Abstract
Cardiovascular diseases are the main causes of morbidity in children with chronic kidney disease (CKD). Electrocardiography (ECG) can provide important information about cardiac functions and parameters associated with sudden cardiac death. This study aims to evaluate the potentially dangerous changes in CKD and kidney replacement therapies by ECG and to determine the value of ECG in predicting cardiovascular outcome compared with echocardiography. 101 patients with CKD were divided into subgroups according to treatment modalities as pre-dialysis CKD, hemodialysis (HD), peritoneal dialysis (PD) and kidney transplantation (KTx). Differences in anthropometric measurements, laboratory results, blood pressures, ECG monitoring were compared within groups as well as with 40 healthy controls. Available echocardiographic findings were noted. In the patients, HD group had highest frequency of hypertension. ECG revealed prolonged QTc as more frequent (16.8% vs 0%, p = 0.006) and higher QTcD (56.7 ± 6.5 vs 39.9 ± 5.1 ms, p = 0.001) in the patients compared to controls, especially in dialysis patients, whereas lowest values were in KTx subgroup. Left ventricular (LV) hypertrophy (LVH) was more frequent (47.1%) in HD compared to other CKD subgroups in ECG (p = 0.052). Echocardiography also showed LV mass index as highest in HD and lowest in KTx (121.4 ± 55.7 vs 63.7 ± 18.3 g/m2, p = 0.000), with numerically highest LVH in HD (58.3%, p = 0.063).
Conclusion: ECG can be used to detect cardiovascular problems in patients with CKD, especially in HD. As ECG results were in line with echocardiography, patients with ECG abnormalities suggestive of LVH should be referred for echocardiographic assessment.
What is Known: • Cardiovascular diseases such as coronary artery disease, congestive heart failure, arrhythmias and sudden cardiac death are major causes of morbidity and mortality in chronic kidney disease. • Electrocardiography has significant advantages in demonstrating cardiac functions in children because it is readily available, non-invasive and often non-experts can interpret the results. | |
What is New: • The heart rate is higher, QTc is longer and QTcD is higher in dialysis patients and the prolonged QTc is more frequent in patients with underlying glomerular diseases. • Left ventricular hypertrophy is more common in HD patients and those with hypertension, hypercalcemia, anemia or glomerular etiology. The cardiovascular risky conditions are less frequent in the patients with kidney transplantation. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic kidney disease (CKD) refers to a condition of irreversible kidney damage and decreased kidney function associated with a progressive loss of kidney function over time [1]. The prevalence of CKD in children is 32.2 per million age-related population in Europe [2]. However, it is probably underestimated because the early stages of CKD are often asymptomatic and lead to an underdiagnosis [3].
Follow-up for CKD includes preventing or slowing the progression of kidney disease, preventing or treating complications (such as mineral and bone disease, anemia, growth failure and cardiovascular diseases), and preparing for kidney replacement therapy (KRT) [4]. In children with kidney failure, KRT options include peritoneal dialysis (PD), hemodialysis (HD) and kidney transplantation (KTx) [5].
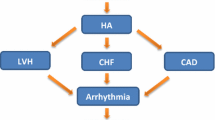
Cardiovascular diseases such as coronary artery disease, congestive heart failure, arrhythmias and sudden cardiac death are major causes of morbidity and mortality in CKD. Cardiovascular disease risk markedly increases parallel to the increase in the CKD stage, especially in patients with CKD stage 3 and beyond [6]. Cardiovascular risk is 20 times greater than general population and mortality in patients on dialysis is up to 10 times that of healthy controls [7, 8].
Electrocardiography (ECG) has significant advantages in demonstrating cardiac functions [9]. Arrhythmias including atrioventricular block, atrial or ventricular tachyarrhythmias; left/right bundle branch block and axis deviations, ST-segment deviation, T-wave inversion, pathologic Q-waves and right/left atrial enlargement can be determined with ECG [10]. Besides, ECG can provide important information about prolonged corrected QT (QTc) interval and increased QTc dispersion (QTcD) and left ventricular hypertrophy (LVH); the parameters which are known to be associated with sudden cardiac death [7, 11]. However, the efficacy or prognostic value of these ECG markers in children with CKD on determining cardiac abnormalities is of debate. Therefore, the aim of this study is to evaluate the presence and nature of potentially dangerous changes of cardiac conduction and repolarization via the 12-leads surface ECG and determine its value in predicting cardiovascular outcome when compared with echocardiographic findings during the course of CKD and in different forms of KRTs.
Material and methods
Design and selection of study subjects
This is a retrospective cohort study conducted on children with CKD with regular follow-up in a tertiary pediatric nephrology clinic in a single university hospital. All included subjects were aged 6 to 18 years.
Twelve-leads surface ECG monitoring was performed in 101 children with CKD who were clinically stable, and the patients were divided into four groups according to the mode of treatment: conservative therapy (i.e., pre-dialysis CKD), maintenance HD and continuous ambulatory PD (CAPD) and those with a successful KTx. Patients were also subdivided into five groups according to the primary etiology: congenital anomalies of the kidney and urinary tract (CAKUT), glomerular diseases, kidney stones, CKD secondary to systemic diseases and unknown causes. Use of angiotensin converting enzyme inhibitors (ACEi) and/or angiotensin receptor blockers (ARBs) were questioned in all participants. The control group consisted of 40 healthy age- and sex-matched children without cardiac disease. Exclusion criteria included the presence of amyloidosis, congenital heart disease and previous cardiac surgery, diabetes mellitus, thyroid gland dysfunction, atrial fibrillation, bundle branch block, and administration of antiarrhythmic drugs that might affect the QT interval.
Patients in the HD group underwent pre-HD session ECG monitoring on a day of dialysis. They were dialyzed routinely three times per week for an average of four hours. Patients on CAPD generally had four to five exchanges a day with a filling volume of 1200–1400 ml/m2 per exchange with 1.36 dialysate. The KTx group consisted of patients who have undergone living-related or cadaveric transplants and continued their follow-up and treatment at the same center regularly.
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the Medical Ethics Committee.
Data collection and assessment of laboratory parameters
Anthropometric measurements, including body weight, height, and blood pressure (BP) values, and laboratory results (hemoglobin (Hb), serum biochemistry including serum creatinine, sodium (Na), potassium (K), adjusted total calcium (Ca), phosphorus (P), magnesium (Mg), and blood gas analysis including pH and bicarbonate (HCO3) of the patients measured on the day of the ECG were recorded from the patient files.
Height-age and weight-age z scores were calculated by using data from Neyzi et al. [12, 13]. Children were categorized as severely underweight, moderately underweight, mildly underweight and overweight according to weight z scores and severely stunted, moderately stunted and mildly stunted according to height z scores [14]. Body mass index (BMI) was calculated using the weight/height2 (kg/m2) formula and BMI-age z score was determined by using growth charts [15, 16]. According to BMI-age z scores, children were categorized as underweight, risk of overweight, overweight, and obese [17].
BP was measured using a manual auscultatory device. BP measurements were made from the right arm using an appropriate cuff size after 3–5 min of rest. We assured that all the measurements were performed by the same fellow pediatric nephrologist in each control of the patients. The diagnosis and classification of hypertension was based on ‘Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents, 2017’ [18].
Anemia was diagnosed with an Hb value below 2.5th percentile according to age and sex [19]. The estimated glomerular filtration rate (eGFR) was calculated using the modified Schwartz formula (20). The eGFR of 90–120 ml/min/1.73 m2 was defined as normal [21].
ECG analysis
Twelve-lead ECG were recorded with a three-channel electrocardiographic recorder (Hewlett Pac- 3. Results kard, model 4745 A; Hewlett Packard, Camas, WA, USA) at a paper speed of 25 mm/s. The tracings were coded and analyzed by one of the authors who was blinded to the clinical data of the patients. All data obtained were confirmed by the pediatric cardiologist. The heart rate is calculated by dividing the number of large boxes between two consecutive R waves by 300. A normal resting heart rate is 60 to 100 beats per minute (bpm) for ≥ 10 years old, 60 to 140 bpm for 6–10 years old [22]. The PR interval, indicating atrial depolarization, is measured from the beginning of the upslope of the P wave to the beginning of the QRS wave. This measurement should be 0.12–0.20 s. The width of the QRS from the beginning of the Q wave to the end of the S wave represents ventricular depolarization and its duration should be less than 0.12 s. The QT interval is the time from the beginning of the QRS complex to the end of the T wave, resulting from ventricular repolarization. The normal QT interval is between 400 to 440 ms (ms) [23]. The QT was corrected for heart rate using Bazzett’s formula [24]. The QTc interval was considered normal if it was < 440 ms [25]. The QTcD was obtained by subtracting the minimum QTc from the maximum QTc. The normal range of QTcD has been determined as 10–70 ms [26, 27]. LVH was determined using Cornell voltage criteria, the method considered to be the most accurate (the specificity of 90% with a sensitivity of 20% to 40%) on ECG. The sex-specific Cornell voltage criteria was computed as the amplitude of R in aVL plus the amplitude of S or QS complex in V3 (RaVL + SV3) with a cutoff of > 2.8 mV in males and > 2.0 mV in females [28]. If an echocardiography evaluation was performed simultaneously with the ECG evaluation in the patient group, measurements of left ventricular end-diastolic diameter (LVEDD), posterior wall thickness (PWT) and diastolic interventricular septal thickness (IVST) were noted. Left ventricular mass (LVM) was calculated according to the formula by Devereux: LVM (g) = 0.8 {1.04 [(LVEDD + PWT + IVST)3—(LVEDD)3] + 0.6} [29]. The LVM index (LVMI) (g/m2) is calculated as the LVM divided by the body surface area (m2) [(4 × Weight (kg) + 7) / (90 + Weight (kg))] [30]. LVH was defined as LVMI exceeding the 95th percentile for sex and age [31].
Statistical analysis
In the presentation of descriptive statistics; the data obtained by measurement were expressed as mean ± standard deviation (SD) and categorical data as number (percentage). Cross-table analyzes and Fisher's exact Chi-square tests were used to compare the qualitative characteristics of the groups. Shapiro Wilks test was used to determine the normal distribution of numerical measurements in groups. Two groups were compared with t-test in independent groups and Mann–Whitney U test for those who did not show normal distribution. IBM SPSS Statistics version 22 package program was used for all statistical analyzes. Significance level of p < 0.05 was taken.
Results
Demographic and anthropometric characteristics of the study population
The study included 101 patients with pre-dialysis CKD (n = 39) and those undergoing KRT [PD (n = 21), HD (n = 17) and KTx (n = 24)] and 40 healthy controls. Majority of the participants were boys (62.4%, n = 63) in the patient group. The sex distribution and mean age was similar in the patient and the control groups (p = 0.794 and p = 0.798, respectively). In the subgroup analysis, although not statistically significant, KTx patients were older than the other patients, while the PD group was the youngest (p = 0.068).
Mean dialysis duration was longest in PD and shortest in KTx patients prior to transplantation [2 (8.3%) patients had preemptive transplant, 15 (62.5%) HD, 7 (29.1%) PD] without statistical significance (p = 0.377). The post-transplant period was 39 ± 24.1 months in KTx patients.
Majority of the patients (61.4%) had CAKUT as the primary CKD etiology followed by glomerular pathologies (19.8%). Most common primary diagnosis was glomerular diseases in HD patients, and CAKUT in PD and pre-dialysis CKD patients. In addition, in KTx patients, the frequency of CAKUT was approximately 3 times higher than glomerular disease (p = 0.000).
Mean weight and height z scores were significantly lower in the patients compared to the controls (p = 0.001 and p = 0.000, respectively). In the subgroup analysis of the patients, weight, height, and BMI z scores were significantly lower in dialysis patients, with the lowest in HD group, and the highest in KTx group (p = 0.000, p = 0.000, and p = 0.025, respectively).
The frequency of severe and moderate underweightness were higher in the patient group (n = 32, 31.6%) than in the healthy controls (n = 3, 7.5%) (p = 0.000). Besides, although none of the patient group had obesity, 5% of the controls consisted of obese subjects. More than half of the patients were stunted, whereas short stature was also observed in a quarter of the controls (p = 0.003). In sub-group analysis, underweightness and short stature were more prominent in HD and PD patients, and at the lowest rate in KTx (p = 0.000 and p = 0.001, respectively).
Demographic and anthropometric characteristics of the study population are shown in Table 1.
Evaluation of blood pressure in the study population
When compared in terms of office BP measurements, mean SBP z score was significantly higher in the patient group than in healthy controls (p = 0.000). In the sub-group analysis, the mean SBP z score was highest in the HD group, and lowest in the PD group (p = 0.000). Although there was no significant difference in terms of DBP z scores in our study, mean DBP z score was numerically higher in the patient group than in healthy controls (p = 0.093). In addition, mean DBP z score was at the highest value in the HD group (p = 0.071, Table 1).
The patients had a lower frequency of having normal BP than healthy controls (66.3% vs 87.5%, p = 0.042). In the subgroup analysis, elevated BP or hypertension was observed in approximately half of the patients with HD, whereas it was present in only around one fourth of the patients with PD and KTx (p = 0.000) (Table 1).
The ACEi and/or ARBs were used in 27.7% of patients. The frequency of using at least one of these drugs was highest in the HD group and lowest in the KTx group (p = 0.000) (Table 1).
Laboratory data of the study group
The mean Hb value was significantly lower and frequency of anemia was approximately 4 times higher in the patients compared to the control subjects (p = 0.000 and p = 0.005, respectively). In sub-group analysis, the lowest mean Hb value was in dialysis patients, especially in those with HD (p = 0.002). Besides, anemia frequency was highest in dialysis patients (p = 0.005). Mean serum creatinine was higher and eGFR was lower in the patients compared with healthy controls, as expected (p = 0.000, for both). Mean serum potassium and phosphorus values were higher and calcium values were also lower in the patients (p = 0.032, p = 0.022, and p = 0.000, respectively). In sub-group analysis, mean serum creatinine, potassium, and phosphorus were higher and mean serum calcium level was lower in dialysis patients (p = 0.000, for all parameters). In addition, mean serum magnesium level was lower in KTx patients compared to other groups (p = 0.001).
There were no significant differences between the patients and healthy controls in terms of hyponatremia or hypernatremia (p = 0.658). However, the frequency of hyperkalemia and hypocalcemia was higher in PD, HD and pre-dialysis CKD patients (p = 0.013 and p = 0.000, respectively); and hyperphosphatemia was higher in HD, PD and pre-dialysis CKD patients in descending order (p = 0.000). All the controls had normal magnesium levels, but approximately one third of the patient group had magnesium levels outside the normal reference ranges. Frequency of hypomagnesemia was highest in the KTx group whereas hypermagnesemia frequency was highest in the PD group (p = 0.000). Metabolic acidosis was present in 18.8% of the patients, with a significantly higher ratio in dialysis patients than the other CKD subgroups (p = 0.000).
Laboratory data of the study population are shown in Table 2.
ECG analysis of the study population
Mean heart rate was higher in the patients compared to the controls (p = 0.004). Mean PR interval was shorter in the patients (p = 0.001). Mean QTc was longer, and QTcD was higher significantly in the patient group (p = 0.000 and p = 0.001, respectively). A total of 17 patients (16.8%) had prolonged OTc compared to none in the healthy control group (p = 0.006). LVH was also seen more frequently in the patients than the controls (21.8% vs 15%) but without statistically significant difference (p = 0.363).
In sub-group analysis, mean heart rate was highest in dialysis patients and lowest in KTx patients (p = 0.014). Mean QTc was longer, and QTcD was significantly higher in dialysis patients while lowest values were detected in KTx patients in terms of these two parameters (p = 0.005 and p = 0.004, respectively). The prolonged OTc frequency was significantly greater in the dialysis subgroup (especially the PD patients, p = 0.004). Although LVH was detected in almost half of HD patients (47.1%), the difference in terms of LVH frequency between CKD subgroups was only in the range of borderline statistical significance (p = 0.052). The ECG findings in the study cohort are shown in Table 3.
Prolonged QTc was observed more frequently in patients followed up for glomerular diseases when compared with those with a primary diagnosis of CAKUT (35% vs 16.1%, p = 0.002). Furthermore, the frequency of the prolonged QTc was higher in patients with hyperkalemia, hypermagnesemia or hyperphosphatemia (p = 0.028, p = 0.000 and p = 0.001, respectively). In addition, this rate was three times higher in patients with metabolic acidosis than in patients without acidosis (36.8% vs 12.2%, p = 0.000). Although not statistically significant, the frequency of prolonged QTc was numerically higher in anemic patients compared to non-anemic ones (21.4% vs 14.2%, p = 0.144).
According to ECG analysis, the frequency of LVH was significantly higher in patients with glomerular disease than in patients with CAKUT (28.6% vs 8.1%, p = 0.000). Approximately half of the patients with stage 2 hypertension had LVH, whereas 19.6% of normotensive patients had LVH (p = 0.066). In addition, LVH was more common in patients with hypercalcemia than in the ones without hypercalcemia (35.7% vs 7.1%, p = 0.009) and in patients with anemia than those without anemia (47.9% vs 9.8%, p = 0.006).
When 66 patients with an available echocardiographic evaluation were investigated, mean LVMI was 76.6 ± 37.9 g/m2. It was highest in HD and lowest in KTx patients (121.4 ± 55.7 vs 63.7 ± 18.3 g/m2, p = 0.000). LVH was detected in 21 (31.8%) patients in general analysis. It was again numerically highest in HD patients (58.3%) (p = 0.063). The prevalence of LVH was 55.6% in glomerular disease and 20.9% in CAKUT (p = 0.048). In stage 2 HT, LVH was found in 61.5% of patients compared to 30% of normotensive patients (p = 0.029).
Cardiac evaluations of the study population are shown in Table 3.
Discussion
In this retrospective study, in addition to impaired growth indices including lower weight and height z scores, findings compatible with CKD such as anemia, hypertension (especially with increased SBP z scores) and abnormalities in electrolytes including potassium, calcium and phosphorus were significant in the patient group despite presence of KRT modalities in the majority. Besides, ECG revealed higher mean heart rate, shorter PR interval, prolonged QTc and higher QTcD values in the patients compared to the controls. Glomerular diseases were more common in the HD group and CAKUT was the leading etiology in the other patients with CKD. Sub-group analysis showed the best growth parameters in KTx patients and worst in the HD group. Despite the considerably higher antihypertensive use, HD group had highest SBP z scores and frequency of hypertension. Hyperkalemia, hyperphosphatemia and hypocalcemia were more frequent in dialysis patients. The heart rate was higher, QTc was longer and QTcD was higher in dialysis patients. Prolonged QTc was more frequent in patients with underlying glomerular diseases. In addition, QTc was found to be longer in the states of electrolyte imbalance (hyperkalemia, hyperphosphatemia, hypermagnesemia) and metabolic acidosis. LVH was more common in HD patients and those with hypertension, hypercalcemia, anemia or glomerular etiology.
Children with CKD have a quite high prevalence of traditional (hypertension, dyslipidemia, obesity, etc.) and uremia-related risk factors for cardiovascular disease [32]. From these, hypertension carries great importance as it affects more than 50% of pediatric CKD patients. Various factors including decreased nephron mass, increased sodium retention and extracellular volume expansion, sympathetic nervous system overactivity, activation of renin–angiotensin–aldosterone system and endothelial dysfunction can play role in hypertension pathogenesis [33]. Prolonged and uncontrolled hypertension is associated with the progression of CKD and the development of end-organ damage, including early cardiomyopathy and atherosclerosis [34]. In a recent study on adult patients with CKD, SBP was measured as significantly higher in dialysis patients than in pre-dialysis CKD [35]. In another study conducted on patients on chronic dialysis, CAKUT and glomerular diseases were compared, and hypertension was found more frequently in patients with underlying glomerular diseases [36]. In our study, office BP measurements revealed significantly higher SBP values in the patient subgroups (especially the HD patients) than in the controls. Although not statistically significant, we also obtained higher DBP values in HD patients. Therefore, we may conclude that patients in HD subgroup were under risk of cardiovascular disease in terms of BP control despite antihypertensive medications and interventions towards volume overload. On the other hand, despite being on dialysis, PD patients had the best values in terms of BP control among the CKD subgroups. We attributed this finding to the fact that majority of the patients in the PD group had a primary diagnosis of CAKUT and they still had sufficient urine output or even polyuria during PD treatment era.
Several clinical parameters and non-invasive tests such as ECG have been developed to determine the risk of cardiovascular complications in CKD [37, 38]. A higher heart rate is a surrogate marker of sympathetic nerve activity and is considered as one of the risk factors for heart failure and cardiovascular disease [23, 39]. A previous study demonstrated increased sympathetic activity in pediatric patients with CKD, which was correlated with the severity of kidney failure. In the same study, it was shown that sympathetic functional recovery occurred after KTx [40]. In another study, Converse et al. found a higher rate of sympathetic nerve discharge and consequently higher heart rate in adult patients on chronic dialysis [41]. There are also pediatric reports showing increased heart rate in patients with kidney failure [37]. In our study, we obtained higher heart rate on ECG analysis in the patient group compared to healthy controls. The highest values were noted in dialysis patients, especially in HD, whereas the heart rate was closest to healthy controls in KTx patients. Even with the heart rate alone, we can consider that our patients were at a higher cardiovascular risk and transplantation can contribute to a decrease in the adverse outcome.
The QTc interval, a measure of net ventricular myocardial depolarization and repolarization, is another important ECG parameter for evaluating cardiovascular health. Prolongation of QT interval is associated with various components of the insulin resistance syndrome, age, body mass index, LVH, hypertension, CKD and in some studies the female gender [42]. Also, its prolongation is well described in association with electrolyte abnormalities including hypokalemia, hypocalcemia, and hypomagnesemia [43,44,45]. The prolongation of QT interval causes life-threatening cardiac arrhythmias including ventricular and atrial fibrillation and sudden cardiac death [46, 47]. QTcD is calculated as the difference between the maximum and the minimum QTc distances and its increase indicates heterogeneity in ventricular repolarization. Increased QT dispersion have been found in myocardial infarction, hypertrophic cardiomyopathy, hypertension, LVH, diabetes, chronic heart failure, mitral valve prolapses and genetically related long QT syndrome [48]. This parameter is also known to represent an increased risk of ventricular arrhythmias and sudden cardiac death like prolonged QTc interval [26, 49,50,51]. In a study conducted on pediatric dialysis patients, although there was no change in serum electrolyte levels, in more than half of the patients, a prolongation of the QT interval up to 40% was detected compared to the control group [45]. Similarly, Familoni et al. showed that QT and QTc intervals were prolonged, QTD and QTcD were increased in CKD patients, which worsened with dialysis treatment [51]. In another study by Özdemir et al., QTc was longer and QTcD was higher in children receiving HD compared to the healthy controls. In that study, it was mentioned that the patients may be at greater risk for sudden death due to the increase in QTcD reflecting the heterogeneous recovery of ventricular excitability [52]. In our study, QTc interval was longer and QTcD was higher in the patient group compared to the control subjects. The highest values for these two parameters were observed in dialysis patients. Although the mean serum potassium level was higher in our dialysis patients, which is unexpected to be associated with prolongation in QT interval, we believe that a combination several factors including the lower mean calcium level, presence of hypertension and CKD itself may have contributed to this outcome in dialysis patients.
Left ventricular hypertrophy remains the most reported cardiac complication in children with CKD [53, 54]. It is mainly secondary to increased BP and volume overload. Also, anemia, which causes a hyperdynamic state, and electrolyte disturbances such as hypocalcemia and hyperphosphatemia in the context of CKD may lead to LVH [54]. Matteucci et al. reported the prevalence of LVH as 35% in pediatric patients with stage 2 to 4 CKD and left ventricular mass was shown to be correlated with the degree of kidney dysfunction [50]. Similarly, LVH was found to be 70% in pediatric patients with CKD stage 5 [55]. On the other hand, a prospective study on pediatric CKD patients showed development of LVH in 32% of patients within two years even in the absence of progression in the CKD stages [56]. Presence of LVH can be estimated via ECG analysis [23]. However, a previous study showed low sensitivity and low negative predictive value of ECG for detecting LVH in children. The authors recommended that echocardiographic examination should be applied to confirm the LVH in clinical practice [9]. On the other hand, a more recent report indicated a higher sensitivity and specificity of ECG for the diagnosis of LVH [28]. Although reports focusing on this topic are scarce, we believe that conflicting results in the literature can stem from the use of different methods in the evaluation of LVH via ECG. In our study, although not statistically significant, LVH was detected more frequently by ECG in the patient group compared to the controls (21.8% vs 15%). In the subgroup analysis, LVH was most prominent in HD patients (47.1%), with a borderline statistical significance. Taking into account the increased percentage of other risk factors associated with LVH in these subsets of patients such as hypertension, anemia, hypocalcemia, hyperphosphatemia, and glomerular disease frequency as a primary diagnosis, we may speculate that LVH detected on ECG reflects the reality. Fortunately, we were able to evaluate 66 patients by echocardiography concurrently. In our study, echocardiography showed highest mean LVMI in HD patients and LVH was proportionally more frequent in them. The frequency of LVH was significantly higher in glomerular disease than in CAKUT. In stage 2 HT, LVH was also significantly more frequent compared to normotensive patients. Therefore, as ECG analysis results were in line with echocardiography, we think that LVH detected on ECG should not be ignored and patients particularly with ECG abnormalities that are suggestive of LVH should be referred for echocardiographic assessment for definitive diagnosis.
Kidney transplantation improves several clinical parameters, including cardiac functions. For example, Souza et al. showed that left ventricular mass decreased in the first two years after transplantation [57]. Similarly, in another study, a significant regression of LVH was observed even within 6 months after KTx [58]. The results of our study showed that the frequency of LVH via both ECG and echocardiography in KTx patients was considerably lower than in HD patients but mildly higher than in PD patients. However, echocardiography demonstrated lowest LVMI values despite increased age in the KTx group. Therefore, we may conclude that a significant improvement has been achieved in terms of LVH after transplantation. In our study, it is noteworthy that. In addition, there was an improvement on growth parameters such as weight and height z scores and BMI, as well as ECG parameters such as heart rate, QTc interval and QTcD in KTx patients when compared to dialysis patients. With this data, it can be concluded that KTx has a significant positive effect on growth and cardiac functions, which can be easily demonstrated via ECG.
In conclusion, we believe that non-invasive tests such as BP measurement and ECG evaluation that can be easily applied in every center can be used to detect cardiovascular problems in patients with CKD and KRT, especially in patients with HD, as our findings indicate highest cardiovascular risk in this group. By this way, it can be ensured that precautions can be taken for cardiovascular complications that may even result in sudden death. In addition, as the cardiovascular risky conditions were less frequent in our patients followed up with KTx, this result also highlights the vital importance and benefit of transplantation on the cardiac health.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Webster AC, Nagler EV, Morton RL, Masson P (2017) Chronic kidney disease. Lancet 389:1238–1252. https://doi.org/10.1016/S0140-6736(16)32064-5
Romagnani P, Remuzzi G, Glassock R et al (2017) Chronic kidney disease. Nat Rev Dis Primers 3:17088. https://doi.org/10.1038/nrdp.2017.88
Harambat J, van Stralen KJ, Kim JJ, Tizard EJ (2012) Epidemiology of chronic kidney disease in children. Pediatr Nephrol 27:363–373. https://doi.org/10.1007/s00467-011-1939-1
Chen TK, Knicely DH, Grams ME (2019) Chronic kidney disease diagnosis and management: a review. JAMA 322:1294–1304. https://doi.org/10.1001/jama.2019.14745
Zhong J, Yang HC, Fogo AB (2017) A perspective on chronic kidney disease progression. Am J Physiol Renal Physiol 312:F375–F384. https://doi.org/10.1152/ajprenal.00266.2016
Di Lullo L, House A, Gorini A, Santoboni A, Russo D, Ronco C (2015) Chronic kidney disease and cardiovascular complications. Heart Fail Rev 20:259–272. https://doi.org/10.1007/s10741-014-9460-9
Jardine GA, McLaughlin K (2001) Cardiovascular complications of renal disease. Heart 86:459–466. https://doi.org/10.1136/heart.86.4.459
Brown JH, Hunt LP, Vites NP, Shunt CD, Gokal R, Mallick NP (1994) Comparative mortality from cardiovascular disease in patients with chronic renal failure. Nephrol Dial Transpl 9:1136–1142. https://doi.org/10.1093/ndt/9.8.1136
Killian L, Simpson JM, Savis A, Rawlins D, Sinha MD (2010) Electrocardiography is a poor screening test to detect left ventricular hypertrophy in children. Arch Dis Child 95:832–836. https://doi.org/10.1136/adc.2009.168377
Panhuyzen-Goedkoop NM, Wellens HJ, Verbeek AL, Jørstad HT, Smeets JR, Peters RJ (2020) ECG criteria for the detection of high-risk cardiovascular conditions in master athletes. Eur J Prev Cardiol 27:1529–1538. https://doi.org/10.1177/2047487319901060
Alonso MAG, Lima VACC, Carreira MAMQ, Lugon JR (2017) Reproducibility and Reliability of QTc and QTcd measurements and their relationships with left ventricular hypertrophy in hemodialysis patients. Arq Bras Cardiol 109:222–230. https://doi.org/10.5935/abc.20170112
Neyzi O, Saka HN, Kurtoğlu S (2013) Anthropometric studies on the Turkish population, a historical review. J Clin Res Pediatr Endocrinol 5:1–12. https://doi.org/10.4274/Jcrpe.957
Turkish Pediatric Endocrinology and Diabetes Society (2017) Oksoloji. https://www.ceddcozum.com/Home/Change?%20Language%20Abbreviation=tr. Accessed 14 Oct 2022
Martinez-Millana A, Hulst JM, Boon M et al (2018) Optimisation of children z-score calculation based on new statistical techniques. PLoS ONE 13:e0208362. https://doi.org/10.1371/journal.pone.0208362
Dietz WH, Robinson TN (1998) Use of the body mass index (BMI) as a measure of overweight in children and adolescents. J Pediatr 132:191–193. https://doi.org/10.1016/s0022-3476(98)70426-3
Demir K, Konakçı E, Özkaya G et al (2020) New features for child metrics: further growth references and blood pressure calculations. J Clin Res Pediatr Endocrinol 12:125–129. https://doi.org/10.4274/jcrpe.galenos.2019.2019.0127
Anderson LN, Carsley S, Lebovic G et al (2017) Misclassification of child body mass index from cut-points defined by rounded percentiles instead of Z-scores. BMC Res Notes 10:639. https://doi.org/10.1186/s13104-017-2983-0
Subcommıttee on Screenıng and Management of High Blood Pressure in Children (2017) Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140:e20171904. https://doi.org/10.1542/peds.2017-1904
Locatelli F, Nissenson AR, Barrett BJ et al (2008) Clinical practice guidelines for anemia in chronic kidney disease: problems and solutions. A position statement from kidney disease: Improving Global Outcomes (KDIGO). Kidney Int 74:1237–1240. https://doi.org/10.1038/ki.2008.299
Schwartz GJ, Work DF (2009) Measurement and etimation of GFR in children and adolescents. Clin J Am Soc Nephrol 4:1832–1843. https://doi.org/10.2215/CJN.01640309
Fadrowski JJ, Furth SL (2011) GFR estimation in children: questions and answers (and questions). Clin J Am Soc Nephrol 6:1810–1812. https://doi.org/10.2215/CJN.05900611
Fleming S, Thompson M, Stevens R et al (2011) Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: a systematic review of observational studies. Lancet 377:1011–1018. https://doi.org/10.1016/S0140-6736(10)62226-X
Rijnbeek PR, Witsenburg M, Schrama E, Hess J, Kors JA (2001) New normal limits for the paediatric electrocardiogram. Eur Heart J 22:702–711. https://doi.org/10.1053/euhj.2000.2399
Bazett HC (1920) An analysis of the time relations of electrocardiograms. Heart 7:353–367
Garson A (1993) How to measure the QT interval-what is normal? Am J Cardiol 72:14B-16B. https://doi.org/10.1016/0002-9149(93)90034-a
Koçak G, Atalay S, Bakkaloglu S, Ekim M, Tutar HE, Imamoglu A (1999) QT/corrected QT (QTc) intervals and QT/QTc dispersions in children with chronic renal failure. Int J Cardiol 70:63–67. https://doi.org/10.1016/s0167-5273(99)00051-0
Malik M, Batchvarov VN (2000) Measurement, interpretation and clinical potential of QT dispersion. J Am Coll Cardiol 36:1749–1766. https://doi.org/10.1016/s0735-1097(00)00962-1
Peguero JG, Lo Presti S, Perez J, Issa O, Brenes JC, Tolentino A (2017) Electrocardiographic criteria for the diagnosis of left ventricular hypertrophy. J Am Coll Cardiol 69:1694–1703. https://doi.org/10.1016/j.jacc.2017.01.037
Devereux RB, Alonso DR, Lutas EM et al (1986) Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57:450–458. https://doi.org/10.1016/0002-9149(86)90771-x
Furqan M, Haque A (2009) Surface area in children: a simple formula. Indian Pediatr 46:1085–1087
Khoury PR, Mitsnefes M, Daniels SR, Kimball TR (2009) Age-specific reference intervals for indexed left ventricular mass in children. J Am Soc Echocardiogr 22:709–714. https://doi.org/10.1016/j.echo.2009.03.003
Mitsnefes MM (2012) Cardiovascular disease in children with chronic kidney disease. J Am Soc Nephrol 23:578–585. https://doi.org/10.1681/ASN.2011111115
Ku E, Lee BJ, Wei J, Weir MR (2019) Hypertension in CKD: Core Curriculum 2019. Am J Kidney Dis 74:120–131. https://doi.org/10.1053/j.ajkd.2018.12.044
VanDeVoorde RG, Mitsnefes MM (2011) Hypertension and CKD. Adv Chronic Kidney Dis 18:355–361. https://doi.org/10.1053/j.ackd.2011.03.003
Alexandrou ME, Loutradis C, Schoina M et al (2020) Ambulatory blood pressure profile and blood pressure variability in peritoneal dialysis compared with hemodialysis and chronic kidney disease patients. Hypertens Res 43:903–913. https://doi.org/10.1038/s41440-020-0442-0
Lübbe K, Nüsken E, Rascher K et al (2019) Glomerular disease patients have higher odds not to reach quality targets in chronic dialysis compared with CAKUT patients: analyses from a nationwide German paediatric dialysis registry. Pediatr Nephrol 34:1229–1236. https://doi.org/10.1007/s00467-019-04218-6
Hallioglu O, Keceli M, Bozlu G, Delibas A, Karpuz D, Selvi H (2018) Evaluation of T-wave alternans in pediatric patients with chronic renal failure. J Electrocardiol 51:622–627. https://doi.org/10.1016/j.jelectrocard.2018.04.013
Skampardoni S, Poulikakos D, Malik M, Green D, Kalra PA (2019) The potential of electrocardiography for cardiac risk prediction in chronic and end-stage kidney disease. Nephrol Dial Transplant 34:1089–1098. https://doi.org/10.1093/ndt/gfy255
Ohashi N, Isobe S, Ishigaki S et al (2019) Increased heart rate is associated with intrarenal renin-angiotensin system activation in chronic kidney disease patients. Clin Exp Nephrol 23:1109–1118. https://doi.org/10.1007/s10157-019-01746-1
Parisotto V, Lima EM, Silva JM, de Sousa MR, Ribeiro AL (2008) Cardiac sympathetic dysautonomia in children with chronic kidney disease. J Nucl Cardiol 15:246–254. https://doi.org/10.1016/j.nuclcard.2008.01.003
Converse RL Jr, Jacobsen TN, Toto RD et al (1992) Sympathetic overactivity in patients with chronic renal failure. N Engl J Med 327:1912–1918. https://doi.org/10.1056/NEJM199212313272704
Festa A, D’Agostino R Jr, Rautaharju P, Mykkänen L, Haffner SM (2000) Relation of blood pressure, left ventricular mass, insulin sensitivity, and coronary artery disease to QT interval duration in nondiabetic and type 2 diabetic subjects. Am J Cardiol 86:1117–1122. https://doi.org/10.1016/s0002-9149(00)01170-x
Williams MJ, Hammond-Tooke GD, Restieaux NJ (1995) Hypokalemic periodic paralysis with cardiac arrhythmia and prolonged QT interval. Aust N Z J Med 25:549. https://doi.org/10.1111/j.1445-5994.1995.tb01512.x
Huang TC, Cecchin FC, Mahoney P, Portman MA (2000) Corrected QT interval (QTc) prolongation and syncope associated with pseudohypoparathyroidism and hypocalcemia. J Pediatr 136:404–407. https://doi.org/10.1067/mpd.2000.103447
Bosch A, Ulmer HE, Keller HE, Bonzel KE, Schärer K (1990) Electrocardiographic monitoring in children with chronic renal failure. Pediatr Nephrol 4:140–144. https://doi.org/10.1007/BF00858825
Butani L, Berg G, Makker SP (2002) QTc interval in children with chronic renal failure and with renal transplants. Pediatr Nephrol 17:6–9. https://doi.org/10.1007/s004670200001
Vandael E, Vandenberk B, Vandenberghe J, Willems R, Foulon V (2017) Risk factors for QTc-prolongation: systematic review of the evidence. Int J Clin Pharm 39:16–25. https://doi.org/10.1007/s11096-016-0414-2
Barr CS, Naas A, Freeman M, Lang CC, Struthers AD (1994) QT dispersion and sudden unexpected death in chronic heart failure. Lancet 343:327–329. https://doi.org/10.1016/s0140-6736(94)91164-9
Ducceschi V, Sarubbi B, Giasi A et al (1996) Correlation between late potentials duration and QTc dispersion: Is there a causal relationship? Int J Cardiol 53:285–290. https://doi.org/10.1016/0167-5273(96)02565-x
Akintunde AA, Oyedeji AT, Familoni OB, Ayodele OE, Opadijo OG (2012) QT Interval prolongation and dispersion: Epidemiology and clinical correlates in subjects with newly diagnosed systemic hypertension in Nigeria. J Cardiovasc Dis Res 3:290–295. https://doi.org/10.4103/0975-3583.102705
Familoni OB, Alebiosu CO, Ayodele OE (2006) Effects and outcome of haemodialysis on QT intervals and QT dispersion in patients with chronic kidney disease. Cardiovasc J S Afr 17:19–23
Ozdemir D, Mese T, Agin H, Calkavur S, Bak M (2005) Impact of haemodialysis on QTc dispersion in children. Nephrology (Carlton) 10:119–123. https://doi.org/10.1111/j.1440-1797.2005.00378.x
Matteucci MC, Wühl E, Picca S et al (2006) Left ventricular geometry in children with mild to moderate chronic renal insufficiency. J Am Soc Nephrol 17:218–226. https://doi.org/10.1681/ASN.2005030276
Taddei S, Nami R, Bruno RM, Quatrini I, Nuti R (2011) Hypertension, left ventricular hypertrophy and chronic kidney disease. Heart Fail Rev 16:615–620. https://doi.org/10.1007/s10741-010-9197-z
Chavers BM, Herzog CA (2004) The spectrum of cardiovascular disease in children with predialysis chronic kidney disease. Adv Chronic Kidney Dis 11:319–327. https://doi.org/10.1053/j.arrt.2004.04.002
Mitsnefes MM, Kimball TR, Kartal J et al (2006) Progression of left ventricular hypertrophy in children with early chronic kidney disease: 2-Year follow-up study. J Pediatr 149:671–675. https://doi.org/10.1016/j.jpeds.2006.08.017
Souza FL, Monteiro Junior FD, Salgado Filho N (2012) Effect of kidney transplantation on cardiac morphology and function. J Bras Nefrol 34:94–100
Jhinger MK, Sohal PM, Makkar V, Tondon R, Wander GS, Sandhu JS (2021) Changes in cardiac structure and function before and after renal transplantation: a longitudinal study. Transplant Proc 53:1014–1018. https://doi.org/10.1016/j.transproceed.2021.01.026
Author information
Authors and Affiliations
Contributions
Emre Leventoğlu, Bahar Büyükkaragöz, Furkan Çağrı Kavas, Mert Can Holoğlu and Akif Kavgacı contributed to conception and design; contributed to acquisition, analysis, and interpretation; Emre Leventoğlu and Bahar Büyükkaragöz wrote the main manuscript text; Furkan Çağrı Kavas, Mert Can Holoğlu and Akif Kavgacı prepared the tables; Bahar Büyükkaragöz, Kibriya Fidan, Aydın Dalgıç, Sevcan A Bakkaloğlu and Fatma Sedef Tunaoğlu critically revised the manuscript; Sevcan A Bakkaloğlu, Fatma Sedef Tunaoğlu and Oğuz Söylemezoğlu gave final approval; All authors agrees to be accountable for all aspects of work ensuring integrity and accuracy. All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by and Akif Kavgacı. The first draft of the manuscript was written by Emre Leventoğlu. Kibriya Fidan, Aydın Dalgıç, Sevcan A Bakkaloğlu, Fatma Sedef Tunaoğlu and Oğuz Söylemezoğlu commented on previous versions of the manuscript and critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the Medical Ethics Committee of Gazi University (file number 2022–1468).
Consent to participate
Written informed consent was obtained from all participants and their parents. Our research was carried out in line in accordance with the standards.
Conflict of interest
The authors have no conflicts of interest to disclose.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Leventoğlu, E., Büyükkaragöz, B., Kavas, F.Ç. et al. Electrocardiographic measurements in children with pre-dialysis chronic kidney disease and undergoing kidney replacement therapy. Eur J Pediatr 182, 4993–5005 (2023). https://doi.org/10.1007/s00431-023-05154-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05154-2