Abstract
The objectives of this prospective case-control study were to determine liver stiffness (LSM) by transient elastography (TE) in children with newly diagnosed chronic liver disease (CLD) and to find out normal values in healthy Indian children. Two groups (A: 50 CLD who underwent liver biopsy and B: 50 healthy) aged 5–18 years were recruited prospectively. Liver biopsies were scored as per Metavir scoring and compared with TE. The median age of 100 recruited children was 13.6 years. In group B, normal LSM was 4.9 (2.5–7.3) kPa with significantly higher LSM in adolescent males (5.6 (4.1–7.3) kPa) as compared with females (4.3 (3.7–4.9) kPa), p = 0.001. In group A, TE was excellent in discriminating significant fibrosis (≥ F2) (P = 0.001) at a cut-off value of 10.6 kPa with area under receiver operating characteristic curve of 0.96. Metavir fibrosis stage (β = 0.611; R2 = 0.586) and age (β = 0.230; R2 = 0.586) were independent variables associated with higher LSM in stepwise multiple logistic regression analysis.
Conclusions: TE is an excellent non-invasive tool to assess significant liver fibrosis and can be used as an alternative to liver biopsy. Normative value of TE in adolescent males is higher than in females.
What is Known: • Transient elastography is a good non-invasive test for liver fibrosis assessment. • Normal liver stiffness depends on race, gender, and age. | |
What is New: • This is the first study from India to show the normative data of transient elastography in healthy Indian children. • We have documented that liver stiffness measurement by fibroscan in treatment naïve chronic liver disease has excellent correlation in significant fibrosis, severe fibrosis, and cirrhosis. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver fibrosis is the result of dynamic reaction of a healthy liver towards chronic cell injury [1]. It is observed in a large proportion of children with chronic liver disease (CLD) regardless of its etiology [2]. Early treatment of the underlying disease may limit or even reverse the progression of fibrosis; hence, early detection of fibrosis is crucial for timely treatment [3]. Currently, liver biopsy is the accepted gold standard for evaluating the fibrosis in liver disease; however, it is limited by its invasive nature with inherent risk of serious complications and sampling error and often it is not possible to get a liver biopsy due to coagulopathy and/or thrombocytopenia [4, 5]. Moreover, due to its invasive nature, repeated liver biopsies to assess the progression of liver disease are practically impossible. Transient elastography (TE) is a non-invasive, rapid, painless, and reproducible tool for assessment of liver fibrosis. It has the potential to reduce or replace the need of liver biopsy for assessment of the progression of liver disease in children. The utility of TE has been documented in several studies in adults [6,7,8,9,10]. A number of studies in children [11,12,13,14,15,16,17,18,19] have addressed the feasibility of TE in healthy children and its utility in chronic liver disease; however, there is scarcity of studies in children from developing countries. The aim of this study was to evaluate the utility and accuracy of liver stiffness measurement (LSM) by TE in children with newly diagnosed CLD and also to determine normative values of LSM in healthy Indian children.
Materials and methods
This case-control prospective study was conducted between May 2014 and May 2016 in the Department of Pediatric Gastroenterology of Sanjay Gandhi Post Graduate Institute Medical Sciences, Lucknow, India. Two groups (group A and group B) of children aged 5 to 18 years were enrolled after obtaining informed written consent from either parent. Group A was comprised of consecutive children with CLD who underwent liver biopsy during the study period. CLD was diagnosed on the basis of history, physical examination, biochemical parameters, Doppler ultrasonography findings such as nodular liver with portosystemic collaterals, dilated portal vein, and/or esophagogastroduodenoscopy (EGD) showing esophageal varices (grade II or more). Group B was comprised of healthy age- and sex-matched children (healthy siblings of either admitted CLD cases or children of hospital employees). At the time of recruitment, data related to detailed clinical history and physical examination findings including anthropometry of all children were recorded. In group B, siblings of admitted CLD cases were subjected to liver function tests, prothrombin time, complete blood counts, HBsAg, Kayser Fleischer ring, serum ceruloplasmin, 24-h urine copper, etc. depending upon the diagnosis of admitted CLD proband. However, due to ethical issues, healthy children of hospital employees did not go for any blood investigations. Children in group A underwent liver function tests, prothrombin time, hemogram, abdominal Doppler ultrasonography, EGD, and if required, ANA/LKM/SMA antibody, serum IgG level, HBsAg (if necessary HBV DNA, HBe, anti HBe), anti HCV (if necessary genotyping, quantitative HCV RNA), Kayser Fleischer ring, serum ceruloplasmin, 24-h urine copper, and percutaneous liver biopsy. Transjugular liver biopsy was done in children with coagulopathy and/or thrombocytopenia. The etiology of CLD was determined as per standard criteria [20,21,22,23,24]. The severity of liver disease was assessed by the Child–Turcotte–Pugh (CTP) score for all ages, model for end-stage liver disease (MELD) in children ≥ 12 years of age, and pediatric end-stage liver disease (PELD) in children of less than 12 years of age. In group A, children with more than minimal ascites (uncontrolled on salt restriction, diuretics, and paracentesis) and obesity (BMI z score > 2) were excluded. In group B, children with growth failure (weight and height z score < − 2), obesity (BMI z score > 2), pallor (which indicates malnutrition and/or underlying chronic disease), any suspicious of systemic illness, or liver disease (on the basis of detailed history and clinical examination) were excluded.
Transient elastography
TE was performed by a single experienced technician who was blinded of histopathological findings. It was done in children of both groups after 4 h of fasting. In group A, TE was performed without any sedative medication after adequate control of ascites by salt restriction, diuretic, or paracentesis whenever needed. However, mild ascites in dependent position was not a contraindication as it did not interfere with TE [25]. TE was performed by using fibroscan touch 502 France version, in dorsal decubitus position with right arm in maximal abduction using the right lobe of the liver through the intercostal space at the site of biopsy. S2 probe was used for chest circumference 45–75 cm and M probe for chest circumference above 75 cm. Ten-millimeter diameter core of tissue with a depth between 20 and 40 mm from skin surface was measured. Ten shots within 3–5 min were performed (at least 60% valid shots). The median liver stiffness measured by shots represents LSM. Ratio of interquartile range (range in which 50% of all shots, IQR) to LSM < 0.3 was taken as valid results.
Liver Biopsy
Liver biopsy was performed in all group A children either through percutaneous or transjugular route after sedation and local anesthesia. The liver biopsy specimen was fixed in formalin followed by paraffin embedding and sectioning with a microtome to 4 mm sections. Histopathology slides were stained with hematoxylin and eosin for routine diagnosis; however, for grading of fibrosis, reticulin/Masson’s trichrome stain was used. The fibrosis in liver histology was graded as per METAVIR scoring system and by a single histopathologist who was blinded to TE results [26]. Different stages of fibrosis as per METAVIR scoring system were F0 = no fibrosis, F1 = portal fibrosis without septa, F2 = portal fibrosis and few septa, F3 = numerous septa without cirrhosis, and F4 = cirrhosis. As per METAVIR scoring system, the different grades of inflammation were A0 = no activity, A1 = mild activity, A2 = moderate activity, and A3 = severe activity.
Statistical analysis
Data analysis was carried out by using SPSS software (version 15.0; SPSS Inc., Chicago, Illinois, USA). Continuous data was expressed as median and categorical data as number (percentage). Mann Whitney U test was used for comparison of continuous variables and Fisher’s exact test for categorical variables. Correlation was tested by Spearman test. A stepwise diagnostic performance of non-invasive methods was assessed by the area under the receiver operating characteristic (AUROC) curve analysis. The receiver operating characteristic (ROC) curve was used to determine the optimal cut-off values (optimal sensitivity and specificity simultaneously) for the presence of any/significant/severe fibrosis and cirrhosis. A p value of < 0.05 was taken as significant.
Results
A total of 100 children were recruited during the study period; 50 children each in group A (CLD) and group B (healthy controls). Clinical details of both groups are given in Table 1. Children in group A and group B were age and sex matched. Though the liver was palpable equally in both the groups, the size (palpable below costal margin) was significantly more in group A than that in group B. As expected, none of the children in group B had pallor, jaundice, ascites, and splenomegaly. Median LSM was significantly higher in group A than in group B.
Chronic liver disease children (group A, n = 50)
Transient elastography was done in all 50 children (31 boys) with CLD. The median duration of symptoms at diagnosis was 15.5 (range, 1–192) months. Etiology of chronic liver disease includes autoimmune hepatitis (AIH) (n = 18), immune tolerant phase of chronic hepatitis B = 15; chronic hepatitis C = 2; Wilson’s disease = 4, NAFLD = 3, and cryptogenic liver disease = 8. Baseline characteristics and LSM values of all children are shown in Table 1.
Liver histology
Liver biopsy was performed percutaneously in 38 children and via transjugular route in 12 children and none had any complications. In the histopathology, fibrosis was absent (F0) in 6 (12%), some degree of fibrosis (≥ F1) was evident in 44 (88%) (F1 = 13, F2 = 10, F3 = 15, F4 = 6). Grades of necroinflammation (activity) were A0 in 9, A1 in 11, A2 in 19, and A3 in 11.
Transient elastography in group A
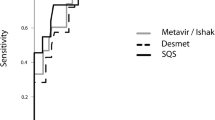
TE was performed successfully in all children; time taken was less than 5 min and without any complications. The comparisons between histological grading and TE results showed that TE is a moderate discriminator for any fibrosis (≥ F1) from no fibrosis (F0) with AUROC for TE was 0.76 (p = 0.04) and a cut-off value of 7.6 kPa (sensitivity 77.3%, specificity 66.7%) but good discriminator for significant fibrosis (≥ F2) from minimal/no fibrosis (< F2) with AUROC of 0.96 (p = 0.001) and a cut-off value of 10.6 kPa (sensitivity 90.3%, specificity 89.5%); for severe fibrosis (≥ F3), AUROC was 0.96 (p = 0.001) with a cut-off was 15.05 kPa (sensitivity 95.3%, specificity 89.7%) and lastly, for cirrhosis (F4) from no cirrhosis (< F4), AUROC was 0.88 (p = 0.001) with a cut-off was 21.8 kPa (sensitivity 83.3%, specificity 77.3%) (Fig. 1a–d). TE was not correlated with necroinflammatory activity in liver biopsies according to METAVIR scoring system (r = 0.167, p = 0.246). Stepwise multiple logistic regression analysis showed METAVIR fibrosis stage (β = 0.611; R2 = 0.586) and age (β = 0.230; R2 = 0.586) were the two independent variables associated with higher LSM.
Healthy children (group B, n = 50)
Out of 50 children, 26 were healthy siblings of CLD patients and the remaining 24 were healthy children of hospital employees. The success rate of TE in healthy children was 100%. The median LSM was 4.9 (range, 2.5–7.3) kPa with 5th centile was 3.1 kPa and 95th percentile is 7.2 kPa. Median LSM in boys were significantly higher (n = 31; 5.2 (range, 2.8–7.3) kPa) as compared with girls (n = 19; 4.3 (range, 2.5–7.1) kPa), p = 0.02. Children were divided into two age groups; young children (n = 26; between 5 and 11 years) and adolescents (n = 24; between 12 and18 years). There was no significant difference in LSM values between two age groups (4.4 (range, 2.5–7.3) vs. 5.1 (range, 3.7–7.3) kPa, p = 0.111, respectively). In adolescents (12–18 years) group, median LSM value in boys was significantly high (n = 17; 5.6 (range, 4.1–7.3) kPa) as compared with girls (n = 7; 4.3 (range, 3.7–4.9) kPa), p = 0.001 (Table 1). The 5th and 95th percentile of LSM (kPa) in both age groups are shown in Table 2.
Discussion
This is for the first time we have generated the normative data of LSM in Indian children between 5 and 18 years of age. In our study, LSM upper limit of normal (95th percentile) across all age groups of healthy children was 7.2 kPa which is higher than the value obtained by Engelman et al. from Germany, in a study of 240 healthy children (3.5 to 4.5 kPa in 0 to 18 years age groups) [16]. Difference in upper limit of normal of LSM and age-dependent increase in LSM might be explained by genetic makeup of regional population and environmental factors such as toxic insults which increases with age and it controls the accumulation of extracellular matrix in the liver. We also demonstrated significantly higher median LSM in boys compared with girls in the age group of 12 to18 years and this finding was similar to that of Engelman et al.’s study [16]. However, a study by Goldschimdt et al. from Germany [17] in 400 healthy children showed no difference in LSM value between adolescent boys and girls. Higher LSM in adolescent boys was supported by animal study showing inhibitory effect of ovarian hormones on extracellular matrix produced by liver stellate cells [28]. The success rate of LSM by TE depends on the age of the patient as younger age poses some difficulties. The reason for 100% success rate of TE in our study is mainly due to the fact that we have recruited children of 5 years or more. The failure rate between 4 and 27% has been documented in various studies [16, 17], when younger children were included. The strength of our study is that we enrolled a homogenous group of healthy controls after excluding the main confounding factors such as food, sedation, obesity, and systemic illness that could have been affected the LSM values [17, 18, 29, 30]. For the first time, we have generated normative TE value for healthy Indian children albeit in a smaller sample. We need further studies with larger number from different parts of the country to substantiate our observation. As the cut-offs derived from this study are based on our population, and no external validation was done, there is a possibility of overestimation of accuracy of the transient elastography. In group A (children with CLD), we have documented the cut-off value for LSM (kPa) by AUROC for significant fibrosis (10.6 kPa) and severe fibrosis (15.05 kPa) with good sensitivity and specificity (close to 90%). This result is similar to the study by de Ledinghen et al. [11] who showed the cut-off value of 10.2 kPa for significant fibrosis. On the contrary, Fitzpatrick et al. [14] showed cut-off value of 6.9 kPa and 7.5 kPa for significant and severe fibrosis respectively in CLD children and in a study of children with NAFLD; Nobili et al. [12] showed LSM value of 7.4 kPa and 10.2 kPa for significant and severe fibrosis, respectively. These differences in cut-off value for significant and severe fibrosis could be due to difference in etiology and severity of the liver disease. We have documented a positive correlation between TE and liver fibrosis assessed by histopathology. However, we could not document significant correlation between TE with histologically documented necroinflammation. This may be due to smaller sample size. Raizner et al. showed children with no/minimal hepatic fibrosis but having significant hepatic inflammation as depicted by high ALT values were associated with high LSM values that typically seen in advanced fibrosis but interpretation of serial LSM with serial liver function test in the absence of repeated liver biopsies might be misleading for the assessment of inflammatory effect on TE [15]. There is an unmet need of a larger study with patients having only inflammation and no fibrosis to document the effect of inflammation on LSM. Often it is not feasible to do repeated liver biopsies after first diagnostic biopsy in CLD patients to document progression. In this context, TE is a valuable tool in long-term follow-up and monitoring of CLD children as it detects the fibrosis progression or regression non-invasively. Patients with non-cirrhotic chronic hepatitis B would be benefited from non-invasive TE monitoring by early detection of significant fibrosis in follow-up especially in patients with normal transaminases or low viral load so that timely treatment can be started. Another important role of TE in monitoring of AIH children as they require longer duration of immunosuppression and early detection of progression or regression of fibrosis may be another parameter which might help in modification of immunosuppressive therapy. Though in this study we have done one-time TE, we have a plan to do serial TE especially in AIH group (the largest subset of CLD cases in our study) to document its utility in assessment of progression or regression of the disease. Further prospective studies are required for serial TE in children with chronic liver disease to assess the effect of treatment on TE. The limitations of our study are, firstly, we could not calculate the LSM cut-off for each disease because of small sample size in each etiology. Secondly, we could not completely negate the effect of inflammation in LSM estimation by TE despite the absence of correlation between necroinflammation and LSM, mainly due to small sample size. Third, we could not do serial TE to assess the progression of fibrosis in liver disease patients; lastly, we could not completely rule out the presence of liver disease in the subset of group B children in whom no laboratory tests were done due to ethical issues and the number of children in age- and gender-specific subgroups was small. In conclusion, the normative data of TE generated in this study for healthy Indian children (with 95th centile) can be used to differentiate various stages of fibrosis in chronic liver disease. It has got good sensitivity and specificity except when any fibrosis (≥ F1) is differentiated from no fibrosis (F0) where TE should be used cautiously because of its average sensitivity and specificity.
Change history
26 February 2020
The author regrets that one of the author’s name was incorrectly presented in the published version of this article. The third author’s name original read as “<Emphasis Type="Bold">Tajwar Singh Negi</Emphasis>” this should have been “<Emphasis Type="Bold">Tajwer Singh Negi</Emphasis>”.
Abbreviations
- AUROC:
-
Area under the receiver operating characteristic
- ANA:
-
Anti-nuclear antibody
- Anti HBe:
-
Antibody to hepatitis B e-antigen
- BMI:
-
Body mass index
- CLD:
-
Chronic liver disease
- CTP:
-
Child–Turcotte–Pugh
- EGD:
-
Esophagogastroduodenoscopy
- HBsAg:
-
Hepatitis B surface antigen
- HBeAg:
-
Hepatitis B e-antigen
- HBV-DNA:
-
Hepatitis B deoxyribonucleic acid
- HCV RNA:
-
Hepatitis C ribonucleic acid
- IQR:
-
Interquartile range
- LSM:
-
Liver stiffness measurement
- LKM:
-
Liver kidney microsomal antibody
- MELD:
-
Model for end-stage liver disease
- NAFLD:
-
Non-alcoholic fatty liver disease
- PELD:
-
Pediatric end-stage liver disease
- ROC:
-
Receiver operating characteristic
- SMA:
-
Anti-smooth muscle antibody
- TE:
-
Transient elastography
References
Sokol RJ (2002) Liver cell injury and fibrosis. J Pediatr Gastroenterol Nutr 35(1):S7–S10
Tanner MS (2002) Mechanisms of liver injury relevant to pediatric hepatology. Crit Rev Clin Lab Sci 39:1–61. https://doi.org/10.1080/10408360290795439
Sun Y, Zhou J, Wang L et al (2017 May) New classification of liver biopsy assessment for fibrosis in chronic hepatitis B patients before and after treatment. Hepatology. 65(5):1438–1450. https://doi.org/10.1002/hep.29009
Cadranel JF, Rufat P, Degos F (2000) Practices of liver biopsy in France: results of a prospective nationwide survey. For the Group of Epidemiology of the French Association for the Study of the liver (AFEF). Hepatology 32:477–481. https://doi.org/10.1053/jhep.2000.16602
Poniachik J, Bernstein DE, Reddy KR, Jeffers LJ, Coelho-Little ME, Civantos F, Schiff ER (1996) The role of laparoscopy in the diagnosis of cirrhosis. Gastrointest Endosc 43:568–571. https://doi.org/10.1016/s0016-5107(96)70192-x
CasteraL VJ, Foucher J, Le Bail B, Chanteloup E, Haaser M, Darriet M, Couzigou P, De Ledinghen V (2005) Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology 128:343–350. https://doi.org/10.1053/j.gastro.2004.11.018
Corpechot C, El Naggar A, Poujol-Robert A, Ziol M, Wendum D, Chazouillères O, de Lédinghen V, Dhumeaux D, Marcellin P, Beaugrand M, Poupon R (2006) Assessment of biliary fibrosis by transient elastography in patients with PBC and PSC. Hepatology 43:1118–1124. https://doi.org/10.1002/hep.21151
Foucher J, Chanteloup E, Vergniol J, Castéra L, Le Bail B, Adhoute X, Bertet J, Couzigou P, de Ledinghen V (2006) Diagnosis of cirrhosis by transient elastography (FibroScan): a prospective study. Gut 55:403–408. https://doi.org/10.1136/gut.2005.069153
Kazemi F, Kettaneh A, N’kontchou G, Pinto E, Ganne-Carrie N, Trinchet JC, Beaugrand M (2006) Liver stiffness measurement selects patients with cirrhosis at risk of bearing large oesophageal varices. J Hepatol 45:230–235. https://doi.org/10.1016/j.jhep.2006.04.006
Carrion JA, Navasa M, Bosch J, Bruguera M, Gilabert R, Forns X (2006) Transient elastography for diagnosis of advanced fibrosis and portal hypertension in patients with hepatitis C recurrence after liver transplantation. Liver Transpl 12:17918. https://doi.org/10.1002/lt.20857
deLedinghen V, Le Bail B, Rebouissoux L, Fournier C, Foucher J, Miette V, Castéra L, Sandrin L, Merrouche W, Lavrand F, Lamireau T (2007) Liver stiffness measurement in children using FibroScan: feasibility study and comparison with Fibrotest, aspartate transaminase to platelets ratio index, and liver biopsy. J Pediatr Gastroenterol Nutr 45:443–450. https://doi.org/10.1097/MPG.0b013e31812e56ff
Nobili V, Vizzutti F, Arena U, Abraldes JG, Marra F, Pietrobattista A, Fruhwirth R, Marcellini M, Pinzani M (2008) Accuracy and reproducibility of transient elastography for the diagnosis of fibrosis in pediatric nonalcoholic steatohepatitis. Hepatology 48:442–448. https://doi.org/10.1002/hep.22376
Alkhouri N, Sedki E, Alisi A, Lopez R, Pinzani M, Feldstein AE, Nobili V (2013) Combined pediatric NAFLD fibrosis index and transient elastography to predict clinically significant fibrosis in children with fatty liver disease. Liver Int 33:79–85. https://doi.org/10.1111/liv.12024
Fitzpatrick E, Quaglia A, Vimalesvaran S, Basso MS, Dhawan A (2013) Transient elastography is a useful noninvasive tool for the evaluation of fibrosis in pediatric chronic liver disease. J Pediatr Gastroenterol Nutr 56:72–76. https://doi.org/10.1097/MPG.0b013e31826f2760
Raizner A, Shillingford N, Mitchell PD, Harney S, Raza R, Serino J, Jonas MM, Lee CK (2017) Hepatic inflammation may influence liver stiffness measurements by transient elastography in children and young adults. J Pediatr GastroenterolNutr 64(4):512–517. https://doi.org/10.1097/MPG.0000000000001376
Engelmann G, Gebhardt C, Wenning D, Wühl E, Hoffmann GF, Selmi B, Grulich-Henn J, Schenk JP, Teufel U (2012) Feasibility study and control values of transient elastography in healthy children. Eur J Pediatr 171:353–360. https://doi.org/10.1007/s00431-011-1558-7
Goldschmidt I, Streckenbach C, Dingemann C, Pfister ED, di Nanni A, Zapf A, Baumann U (2013) Application and limitations of transient liver elastography in children. J Pediatr Gastroenterol Nutr 57:109–113. https://doi.org/10.1097/MPG.0b013e31829206a0
Lewindon PJ, Balouch F, Pereira TN, Puertolas-Lopez MV, Noble C, Wixey JA, Ramm GA (2016) Transient liver elastography in unsedated control children: impact of age and intercurrent illness. J Paediatr Child Health 52:637–642. https://doi.org/10.1111/jpc.13151
Lee CK, Mitchell PD, Raza R, Harney S, Wiggins SM, Jonas MM (2018) Validation of transient elastography cut points to assess advanced liver fibrosis in children and young adults: the Boston Children’s Hospital experience. J Pediatr 198:84–89.e2. https://doi.org/10.1016/j.jpeds.2018.02.062
Mileti E, Rosenthal P, Peters MG (2012) Validation and modification of simplified diagnostic criteria for autoimmune hepatitis in children. Clin Gastroenterol Hepatol 10:417–421. https://doi.org/10.1016/j.cgh.2011.11.030
Lok AS, McMahon BJ (2007) Chronic hepatitis B. Hepatology 45:507–539. https://doi.org/10.1002/hep.21513
Ghany MG, Strader DB, Thomas DL, Seeff LB, American Association for the study of Liver Disease (2009) Diagnosis, management andtreatment of hepatitis C: an update. Hepatology 49:1335–1374. https://doi.org/10.1002/hep.22759
Roberts EA, Schilsky ML (2008) Diagnosis and treatment of Wilson disease: an update. Hepatology 47:2089–2111. https://doi.org/10.1002/hep.22261
Valla DC (2003) The diagnosis and management of the Budd-Chiari syndrome: consensus and controversies. Hepatology 38:793–803. https://doi.org/10.1053/jhep.2003.50415
Foucher J, Castéra L, Bernard PH, Adhoute X, Laharie D, Bertet J, Couzigou P, de Lédinghen V (2006) Prevalence and factors associated with failure of liver stiffness measurement using FibroScan in a prospective study of 2114 examinations. Eur J Gastroenterol Hepatol 18:411–412
Bedossa P, Poynard T (1996) An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology 24:289–293. https://doi.org/10.1002/hep.510240201
Kalantri A, Karambelkar M, Joshi R, Kalantri S, Jajoo U (2010) Accuracy and reliability of pallor for detecting anaemia: a hospital-based diagnostic accuracy study. PLoS One 5(1):e8545. https://doi.org/10.1371/journal.pone.0008545
Yasuda M, Shimizu I, Shiba M, Ito S (1999) Suppressive effects of estradiol on dimethylnitrosamine-induced fibrosis of the liver in rats. Hepatology 29:719–727. https://doi.org/10.1002/hep.510290307
Mederacke I, Wursthorn K, Kirschner J, Rifai K, Manns MP, Wedemeyer H, Bahr MJ (2009) Food intake increases liverstiffness in patients with chronic or resolved hepatitis C virus infection. Liver Int 29:1500–1506. https://doi.org/10.1111/j.1478-3231.2009.02100.x
Cho Y, Tokuhara D, Morikawa H, Kuwae Y, Hayashi E, Hirose M, Hamazaki T, Tanaka A, Kawamura T, Kawada N, Shintaku H (2015) Transient elastography-based liver profiles in a hospital-based pediatric population in Japan. PLoS One 10:e0137239. https://doi.org/10.1371/journal.pone.0137239
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Vikas Jain, Ujjal Poddar, Negi TS, Vivek A Saraswat, Narendra Krishnani, Surender K Yachha, and Anshu Srivastav. The first draft of the manuscript was written by Vikas Jain and Ujjal Poddar. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. The study was conducted after obtaining clearance from the Institutional Ethics Committee (IEC code: 2014-83-DM-77). Informed written consent was obtained from either parent before doing all invasive procedures and TE. Informed consent: Informed written consent was obtained from either parent before doing all invasive procedures and transient elastography.
Additional information
Communicated by Peter de Winter
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The author regrets that one of the author’s name was incorrectly presented in the published version of this article. The third author’s name original read as “Tajwer Singh Negi”, this should have been “Tajwar Singh Negi”.
Rights and permissions
About this article
Cite this article
Jain, V., Poddar, U., Negi, T.S. et al. Utility and accuracy of transient elastography in determining liver fibrosis: a case-control study. Eur J Pediatr 179, 671–677 (2020). https://doi.org/10.1007/s00431-019-03561-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-019-03561-y