan ZF (2011) Expressions of MACC1, HGF, and C-met protein in epithelial ovarian cancer and their significance. J South Med Univ 31:1551–1555
Zhang X et al (2012) Detection of circulating Bmi-1 mRNA in plasma and its potential diagnostic and prognostic value for uterine cervical cancer. Int J Cancer 131:165–172. doi:10.1002/ijc.26360
Zhang K et al (2013a) MACC1 is involved in the regulation of proliferation, colony formation, invasion ability, cell cycle distribution, apoptosis and tumorigenicity by altering Akt signaling pathway in human osteosarcoma. Tumour Biol. doi:10.1007/s13277-013-1335-5
Zhang K, Zhang Y, Zhu H, Xue N, Liu J, Shan C, Zhu Q (2013b) High expression of MACC1 predicts poor prognosis in patients with osteosarcoma. Tumour Biol. doi:10.1007/s13277-013-1180-6
Zhu M, Xu Y, Mao X, Gao Y, Shao L, Yan F (2013) Overexpression of metastasis-associated in colon cancer-1 associated with poor prognosis in patients with esophageal cancer. Pathol Oncol Res 19:749–753. doi:10.1007/s12253-013-9638-9
Acknowledgments
We would like to thank Yonggong Wang, Yang Xia, and Jiajie Hou from Nanjing Medical University for technical assistance.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, Z., Cai, M., Weng, Y. et al. Circulating MACC1 as a novel diagnostic and prognostic biomarker for nonsmall cell lung cancer. J Cancer Res Clin Oncol 141, 1353–1361 (2015). https://doi.org/10.1007/s00432-014-1903-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-014-1903-0