Abstract
Bronchopulmonary dysplasia (BPD) poses a significant challenge as the most common late morbidity of preterm infants. This study aimed to evaluate airway abnormalities in infants with BPD who underwent flexible bronchoscopy (FB) to gain insights into the prevalence of upper airway obstruction and associated complications. A retrospective case–control study was conducted on BPD patients who underwent FB at a tertiary center between 2013 and 2023. BPD patients were matched (1:3) with a reference group based on age, gender, and ethnicity, who also had undergone FB. Demographic data, comorbidities, indications for FB, findings, and complications during and after FB were collected. The study included 50 BPD patients (mean age 1.26 ± 0.9 years, 58% males), and 150 controls. As expected, BPD patients had a lower gestational age, lower birth weight, and longer hospitalizations and were treated with more medications. Abnormal bronchoscopy findings were significantly more common in the BPD group compared to the reference group, with an increased rate of turbinate hypertrophy (OR [95% CI]: 3.44 [1.27–9.37], P = 0.014), adenoid hypertrophy (OR: 2.7 [1.38–5.29], P = 0.004), lingual tonsils (OR: 5.44 [1.29–27.4], P = 0.0024), subglottic stenosis (OR: 6.95 [2.08–27.1], P = 0.002), and tracheomalacia (OR: 2.98 [1.06–8.19], P = 0.034). Complications including desaturation (OR: 3.89 [1.32–11.7], P = 0.013) and PICU admission (OR: 16.6 [2.58–322], P = 0.011) were more frequent in the BPD than in the reference group.
Conclusion: The study revealed a high prevalence of structural anomalies leading to upper airway obstruction and complications in infants with BPD undergoing FB. These findings emphasize the importance of careful consideration and preparation for bronchoscopic procedures in this vulnerable population.
What is known: • Bronchopulmonary dysplasia (BPD) represents the most prevalent late morbidity among preterm infants. • Preterm infants diagnosed with BPD frequently undergo diagnostic procedures, including flexible and rigid bronchoscopies, to identify structural pathologies within the respiratory tract. | |
What is new: • A significantly higher prevalence of structural anomalies leading to upper airway obstruction was observed in the BPD group compared to controls. • The incidence of complications during flexible bronchoscopy was higher in the BPD group than in controls. |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Bronchopulmonary dysplasia (BPD) is a chronic lung disease of premature infants, defined by the need for supplemental oxygen at 36 weeks postmenstrual age [1,2,3,4]. It is the most common late morbidity of preterm birth, affecting approximately 10,000 infants per year in the USA [5]. Despite improved perinatal care, the overall incidence of BPD has remained unchanged over the past few decades due to the increased survival of extremely premature infants. The incidence of BPD in infants born before 28 weeks of gestational age (GA) is estimated between 48 and 68%, with the incidence being inversely proportional to GA [6].
The pathogenesis of BPD is multifactorial. In addition to GA and birth weight, other risk factors include antenatal factors such as genetic susceptibility, intrauterine growth retardation, and pregnancy-induced hypertensive disorders. Postnatal factors include ventilator-induced lung injury, patent ductus arteriosus, and infections [7]. BPD presumably results from an imbalance between lung injury and repair mechanisms in the developing immature lung [8]. Histopathological features show arrested alveolar-capillary development with large, simplified alveoli, increased interstitial fibrosis, and abnormal pulmonary vasculature with decreased branching and precapillary arteriovenous anastomoses [9].
Long-term respiratory morbidity with BPD includes the development of asthma, chronic obstructive pulmonary disease, and pulmonary vascular abnormalities [10,11,12,13,14]. Infants with lack of lung development and persistent structural abnormalities due to BPD have a higher vulnerability to lower respiratory tract infections (LRTI) than term infants and healthy premature infants, which can result in frequent and prolonged hospitalizations, pediatric intensive care unit (PICU) admissions, and the need for mechanical ventilation [15,16,17,18,19]. Histopathologic specimens from adolescents with BPD show thickened basement membranes with lymphocytic infiltration and signs of immature neo-angiogenesis, indicating the presence of active ongoing airway disease [20,21,22]. Aside from the reported alveolar damage, neonates with BPD may also experience tracheobronchial changes such as partial or near-total airway occlusion by abnormal tissue growth, tracheomalacia, bronchomalacia, and thickened secretions [23].
Considering the high prevalence of respiratory symptoms in premature infants with BPD, they often undergo various diagnostic procedures, including flexible and rigid bronchoscopies to diagnose structural pathologies in the respiratory tract [24, 25]. Flexible bronchoscopy, which is typically performed under general anesthesia while maintaining spontaneous breathing with supplementary oxygen, is a useful method for both diagnostic assessments and therapeutic interventions.
However, there is only scant data regarding the long-term effects of BPD on the upper airway and tracheobronchial tree. Furthermore, there is limited data on the complications experienced by BPD patients compared to non-BPD patients undergoing flexible bronchoscopy.
This study aims to describe the indications, findings, and complications of flexible bronchoscopy in pediatric BPD patients compared to a matched control group of children with respiratory symptoms but without BPD. We hypothesize a higher rate of abnormal bronchoscopies and complications among BPD patients compared with the reference group.
Methods
Study design
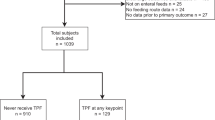
This is a retrospective matched cohort study that evaluated patients with BPD who underwent flexible bronchoscopy (FB) between 2013 and 2023 at Soroka University Medical Center, a single tertiary center in southern Israel. The BPD patients were compared to a reference group of children without BPD, who were matched based on age (± 6 months), sex, and ethnicity. The reference group (with a 1:3 ratio) underwent flexible bronchoscopy at our center for various respiratory indications during the same study period.
Study population
The study included pediatric patients aged 0–6 years old who had been previously diagnosed with BPD. To meet the definition of BPD, these patients had to be born at or before 32 weeks of gestation and required supplemental oxygen at the age of 36 weeks postmenstrual. BPD severity was classified at 36 weeks into grade 1 if the premature infant required 2 L/min nasal cannula or less, grade 2 if the premature infant required more than 2 L/min or other forms of non-invasive ventilation support, and grade 3 if the premature infant required invasive mechanical ventilation [4]. Only those who had undergone FB were included. Any patient lacking comprehensive data in their medical records regarding FB was excluded. A pediatric pulmonologist assessed each patient before they proceeded with the bronchoscopy.
Bronchoscopies
FBs were conducted either in the pediatric bronchoscopy suite or within the NICU/PICU, utilizing Olympus pediatric bronchoscopes with external diameters ranging from 2.8 o 3.6 mm. These procedures included an assessment of both upper and lower airways. However, they did not include an ENT exam using rigid bronchoscopy. Sedation was typically administered by a pediatric anesthesiologist or a PICU specialist, and patients were maintained on oxygen via a reservoir mask throughout the procedure. In instances where a patient was already intubated, the bronchoscopy was performed through the endotracheal tube or laryngeal mask. For these patients, upper airway evaluation was performed as a separate procedure at a time when the patient was not intubated.
Data collection
Data was collected from the FB medical records for both patients with and without BPD. Demographic information included age, gender, and ethnicity. Medical comorbidities included both respiratory and non-respiratory illnesses. Additional data gathered included whether the FB was elective or urgent, the patient’s hospitalization status in the pediatric ward or NICU/PICU at the time of the procedure, the length of hospitalization, the indication for FB, bronchoscopy findings of the upper and lower airway, and any complications. Specifically, indications for FB related to sleep apnea were based on a history of snoring, observed apnea during sleep, or prior polysomnography results, with an apnea–hypopnea index ≥ 5. Stridor and wheezing were diagnosed based on a physical examination by a pediatric pulmonologist. Complications included desaturation (oxygen saturation ≤ 90%) necessitating the termination of the procedure, the need for intubation, bleeding, fever (defined as a rectal temperature > 38 °C within 24 h post-procedure), and hospitalization in a pediatric ward or PICU within 72 h following the procedure. The study received approval from the institutional review board at Soroka University Medical Center (No. 532–20 SOR).
Statistical analysis
Descriptive statistical analyses were performed to evaluate different characteristics of the study population. Continuous variables with a normal distribution are depicted as mean ± standard deviation (SD), whereas continuous variables with non-normal distribution or ordinal variables are depicted as the median and interquartile range (IQR). Categorical variables are depicted as frequency and percentages. Patients’ demographic characteristics were analyzed using Pearson’s chi-squared test for categorical variables and the Wilcoxon rank-sum test for continuous variables. To determine the association between bronchoscopy findings and the presence of BPD, a univariate logistic regression was performed. This analysis provided the odds ratios (ORs) for each bronchoscopy finding, serving as a measure of the strength of association with BPD.
The significance level was set at P < 0.05 (two-sided). All analyses were performed using R statistical software version 4.1.1.
Results
Study population
The study included 50 pediatric patients (mean age of 1.26 years, 58% males) with BPD and a reference group of 150 non‐BPD pediatric patients (mean age of 1.25 years, 57% males). Table 1 summarizes the demographic data and characteristics of the BPD and reference groups. Naturally, the BPD group had a significantly lower gestational age and birth weight compared to the non-BPD group. The median length of hospital stay after birth was significantly longer for the BPD group (112 vs. 3 days, P < 0.001), and a higher proportion required prolonged durations of oxygen support, non-invasive ventilation, and invasive ventilation compared to the reference group. At the time of bronchoscopy, the mean weight of the BPD patients was lower than that of the reference group (mean of 7.5 kg vs. 8.9 kg, P = 0.037).
A total of 49 (98%) BPD patients compared to 13 (6.5%) non-BPD patients had additional comorbidities, with respiratory distress syndrome (RDS) being the most common (86%). Severe BPD may be associated with pulmonary hypertension and higher morbidity [26, 27]. In our study, information on transthoracic echocardiography (TTE) was available on 44 BPD patients. One had moderate pulmonary hypertension and was treated with Sildenafil, six had mild tricuspid regurgitation which did not necessitate medical treatment, and the rest had no suspected pulmonary hypertension on their TTE. None of the BPD patients underwent cardiac catheterization for definitive confirmation. Examining the medical treatments of the study population around the time of birth, not surprisingly, BPD patients were treated with significantly higher rates of systemic steroids, caffeine, intravenous antibiotics, insulin, diuretics, and other medical treatments. Chronic medical treatments, specifically anti-asthmatic treatments, were significantly higher in the BPD group compared to the non-BPD group (Table 1S).
Bronchoscopy indications and findings
Ten patients (20%) in the BPD group and 69 (46%) in the reference group were hospitalized before the FB.
During the FB procedures, propofol (2.5–3.5 mg/kg for induction of anesthesia with titration to the desired response) was the anesthetic most frequently utilized, administered to 98% of the BPD group and 97% of the non-BPD group. The administration of other anesthetics such as ketamine and midazolam was sporadic, with no significant differences in their use between the two groups. Local lidocaine (Lidocaine 1%, 0.5 ml through the working channel in 3 doses: vocal cords, mid-trachea, and carina) was applied in 44% of patients in both groups, without a significant difference.
Table 2 presents the indications for FB within the study groups. Common indications among the BPD group included obstructive sleep apnea-related symptoms, oxygen dependence, and recurrent wheezing. Suspected foreign body aspiration as an indication for FB was the most common indication for FB in the reference group (36% vs. 0%, P < 0.001).
Table 3, which summarizes the findings from the FB procedures, shows that patients with BPD had significantly higher rates of turbinate hypertrophy (18% vs. 6%, P = 0.014), adenoid hypertrophy (46% vs. 24%, P = 0.004), lingual tonsils (10% vs. 2%, P = 0.024), subglottic stenosis (16% vs. 2.7%, P = 0.002), and tracheomalacia (16% vs. 6%, P = 0.034). Furthermore, patients with BPD had significantly lower rates of normal bronchoscopy results (12% vs. 30%, P = 0.015). Figure 1 illustrates some of the bronchoscopy findings among the BPD patients.
Table 4 reports the complications associated with FB. Among the 50 BPD patients, 11 (22%) experienced at least one complication, whereas in the non-BPD group, 25 (17%) patients experienced a complication (P = 0.4). Desaturation was the most frequent complication in BPD patients compared to non-BPD patients (16% vs. 4.7%, P = 0.013). Five BPD patients (10%) required intubation, while no patients in the non-BPD group did. The hospitalization rate following FB was three times higher for BPD patients (14% vs. 5.3%, P = 0.052), including admissions to the NICU/PICU (10% vs. 0.7%, P = 0.011).
Discussion
In the current study, we evaluated the indications, findings, and complications associated with FB in formerly preterm infants diagnosed with BPD, compared to a matched reference group in a 1 to 3 ratio. Our study illuminates the significantly higher prevalence of upper airway obstruction and structural anomalies in premature infants with BPD. The anatomical abnormalities identified, such as turbinate hypertrophy, adenoid hypertrophy, lingual tonsils, subglottic stenosis, and tracheomalacia, highlight the complex relationship between prematurity and BPD in airway development. Furthermore, our findings reveal a substantial burden on the healthcare system, evidenced by high rates of hospitalizations, particularly following bronchoscopy. This emphasizes the critical need for specialized care and meticulous consideration before and during invasive procedures in this vulnerable population.
The study found several differences between the BPD and non-BPD groups. Patients with BPD had lower gestational age and birth weight, indicating their premature and underdeveloped lung status, which is consistent with the known association between BPD and preterm birth. Moreover, the BPD group experienced longer hospital stays post-birth and required prolonged durations of respiratory support, including oxygen therapy, non-invasive ventilation, and invasive ventilation. These findings further emphasize the significant respiratory challenges experienced by patients with BPD and the severity of their condition.
The administration of medical treatments around the time of birth was notably different between the two groups. BPD patients were treated with various medications, such as systemic steroids, caffeine, antibiotics, and other medical treatments. This disparity likely reflects the complex and multi-disciplinary medical management required for premature infants, aimed at supporting their compromised respiratory function and addressing associated comorbidities.
Regarding, bronchoscopy indications, the BPD group exhibited a higher incidence of obstructive sleep apnea-related symptoms [28], oxygen dependency, and recurrent wheezing. This difference may be attributed to the unique anatomical and physiological characteristics of the BPD group which predisposes them to upper airway obstruction [29] and recurrent respiratory symptoms. In contrast, suspected foreign body aspiration, one of the primary indications for FB in the broader pediatric population, was frequently observed as an indication for FB in the non-BPD group. More non-BPD patients were hospitalized before the FB than BPD patients, likely because most FB procedures among the BPD group were performed ambulatory, whereas the higher hospitalization rate among the non-BPD group was likely due to our center’s protocol for suspected foreign body aspiration, which typically necessitates hospitalization for observation and further evaluation before performing FB.
Bronchoscopy findings provide valuable insights into the structural abnormalities associated with BPD. Patients with BPD have higher rates of turbinate hypertrophy, adenoid hypertrophy, lingual tonsils, subglottic stenosis, and tracheomalacia [30,31,32,33] compared to the non-BPD group. These findings indicate the presence of upper airway narrowing, adenotonsillar hypertrophy [34], and tracheobronchial anomalies, all contributing to the respiratory morbidity observed in BPD patients. Notably, a normal bronchoscopy examination was rare among BPD patients, further emphasizing the influence of their underlying condition on airway structure and function.
In addition to the heightened prevalence of structural anomalies leading to upper airway obstruction observed in our study, it is essential to contextualize our findings within the broader landscape of pediatric respiratory health. Existing literature has indicated a multifaceted relationship between prematurity and susceptibility to OSA later in life [35]. This increased risk of OSA in premature infants may contribute to a subsequent rise in adenoidectomy procedures as part of the management strategy for upper airway obstruction [36]. Therefore, our study’s discovery of higher rates of adenoid and choanal hypertrophy in BPD patients aligns with a broader narrative in the literature, emphasizing the intricate relationship between prematurity, upper airway abnormalities, and the likelihood of respiratory complications throughout childhood and beyond [34, 37]. Further research is warranted to explore these interconnected factors comprehensively, shedding light on long-term respiratory implications and guiding optimal clinical management strategies for this vulnerable population.
Regarding complications during the FB, desaturation occurred more frequently in BPD patients, highlighting their decreased lung reserve and vulnerability to respiratory compromise during the procedure. Furthermore, a larger proportion of BPD patients required intubation, hospitalization, and admission to the intensive care unit, emphasizing the risks associated with FB evaluation in this population. Beyond these clinical aspects, our findings also reveal a substantial burden on healthcare resources, notably marked by a high rate of hospitalizations following bronchoscopy. These findings highlight the critical need for specialized care and meticulous consideration during invasive procedures in this vulnerable population. Both physicians and parents should be aware of the relatively higher rate of complications, and carefully consider the risk–benefit ratio of the procedure. Practical measures may include conducting FB in BPD patients within an intensive care unit setting. Since we found no difference in the anesthetic drugs administered during the procedure between the groups, we propose that any observed differences in outcomes were not related to the anesthetic medications.
Overall, our study illuminates the distinct characteristics and outcomes of bronchoscopy in pediatric patients with BPD. The findings highlight the need to consider upper airway obstruction and tracheobronchial anomalies in the evaluation and management of BPD patients. Clinicians should be cognizant of the heightened prevalence of these structural abnormalities in BPD patients, which may influence treatment decisions and interventions aimed at optimizing their respiratory health. Most of these anatomical obstructions can be treated with surgical measures (adenoidectomy/adenotonsillectomy) or with positive pressure ventilation such as continuous positive airway pressure (CPAP) ventilation for tracheomalacia.
To the best of our knowledge, this is the first study on bronchoscopic findings in BPD patients with a large comparison group, originating from a single tertiary center. All bronchoscopies were performed under the same conditions, with consistent anesthetics and personnel. However, our study has several limitations. First, the small sample size of 50 patients with BPD who underwent FB is noteworthy. Despite this, most of the results were statistically significant, substantiating the results and potentially highlighting underdiagnoses. Second, given the increased prevalence of other comorbidities within the BPD group, it is plausible that some of the observed differences between the groups could be attributed to factors beyond BPD. These factors include variations in birth weight, the inherent prematurity of the patients, and mechanical ventilation status, all of which differ within this specific patient population. The use of other methods, such as lung ultrasound, was not assessed in this study, although recent meta-analyses demonstrated good accuracy for early prediction of BPD [38]. Furthermore, bronchoalveolar lavage was not performed routinely during the bronchoscopies. Further and large-scale studies are needed to explore these associations in more detail and guide clinical practice in this high-risk population.
Conclusion
Our findings provide valuable insights into the bronchoscopy characteristics and outcomes in pediatric patients with BPD. The results suggest that BPD is associated with specific bronchoscopy findings, mainly upper airway obstruction and tracheobronchial anomalies. Moreover, FB in BPD patients carries a higher complication rate in this unique population. Such findings highlight the importance of considering these factors in the assessment and management of patients with BPD. This insight is crucial for optimizing diagnostic and therapeutic approaches, ultimately improving the respiratory outcomes of infants with BPD.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- BPD:
-
Bronchopulmonary dysplasia
- ENT:
-
Ears, nose, and throat
- GA:
-
Gestational age
- FB:
-
Flexible bronchoscopy
- OR:
-
Odds ratio
- OSA:
-
Obstructive sleep apnea
- IRR:
-
Incidence rate ratio
- PICU:
-
Pediatric intensive care unit
- NICU:
-
Neonatal intensive care unit
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- ASD:
-
Atrial septal defect
- VSD:
-
Ventricular septal defect
- PDA:
-
Patent ductus arteriosus
References
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM (1998) Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics 82(4):527–532
Higgins RD, Jobe AH, Koso-Thomas M, Bancalari E, Viscardi RM, Hartert TV, Ryan RM, Kallapur SG, Steinhorn RH, Konduri GG, Davis SD, Thebaud B, Clyman RI, Collaco JM, Martin CR, Woods JC, Finer NN, Raju TNK (2018) Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr 197:300–308
Jobe AH, Bancalari E (2001) Bronchopulmonary dysplasia. Am J Respir Crit Care Med 163:1723–1729
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, Kirpalani H, Laughon MM, Poindexter BB, Duncan AF, Yoder BA, Eichenwald EC, DeMauro SB (2019) The diagnosis of bronchopulmonary dysplasia in very preterm infants. An evidence-based approach. Am J Respir Crit Care Med 200(6):751–759
McEvoy CT, Jain L, Schmidt B, Abman S, Bancalari E, Aschner JL (2014) Bronchopulmonary dysplasia: NHLBI workshop on the primary prevention of chronic lung diseases. Ann Am Thoracic Soc 11(Suppl 3):S146-153
Stoll BJ, Hansen NI, Bell EF et al (2010) Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126(3):443–456
Kalikkot Thekkeveedu R, Guaman MC, Shivanna B (2017) Bronchopulmonary dysplasia: a review of pathogenesis and pathophysiology. Respir Med 132:170–177
Jobe AH (2015) Animal models, learning lessons to prevent and treat neonatal chronic lung disease. Front Med 2:49
Coalson JJ (2003) Pathology of new bronchopulmonary dysplasia. Sem Neonatol: SN 8(1):73–81
Duijts L, van Meel ER, Moschino L, Baraldi E, Barnhoorn M, Bramer WM et al (2019) European Respiratory Society guideline on long term management of children with bronchopulmonary dysplasia. Eur Respir J 55:1900788
Gough A, Linden M, Spence D, Patterson CC, Halliday HL, McGarvey LPA (2014) Impaired lung function and health status in adult survivors of bronchopulmonary dysplasia. Eur Respir J 43:808–816
Álvarez-Fuente M, Arruza L, Muro M, Zozaya C, Avila A, López-Ortego P et al (2017) The economic impact of prematurity and bronchopulmonary dysplasia. Eur J Pediatr 176:1587–1593
Altit G, Dancea A, Renaud C, Perreault T, Lands LC, Sant’Anna G (2017) Pathophysiology, screening and diagnosis of pulmonary hypertension in infants with bronchopulmonary dysplasia - a review of the literature. Paediatr Respir Rev 23:16–26
Tracy MC, Cornfield DN (2017) The evolution of disease: chronic lung disease of infancy and pulmonary hypertension. Curr Opin Pediatr 29(3):320–325
Tracy MK, Berkelhamer SK (2019) Bronchopulmonary dysplasia and pulmonary outcomes of prematurity. Pediatr Ann 48:148–153
Cheong JLY, Doyle LW (2018) An update on pulmonary and neurodevelopmental outcomes of bronchopulmonary dysplasia. Semin Perinatol 42:478–484
Day CL, Ryan RM (2017) Bronchopulmonary dysplasia: new becomes old again! Pediatr Res 81:210–213
Voynow JA (2017) “New” bronchopulmonary dysplasia and chronic lung disease. Paediatr Respir Rev 24:17–18
Zurita-Cruz J, Gutierrez-Gonzalez A, Manuel-Apolinar L et al (2020) The impact of a history of pre-maturity on viral respiratory infections in children under 2 years of age: a propensity score-matching analysis of in-hospital complications and mortality. Front Pediatr 8:499013
Galderisi A, Calabrese F, Fortarezza F, Abman S, Baraldi E (2019) Airway histopathology of adolescent survivors of bronchopulmonary dysplasia. J Pediatr 211:215–218. https://doi.org/10.1016/j.jpeds.2019.04.006
Bårdsen T, Røksund OD, Benestad MR, Hufthammer KO, Clemm HH, Mikalsen IB, Øymar K, Markestad T, Halvorsen T, Vollsæter M (2022) Tracking of lung function from 10 to 35 years after being born extremely preterm or with extremely low birth weight. Thorax, thoraxjnl-2021–218400. https://doi.org/10.1136/thoraxjnl-2021-218400
Doyle LW, Ranganathan S, Cheong J, Victorian Infant Collaborative Study Group (2022) Bronchopulmonary dysplasia and expiratory airflow at 8 years in children born extremely preterm in the post-surfactant era. Thorax, thoraxjnl-2022–218792. https://doi.org/10.1136/thoraxjnl-2022-218792
Miller RW, Woo P, Kellman RK, Slagle TS (1987) Tracheobronchial abnormalities in infants with bronchopulmonary dysplasia. J Pediatr 111(5):779–782. https://doi.org/10.1016/s0022-3476(87)80267-6
Hysinger E, Friedman N, Jensen E et al (2019) Bronchoscopy in neonates with severe bronchopulmonary dysplasia in the NICU. J Perinatol 39:263–268
Ferraro VA, Baraldi E, Stabinger D, Zamunaro A, Zanconato S, Carraro S (2021) Pediatric flexible bronchoscopy: a single-center report. Pediatr Pulmonol 56:2634–2641
Hansmann G, Sallmon H, Roehr CC, Kourembanas S, Austin ED, Koestenberger M, European Pediatric Pulmonary Vascular Disease Network (EPPVDN) (2021) Pulmonary hypertension in bronchopulmonary dysplasia. Pediatr Res 89(3):446–455
Hilgendorff A, Apitz C, Bonnet D, Hansmann G (2016) Pulmonary hypertension associated with acute or chronic lung diseases in the preterm and term neonate and infant. The European Paediatric Pulmonary Vascular Disease Network, endorsed by ISHLT and DGPK. Heart 102 Suppl 2:ii49-56
Tsou PY, Hayden LP (2023) Obstructive sleep apnea is associated with use of assisted ventilation among children with bronchopulmonary dysplasia hospitalized with respiratory illness: a nationwide inpatient cohort. Sleep Med 109:181–189
Ortiz LE, McGrath-Morrow SA, Sterni LM, Collaco JM (2017) Sleep disordered breathing in bronchopulmonary dysplasia. Pediatr Pulmonol 52(12):1583–1591
Cohn RC, Kercsmar C, Dearborn D (1988) Safety and efficacy of flexible endoscopy in children with bronchopulmonary dysplasia. Am J Dis Child 142(11):1225–1228
Duncan S, Eid N (1991) Tracheomalacia and bronchopulmonary dysplasia. Ann Otol Rhinol Laryngol 100(10):856–858
Amin RS, Rutter MJ (2015) Airway disease and management in bronchopulmonary dysplasia. Clin Perinatol 42(4):857–870
Bush D, Juliano C, Bowler S, Tiozzo C (2023) Development and disorders of the airway in bronchopulmonary dysplasia. Children (Basel) 10(7):1127
Sharma PB, Baroody F, Gozal D, Lester LA (2011) Obstructive sleep apnea in the formerly preterm infant: an overlooked diagnosis. Front Neurol 29(2):73. https://doi.org/10.3389/fneur.2011.00073
Tapia IE, Shults J, Doyle LW, Nixon GM, Cielo CM, Traylor J, Marcus CL, Caffeine for Apnea of Prematurity – Sleep Study Group (2016) Perinatal risk factors associated with the obstructive sleep apnea syndrome in school-aged children born preterm. Sleep 39(4):737–42
Leonardis RL, Robison JG, Otteson TD (2013) Evaluating the management of obstructive sleep apnea in neonates and infants. JAMA Otolaryngol Head Neck Surg 139(2):139–146
Zalzal HG, Newman D, Behzadpour H, Nino G, Lawlor CM (2023) Phenotypical characterization of obstructive sleep apnea in premature infants using polysomnography. Laryngoscope. https://doi.org/10.1002/lary.30991
Pezza L, Alonso-Ojembarrena A, Elsayed Y, Yousef N, Vedovelli L, Raimondi F, De Luca D (2022) Meta-analysis of lung ultrasound scores for early prediction of bronchopulmonary dysplasia. Ann Am Thorac Soc 19(4):659–667
Acknowledgements
We express our gratitude to Dr. Soliman Alkrinawi for his dedicated, compassionate, and professional care of patients over the years, and for being an integral part of the pediatric pulmonary unit at the Soroka University Medical Center during this time.
Author information
Authors and Affiliations
Contributions
IGT, MA and AG contributed to the study's conception and design. Material preparation and data collection were performed by NS, NA, DY and ST. Statistical analysis was performed by IH and GH. The first draft of the manuscript was written by NS and IGT and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study received the approval of the institutional Review Board (in accordance with the Declaration of Helsinki) at Soroka University Medical Center (No. 532–20 SOR). The need for informed consent was waived as data was retrospectively collected and participants’ identity was kept anonymous.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shemesh Gilboa, N., Aviram, M., Goldbart, A. et al. Flexible bronchoscopy in preterm infants with bronchopulmonary dysplasia: findings and complications in a matched control study. Eur J Pediatr (2024). https://doi.org/10.1007/s00431-024-05750-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00431-024-05750-w