Abstract
Infection is an important cause of death during infancy worldwide and is a frequent etiology of sudden unexpected death in infancy (SUDI). Procalcitonin (PCT) is a useful marker to diagnose infection in patients, and several studies report the stability of PCT after death. The added value of a biological marker, such as the PCT level in the blood, remains controversial in investigating SUDI. The aim of this study was to determine if PCT can help clinicians determine whether infection caused SUDI. We conducted a retrospective, multicenter study with the French SUDI registry (Observatoire National des Morts Inattendues du Nourrisson; OMIN). We collected data from this registry on children who died between May 2015 and June 2021. The levels of PCT in the blood of 540 SUDI patients were measured. We compared PCT and other biological tests performed in terms of infection status, autopsy results, and cause of death using clinical and biological data compiled by pediatricians at the SUDI referral center. PCT levels were significantly higher in the children who died from infection than in those who did not (0.12 µg/L vs. 0.08 µg/L, p < 0.001). A PCT blood level exceeding 0.2 µg/L was more frequently observed when infection was present than in the absence of infection (44.3% vs. 15.4%, p < 0.001). The same data were obtained with a 0.5 µg/L cut-off (36.1% with infection vs. 9.2% without, p < 0.001).
Conclusions: PCT is a sensitive biomarker for detecting infections postmortem; thus, additional samples may be necessary during autopsy.
What is known: • PCT is a stable marker postmortem and increases earlier than CRP, i.e., 2–4 h after the beginning of an infection vs. 6 h. • PCT can be measured up to 140 h after death. | |
What is new: • PCT is a sensitive marker for detecting infection in SUDI patients postmortem. • This test can reveal an infection from non-standardized samples obtained during autopsy if such an infection was not determined before death. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sudden unexpected death in infancy (SUDI) is the sudden and unexpected death of a child under 1 year of age without any predictive clinical history [1, 2]. SUDI is the leading cause of death between 1 month and 1 year [1, 3, 4]. The French National Authority for Health (Haute Autorité de Santé: HAS) provides guidelines for SUDI management. The latest guidelines, published in 2007, recommend laboratory tests and autopsy to determine the cause of death (infection, asphyxia, heart disease, abuse, or poisoning) [2]. In France, SUDI data are collected by the French Institute for Public Health Surveillance (Institut de Veille Sanitaire; InVS). The French Sudden Unexpected Infant Death registry (Observatoire National des Morts Inattendues du Nourrisson registry; OMIN) reports between 250 and 350 deaths annually among 37 centers [3]. Each case is documented by the pediatrician who obtained postmortem samples and ordered the autopsy, as recommended by the French guidelines [5].
Infection is the second leading cause of death among SUDI patients [1, 2]. Viral infections of the respiratory tract are the most common [6, 7]. The procalcitonin (PCT) blood test is not recommended [2], which may explain why PCT testing is performed in only 30.8% of cases, unlike C-reactive protein (CRP) testing, which is performed in 85.5% of cases, according to InVS data [5].
PCT is a 116 amino–acid peptide precursor generated from calcitonin. PCT blood levels are increased in cases of bacterial infection [8,9,10]. In clinical conditions, a PCT blood level above 0.5 µg/L is generally considered to indicate infection [9, 11]. PCT may be a valuable marker for discriminating sepsis [12], which has been confirmed by several studies [13,14,15]. Infection is possible if the PCT blood level is between 0.25 and 0.5 µg/L [11].
Few data exist regarding PCT levels after death. PCT has been reported to remain stable for many hours after death, with levels remaining significantly different for 140 h among patients who died from sepsis vs. non-sepsis–related deaths [12]. PCT blood levels increase within 2 h after the beginning of the infection, while CRP levels increase after 6 h [9, 16]. PCT may be a relevant predictor of death at the beginning of an infection; however, no studies have evaluated the value of PCT testing in SUDI. Indicators of an infectious cause of death would have several impacts on autopsy. Additional samples may have to be taken during autopsy to research a human microbiological pathogen. The aim of our study was to determine if PCT could be a sensitive biological marker to identify infection as a possible cause of SUDI.
Material and methods
Study design
We conducted a multicenter retrospective study using French SUDI registry data. We collected all SUDI data from May 1, 2015, to June 30, 2021, including the demographic characteristics (sex, gestational age, and multiple-birth information), medical history (chronic disease, postnatal smoke exposure, and family history of sudden infant death syndrome), characteristics at the time of death (age, weight, height, the occurrence of death while sleeping, the occurrence of death during winter, and resuscitation attempts), and medically significant events in the 72 h preceding SUDI (signs of dehydration, purpura, clinical manifestations, and medical consultation information). We also collected available biological and microbiological laboratory test results, radiological data, and whether an autopsy had been performed. Post-mortem blood samples are taken by pediatricians caring for children in French reference center part of the OMIM group. The sample can be taken by intracardiac puncture via the subxiphoid route or by a puncture of the subclavian artery. Children for whom PCT blood levels were not measured were excluded since we investigated PCT as a biomarker associated with infectious causes of death; we also excluded case whom PCT blood level was measured but without data to explore the infectious status of the child.
Determination of infection as the cause of death
All patients included in the study were classified into two groups based on their medical records and the presence of an infectious process as the trigger for death. We exclude cases with a medical conclusion and without any clinical data. Two authors (M.C. and A.W.) reviewed all cases to verify the medical referent’s conclusion with the medical history and microbiological and autopsy results documented in the registry. We only classified a SUDI case in the infected group in case of both microbiological and histological element abnormalities in favor of an infectious process. In cases with no microbiological identification and no evidence of infection in the autopsy conclusion, the case was considered classified in the “non-infected group,” even if the medical referent concluded that the cause of death was an infection. We also considered SUDI cases in the non-infected group in absence of histological element associated with blood culture samples. In cases where the two authors disagreed, a third author (M.H. a pediatrician expert in forensic medicine) reviewed the case to determine if an infection was the cause of death.
Procalcitonin blood level interpretation
A PCT blood level above 0.5 µg/L is a marker of infection [9] with a sensitivity between 70 and 80% and a specificity of approximately 70%, according to different studies [11, 17,18,19].
We also considered those with levels of 0.2 µg/L since this is considered a good negative predictive value [10, 20] and may rule out infection [9, 10].
Statistical analysis
The analytical data are presented as the median with 25th and 75th percentiles (median and interquartile range) for continuous variables; categorical variables are presented as numbers and percentages. Comparisons of baseline characteristics associated with infectious causes of SUDI were conducted by using Wilcoxon or Kruskal‒Wallis tests for continuous variables and the Fisher exact or χ2 test for categorical variables. A two-sided p-value ≤ 0.05 was considered to indicate significance. Statistical analyses were performed using R version 4.1.1 (2021–08-10) (R Foundation for Statistical Computing, Vienna, Austria).
Ethics
The French SUDI registry was approved by an independent ethics committee (Groupe Nantais d’Ethique dans le Domaine de la Santé — n°2015–01-27) within the French Data Protection Authority in clinical research (Commission Nationale de l’Informatique et des Libertés — CNIL — n°915,273) and by the national registry evaluation committee, comprising the National Institute of Health for Medical Research (Inserm), the National Cancer Institute (INCa) and the National Public Health Agency (Santé Publique France).
Results
Baseline characteristics (Table 1)
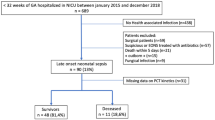
Among 1185 SUDI cases in the French SUDI registry, the PCT blood level was available for 540 (45.6%). A total of 158/540 (29.3%) children died from infection, as shown in the flow chart (Fig. 1).
In our population, 298 of the patients were male (55.3%), the median term was 39.1 weeks and 87 (17.2%) were preterm. Thirty-nine were from multiple-birth pregnancies. A total of 11.8% of the survey population had a chronic disease, and 13.1% had a family history of SUDI. Only 28.3% of SUDI occurred during the winter. The median age at the time of death was 115 days. Half of the children exhibited clinical manifestations in the 72 h preceding death (50.8%), and 39.8% was medically evaluated.
The most frequent postmortem samples taken were nasopharyngeal swabs (84.8% for virology), blood cultures (82.2% for bacteriology) and cerebrospinal fluid draws (74.4% for bacteriology). Urine and feces samples are taken less frequently. Among all SUDI cases, 117 had a bacterial documentation (46 cases had at least 2 different bacteria), 135 cases had a viral documentation (52 had at least 2 different viruses), and 67 SUDI cases had at least one bacteria and one virus.
An autopsy was performed on 81.3% of the patients. Parental refusal was the most frequent reason an autopsy was not performed (85.1%). The median time between death and autopsy was 36 h (maximum 60 h). Toxicology analyses were performed on 11.3% of the patients.
Cause of death (Table 1)
Asphyxia was the most commonly reported cause of death (49.2%); the second most common cause was infection (37.4%). Viruses in the respiratory tract were more frequently observed among those who died from infection than in those who did not (39.9% vs. 18% p < 0.001). The same observation was made for bacteremia (24.7% vs. 0% p < 0.001) and viral infections of the ear, nose and throat (ENT) (21.5% vs. 6% p < 0.001).
Comparison of children who died from infection vs. other etiologies (Table 2)
No significant differences were observed in terms of sex, death occurrence in winter, chronic diseases or gestational age at birth. Children who died from infection were significantly older (144 vs. 107 days, p < 0.001) and heavier (6520 vs. 5910 g, p < 0.001) than those who died from other causes.
No significant difference was noticed regarding purpura between the two groups; however, 5 non-infected children had purpura. Clinical manifestations (66% vs. 44.4%, p 0.014) and medical consultations before death were more frequent in the infection group vs. the non-infection group (49.4% vs. 33.3% p < 0.001).
In 86.9% of cases (437/503), CRP levels were below 10 mg/L. In these 437 cases, the median CRP blood level was 28.2 mg/L. CRP < 10 mg/L was most frequently associated with noninfectious causes of death (92.4% vs. 73.5%, p < 0.001). There was no significant difference in the median CRP blood level between the groups (34 mg/L in the infected group vs. 20 mg/L in the non-infected group, p = 0.054).
Bacteria and virus identifications in both groups are detailed in the supplementary data.
Procalcitonin levels according to infectious status (Table 2)
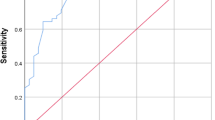
In the whole population, the median PCT blood level was 0.09 µg/L (IQR 0.06–0.16). The PCT blood levels exceeded 0.2 µg/L in 22.6% of the patients (122/540). The median PCT blood level was 0.12 µg/L in patients who died from infection (IQR 0.06–1.88), significantly different from that of patients who died from other etiologies (0.08 µg/L, IQR 0.05–0.11) (Fig. 2) (p < 0.001). A PCT blood level exceeding 0.2 µg/L was more frequently observed in the infected group (44.3% vs. 15.4% p < 0.001).
Discussion
Among the 540 cases of SUDI studied, the PCT blood level was significantly higher in children who died from infection than in those who died from other causes. These results suggest that PCT is a potential biomarker for exploring SUDI etiology. Our population is similar to other SUDI populations described by InVS in terms of patient age, weight [5] and etiology (most commonly asphyxia) [2, 5]. The second most frequent cause of SUDI is infection (Table 1), typically respiratory infection [6, 7] (Table 2).
We determined infection as the cause of death using medical records and microbiological documentation. We excluded cases without evidence of sepsis or infection in the autopsy conclusion and without microbiological documentation, even if the medical conclusion indicated infection.
Postmortem microbiological samples are difficult to analyze [19]. Postmortem contamination [21], bacterial translocation [21, 22] and agonal spread [22] cause numerous false-positive microbiological results. We also observed substantial contamination in our population, as shown in the supplementary table. Coagulase-negative Staphylococcus is reported to be the most common species observed in contamination cases [21]. We also frequently observed oral Streptococci. ENT samples are most commonly contaminated due to the commensal species in the respiratory tract. In our cohort, the maximum delay between death and autopsy was 60 h, and autopsy data are interpretable up to this point.
Clinicians frequently look for evidence of infection by measuring CRP blood levels. The kinetics of CRP and PCT differ [8, 9, 23]; PCT levels increase during the first 2 h of infection [8, 14], whereas CRP levels increase during the first 6 h [24, 25]. Several studies have shown that PCT is a stable marker, even after death [13,14,15]. CRP levels can be measured up to 48 h postmortem [25], whereas PCT testing can be performed up to 140 h after death [10, 14]. We observed that low CRP blood levels (< 10 mg/L) were significantly more frequently associated with death from noninfectious causes. Additionally, the median CRP blood level did not significantly differ depending on infection status. Thus, our results suggest that CRP may not be as discriminating as PCT in SUDI.
In our population, the median PCT level differed significantly among those who died from bacterial and viral infections and those who died from other etiologies. “It is generally assumed that PCT is good indicator for bacterial infection only, although there are reports of increased PCT in viral infection as well, and we observe an increase PCT blood value in both bacterial and viral infections. We also notice a numerous cases of bacterial and virus coinfection.” A PCT threshold above 0.2 or 0.5 µg/L was discriminant, potentially helping clinicians obtain relevant samples when exploring SUDI cases.
Downes et al. observed that PCT is a better marker than CRP for detecting sepsis and guiding antibiotic discontinuation in children [26]. Wacker et al. conducted a systematic review and meta-analysis and concluded that PCT is a predictive biomarker, revealing an association between PCT and infection status of 0.85 [27]. Kim et al. focused on pediatric bacterial meningitis. PCT is an accurate marker for diagnosing meningitis and reducing unnecessary antibiotic prescriptions and course durations, with an area under the curve value of 0.921 [28]. Stassi et al. reported in a systematic review that a CRP blood level > 10 mg/L and a PCT blood level > 2 µg/L indicate infection [29]. This review focused on sepsis and did not consider all types of infection. However, the reported association between PCT and CRP is interesting.
The above findings are consistent with the sensitivity of PCT as a marker in children; however, medical history and physical and microbiological examinations should not be overlooked. Furthermore, from a forensic perspective, an elevated blood PCT level is a key indicator that the cause of death was not criminal. We intended to determine whether PCT is a good marker in SUDI. In our study, the PCT blood level was a sensitive marker associated with postmortem etiology. When PCT is increased, practitioners should perform microbiological sampling to document early infection and conduct exhaustive infection-related sampling during autopsy to increase the possibility of detecting an infection; typically, during an autopsy, samples are not routinely taken from all organs.
One limitation of our study is the small sample size. We only included cases with available PCT blood levels, and this test was not performed in many cases. Moreover PCT blood level is not recommended is case of SUDI in France. Despite these guidelines, clinician could decide to evaluate PCT blood level, and more frequently when they hypothesize an infectious process. A second limitation is that the pediatrician may not be informed of the microbiological results, as positive test results can take several days of culture to obtain. We reviewed all cases twice to determine whether an infection was present and avoid misclassification and incorrect analyses. Few patients underwent toxicological testing (11.3%), which is surprising since this is an important and easy-to-perform test to obtain a differential diagnosis. We only classified in the infected group, SUDI cases that associate histological element in favor of an infectious process and a microbiological documentation. By this method, we hope to limit the risk to consider as non-infected a child that died because of an infectious process. We also excluded SUDI cases in which PCT blood level was measured but lack elements to explore infectious status according to these two points. But we could have wrongly classified some SUDI cases in the non-infected group despite that the child died because of an infectious process, for example, in case of positive blood culture but in absence of histological lesions. In most of these cases, the identified bacteria are often associated with a contamination status [30], but it is possible that the infectious process is not already clinically and macroscopically apparent. This is the third limit of our study and demonstrates the importance of having a biomarker to suggest the existence of an infectious process at the time of death, which could impact the realization of multiple samples for histological analyses.
Conclusion
Infection is the leading cause of infant death worldwide. Infection is also the second most common etiology of SUDI after asphyxia. PCT testing may be a useful tool in research on the etiology of SUDI. The PCT blood level is a valuable and sensitive postmortem biomarker; increased PCT is associated with infection. PCT testing could be generalized to all cases of SUDI to research evidence of infection. A prospective study with a specific autopsy program for patients with increased PCT blood levels could determine whether PCT-level testing can increase the detection of infections and improve microbiological documentation.
References
Levieux K, Patural H, Harrewijn I, Briand Huchet E, de Visme S, Gallot G, Chalumeau M, Gras Le Guen C, Hanf M, OMIN Study Group (2018) The French prospective multisite registry on sudden unexpected infant death (OMIN): rationale and study protocol. Br Med J 8(4):e020883. https://doi.org/10.1136/bmjopen-2017-020883
HAS (2007) Prise en charge en cas de mort inattendue du nourrisson (moins de 2 ans). https://www.has-sante.fr/jcms/c_533467/fr/prise-en-charge-en-cas-de-mort-inattendue-du-nourrisson-moins-de-2-ans. Accessed 3 Jan 2022
OMIN (2022) Observatoire national des morts inattendues du nourrisson. OMIN https://www.omin.fr/. Accessed 10 Jan 2022
de Visme S, Chalumeau M, Levieux K, Patural H, Harrewijn I, Briand-Huchet É, Rey G, Morgand C, Blondel B, Gras-Le Guen C, Hanf M (2020) National variations in recent trends of sudden unexpected infant death rate in Western Europe. J Pediatr 226:179-185.e4. https://doi.org/10.1016/j.jpeds.2020.06.052
Bloch J, Denis P, Jezewski-Serra D (2022) Les morts inattendues des nourrissons de moins de 2 ans. InVS. http://archives.invs.santepubliquefrance.fr/publications/2011/morts_nourrissons/index.html. Accessed 10 Jan 2022
Oliveira M, Amorim A (2018) Microbial forensics: new breakthroughs and future prospects. Appl Microbiol Biotechnol 102(24):10377–10391. https://doi.org/10.1007/s00253-018-9414-6
Gaaloul I, Riabi S, Evans M, Hunter T, Huber S, Aouni M (2016) Postmortem diagnosis of infectious heart diseases: a mystifying cause of Sudden Infant Death. Forensic Sci Int 262:166–172. https://doi.org/10.1016/j.forsciint.2016.03.002
Hamade B, Huang DT (2020) Procalcitonin : where are we now? Crit Care Clin 36(1):23–40. https://doi.org/10.1016/j.ccc.2019.08.003
Biomnis (2012) Procalcitonine In : Précis de biopathologie analyses médicales spécialisées Biomnis. https://www.eurofins-biomnis.com/referentiel/liendoc/precis/PROCALCITONINE.pdf. Accessed 15 Jan 2022
Damman J, Arias P, Kerner J, Zhang K-Y, Dehghan M, Krishnan G, Nespor C, Bensen R, Park KT (2019) Procalcitonin as a predictive marker for bacteremia in children with a central line and fever. Hosp Pediatr 9(6):434–439. https://doi.org/10.1542/hpeds.2018-0123
Shaikh KJ, Osio VA, Leeflang MM, Shaikh N (2020) Procalcitonin, C-reactive protein, and erythrocyte sedimentation rate for the diagnosis of acute pyelonephritis in children. Cochr Data Syst Rev 9(9):CD009185. https://doi.org/10.1002/14651858.CD009185.pub3
Tsokos M, Reichelt U, Nierhaus A, Püschel K (2001) Serum procalcitonin (PCT): a valuable biochemical parameter for the post-mortem diagnosis of sepsis. Int J Leg Med 114(4–5):237–243. https://doi.org/10.1007/s004140000177
Schrag B, Roux-Lombard P, Schneiter D, Vaucher P, Mangin P, Palmiere C (2012) Evaluation of C-reactive protein, procalcitonin, tumor necrosis factor alpha, interleukin-6, and interleukin-8 as diagnostic parameters in sepsis-related fatalities. Int J Leg Med 126(4):505–512. https://doi.org/10.1007/s00414-011-0596-z
Barranco R, Ventura F (2019) Biochemical markers and microbiology in post-mortem diagnosis of sepsis: a systematic review. Rom J Leg Med 27(3):230–238. https://doi.org/10.4323/rjlm.2019.230
Attia AM, Abo El-Atta HM, El-sherbiny M, El-Shahat EE (2016) Evaluation of procalcitonin postmortem levels in some models of death: an experimental study. J Forensic Leg Med 37:28–32. https://doi.org/10.1016/j.jflm.2015.08.011
Ferrière F (2000) Intérêt de la procalcitonine, nouveau marqueur de l’infection bactérienne. Ann Biol Clin 58(1):49–59
Bruel AV, den Thompson MJ, Haj-Hassan T, Stevens R, Moll H, Lakhanpaul M, Mant D (2011) Diagnostic value of laboratory tests in identifying serious infections in febrile children: systematic review. BMJ 342:d3082. https://doi.org/10.1136/bmj.d3082
Leroy S, Fernandez-Lopez A, Nikfar R, Romanello C, Bouissou F, Gervaix A, Gurgoze MK, Bressan S, Smolkin V, Tuerlinckx D, Stefanidis CJ, Vaos G, Leblond P, Gungor F, Gendrel D, Chalumeau M (2013) Association of procalcitonin with acute pyelonephritis and renal scars in pediatric UTI. Pediatr 131(5):870–879. https://doi.org/10.1542/peds.2012-2408
Oussalah A, Ferrand J, Filhine-Tresarrieu P, Aissa N, Aimone-Gastin I, Namour F, Garcia M, Lozniewski A, Guéant JL (2015) Diagnostic accuracy of procalcitonin for predicting blood culture results in patients with suspected bloodstream infection. Medicine 94(44):e1774. https://doi.org/10.1097/MD.0000000000001774
Sager R, Kutz A, Mueller B, Schuetz P (2017) Procalcitonin-guided diagnosis and antibiotic stewardship revisited. BMC Med 15(1):15. https://doi.org/10.1186/s12916-017-0795-7
Saegeman V, Cohen MC, Burton JL, Martinez MJ, Rakislova N, Offiah AC, Fernandez-Rodriguez A (2021) Microbiology in minimally invasive autopsy: best techniques to detect infection. ESGFOR (ESCMID study group of forensic and post-mortem microbiology) guidelines. Forensic Sci Med Pathol 17(1):87–100. https://doi.org/10.1007/s12024-020-00337-x
Weber MA, Hartley JC, Brooke I, Lock PE, Klein NJ, Malone M, Sebire NJ (2010) Post-mortem interval and bacteriological culture yield in sudden unexpected death in infancy (SUDI). Forensic Sci Int 198(1–3):121–125. https://doi.org/10.1016/j.forsciint.2010.02.002
Astrup BS, Thomsen JL (2007) The routine use of C-reactive protein in forensic investigations. Forensic Sci Int 172(1):49–55. https://doi.org/10.1016/j.forsciint.2006.10.021
Ondruschka B, Woydt L, Bernhard M, Franke H, Kirsten H, Löffler S, Pohlers D, Hammer N, Dreßler J (2019) Post-mortem in situ stability of serum markers of cerebral damage and acute phase response. Int J Leg Med 133(3):871–881. https://doi.org/10.1007/s00414-018-1925-2
Lindroos-Jokinen K, Keltanen T, Vanhala T, Valonen T, Sajantila A (2012) Postmortem measurement of C-reactive protein and interpretation of results in ketoacidosis. Leg Med 14(3):140–146. https://doi.org/10.1016/j.legalmed.2012.01.009
Downes KJ, Fitzgerald JC, Weiss SL (2020) Utility of procalcitonin as a biomarker for sepsis in children. J Clin Microbiol 58(7):e01851-e1919. https://doi.org/10.1128/JCM.01851-19
Wacker C, Prkno A, Brunkhorst FM, Schlattmann P (2013) Procalcitonin as a diagnostic marker for sepsis : a systematic review and meta-analysis. Lancet Infect Dis 13(5):426–435. https://doi.org/10.1016/S1473-3099(12)70323-7
Kim H, Roh YH, Yoon SH (2021) Blood procalcitonin level as a diagnostic marker of pediatric bacterial meningitis: a systematic review and meta-analysis. Diagn (Basel, Switzerland) 11(5):846. https://doi.org/10.3390/diagnostics11050846
Stassi C, Mondello C, Baldino G, Ventura Spagnolo E (2020) Post-mortem investigations for the diagnosis of sepsis: a review of literature. Diagn 10(10):E849. https://doi.org/10.3390/diagnostics10100849
Segal GS, Chamberlain JM (2000) Resource utilization and contaminated blood cultures in children at risk for occult bacteremia. Arch Pediatr Adolesc Med 154(5):469–473. https://doi.org/10.1001/archpedi.154.5.469
Acknowledgements
We thank the families affected by SUDI as well as the participating centers. We also are grateful to the OMIN study group for the data.
Author information
Authors and Affiliations
Contributions
Author Contributions: All authors contributed to the study's conception and design. Material preparation, data collection and analysis were performed by M.C., M.H. and A.W.. M.C. and A.W. wrote the first draft of the manuscript, and all authors commented on the previous versions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Daniele De Luca
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Collette, M., Hauet, M., de Visme, S. et al. Procalcitonin is associated with sudden unexpected death in infancy due to infection. Eur J Pediatr 182, 3929–3937 (2023). https://doi.org/10.1007/s00431-023-05064-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05064-3