Abstract
Post-traumatic fat embolism syndrome (FES) is a severe complication consequent to bone fractures. The authors describe its clinical features and management in a population of teenagers by detailing demographics, organ involvement, laboratory, and imaging findings, as well as outcome. Moreover, a systematic review of pediatric published case reports of post-traumatic FES is provided. First, a series of eight episodes of post-traumatic FES that occurred in seven patients (median age 16.0 years, IQR 16.0–17.5) admitted to a pediatric intensive care unit (PICU) in an 8-year period was analyzed through a retrospective chart review. Secondly, a systematic research was performed on PUBMED database. Trauma patients ≤ 18 years without comorbidities in a 20-year period (2002–2022) were included in the review. Neurological impairment was present in five out of seven patients, and a patent foramen ovale was found in four cases. Hemodynamic instability requiring vasoactive drugs was recorded in four patients. A severe form of acute respiratory distress syndrome (ARDS) occurred in five cases, with the evidence of hemorrhagic alveolitis in three of them. In the literature review, eighteen cases were examined. Most cases refer to adolescents (median age 17.0 years). More than half of patients experienced two or more long bone fractures (median: 2 fractures). Both respiratory and neurological impairment were common (77.8% and 83.3%, respectively). 88.9% of patients underwent invasive mechanical ventilation and 33.3% of them required vasoactive drugs support. Neurological sequelae were reported in 22.2% of patients.
Conclusion: Post-traumatic FES is an uncommon multi-faceted condition even in pediatric trauma patients, requiring a high level of suspicion. Prognosis of patients who receive prompt support in an intensive care setting is generally favorable.
What is Known: •Post-traumatic fat embolism syndrome is a severe condition complicating long bone or pelvic fractures. •Little is known about clinical features and management in pediatric age. | |
What is New: •Post-traumatic fat embolism syndrome can cause multiple organ failure, often requiring an intensive care management. •Prompt supportive care contributes to a favorable prognosis. |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Post-traumatic fat embolism syndrome (FES) represents a severe complication which mostly involves patients suffering from long bone or pelvic fractures. Respiratory insufficiency, neurologic changes, and a skin petechial rash (within 72 h from trauma) are typical signs, but fever, tachycardia, retinal artery occlusion, jaundice, hematuria, and oliguria may also occur. Even though several diagnostic criteria have been proposed in order to aid in the diagnosis [1,2,3], this medical condition still poses a major diagnostic challenge for most clinicians. The most commonly used diagnostic tool is those proposed by Gurd [1], which includes three major and minor criteria; diagnosis of FES is made by the presence of at least two major, or one major and four minor criteria. More recently, Schonfeld suggested a semi-quantitative means for diagnosis of FES, based on seven clinical variables [2]: according to this index, a score above 5 is indicative of FES (Table 1). Since a specific diagnostic tool for pediatrics has not yet been developed, the above descripted criteria are commonly used in clinical practice ever for patients under 18 years old.
Besides primary embolization from initial trauma, orthopedic surgery involving manipulation of intramedullary canal, such as nail placement, may result in additional fat embolism. Indeed, its prevalence appears to increase in bilateral femoral fractures and after intramedullary nail fixation [4]. When a multisystemic involvement is present, the overall syndrome’s mortality can reach 10–20%, as reported in historical series [5], though decreasing with modern intensive care availability. Post-traumatic FES is reported among adult patients with a prevalence of 1–2%, while it is relatively uncommon also in high-volume pediatric trauma centers [6], where adolescents are referred, so that a deep investigation about the clinical course and management of post-traumatic FES in pediatric intensive care unit (PICU) is not reported in literature. A possible explanation could be found, apart from the higher cellularity in childhood, in the different composition of children’s fat marrow, which contains less olein and more palmitin and stearin [7].
Literature reports regarding the clinical management of post-traumatic FES in pediatrics are limited to single experiences depicted in case reports or as a part of larger series including adult patients. In this paper, we discuss eight episodes of post-traumatic FES occurring in seven patients admitted to our PICU over an 8-year period. Moreover, by reviewing the recent literature about this topic, we highlight clinical features, diagnostic workout, in-hospital course, and outcome of children affected by post-traumatic FES, with the aim to define its potential to result in life-threatening complications.
Materials and methods
This single-center retrospective cohort study was approved by the local Institutional Review Board (Prot. 30,870/19) on September 12, 2019. The need for individual informed consent was waived due to retrospective nature of the study. The study was carried out according to institutional and Good Clinical Practice (GCP) guidelines. Results of the retrospective analysis are reported in accordance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement, while the systematic review was designed according to the PRISMA (preferred reporting items for systematic reviews and meta-analyses) procedure.
A retrospective review of our institutional PICU trauma registry was performed. An 8-year period (2013–2020) was considered, during which 642 patients, aged from 0 to 18 years, had been admitted to the PICU with a diagnosis of trauma. After clinical suspicion of FES had been raised, the diagnosis was confirmed by referring to Gurd’s criteria [1] and Schonfeld’s fat embolism index [2] and ruling out possible alternative diagnoses by lung and brain imaging. Accordingly to Gurd’s criteria, in patients admitted in PICU after trauma, diagnosis of fat embolism was made by the presence of at least two out of three major signs, including neurologic abnormalities, respiratory insufficiency and skin petechial rash, or, alternatively, by the presence of one major and at least four minor criteria, and the absence of an alternative explanation [8]. Data recorded from chart review include demographic information, type of fracture, time from injury to symptoms onset, clinical signs, neurological status (through Glasgow coma score), laboratory and imaging findings, and outcome. Moreover, information about respiratory failure (level of hypoxemia, type and length of mechanical ventilation, presence of hemorrhagic alveolitis) was reported. In addition, a systematic research of the literature reporting post-traumatic fat embolism in PubMed database in the last 20 years (2002–2022) was conducted: the search terms were “fat embolism”, “fat embolism AND child”, and “fat embolism AND adolescent”, and the results were filtered by age (birth–18 years). All the studies which provided a partial or complete clinical description of post-traumatic FES were included in the review. Only studies involving patients without comorbidities were included in the analysis. Data collected from the review included age, sex, number of long bone fractures, time of onset of symptoms, onset before or after surgery, worst Glasgow coma scale (GCS), worst PaO2/FiO2, brain and chest imaging, use of vasoactive drugs, Gurd’s criteria, presence of patent foramen ovale, PICU length of stay, days of mechanical ventilation, need for tracheostomy, use of additional treatments beyond vital function support and neurological outcome through the cerebral performance category (CPC) score. In case some data were missing, they were coded as “NR” (not reported).
Data were collected and analyzed using a Microsoft Excel 2016 spreadsheet (Microsoft Corporation, Redmond, USA). Median and interquartile range (IR) were given for metric variables, while frequencies and percentages were given for non-metric variables. The study was approved by the local Ethical Committee.
Results
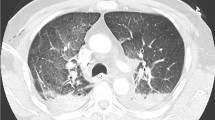
Patients’ clinical characteristics, radiological findings, therapeutic approach, and clinical course in PICU, including neurological and cardiovascular complications, are depicted in Fig. 1 and Table 2, while a focus on respiratory features and management is reported in Table 3. Family history was unremarkable for all patients.
Median age of the seven patients was 16.0 years (IQR 16.0–17.5). Median time of symptoms onset was 24 h (IQR 19–24 h) and median GCS at presentation was 11 (IQR 7.75–15). FES occurred after surgery in patient #1, who underwent intramedullary nail fixation of humeral fracture and external fixation for the other fractures, and in patient #7, who underwent intramedullary nail fixation for ulnar and femoral fractures. All the other patients underwent close fracture reduction and developed FES before surgery. After fat embolism had occurred, first step of surgery always consisted in external fixation. All patients were considered at high risk for venous thromboembolism and received appropriate DVT prophylaxis. Lower extremity venous echo color Doppler scan was performed in all patients within the first 24 h after FES diagnosis, resulting always negative. Vasoactive drugs were required in four out of eight episodes (50.0%). Six episodes (75.0%) were characterized by the occurrence of an acute respiratory distress syndrome (ARDS), according to the Berlin definition [9]: in these patients, the minimum PaO2/FiO2 had a median value of 83 (IQR 76.5–94.75), and the median duration of mechanical ventilation was 170 h (IQR 168–192 h) (Table 3). Seven out of eight teenagers (87.5%) had a favorable outcome while, in one patient, a severe neurological deficit (i.e., decerebrate posturing and dysautonomia) persisted 1 month after trauma.
As a second step, 152 articles were screened, and a total of 18 research studies, describing 19 clinical episodes of fat embolization, were identified and included in the review (Table 4) [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27]. All episodes but one occurred in adolescents (median age 17.0 years, male 55.6%) and symptoms consistent with FES appeared on median 18 h after trauma. Most patients presented neurological (n = 14, 77.8%) and/or respiratory (n = 15, 83.3%) involvement, as found on cerebral and/or chest imaging, whereas other symptoms were less common. Use of vasoactive drugs was reported in six out of eighteen cases (33.3%). More than half of patients experienced two or more long bone fractures (median: 2 fractures). In reports in which a patent foramen ovale was actively sought, it was found in 16.7% of cases. Additional/unusual treatments were reported in 38.9% of the clinical experiences: in particular, statins and inhaled nitric oxide were used in three cases, while one patient required cardiopulmonary resuscitation, another one underwent decompressive craniectomy and the only infant of the series underwent high-frequency oscillatory ventilation and continuous renal replacement treatment. Invasive mechanical ventilation was often necessary (median length: 14 days; reported in 10 out of 18 studies) and tracheostomy was performed in four patients (22.2%). No fatalities were evidenced in the review. Fourteen patients were discharged with a good cerebral performance, while a severe cerebral disability remained in one patient.
Discussion
The release of fat globules into the peripheral circulation is a known complication of blunt force injuries, especially acting on pelvic or long bone fractures [28]. Two theories are postulated for the occurrence of FES. The mechanical theory states that elevation of intramedullary pressure due to trauma facilitates the release of large fat droplets into the venous system [29]; consequently, fat globules can reach the pulmonary vessels and, through arteriovenous shunts or a patent foramen ovale, pass into the systemic circulation, thus producing systemic effects on end-organs, such as brain, skin or kidneys. This theory provides a good explanation for the onset of complications such as hypoxia (due to ventilation-perfusion mismatch) and transient pulmonary hypertension [30]. According to the biochemical theory, fat globules migrating in capillary bed release free fatty acids and glycerol, which initiate an inflammatory response leading to altered microcirculation with increased vascular permeability, local ischemia, and hemorrhage [31, 32]. This theory may account for non-traumatic cases of FES, as well as the variable delay between fat release and onset of symptoms. Actually, the temporal presentation of symptoms has a bimodal distribution, with an early onset usually within 12 h and a late onset between 24 and 72 h after injury [5]. The same patient can experience relapsing symptoms after early-onset FES, as occurred in our patient #2, as well as in the case reported by Whalen et al. [16]
The presence of fat embolism is common in pediatric autoptic observations [6]; however, only a small number of patients admitted to PICUs/pediatric trauma centers after major trauma experiences the typical symptoms of post-traumatic FES, so that a description of the clinical course of these patients is limited to single case reports or as a part of larger series including mostly adult patients. The discrepancy between autoptic and clinical findings could be explained by the fact that the passage of fat globules into the systemic circulation, although frequent, does not usually produce clinical changes; moreover, the true incidence of post-traumatic FES could be underestimated in more severely injured children.
Although the criteria proposed by Gurd may help in diagnosis [8], FES often represents a major diagnostic challenge to most clinicians. Besides traditional clinical signs, cytological examination of broncho-alveolar lavage may be useful to strengthen the clinical suspect when the diagnosis is not clear [33, 34]. In addition, an elevated serum interleukin-6 level may be useful as an early marker of FES in patients with isolated skeletal trauma, combined to the commonly altered laboratory findings [35].
In our series, a femoral fracture was always present, whereas the time gap between the injury and the clinical syndrome was usually between 18 and 24 h. Neurological impairment was evidenced in five out of eight episodes, having a delayed recovery in two cases and an unfavorable neurological outcome for one of them: in these patients, brain magnetic resonance imaging (MRI) showed the typical “starfield” pattern determined by multiple ischemic foci, while brain CT scan remained persistently normal. Brain damage may progress to severe cerebral edema, leading to rapid deterioration and requiring a surgical treatment [11, 36]. The incidence of patent foramen ovale is known to be higher in younger people [37, 38]. This may allow larger fat globules to pass to the systemic circulation and potentially cause more frequent and/or severe neurologic symptoms in pediatric and adolescent patients. Brain involvement may worsen the prognosis of post-traumatic FES; clinical findings vary from confusion to encephalopathy with coma and seizures [39]: in our report, four out of seven patients sustained cerebral fat embolism, with typical CT or MRI findings. Transient deficits were observed, while long-term neurological impairment was less common.
The etiology of FES is likely secondary to a combination of the mechanical and biochemical pathways. The presence or the reopening of a patent foramen ovale with right-to-left shunt due to pulmonary hypertensionmay be associated with an increased risk for FES-related systemic manifestations, due to larger fat globules, though several studies failed to demonstrate any intracardiac shunts [40]. However, fat globules ranging from 7 to 10 μm in diameter have been documented to cross the pulmonary vasculature [41].
Respiratory distress has long been recognized as an essential feature of post-traumatic FES: pulmonary involvement can occur in up to 92–95% of cases, while hypoxemia is almost universally present. In our series, four out of seven patients developed a severe ARDS picture, while alveolar hemorrhage was evidenced in three patients. Hypoxemia can also be worsened by pleural effusions, lung contusion, and transfusion-related lung injury, all consistent with major trauma. Management of ARDS should follow current recommendations for ventilator setting, including low tidal volumes and individualized PEEP [42]. In case of refractory hypoxemia, several salvage strategies can be adopted. High-frequency oscillatory ventilation (HFOV) could be necessary, particularly when post-traumatic FES syndrome involves infants, as depicted in the case by Amigoni et al. [19]. Even inhaled nitric oxide represents a safe and feasible option in this condition, since it can improve the ventilation/perfusion mismatch by redistributing lung perfusion to well-aerated areas; moreover, it may offer a benefit for the prevention or treatment of pulmonary hypertension [43]. In patients with obstructive shock from massive pulmonary embolism, early introduction of vasoactive drugs is crucial; in this view, dobutamine is probably superior to norepinephrine in restoring right ventricle function [44]. While invasive ventilation is frequently needed due to both neurological impairment and associated chest injury, most authors agree on the clinical advantage of early weaning from invasive ventilation. Actually, in our series, four patients received NIV as a part of respiratory support. Tracheostomy is required in case of long-lasting neurological impairment.
To date, symptomatic and supportive therapy remains the main approach for post-traumatic FES, since a specific treatment has not been yet identified. Treatment of hypoxemia, adequate hemodynamic support a and prompt recognition of neurologic deterioration are fundamental therapeutic goals [5, 45]. Early immobilization, stabilization and fixation of long-bone fractures contribute to prevent the release of fat emboli [45, 46]. Systemic corticosteroids administration is suggested to be beneficial in preventing FES and hypoxia in patients with long-bone fractures, since these drugs can blunt the inflammatory response, although the quality of evidence is low [47,48,49]. The role of inhaled corticosteroids in the prophylaxis of post-traumatic FES is controversial [50, 51]. Statins may represent a promising treatment for fat embolism: their main effect lies in the reduction of cholesterol synthesis in the liver by inhibition of HMG-CoA reductase; however, statins have pleiotropic effects, including modulation of inflammatory response and improvement of endothelial function, which have been observed even in short therapeutic courses and which could account for a beneficial effect in the acute management of FES [52, 53]. Albumin has shown therapeutic effects in experimental models of FES, likely due to its ability to bind free fatty acids, which are largely involved in the inflammatory cascade ultimately leading to lung injury [54]; still, benefits associated with its use in clinical practice are uncertain. Heparin is known to stimulate lipase activity and improve clearance of lipids from the bloodstream, but it also causes an increase in free fatty acids which could worsen tissue injury [55]. Moreover, its use can be considered unsafe, since some cases of post-traumatic FES can be complicated by alveolar hemorrhage, as reported in our series.
Conclusion
Post-traumatic FES is a rare condition in pediatrics. The wide spectrum of clinical manifestations — as depicted in the present series — of this uncommon multi-faceted condition requires a high level of suspicion. A delay in diagnosis should be avoided, since the outcome of patients with post-traumatic FES who promptly receive appropriate supportive care is generally favorable. These patients should be managed in a tertiary referral center with the required expertise and high-volume flow of critically ill trauma patients.
Data availability
The data that support the findings of this study are available from the corresponding author, [EP], upon request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- CPC:
-
Cerebral performance category
- CT:
-
Computerized thomography
- FES:
-
Fat embolism syndrome
- GCS:
-
Glasgow coma scale
- HMG-CoA:
-
3-Hydroxy-3-methylglutaryl-coenzyme A
- MRI:
-
Magnetic resonance imaging
- PICU:
-
Pediatric intensive care unit
References
Gurd AR, Wilson RI (1974) The fat embolism syndrome. J Bone Joint Surg Br 56B:408–416
Schonfeld SA, Ploysongsang Y, DiLisio R, Crissman JD, Miller E, Hammerschmidt DE, Jacob HS (1983) Fat embolism prophylaxis with corticosteroids. A prospective study in high-risk patients. Ann Intern Med 99:438–443
Lindeque BG, Schoeman HS, Dommisse GF, Boeyens MC, Vlok AL (1987) Fat embolism and the fat embolism syndrome. A double-blind therapeutic study. J Bone Joint Surg Br 69:128–131
Kontakis GM, Tossounidis T, Weiss K, Pape HC, Giannoudis PV (2006) Fat embolism: special situations bilateral femoral fractures and pathologic femoral fractures. Injury 37(Suppl 4):S19-24
Bulger EM, Smith DG, Maier RV, Jurkovich GJ (1997) Fat embolism syndrome. A 10-year review. Arch Surg 132:435–439
Eriksson EA, Rickey J, Leon SM, Minshall CT, Fakhry SM, Schandl CA (2015) Fat embolism in pediatric patients: an autopsy evaluation of incidence and etiology. J Crit Care 30(221):e221-225
Papagelopoulos PJ, Apostolou CD, Karachalios TS, Themistocleous GS, Giannakopoulos CK, Ioannidis TT (2003) Pulmonary fat embolism after total hip and total knee arthroplasty. Orthopedics 26:523–527; quiz 528–529
Gupta A, Reilly CS (2007) Fat embolism. Contin Educ Anaesth Crit Care Pain 7:148–151. https://doi.org/10.1093/bjaceaccp/mkm027
Force ADT, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS (2012) Acute respiratory distress syndrome: the Berlin Definition. JAMA 307:2526–2533
Ostlie A, Gilbert M, Lewis C, Ostlie D, Hargis-Villanueva A (2022) Fat embolism syndrome with neurological involvement: a case report. Trauma Case Rep 38:100607
Millen JA, Watson C, Cain JM, Hagan J, Richards WT, Taylor D, Ang D, Clark JM (2021) An early case of fat embolism syndrome occurring following polytrauma. Am Surg 87:86–88
O’Neill DC, Dekeyser GJ, Mortensen AJ, Makarewich CA (2021) Adolescent fat embolism syndrome after closed tibial shaft fracture: treatment with emergent external fixation. Case Rep Orthop 2021:5585085
Huffman JS, Humston C, Tobias J (2020) Fat embolism syndrome revisited: a case report and review of literature, with new recommendations for the anesthetized patient. AANA J 88:222–228
Aggarwal R, Banerjee A, Soni KD, Kumar A, Trikha A (2019) Clinical characteristics and management of patients with fat embolism syndrome in level I Apex Trauma Centre. Chin J Traumatol 22:172–176
Moliere S, Kremer S, Bierry G (2018) Case 254: posttraumatic migrating fat embolus causing fat emboli syndrome. Radiology 287:1073–1080
Whalen LD, Khot SP, Standage SW (2014) High-dose rosuvastatin treatment for multifocal stroke in trauma-induced cerebral fat embolism syndrome: a case report. Pediatr Neurol 51:410–413
Nawaf CB, Kelly DM, Warner WC Jr, Beaty JH, Rhodes L, Sawyer JR (2012) Fat embolism syndrome in an adolescent before surgical treatment of an isolated closed tibial shaft fracture. Am J Orthop (Belle Mead NJ) 41:565–568
Honda S, Inatomi Y, Yonehara T, Hashimoto Y, Hirano T, Uchino M (2010) A case report of serial MRI findings of cerebral fat embolism. Rinsho Shinkeigaku 50:566–571
Amigoni A, Corner P, Zanella F, Pettenazzo A (2010) Successful use of inhaled nitric oxide in a child with fat embolism syndrome. J Trauma 68:E80-82
Hufner K, Holtmannspotter M, Burkle H, Schaller UC, Ebert AD, Trentzsch H, Pfister HW, Lucking CB (2008) Fat embolism syndrome as a neurologic emergency. Arch Neurol 65:1124–1125
Meyer N, Pennington WT, Dewitt D, Schmeling GJ (2007) Isolated cerebral fat emboli syndrome in multiply injured patients: a review of three cases and the literature. J Trauma 63:1395–1402
Ozyurt Y, Erkal H, Ozay K, Arikan Z (2006) Traumatic fat embolism syndrome: a case report. Ulus Travma Acil Cerrahi Derg 12:254–257
Butteriss DJ, Mahad D, Soh C, Walls T, Weir D, Birchall D (2006) Reversible cytotoxic cerebral edema in cerebral fat embolism. AJNR Am J Neuroradiol 27:620–623
Van den Brande FG, Hellemans S, De Schepper A, De Paep R, Op De Beeck B, De Raeve HR, Jorens PG (2006) Post-traumatic severe fat embolism syndrome with uncommon CT findings. Anaesth Intensive Care 34:102–106
Nastanski F, Gordon WI, Lekawa ME (2005) Posttraumatic paradoxical fat embolism to the brain: a case report. J Trauma 58:372–374
Malagari K, Economopoulos N, Stoupis C, Daniil Z, Papiris S, Muller NL, Kelekis D (2003) High-resolution CT findings in mild pulmonary fat embolism. Chest 123:1196–1201
Forteza AM, Rabinstein A, Koch S, Zych G, Chandar J, Romano JG, Bustillo IC (2002) Endovascular closure of a patent foramen ovale in the fat embolism syndrome: changes in the embolic patterns as detected by transcranial Doppler. Arch Neurol 59:455–459
Rothberg DL, Makarewich CA (2019) Fat embolism and fat embolism syndrome. J Am Acad Orthop Surg 27:e346–e355
Hulman G (1995) The pathogenesis of fat embolism. J Pathol 176:3–9
Newbigin K, Souza CA, Torres C, Marchiori E, Gupta A, Inacio J, Armstrong M, Pena E (2016) Fat embolism syndrome: state-of-the-art review focused on pulmonary imaging findings. Respir Med 113:93–100
Nixon JR, Brock-Utne JG (1978) Free fatty acid and arterial oxygen changes following major injury: a correlation between hypoxemia and increased free fatty acid levels. J Trauma Acute Care Surg 18:23–26
Parker FB Jr, Wax SD, Kusajima K, Webb WR (1974) Hemodynamic and pathological findings in experimental fat embolism. Arch Surg 108:70–74
Trisolini R, Cancellieri A, Giovannitti A, Paioli D, Patelli M (2010) Fat embolism may be responsible for hypoxemia in trauma patients with no radiological pulmonary abnormalities. J Trauma 68:E53-54
Mimoz O, Edouard A, Beydon L, Quillard J, Verra F, Fleury J, Bonnet F, Samii K (1995) Contribution of bronchoalveolar lavage to the diagnosis of posttraumatic pulmonary fat embolism. Intensive Care Med 21:973–980
Prakash S, Sen RK, Tripathy SK, Sen IM, Sharma RR, Sharma S (2013) Role of interleukin-6 as an early marker of fat embolism syndrome: a clinical study. Clin Orthop Relat Res 471:2340–2346
Morales-Vidal SG (2019) Neurologic complications of fat embolism syndrome. Curr Neurol Neurosci Rep 19:14
Hagen PT, Scholz DG, Edwards WD (1984) Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc 59:17–20
Koutroulou I, Tsivgoulis G, Tsalikakis D, Karacostas D, Grigoriadis N, Karapanayiotides T (2020) Epidemiology of patent foramen ovale in general population and in stroke patients: a narrative review. Front Neurol 11:281
Jacobson DM, Terrence CF, Reinmuth OM (1986) The neurologic manifestations of fat embolism. Neurology 36:847–851
Pell AC, Hughes D, Keating J, Christie J, Busuttil A, Sutherland GR (1993) Brief report: fulminating fat embolism syndrome caused by paradoxical embolism through a patent foramen ovale. N Engl J Med 329:926–929
Nikolic S, Zivkovic V, Babic D, Djonic D, Djuric M (2012) Systemic fat embolism and the patent foramen ovale–a prospective autopsy study. Injury 43:608–612
The Pediatric Acute Lung Injury Consensus Conference G (2015) Pediatric acute respiratory distress syndrome: consensus recommendations from the pediatric acute lung injury consensus conference. Pediatr Criti Care Med 16:428–439
Adhikari NK, Burns KE, Friedrich JO, Granton JT, Cook DJ, Meade MO (2007) Effect of nitric oxide on oxygenation and mortality in acute lung injury: systematic review and meta-analysis. BMJ 334:779
Zamanian RT, Haddad F, Doyle RL, Weinacker AB (2007) Management strategies for patients with pulmonary hypertension in the intensive care unit. Crit Care Med 35:2037–2050
Shaikh N (2009) Emergency management of fat embolism syndrome. J Emerg Trauma Shock 2:29–33
Robert JH, Hoffmeyer P, Broquet PE, Cerutti P, Vasey H (1993) Fat embolism syndrome. Orthop Rev 22:567–571
Silva DF, Carmona CV, Calderan TR, Fraga GP, Nascimento B, Rizoli S (2013) The use of corticosteroid for the prophylaxis of fat embolism syndrome in patients with long bone fracture. Rev Col Bras Cir 40:423–426
Bederman SS, Bhandari M, McKee MD, Schemitsch EH (2009) Do corticosteroids reduce the risk of fat embolism syndrome in patients with long-bone fractures? A meta-analysis. Can J Surg 52:386–393
Habashi NM, Andrews PL, Scalea TM (2006) Therapeutic aspects of fat embolism syndrome. Injury 37(Suppl 4):S68-73
Agarwal AK, Sen R, Tripathy SK, Aggarwal S, NirmalrajGupta GD (2015) Is there any role of inhalational corticosteroids in the prophylaxis of post-traumatic fat embolism syndrome? Cureus 7:e332
Sen RK, Prakash S, Tripathy SK, Agarwal A, Sen IM (2017) Inhalational ciclesonide found beneficial in prevention of fat embolism syndrome and improvement of hypoxia in isolated skeletal trauma victims. Eur J Trauma Emerg Surg 43:313–318
Thongtang N, Ai M, Otokozawa S, Himbergen TV, Asztalos BF, Nakajima K, Stein E, Jones PH, Schaefer EJ (2011) Effects of maximal atorvastatin and rosuvastatin treatment on markers of glucose homeostasis and inflammation. Am J Cardiol 107:387–392
Taqueti VR, Ridker PM (2017) Lipid-lowering and anti-inflammatory benefits of statin therapy: more than meets the plaque. Circ Cardiovasc Imaging 10
Agnantis N, Gyras M, Tserkezoglou A, Apostolikas N, Papacharalampous N (1988) Therapeutic effect of bovine albumin in the experimental fat embolism syndrome. Respiration 53:50–57
Mellor A, Soni N (2001) Fat embolism. Anaesthesia 56:145–154
Author information
Authors and Affiliations
Contributions
Marco Piastra conceived the study, collected, and interpreted the case series data and performed the statistical analysis. Enzo Picconi contributed to data collection, gave important contribute to paper preparation, and drafted the manuscript. Tony Christian Morena and Vittoria Ferrari were involved in manuscript preparation. Camilla Gelormini and Anselmo Caricato were responsible for patient care and contributed to data collection. Daniele De Luca, Federico Visconti, and Giorgio Conti contributed important intellectual content to the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the institutional review board (Prot. 30870/19) on September 12, 2019, at Fondazione Policlinico Universitario “A. Gemelli” IRCCS – Rome, Italy.
Consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Piet Leroy.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Piastra, M., Picconi, E., Morena, T.C. et al. Multisystemic involvement of post-traumatic fat embolism at a Pediatric Trauma Center: a clinical series and literature review. Eur J Pediatr 182, 1811–1821 (2023). https://doi.org/10.1007/s00431-023-04869-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04869-6