Abstract
Hemolytic uremic syndrome (HUS) is a disease characterized by thrombotic microangiopathy with a triad of non-immune hemolytic anemia, thrombocytopenia, and renal impairment. Approximately 10% of cases of HUS are classified as atypical (aHUS). While today many genetically forms of aHUS pathology are known, only about 50% of carriers precipitate the disease. The reason remains unclear, and triggering events like intercurrent infections have been postulated. In rare cases, influenza A is the known trigger of aHUS; however, no cases of influenza B have been reported.
Conclusion: We describe for the first time that influenza B strain as a trigger for aHUS in children with primary hereditary forms. We also showed in our three cases that immunization appears to be safe; however, this needs to be confirmed in a larger cohort.
What is Known: |
• Known triggers of aHUS are infectious specimen. |
• Influenza A-associated aHUS cases are rarely published. |
What is New: |
• aHUS can be triggered by influenza B virus infection. |
• Influenza vaccination of patients with aHUS appears safe. |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hemolytic uremic syndrome (HUS) is characterized by thrombotic microangiopathy with a triad of non-immune hemolytic anemia, thrombocytopenia, and renal impairment [1, 2]. Ninety percent of the cases are caused by verotoxin-producing Escherichia coli (EHEC) and are coined as typical or D+ HUS because of the history of hemorrhagic colitis [1, 2]. HUS is classified as atypical (aHUS) in approximately 5–10% of cases [1–3]. aHUS has an incidence of two per million population per year [4] and is a serious life-threatening disease with progression to end-stage renal disease in 50 to 80% of the cases (depending on the underlying defect) [1, 2, 5]. Many triggers are known to induce aHUS including infections with Streptococcus pneumoniae, Epstein-Barr virus, varicella, and human immunodeficiency virus [1, 2]. In rare cases, influenza A was reported as a trigger of aHUS [3]. However, no cases of aHUS triggered by influenza B have been described so far.
During the winter of 2012–2013, three patients presented at our department with an aHUS most likely triggered by influenza B virus infection. In all three patients, an extensive etiological work-up was performed. Different investigations could exclude the presence of the EHEC bacteria or Shigella dysenteriae type 1 neither on stool, blood, nor urine samples. Other viruses such as Epstein-Barr virus, cytomegalovirus, and hepatitis A, B, or C were not detected. Thrombotic thrombocytopenic purpura (TTP) was ruled out based on normal ADAMTS13 (Von Willebrand factor-cleaving protease) activity. There was no evidence of a secondary aHUS due to autoimmune disease. Screening was negative for anti-nuclear factor antibodies, anti-nuclear cardiolipine antibody, anticardiolipine, and lupus anticoagulant. No clinical evidence of lupus erythematosus was detected. Normal homocysteine and the absence of methylmalonic acidemia ruled out a cobalamin deficiency. On personal history, no medication use could be identified as a trigger of aHUS. No defect was found in the complement regulatory proteins (normal serum total complement, C3, C4, complement B, H, and I). Genetic testing revealed in all patients later on an underlying genetic complement dysregulation.
Case reports
Patient one
A previously healthy 10-year-old boy was transferred to our hospital with a suspicion of aHUS. He presented with a 3-day history of flu-like symptoms. His parents consulted because of progressive illness, jaundice, drowsiness, and macroscopic hematuria.
Physical examination showed an alert child with a blood pressure (BP) of 123/79 mmHg (P95, 121/81 mmHg). Petechiae on the lower limbs, jaundice, and mild peripheral edema were present. Blood results are shown in Table 1. He was admitted for supportive treatment (fluid, furosemide infusion, and platelet and packed cell transfusion). During the hospitalization, the kidney function declined with a maximum serum creatinine of 2.06 mg/dl (estimated glomerular filtration rate (eGFR) calculated with the Schwartz formula of 29 ml/min/1.73m2) and oliguria, without electrolyte disturbances. Recovery was observed after 1 week with conservative treatment and normalization of serum creatinine 1 month later.
Family history revealed that the maternal grandmother and her sister were known with end-stage renal disease (ESRD) due to aHUS with low C3, but undefined genetic cause. Genetic testing in our patient revealed a heterozygote mutation in the C3 gene (c.481C>T (p.Arg161Trp) in exon 4) [4, 6, 7].
Patient two
A 15-year-old boy known with aHUS due to a primary hereditary complement disorder presented with the third recurrence of aHUS after flu-like symptoms since 2 days and no history of diarrhea. He has a heterozygote mutation in the clusterin gene (c.1298A>C (p.Thr433Asn) in exon 7) and a heterozygote mutation in the membrane cofactor protein gene (MCP, c.811-816delGACAGT(p.Asp271-Ser272del) in exon 6) [8, 9] as described previously [5].
At presentation, he had a BP of 135/90 mmHg (P95, 133/84 mmHg) and orbital and peripheral edema of the lower limbs due to oliguria and acute kidney insufficiency with a serum creatinine of 4.1 mg/dl (eGFR of 18 ml/min/1.73m2). Initial laboratory findings are shown in Table 1. He was treated with plasma exchanges (six times in total) with improvement of diuresis and renal function. There was no need of dialysis or antiviral medication. Normalization of serum creatinine was seen 2 months later and remained stable during follow-up.
Patient three
The patient was a 9-year-old boy known with a previous episode of aHUS after a Salmonella typhimurium infection, with spontaneously recovery. He presented with a recurrence of aHUS after an episode of epistaxis, macroscopic hematuria, and flu-like symptoms since 2 days. On physical examination, he was euvolemic with a normal BP, petechiae on the lower limbs, and jaundice. Laboratory findings are shown in Table 1.
Genetic testing revealed a heterozygote mutation in the MCP gene (c.565T>G (p.Tyr189Asp) [6, 10]) and a heterozygote mutation in the CFB gene (c.26T>A(p.Leu9His), in exon 1) [11]. Plasma exchanges were started with improvement of the renal function and were stopped after six sessions. There was no need of dialysis or antiviral medication. Normalization of serum creatinine was seen 1 month later and remained stable during follow-up.
Because of flu-like symptoms, a nasopharyngeal swab was performed in all three patients and was positive for influenza B using the rapid antigen detection test. We suggested that the most probable diagnosis was an aHUS triggered by influenza B. All three patients (within the same flu season 2012–2013) were infected with the same B strain, from the B/Yamagata lineage as determined by sequencing of the hemagglutinin gene.
Discussion
We report for the first time three patients that presented with aHUS most probably triggered by influenza B virus infection during the same flu season before that eculizumab was available (2012–2013).
Etiologically, aHUS is a heterogeneous group with primary underlying genetic causes found in ∼50% of the patients. These genetic defects are involved in the regulation of the alternative complement pathway on vascular endothelial cells. They include defects of complement factor H (CFH), factor I, factor B, thrombomodulin (CD141), C3, MCP (CD46), and autoantibodies against factor H with or without CFH-related protein 1 and 3 deficiency [1–3, 12, 13]. Also, Von Willebrand factor-cleaving protease deficiency or defective cobalamin metabolism is known to cause aHUS [1–3, 13]. Furthermore, aHUS can be secondary to systemic diseases characterized by microvascular injury (such as systemic lupus erythematosus) [1–3, 13] and can be triggered by medication (like calcineurin inhibitors, cytotoxic, chemotherapy agents, and quinine) or infectious diseases (like S. pneumoniae, Epstein-Barr virus, varicella, and human immunodeficiency virus) [1–3, 13–17]. In rare cases, influenza A viruses have been reported to trigger aHUS [3].
There are three types of influenza viruses (A, B, and C) of which A and B are known to cause illnesses in humans [18]. Most influenza infections are self-limited, but infants or patients with underlying medical conditions are at increased risk for complications attributable to influenza [19]. Various pulmonary, neurological, cardiac, and muscular complications of influenza virus infection have been reported [3]. Renal complications of influenza virus infections are uncommon but can lead to deterioration in patient’s condition, such as acute kidney injury in critically ill patients, rhabdomyolysis, acute glomerulonephritis, disseminated intravascular coagulation, Goodpasture’s syndrome, and acute tubulointerstitial nephritis [3, 20]. Also, influenza A has been described to trigger aHUS [3].
aHUS associated with influenza virus is extremely rare. We can divide the reports of aHUS triggered by influenza A into two major groups (Table 2): seasonal influenza A caused by epigenetic drift and pandemic H1N1 influenza A caused by epigenetic shift [3].
Only six patients have been reported so far with aHUS associated with seasonal influenza A [3, 21–25] where in two patients, the serotype of influenza A is defined as H3N2 (Table 2) [21, 22]. In two post-renal transplant patients, the use of immunosuppressants may also have triggered aHUS [22, 23, 26].
Influenza A virus has eight separate gene segments [18]. Reassortment of genes between two strains of influenza (humans, avian, swine, etc.) can create a pandemic strain of influenza A to which humans have no protective immunity [18]. In 2009, due to epigenetic shift, influenza A (pH1N1) reappeared [18] and in a short period, more cases of aHUS were described in the literature, namely eight patients worldwide (Table 2) [19, 27–33]. It is not clear whether the virulence of the influenza A virus is important in causing or triggering aHUS [18]. In the literature, the pandemic group can be divided further into three groups (Table 2) [3]: (1) S. pneumoniae-associated HUS following H1N1 infection; (2) HUS triggered by H1N1 in patients with genetic complement dysregulation (four persons [27–30]); and (3) HUS associated with H1N1 without any known underlying disorder (three persons [31–33]). Although in the latter group, a thorough search in each patient to rule out a genetic complement dysregulation has not been done [3].
S. pneumoniae-associated HUS following influenza infection was only described in one patient [19]. S. pneumoniae is known to trigger HUS [3, 15, 18, 19]. Therefore, co-infection of S. pneumoniae should be sought in patients with aHUS following influenza infection [15, 18]. Influenza virus can precipitate the infection of the pneumococcus by inducing epithelial damage that predispose invasion of the pneumococcus, by exposure or upregulation of existing receptors and by altering the immune response by diminishing the ability of the host to clear pneumococcus or due to activation of the inflammatory cascade [3].
Although the mechanisms of influenza A virus-associated HUS have not been elucidated, two hypotheses have been postulated. One hypothesis suggests an altered immune response with activation of mononuclear cell that produces tumor necrosis factor alpha [3, 21, 22]. The second hypothesis suspects unmasking the cryptic Thomsen-Friedenreich antigen on the red blood cells, platelets, and glomerular epithelia caused by viral neuraminidase of influenza A that cleaves sialic acid residues from various glycoproteins [3, 31, 32, 34]. This latter hypothesis has also been postulated in S. pneumoniae-associated HUS [31, 35]. Since this is the first case report on aHUS caused by influenza B strains, we assume that similar mechanisms are involved, but specific studies should be done to elucidate the pathophysiology.
In our series, the three patients presented with an aHUS triggered by influenza B had all an underlying genetic complement dysregulation. The three children received further follow-up and with the upcoming influenza season, the question was raised whether it would be safe or even advisable to vaccinate these patients with aHUS triggered by influenza.
In Belgium, the Superior Health Council recommends seasonal influenza vaccination for high-risk populations [36]. In Europe/Belgium, only inactivated influenza vaccines were available at the time, namely influenza vaccines consist of split virus particles (split virion) or specific purified hemagglutinin (H) and neuraminidase (N) (subunit). For the 2013–2014 Northern hemisphere influenza season, WHO recommended the following strains to be included in the seasonal influenza vaccine: an A/California/7/2009 (H1N1) pdm09-like virus; an A (H3N2) virus antigenically like the cell-propagated prototype virus A/Victoria/361/2011; and a B/Massachusetts/2/2012-like virus [37].
The next year, we decided to vaccinate our patients because of the lack of literature [38], and because vaccination is the only available mean to prevent influenza infection and therefore possible relapse. Also, the likelihood of influenza infection causing a recurrence of aHUS was perceived to be far greater than the possibility of the inactivated trivalent vaccine. Our three patients were vaccinated prior to the 2013–2014, 2014–2015, and 2015–2016 influenza season. We followed them very carefully and they did not relapse. From our experience, even though it is based on a small cohort of three cases, we would like to suggest that influenza vaccination can be presumed safe in this population. Whether the vaccination protects them for a recurrence is still open for discussion, since the infecting B strain in 2014–2015 was the same strain used in the 2013–2014 and the 2014–2015 influenza vaccine.
Conclusion
Influenza viruses are uncommon triggers of aHUS. Influenza A viruses have been recognized as a trigger for aHUS in the past. We describe that the influenza B strain is also capable of triggering aHUS in children with a genetic predisposition. We also showed that immunization of these children with an inactivated trivalent vaccine appears to be safe.
Abbreviations
- aHUS:
-
Atypical hemolytic uremic syndrome
- CFH:
-
Complement factor H
- eGFR:
-
Estimated glomerular filtration rate
- EHEC:
-
Enterohemorragische Escherichia coli
- HUS:
-
Hemolytic uremic syndrome
- MCP:
-
Membrane cofactor protein
- TTP:
-
Thrombotic thrombocytopenic purpura
References
Scheiring J, Rosales A, Zimmerhackl LB (2010) Clinical practice. Today’s understanding of the haemolytic uraemic syndrome. Eur J Pediatr 169(1):7–13
Westra D, Wetzels JF, Volokhina EB, van den Heuvel LP, van de Kar NC (2012) A new era in the diagnosis and treatment of atypical haemolytic uraemic syndrome. Neth J Med 70(3):121–129
Watanabe T (2013) Renal complications of seasonal and pandemic influenza A virus infections. Eur J Pediatr 172(1):15–22
Roumenina LT, Frimat M, Miller EC, Provot F, Dragon-Durey MA, Bordereau P, Bigot S, Hue C, Satchell SC, Mathieson PW, Mousson C, Noel C, Sautes-Fridman C, Halbwachs-Mecarelli L, Atkinson JP, Lionet A, Fremeaux-Bacchi V (2012) A prevalent C3 mutation in aHUS patients causes a direct C3 convertase gain of function. Blood 119(18):4182–4191
Ståhl AL, Kristoffersson A, Olin AI, Olsson ML, Roodhooft AM, Proesmans W, Karpman D (2009) A novel mutation in the complement regulator clusterin in recurrent hemolytic uremic syndrome. Mol Immunol 46(11–12):2236–2243
Volokhina E, Westra D, Xue X, Gros P, van de Kar N, van den Heuvel L (2012) Novel C3 mutation p.Lys65Gln in aHUS affects complement factor H binding. Pediatr Nephrol 27(9):1519–1524
Fremeaux-Bacchi V, Moulton EA, Kavanagh D, Dragon-Durey MA, Blouin J, Caudy A, Arzouk N, Cleper R, Francois M, Guest G, Pourrat J, Seligman R, Fridman WH, Loirat C, Atkinson JP (2006) Genetic and functional analyses of membrane cofactor protein (CD46) mutations in atypical hemolytic uremic syndrome. J Am Soc Nephrol 17(7):2017–2025
Richards A, Kemp EJ, Liszewski MK, Goodship JA, Lampe AK, Decorte R, Müslümanoğlu MH, Kavukcu S, Filler G, Pirson Y, Wen LS, Atkinson JP, Goodship TH (2003) Mutations in human complement regulator, membrane cofactor protein (CD46), predispose to development of familial hemolytic uremic syndrome. Proc Natl Acad Sci U S A 100(22):12966–12971
Geerdink LM1, Westra D, van Wijk JA, Dorresteijn EM, Lilien MR, Davin JC, Kömhoff M, Van Hoeck K, van der Vlugt A, van den Heuvel LP, van de Kar NC (2012) Atypical hemolytic uremic syndrome in children: complement mutations and clinical characteristics. Pediatr Nephrol 27(8):1283–1291
Fan X, Yoshida Y, Honda S, Matsumoto M, Sawada Y, Hattori M, Hisanaga S, Hiwa R, Nakamura F, Tomomori M, Miyagawa S, Fujimaru R, Yamada H, Sawai T, Ikeda Y, Iwata N, Uemura O, Matsukuma E, Aizawa Y, Harada H, Wada H, Ishikawa E, Ashida A, Nangaku M, Miyata T, Fujimura Y (2013) Analysis of genetic and predisposing factors in Japanese patients with atypical hemolytic uremic syndrome. Mol Immunol 54(2):238–246
Gold B, Merriam JE, Zernant J, Hancox LS, Taiber AJ, Gehrs K, Cramer K, Neel J, Bergeron J, Barile GR, Smith RT, AMD Genetics Clinical Study Group, Hageman GS, Dean M, Allikmets R (2006) Variation in factor B (BF) and complement component 2 (C2) genes is associated with age-related macular degeneration. Nat Genet 38(4):458–462
Joseph C, Gattineni J (2013) Complement disorders and hemolytic uremic syndrome. Curr Opin Pediatr 25(2):209–215
Salvadori M, Bertoni E (2013) Update on hemolytic uremic syndrome: diagnostic and therapeutic recommendations. World J Nephrol 2(3):56–76
Lee MH, Cho KS, Kahng KW, Kang CM (1998) A case of hemolytic uremic syndrome associated with Epstein-Barr virus infection. Korean J Intern Med 13(2):131–135
Spinale JM, Ruebner RL, Kaplan BS, Copelovitch L (2013) Update on Streptococcus pneumoniae associated hemolytic uremic syndrome. Curr Opin Pediatr 25(2):203–208
Kwon T, Belot A, Ranchin B, Baudouin V, Fremeaux-Bacchi V, Dragon-Durey MA, Cochat P, Loirat C (2009) Varicella as a trigger of atypical haemolytic uraemic syndrome associated with complement dysfunction: two cases. Nephrol Dial Transplant 24(9):2752–2754
Burke PA Jr, Aljadir D, Raman T (2010) Diagnosis, management, and pathogenesis of TTP/HUS in an HIV positive patient. Del Med J 82(9):309–312
Allen U, Licht C (2011) Pandemic H1N1 influenza A infection and (atypical) HUS—more than just another trigger? Pediatr Nephrol 26(1):3–5
Lei TH, Hsia SH, Wu CT, Lin JJ (2010) Streptococcus pneumoniae-associated haemolytic uremic syndrome following influenza A virus infection. Eur J Pediatr 169(2):237–239
Pettilä V, Webb SA, Bailey M, Howe B, Seppelt IM, Bellomo R (2011) Acute kidney injury in patients with influenza A (H1N1) 2009. Intensive Care Med 37(5):763–767
Watanabe T (2001) Hemolytic uremic syndrome associated with influenza A virus infection. Nephron 89(3):359–360
Asaka M, Ishikawa I, Nakazawa T, Tomosugi N, Yuri T, Suzuki K (2000) Hemolytic uremic syndrome associated with influenza A virus infection in an adult renal allograft recipient: case report and review of the literature. Nephron 84(3):258–266
Petersen VP, Olsen TS (1971) Late renal transplant failure due to the hemolytic-uremic syndrome. Acta Med Scand 189:377–380
Claude D, Delorme N, Schooneman F, Laprevote-Heully MC, Lambert H, Larcan A (1984) Hemolytic-uremic syndrome of viral origin successfully treated by plasma exchange. Presse Med 13(16):1003–1004
Davison AM, Thomson D, Robson JS (1973) Intravascular coagulation complicating influenza A virus infection. Brit Med J 1:654–655
Fortin MC, Raymond MA, Madore F, Fugère JA, Pâquet M, St-Louis G, Hébert MJ (2004) Increased risk of thrombotic microangiopathy in patients receiving cyclosporine-sirolimus combination. Am J Transplant 4:946–952
Caltik A, Akyüz SG, Erdogan O, Demircin G (2011) Hemolytic uremic syndrome triggered with a new pandemic virus: influenza A (H1N1). Pediatr Nephrol 26(1):147–148
Al-Akash SI, Almond PS, Savell VH Jr, Gharaybeh SI, Hogue C (2011) Eculizumab induces long-term remission in recurrent post-transplant HUS associated with C3 gene mutation. Pediatr Nephrol 26(4):613–619
Rhee H, Song SH, Lee YJ, Choi HJ, Ahn JH, Seong EY, Lee SB, Kwak IS (2011) Pandemic H1N1 influenza A viral infection complicated by atypical hemolytic uremic syndrome and diffuse alveolar hemorrhage. Clin Exp Nephrol 15(6):948–952
Bento D, Mapril J, Rocha C, Marchbank KJ, Kavanagh D, Barge D, Strain L, Goodship TH, Meneses-Oliveira C (2010) Triggering of atypical hemolytic uremic syndrome by influenza A (H1N1). Ren Fail 32(6):753–756
Golubovic E, Miljkovic P, Zivic S, Jovancic D, Kostic G (2011) Hemolytic uremic syndrome associated with novel influenza A H1N1 infection. Pediatr Nephrol 26(1):149–150
Printza N, Roilides E, Kotsiou M, Zafeiriou D, Hatzidimitriou V, Papachristou F (2011) Pandemic influenza A (H1N1) 2009-associated hemolytic uremic syndrome. Pediatr Nephrol 26(1):143–144
Trachtman H, Sethna C, Epstein R, D’Souza M, Rubin LG, Ginocchio CC (2011) Atypical hemolytic uremic syndrome associated with H1N1 influenza A virus infection. Pediatr Nephrol 26(1):145–146
Huang RT, Dietsch E, Rott R (1985) Further studies on the role of neuraminidase and the mechanism of low pH dependence in influenza virus-induced membrane fusion. J Gen Virol 66(Pt 2):295–301
Cochran JB, Panzarino VM, Maes LY, Tecklenburg FW (2004) Pneumococcus-induced T antigen activation in hemolytic uremic syndrome and anemia. Pediatr Nephrol 19:317–321
Superior Health Council Vaccination against seasonal flu (winter 2013–2014) http://www.health.belgium.be/internet2Prd/groups/public/@public/@shc/documents/ie2divers/19088802.pdf. Accessed 04 Jun 2014
Centers for Disease Control and Prevention http://www.cdc.gov/flu/professionals/acip/2013-summary-recommendations.htm
Matsumoto T, Fan X, Ishikawa E, Ito M, Amano K, Toyoda H, Komada Y, Ohishi K, Katayama N, Yoshida Y, Matsumoto M, Fujimura Y, Ikejiri M, Wada H, Miyata T (2014) Analysis of patients with atypical hemolytic uremic syndrome treated at the Mie University Hospital: concentration of C3 p.I1157T mutation. Int J Hematol 100(5):437–442
Authors’ contributions
Karen van Hoeve: Dr. van Hoeve is the first author and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted.
Corine Vandermeulen: Prof Vandermeulen was the advisor regarding the flu vaccination of subjects and therefore acquisition of data. She provided input and feedback on the manuscript and approved the final manuscript as submitted.
Marc Van Ranst: Prof Van Ranst supervised virology data collection and approved the final manuscript as submitted.
Elena Levtchenko: Dr. Levchenko reviewed and revised the manuscript, and approved the final manuscript as submitted.
Lambert van den Heuvel: Mr. van den Heuvel analyzed and interpreted the genetic data and approved the final manuscript as submitted.
Djalila Mekahli: Dr. Mekahli conceptualized the study and approved the final manuscript as submitted.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The manuscript has not been submitted to more than one journal for simultaneous consideration. The article has not been published previously. All authors have materially participated in the research and/or article preparation. All authors have approved the final article.
Funding
All authors acknowledge receiving no funding for this work from any organization, nor any sources of support, including pharmaceutical and industry support.
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Communicated by Mario Bianchetti
Electronic supplementary material
Figure S1
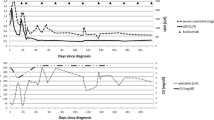
Evolution of the hematological testing during hospitalization. - X-axis: time of hospitalization (day). Day 0: time of hospitalization. - Y-axis: Blood results of hemoglubin, platelet count, creatinine level, haptoglobin, LDH and total bilirubine. - Curve: full line (▬) Patient 1, dashed line (- -) Patient 2 and dotted line (…) Patient 3. - Cut off reference value (blue line) (PDF 226 kb)
Rights and permissions
About this article
Cite this article
van Hoeve, K., Vandermeulen, C., Van Ranst, M. et al. Occurrence of atypical HUS associated with influenza B. Eur J Pediatr 176, 449–454 (2017). https://doi.org/10.1007/s00431-017-2856-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-017-2856-5