Abstract
Transient elastography (TE) is a new technique for the non-invasive assessment of liver fibrosis. The degree of fibrosis is equivalent to the liver stiffness measured in kilopascal (kPa). It is frequently used in adult patients with a mean normal stiffness of 4.4–5.5 kPa. Since 2008, liver stiffness can be measured even in small children and infants following the availability of a new probe with a smaller diameter (S-probe 5 mm) than the regular probe (M-probe 7 mm). We report control values for healthy children between 0 and 18 years and investigated the feasibility of this technique in a pediatric population. For control values, TE was performed in infants and children after exclusion of liver disease by medical history, clinical examination, blood investigation, and abdominal ultrasound. For feasibility analyses the results of all TE performed in our clinic were analyzed irrespective of the underlying disease. Liver stiffness was measured with the S-probe (thorax diameter <45 cm (S1) or 45–75 cm (S2)) and the M-probe (thorax diameter >75 cm) according to the manufacturer’s recommendations. A total of 240 healthy children were analyzed to establish control values. The median liver stiffness was 4.7 kPa resulting in an upper limit of normal of 6.47 kPa. Median values of stiffness were significantly age dependent with 4.40, 4.73, and 5.1 kPa in children 0–5, 6–11, and 12–18 years (p = 0.001) while the interquartile range decreased with age (0.8, 0.7, and 0.6 kPa). The resulting upper limit of normal (median plus 1.64 times standard deviation) was 5.96, 6.65, and 6.82 kPa. Girls between 11 and 18 years showed a significantly lower median stiffness than boys of the same age (4.7 vs. 5.6 kPa; p < 0.005). Feasibility was tested in 975 consecutive liver stiffness measurements (LSM) in children 0–18 years of age. Patients with invalid LSM were significantly younger than those with valid LSM (5.8 vs. 9.7 years, p < 0.0001), showed a significantly higher stiffness (10.2 vs. 6.17, p < 0.0001), and examinations took significantly longer (202 vs. 160 s, p < 0.0001). TE is technically possible in children of all age groups. The upper limit of normal increases significantly with age. Due to movement artifacts the measurement is reliable from the age of 6 without sedation. In younger children the number of invalid measurements increases significantly. Further studies are needed to asses the value of TE in the diagnosis and follow-up of liver disease in pediatric hepatology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver fibrosis is the result of dynamic reactions of a healthy liver towards chronic cell injury [31]. It can be observed in a large proportion of children with chronic liver disease, regardless of its cause [32]. Early treatment of the underlying disease may limit the progression of fibrosis. An early detection and treatment of fibrotic changes is important to avoid complications like portal hypertension with esophageal varices or ascites.
Aminotransferases poorly reflect the stage of liver fibrosis or cirrhosis. They may even be normal or only slightly elevated in fibrotic or cirrhotic livers. Biochemical markers of liver fibrosis (e.g., pediatric non-alcoholic fatty liver disease (NAFLD) fibrosis index or enhanced liver fibrosis test) in children with NAFLD [1, 24] could non-invasively predict liver fibrosis in more than 80% of NAFLD patients. Hyaluronic acid [25] and tissue inhibitory metalloproteinase type 1 [24] have also been tested as markers of fibrosis in children with NAFLD and reliably predict fibrosis in NAFLD patients. Data on non-invasive liver fibrosis tests in other pediatric diseases are scarce. The aspartate transaminase to platelets ratio index (APRI score) has been validated in children with varying liver diseases [15]. The negative predictive values of this test for fibrosis is 90% (APRI score <0.5) and for cirrhosis 100% for an APRI score of <1. Other non-invasive tests, like Forns score, with a better negative predictive value of 96% are not validated in children [17]. To date, the gold standard for diagnosis and follow-up of liver fibrosis or cirrhosis in infants and children is the histologic examination of a liver specimen obtained by percutaneous liver biopsy [20]. Liver biopsy is the method of choice in clarifying the etiology of hepatopathies. It has the advantage of obtaining direct information not only about the degree of fibrosis, but also about inflammation, necrosis, steatosis, and iron or copper deposits. But histopathologic examinations of a liver biopsy have limitations. Studies clearly indicate that liver biopsies are prone to sampling errors and may underestimate the amount of liver fibrosis. Cirrhosis could be missed on a single blind percutaneous liver biopsy in 10–30% of cases [19, 26]. In addition, it is a painful and invasive procedure making sedation in children necessary. Potentially life-threatening complications like bleeding [4, 6] are described. Therefore, it does not come first in the work-up of patients with suggested hepatopathy and is not a suitable technique for serial examinations of patients with known fibrosis.
In recent years, non-invasive methods for diagnosing liver-fibrosis have been developed. One of these new techniques is the transient elastography (TE). TE is a technique based on the measurement of the velocity of a shear wave that is induced to the liver by a mechanical probe. This velocity reflects the stiffness of the liver. Stiffness primarily depends on the amount of fibrotic tissue in the liver. Therefore, liver stiffness measurement (LSM) in kilopascal (kPa) is equivalent with fibrosis. The ability of TE to assess hepatic fibrosis when compared to the gold standard of liver biopsy was shown in large studies in adult patients and has been summarized in reviews and meta-analyses [7, 8, 14, 18, 29, 36, 37].
Median values of TE in healthy adult individuals vary between 4.4 and 5.5 [28, 30]. There is evidence that stiffness increases with male gender and body mass index (BMI) in adult patients and tends to increase with age without reaching significance [28, 34]. Since the introduction of TE, the limitations of this method have also become obvious. Extrahepatic factors like elevated blood or central venous pressure, ascites, and obesity influence LSM without influencing the degree of fibrosis [5, 9, 21, 22]. The introduction of a small TE probe, that is also suitable for the small intercostal space of young children and infants, has made TE possible in every age group. On the other hand, the technical limitation of invalid LSM due to moving and crying becomes more evident in these patients. The extent of this problem in a healthy pediatric population has not been assessed yet.
Within the first years of life the liver develops an increasing metabolic capacity. Therefore, the liver doubles its weight within the first 12 months and increases its weight by another 50% within the next 2 years. Therefore, we hypothesize that normal values from adult patients may not be suitable in young infants and children. Hitherto no control data from healthy children exist. A prospective study was performed aiming to define the upper limit of normal of the liver stiffness in healthy infants and children and to investigate the feasibility of this new technique in infants, children, and adolescents.
Methods
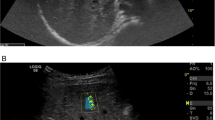
Study patients were recruited from regular referrals to our clinic. Informed consent to take part in the study was obtained. A detailed medical history concerning diagnoses, reason for referral, possible liver diseases, hepatotoxic drugs, corticosteroids, and liver injuries including liver surgery and a thorough clinical examination focusing on putative liver diseases were performed. The following anthropometric data were collected at the time of recruitment: age, gender, weight, and height. The body mass index (BMI), BMI standard deviation score (BMI-SDS), and SDS for height and weight were calculated. A fasting blood sample was drawn to measure alanine aminotransferase, aspartate aminotransferase (AST), γ-glutamyl-transpeptidase, total bilirubin, direct bilirubin, and thrombocytes. For non-invasive exclusion of fibrosis the APRI score [15, 33] was calculated. An abdominal ultrasound was performed (Sequoia™ 512, ACUSON, and Antares™ Siemens/Acuson). Liver echogenity, echotexture, and size in sternal line, medioclavicular line, and ventral axillary line were determined by an experienced pediatric radiologist. Ascites and portal vein occlusion were excluded by ultrasound. Frequent sonographical findings in liver cirrhosis [2] (homogeneously increased echogenicity, heterogeneously increased echogenicity and nodular liver) were sonographically determined.
For the normal value, only patients with normal liver enzymes, an APRI score below 0.5, BMI-SDS below 90th PC, a normal appearing liver on abdominal ultrasound, and patients without a history of hepatopathy were included. Patients with a history of recent medication with drugs affecting the liver (e.g., patients with a steroid therapy, azathioprine or MTX for Crohn’s disease, ulcerative colitis or juvenile rheumatoid arthritis, or patients after chemotherapy) and with diseases putatively affecting the liver (e.g., cystic fibrosis) were excluded.
For feasibility study, patients that fulfilled the inclusion criteria for the control group and patients that did not fulfill these criteria were analyzed.
Transient elastography (Fibroscan®, Echosense Paris, France) of the liver was performed by two experienced observers as previously described [29]. In brief a mechanical pulse of low amplitude and low frequency (50 Hz) is transcutaneously applied to the liver using a probe that contains an ultrasound transducer and a vibrator. It induces an elastic shear wave. The velocity of the shear wave in the liver is measured by ultrasound. Velocity of the wave and stiffness of the organ are proportionally related. Ten shots within 3 to 5 min were performed in each patient under standardized conditions. The software itself determined, whether a shot was valid or not. Sixty percent of all shots performed on the individual patient should be valid. The median stiffness measured by these shots represents the LSM. Measurements with a success rate of less than 60% valid shots were excluded from the analysis. The median stiffness and the interquartile range (IQR, the IQR expresses the range in which 50% of all shots are), expressed in kilopascal (range 2.5–75 kPa) were calculated automatically on a microcomputer installed in the Fibroscan®. If the IQR/LSM ratio was below 0.3 the LSM was called representative of the liver stiffness.
Two different probes were used for examination. They differed in terms of probe diameter (S < M), impulse power and measurement depth. Children with a thorax circumference of less than 75 cm were examined by the S-probe (5 MHz, diameter 5 mm) whereas children with a thorax circumference above 75 cm were measured by the M-probe (3.5 mHz, diameter 7 mm). The S-probe has two different modes. The S1 mode enables the observer to examine babies with a thorax circumference less than 45 cm. S2 mode is used in patients with a thorax circumference of 45–75 cm. The measurement depth is 25–65 mm with the M-probe and 15–40 mm and 20–50 mm with the S1- and S2-probe, respectively. Each patient was studied with only one probe, according to the manufactures recommendations.
LSM was performed with the patients in supine position with the right arm placed behind the head. The tip of the probe was covered with coupling gel and positioned on the skin in the seventh or eighth intercostal space at the front axillary line vertical to the xiphoid on the right hemi-thorax. The amount of pressure applied to the probe by the examiner is standardized by a visual indicator on the Fibroscan® itself. An ultrasound image (M mode) enables the examiner to orientate the probe above liver tissue. The located liver portion should be free of large vascular structures.
The study was performed in accordance with the principles of the Declaration of Helsinki and approval was obtained from the local ethics committee. (S-076/2008). All parents gave written informed consent for participation in the study.
Statistical analysis
SPSS 19.0 for windows (SPSS Inc. Chicago, IL, USA) was used for statistical analysis. All results are expressed as median if they were not normally distributed. The normality of data distribution was evaluated by the Shapiro–Wilks test. Descriptive statistics were performed by ANOVA followed by Student–Newman–Keuls’ test for multiple comparisons. Associations between individual parameters were evaluated by Pearson product–moment correlation analysis. Stepwise linear regression analysis was performed in order to identify independent predictors of stiffness.
The upper limit of normal or 95th percentile was defined as median stiffness values in kilopascal plus 1.64 times the standard deviation.
Age-specific reference values were established using the LMS method of Cole and Green [12]. The LMS method describes the distribution of a measurement Y by its median (M), the coefficient of variation (S), and a measure of skewness (L) required to transform the data to normality. Estimates for these parameters are obtained by applying a maximum-likelihood curve-fitting algorithm to the original data plotted over the independent variable of interest, in this case age. The resulting estimates of L, M, and S can be used to construct percentiles (C alpha (t)) by the equation:
where M(t), L(t), S(t), and C alpha (t) indicate the corresponding values of each parameter at age t. z alpha is the appropriate normal equivalent deviate (e.g., for alpha = 97%, z alpha = 1.88). This equation can be rearranged to convert an individual child’s liver stiffness value to an exact standard deviation score (SDS):
where Y is the child’s individual stiffness value, and L(t), M(t), and S(t) are the gender-specific values of L, M, and S interpolated for the child’s age.
Results
From September 2009 until March 2011 a total of 1,001 LSM were performed in 975 patients. All patients were of Caucasian origin. The examinations were performed by two experienced observers. If repeated LSM were done in the same patient, the first measurement that was performed was used for analyses.
Control values
In 259 children the medical history concerning liver diseases as well as abdominal examination were completely uneventful. Seventy-four of those came for medical check-up before minor ear, nose, and throat surgery. One hundred eighty-five patients either suffered from functional diseases (n = 129, functional abdominal pain, constipation, and headache) or minor infections (n = 56, upper airway infections, gastroenteritis, and urinary tract infections). They were not obese as defined by BMI-SDS < 90th PC. The liver appeared normal concerning structure and size (MCL < 90th PC) [16] on ultrasound, and the laboratory results and APRI score were all normal (Table 1). For the purpose of performing reliable normal values 19 patients (7%) had to be excluded because of invalid LSM. Ten of these patients (52%) were younger than 6 years while four were between 6 and 11 and five were over 12 years. LSM of the remaining 240 patients was used for calculation of normal values. Anthropometric and key laboratory data of these 240 patients are shown in Table 1. The patients were divided into three relevant age groups: preschool (n = 91; 0–5 years), school children (n = 78; 6–11 years), and adolescents/young adults (n = 71; 12–18 years). BMI-SDS and liver enzymes did not differ significantly between age groups (p > 0.1).
The male/female ratio of all patients was 1.1:1. The median age was 9.3 (female) and 7.9 years (male) and median BMI-SDS was 0.34 and 0.55, respectively. Patient data according BMI-SDS, liver enzymes, and thrombocytes were independent of gender (p > 0.1).
Eighty percent (n = 191) of LSM were performed with the S-probe (S1 mode, 15; S2 mode, 176) and 20% (n = 49) with the M-probe. The mean duration of the measurements was 209 and 162 s (S-probe, S1 and S2 mode) and 158 s with the M-probe (Table 2). We did not obtain results by using different probes in one patient. Therefore, the effect of different probes on the quality of LSM cannot be estimated.
The median liver stiffness of all patients was 4.70 kPa resulting in an upper limit of normal of 6.47 kPa. Age-specific reference values using the LMS method of Cole and Green are shown in Fig. 1. The curve shows a significant increase of liver stiffness in relationship to the age of the patient of around 0.06 kPa per year.
Liver stiffness in healthy children according to age; 5th to 95th percentile curves for liver stiffness in kilopascal. Percentile curves were derived by the LMS method [17] from measurements in 122 girls (triangles) and 118 boys (dots)
Median stiffness was 4.40 kPa in children 0–5 years of age, 4.73 in children between 6 and 11 years of age, and 5.1 in those older than 11 years (Fig. 1; ANOVA test p = 0.001). According to our data, an upper limit of normal of stiffness in the three age groups of 5.96, 6.65, and 6.82 kPa was calculated (Table 2). No significant differences in liver stiffness according to gender were detected in children from 0 to 11 years, while in patients above 11 years of age stiffness differed significantly between sexes (boys, 5.6 kPa; girls, 4.7 kPa, t test p < 0.005). There were no significant differences between boys and girls in the other age groups.
Feasibility
For the feasibility study, we analyzed the data of 975 LSM performed in children from our hospital suffering from various diseases (data not shown). According to the manufacturer, TE is reliable when more than 60% of the shots produce a valid result and if the IQR/LSM range is below 0.3. Feasibility of the technique therefore was estimated counting the number of valid and invalid shots and counting the number of valid and invalid LSM in each age group.
Mean age of the patients was 9.1 years and the male/female ratio was 1:1. The mean stiffness in the 827 patients with valid LSM was 6.3, thus 1.8 kPa higher compared to the healthy control group.
In 148 of the 975 patients LSM were not valid (15%). This was either due to too many invalid shots (n = 44), too high IQR/LSM ranges (n = 2), or due to both (n = 102). When counting the shots performed in each individual patient an average of 15% (513/3,494) invalid shots occurred in children below 6 years of age while in the older patients it was 10% and 8%, respectively. The number of invalid LSM was highest in children below 6 years (27%). In older children it was 9% and 10% (Table 3). Patients with invalid LSM were significantly younger than those with valid LSM (5.8 vs. 9.7 years, p < 0.0001), showed a significantly higher stiffness (10.2 vs. 6.17, p < 0.0001), and examinations took significantly longer (202 vs. 160 s, p < 0.0001).
Another quality criterion is the IQR/LSM ratio. This ratio must be below 0.3 in valid LSM. Comparing IQR/LSM of valid LSM in the three age groups revealed a significantly higher ratio (0.16) in the youngest patients compared to 0.14 and 0.12 in school children and adolescents.
Discussion
We have investigated a large sample of healthy Caucasian children between 0 and 18 years of age to define a reliable upper limit of normal for the assessment of liver stiffness by TE. We defined “healthy” as absence of liver disease in clinical history, ultrasound [27], liver enzymes, and APRI score. A liver biopsy was not performed in these patients.
Upper limit of normal was defined as median stiffness in kilopascal plus 1.64 times standard deviation. This is equal with the 95th percentile. In healthy children the upper limit of normal for liver stiffness is 5.96 (0–5 years), 6.65 (6–11 years), and 6.82 (12–18 years) kPa. Our data suggest a significant age dependency of liver stiffness in healthy children. Stiffness increases by approximately 0.06 kPa each year. In stepwise regression age was the main factor for this phenomenon. Height and weight showed no influence on stiffness while male gender significantly increased stiffness only in adolescents.
There are few data on normal values in healthy adults. Significant age dependency of liver stiffness could not be demonstrated [30] although a tendency towards increasing stiffness values was observed. However, data from published studies are not consistent. Roulot et al. [28] have found a median stiffness of 5.49 in 429 liver healthy adults while Fung et al. have demonstrated a median stiffness of 4.6 kPa (range 2.0–7.1) in 28 healthy liver donors in a living related liver transplantation program [18], and Sirli et al. found a mean stiffness of 4.8 kPa in 152 normal volunteers [30]. Our data on adolescents with a median stiffness of 5.1 kPa are within the range of published data on adults.
A higher liver stiffness could be demonstrated in healthy boys, compared to girls in children over 11 years of age. This difference reached significance (5.6 vs. 4.7 kPa). Studies in adult populations have also demonstrated a higher stiffness in men compared to women. Roulot et al. [28] describes significantly higher liver stiffness values in men than in women (5.81 ± 1.54 vs. 5.23 ± 1.59 kPa). This was also seen in a small healthy population [13]. There are speculations about the existence of intrinsic differences between men and women in the density of liver extracellular matrix [3]. This hypothesis is supported by previous studies showing that ovarian hormones inhibit extracellular matrix production by liver stellate cells [35]. From our data factors that contributed to this difference could not be identified.
In our feasibility study with 975 consecutive examinations 15% of measurements were invalid. Literature reports a failure rate around 5% in healthy adults [28]. In a Chinese study group, Wong et al. [34] report on a higher failure rate of 11%. BMI and central obesity were independent risk factors for unreliable LSM and the authors speculate that in obese Chinese patients a different body composition leads to unreliable LSM at a lower BMI of 28 kg/m2 compared to Caucasian populations (30 kg/m2 [9]). Therefore we suggest that our data, as they are derived from a homogeneous Caucasian study group, should be used with care in other ethnicities [10]. The higher failure rate in the feasibility study was mainly due to the invalid LSM in children below 6 years. Fifty-nine percent of invalid LSM appeared in that age group due to a very high number of invalid shots. While in older children 9% to 10% of shots were invalid, in young children it was 15%. The technique of TE relies on perfectly relaxed patients that do not move during the shots. TE is technically possible without problems in sedated infants, toddlers, and children before school age. Therefore, we do believe that the development of the new S-probe with a smaller diameter sufficiently overcomes the problem of small intercostal spaces in infants and young children that made LSM in that patient group almost impossible before. If the children are agitated or crying a reliable examination may become impossible due to too many invalid shots. For a reliable examination there should not be an elevated intra-abdominal pressure and no elevated blood pressure because of crying. Recent studies could clearly demonstrate that extrahepatic factors like elevated central venous pressure, elevated blood pressure, obesity, ascites, or extrahepatic cholestasis are significantly influencing LSM [5, 9, 11, 21–23]. Therefore, besides an ultrasound of the liver and a thorough clinical examination to exclude these factors we also recommend to perform TE only in sleeping or sedated infants and small children. As sedation makes the non-invasive measurement of liver stiffness much more invasive, the main indication for this technique in young children should be a correlation of LSM with the degree of fibroses estimated by histology at the time of TE and the use of reliably measured stiffness in the follow-up of the liver disease as the child gets older. TE reliably works without prerequisite in school children from the age of around 6 years. In older children TE becomes more and more feasible which is demonstrated by the significantly smaller number of invalid shots per LSM in older children. Therefore, it may be used in these children in the work-up of liver disease even before liver biopsy, but it does not replace a histological examination as it provides no information on etiology of the liver disease causing fibrosis.
Sixty-eight percent of our pediatric patients were examined with the S-probe. The larger M-probe, which is used in most centers for examinations in adult patients, was feasible down to the age of 4 years only in extremely obese children. Ninety-six percent of examinations with the M-probe were performed in patients older than 8 years. It is suggested that pediatric centers, intending to perform TE in children need both probes to cover the complete spectrum of pediatric patients.
In conclusion, TE is a feasible technique in school children. In infants and small children LSM was invalid in 27% of cases without sedation. In small children TE should be preferentially performed in combination with sedation. LSM derived from TE in young children obtained without sedation must be interpreted with care. Upper limit of normal of liver stiffness is increasing with age. Taken from three distinct age groups, young children, school children, and adolescents, the upper limit of normal is 5.96, 6.65, and 6.82 kPa, respectively. Further studies should now address the value of TE in pediatric hepatology taken into account the physiological variables delineated in this study.
References
Alkhouri N, Carter-Kent C, Lopez R, Rosenberg WM, Pinzani M, Bedogni G, Feldstein AE, Nobili V (2011) A combination of the pediatric NAFLD fibrosis index and enhanced liver fibrosis test identifies children with fibrosis. Clin Gastroenterol Hepatol 9:150–155
Aube C, Oberti F, Korali N, Namour MA, Loisel D, Tanguy JY, Valsesia E, Pilette C, Rousselet MC, Bedossa P, Rifflet H, Maiga MY, Penneau-Fontbonne D, Caron C, Cales P (1999) Ultrasonographic diagnosis of hepatic fibrosis or cirrhosis. J Hepatol 30:472–478
Bissell DM (1999) Sex and hepatic fibrosis. Hepatology 29:988–989
Bravo AA, Sheth SG, Chopra S (2001) Liver biopsy. N Engl J Med 344:495–500
Calvaruso V, Camma C, Di Marco V, Maimone S, Bronte F, Enea M, Dardanoni V, Manousou P, Pleguezuelo M, Xirouchakis E, Attanasio M, Dusheiko G, Burroughs AK, Craxi A (2010) Fibrosis staging in chronic hepatitis C: analysis of discordance between transient elastography and liver biopsy. J Viral Hepat 17:469–474
Castera L, Negre I, Samii K, Buffet C (1999) Pain experienced during percutaneous liver biopsy. Hepatology 30:1529–1530
Castera L, Vergniol J, Foucher J, Le Bail B, Chanteloup E, Haaser M, Darriet M, Couzigou P, De Ledinghen V (2005) Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology 128:343–350
Castera L, Forns X, Alberti A (2008) Non-invasive evaluation of liver fibrosis using transient elastography. J Hepatol 48:835–847
Castera L, Foucher J, Bernard P, Carvalho F, Allaix D, Merrouche W, Couzigou P, de Ledinghen V (2010) Pitfalls of liver stiffness measurement: a 5-year prospective study of 13,369 examinations. Hepatology 51:828–835
Chang PE, Lui HF, Chau YP, Lim KH, Yap WM, Tan CK, Chow WC (2008) Prospective evaluation of transient elastography for the diagnosis of hepatic fibrosis in Asians: comparison with liver biopsy and aspartate transaminase platelet ratio index. Aliment Pharmacol Ther 28:51–61
Coco B, Oliveri F, Maina AM, Ciccorossi P, Sacco R, Colombatto P, Bonino F, Brunetto MR (2007) Transient elastography: a new surrogate marker of liver fibrosis influenced by major changes of transaminases. J Viral Hepat 14:360–369
Cole TJ, Green PJ (1992) Smoothing reference centile curves: the LMS method and penalized likelihood. Stat Med 11:1305–1319
Corpechot C, El Naggar A, Poupon R (2006) Gender and liver: is the liver stiffness weaker in weaker sex? Hepatology 44:513–514
de Ledinghen V, Douvin C, Kettaneh A, Ziol M, Roulot D, Marcellin P, Dhumeaux D, Beaugrand M (2006) Diagnosis of hepatic fibrosis and cirrhosis by transient elastography in HIV/hepatitis C virus-coinfected patients. J Acquir Immune Defic Syndr 41:175–179
de Ledinghen V, Le Bail B, Rebouissoux L, Fournier C, Foucher J, Miette V, Castera L, Sandrin L, Merrouche W, Lavrand F, Lamireau T (2007) Liver stiffness measurement in children using FibroScan: feasibility study and comparison with Fibrotest, aspartate transaminase to platelets ratio index, and liver biopsy. J Pediatr Gastroenterol Nutr 45:443–450
Dittrich M, Milde S, Dinkel E, Baumann W, Weitzel D (1983) Sonographic biometry of liver and spleen size in childhood. Pediatr Radiol 13:206–211
Forns X, Ampurdanes S, Llovet JM, Aponte J, Quinto L, Martinez-Bauer E, Bruguera M, Sanchez-Tapias JM, Rodes J (2002) Identification of chronic hepatitis C patients without hepatic fibrosis by a simple predictive model. Hepatology 36:986–992
Fung J, Lai C, Chan S, But D, Seto W, Cheng C, Wong DK, Lo C, Fan S, Yuen M (2010) Correlation of liver stiffness and histological features in healthy persons and in patients with occult hepatitis B, chronic active hepatitis B, or hepatitis B cirrhosis. Am J Gastroenterol 105:1116–1122
Maharaj B, Maharaj RJ, Leary WP, Cooppan RM, Naran AD, Pirie D, Pudifin DJ (1986) Sampling variability and its influence on the diagnostic yield of percutaneous needle biopsy of the liver. Lancet 1:523–525
McHutchison J, Poynard T, Afdhal N (2006) Fibrosis as an end point for clinical trials in liver disease: a report of the international fibrosis group. Clin Gastroenterol Hepatol 4:1214–1220
Millonig G, Reimann FM, Friedrich S, Fonouni H, Mehrabi A, Buchler MW, Seitz HK, Mueller S (2008) Extrahepatic cholestasis increases liver stiffness (FibroScan) irrespective of fibrosis. Hepatology 48:1718–1723
Millonig G, Friedrich S, Adolf S, Fonouni H, Golriz M, Mehrabi A, Stiefel P, Poschl G, Buchler MW, Seitz HK, Mueller S (2010) Liver stiffness is directly influenced by central venous pressure. J Hepatol 52:206–210
Mueller S, Millonig G, Sarovska L, Friedrich S, Reimann FM, Pritsch M, Eisele S, Stickel F, Longerich T, Schirmacher P, Seitz HK (2010) Increased liver stiffness in alcoholic liver disease: differentiating fibrosis from steatohepatitis. World J Gastroenterol 16:966–972
Nobili V, Parkes J, Bottazzo G, Marcellini M, Cross R, Newman D, Vizzutti F, Pinzani M, Rosenberg WM (2009) Performance of ELF serum markers in predicting fibrosis stage in pediatric non-alcoholic fatty liver disease. Gastroenterology 136:160–167
Nobili V, Alisi A, Torre G, De Vito R, Pietrobattista A, Morino G, De Ville De Goyet J, Bedogni G, Pinzani M (2010) Hyaluronic acid predicts hepatic fibrosis in children with nonalcoholic fatty liver disease. Transl Res 156:229–234
Poniachik J, Bernstein DE, Reddy KR, Jeffers LJ, Coelho-Little ME, Civantos F, Schiff ER (1996) The role of laparoscopy in the diagnosis of cirrhosis. Gastrointest Endosc 43:568–571
Quillin SP, Siegel MJ, Rothbaum R (1993) Hepatobiliary sonography in cystic fibrosis. Pediatr Radiol 23:533–535
Roulot D, Czernichow S, Le Clesiau H, Costes J, Vergnaud A, Beaugrand M (2008) Liver stiffness values in apparently healthy subjects: influence of gender and metabolic syndrome. J Hepatol 48:606–613
Sandrin L, Fourquet B, Hasquenoph J, Yon S, Fournier C, Mal F, Christidis C, Ziol M, Poulet B, Kazemi F, Beaugrand M, Palau R (2003) Transient elastography: a new noninvasive method for assessment of hepatic fibrosis. Ultrasound Med Biol 29:1705–1713
Sirli R, Sporea I, Tudora A, Deleanu A, Popescu A (2009) Transient elastographic evaluation of subjects without known hepatic pathology: does age change the liver stiffness? J Gastrointestin Liver Dis 18:57–60
Sokol RJ (2002) Liver cell injury and fibrosis. J Pediatr Gastroenterol Nutr 35(1):S7–10
Tanner MS (2002) Mechanisms of liver injury relevant to pediatric hepatology. Crit Rev Clin Lab Sci 39:1–61
Wai C, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, Lok AS (2003) A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology 38:518–526
Wong GL, Wong VW, Chim AM, Yiu KK, Chu SH, Li MK, Chan HL (2011) Factors associated with unreliable liver stiffness measurement and its failure with transient elastography in the Chinese population. J Gastroenterol Hepatol 26:300–305
Yasuda M, Shimizu I, Shiba M, Ito S (1999) Suppressive effects of estradiol on dimethylnitrosamine-induced fibrosis of the liver in rats. Hepatology 29:719–727
Yeshua H, Oren R (2008) Non invasive assessment of liver fibrosis. Ann Transplant 13:5–11
Ziol M, Handra-Luca A, Kettaneh A, Christidis C, Mal F, Kazemi F, de Ledinghen V, Marcellin P, Dhumeaux D, Trinchet J, Beaugrand M (2005) Noninvasive assessment of liver fibrosis by measurement of stiffness in patients with chronic hepatitis C. Hepatology 41:48–54
Acknowledgments
This study was generously funded by the Dietmar Hopp Stiftung.
Conflict of interest
There was no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jens Peter Schenk and Ulrike Teufel contributed equally to the study.
Rights and permissions
About this article
Cite this article
Engelmann, G., Gebhardt, C., Wenning, D. et al. Feasibility study and control values of transient elastography in healthy children. Eur J Pediatr 171, 353–360 (2012). https://doi.org/10.1007/s00431-011-1558-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-011-1558-7