Abstract
Celiac disease remains one of the most challenging pathologies of the small intestine. It involves multiple pathogenic pathways and there are no disease-changing pharmacological agents available against it yet. The term microbiota refers to the community of microorganisms that inhabit a particular region of the body. Normal gut microbiota has a vital role in maintaining the intestinal homeostasis and promoting health. Celiac disease is associated with microbiota alteration, especially with an increase in the number of Gram-negative bacteria and a decrease in the number of Gram-positive bacteria. There is a strong relationship between intestinal dysbiosis and celiac disease, and recent studies are aimed at determining whether the celiac disease is a risk factor for dysbiosis or dysbiosis is for celiac disease. Therefore, the aim of this review was to assess the latest findings regarding the gut microbiota and its impact on the celiac disease, including therapeutic aspects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
What is known?
-
The gut microbiota contains the microorganisms that, at a certain point, colonize the intestine.
-
The role of gut microbiota is to maintain the physiological homeostasis of the intestine.
What is new?
-
The human leukocyte antigen genotype influences the gut colonization, while the gut microbiota alteration contributes to the risk of developing celiac disease (CD).
-
Both duodenal and colonic dysbiosis are associated with CD.
-
The bacterial virulence feature is considered higher in CD patients.
-
Probiotics, such as Bdellovibrio bacteriovorus, Lactobacillus spp, and Bifidobacterium, could improve the management of the CD patients.
Introduction
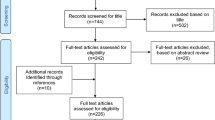
Celiac disease (CD) is an immune-mediated disorder affecting the small intestine, triggered by the ingestion of gluten-containing food in people who are genetically predisposed. It is known that the prevalence of HLA-DR3 and HLA-DQ2 genes in healthy subjects increases the risk of developing CD [1]. The gut microbiota contains the microorganisms that colonize the intestine at a certain point. The entire bacterial gut population is estimated to be around 35,000 bacterial species [2]. The role of gut microbiota is to maintain the physiological homeostasis of the intestine, and recent data highlight the implication of the microbiota in maintaining the host’s health [3]. Recent data suggest that the intestinal microbiota plays a critical role in the pathogenesis of the gastrointestinal diseases [4]. We aimed to assess the latest findings regarding the gut microbiota and its impact on the CD using the studies from the “PubMed” online database published during 2008–2016. The keywords used for the search engine were “celiac disease” and “microbiota,” which yielded 152 studies out of which 49 relevant studies were included.
The HLA genotype influences gut colonization
De Palma G et al. conducted a cohort study on newborn infants having at least one first-degree relative with CD, which concluded that the Gram-negative bacteria and the ones from the Bacteroides–Prevotella group were significantly higher in the high-risk group than in the control group [5]. This revealed that the HLA-DQ genotype interferes with the gut colonization process. Moreover, the combination between the HLA-DQ allele and the milk-feeding type in infants has an impact on the subsequent gut colonization, breastfeeding having a protective role in CD pathogenesis due to the facilitation of the gut colonization of Clostridium leptum, Bifidobacterium longum, and Bifidobacterium breve in infants with HLA-DQ genotype [6]. Furthermore, the HLA-DQ genotype favors the staphylococcal colonization of the gut [7]. The prospective study conducted by Olivares et al. on healthy children with one first-degree relative with CD revealed that those at high-risk had a lower number of Bifidobacterium spp and significantly higher numbers of Corynebacterium, Gemella, and Clostridium sensu stricto [8]. Therefore, it is believed that the HLA-DQ genotype may influence the first gut colonizers, contributing to dysbiosis being a risk factor.
Immunological aspects in celiac disease
In the gut lumen (Fig. 1), due to the digestion process, gliadin is formed, which is considered to be toxic to the epithelial cells of CD patients. Furthermore, gliadin is transported in the lamina propria mainly by transcellular pathways [9]. From that point, tissue transglutaminase (tTG) causes the deamidation of gliadin-resulting peptides, which are taken by the antigen presenting cells (APC) more efficiently than its precursors, thus resulting in increased immunogenicity [10]. The genetic factors also play a role. For example, it has been described that the DQB1*02 homozygous genotype provokes a stronger response from the CD4+ helper T cell than the heterozygous genotype [9]. In addition to this, the tTG-gliadin complexes are presented to CD4− T cells, resulting in the synthesis of antibodies against both tTG and deamidated gliadin. Moreover, the release of pro-inflammatory cytokines, such as Interferon gamma (IFNγ), IL-15, IL-18, and IL-21, has an impact on CD pathogenesis. The previous cytokines are responsible for the villous atrophy, crypt hyperplasia, and intraepithelial lymphocytes accumulation [11]. Another important factor is the increased permeability caused by environmental factors, such as: the amount of gluten and the time of gluten introduction, and the acquired infections [12].
Dysbiosis, the possible pathogenetic role in CD
Studies suggest that microbiota alterations play a role in the pathogenesis of not only CD, but other diseases, such as: non-alcoholic fatty liver disease, hepatic encephalopathy, irritable bowel syndrome, inflammatory bowel disease, metabolic syndrome, cardiovascular disease, obesity, autoimmune disorders, such as type 1 diabetes, and rheumatoid arthritis [13–16]. One piece of evidence demonstrating the role of gut dysbiosis was concluded after the Swedish CD epidemic (2004–2007) when a study conducted by Ou G et al. revealed that rod-shaped bacteria (Clostridium spp, Prevotella spp, and Actinomyces spp) was a risk factor for developing CD, contributing to incidence increase of CD during that period [17].
Cinova et al. conducted a study on germ-free rats that were infected with various bacterial strains, which were isolated from CD and healthy subjects, in the presence of gliadin and IFN- γ known as CD triggering factors [18]. It was found that, in the presence of CD triggering factors with Escherichia coli CBL2 or Shigella CBD8, the number of goblet cells in the small intestine was significantly lower resulting in the alteration of the intestinal barrier and tight junctions. However, gliadin and IFN-γ incubated with of Bifidobacterium bifidum IATA-ES2 promoted the increase in number of goblet cells. Moreover, Bifidobacterium bifidum augmented the production of inhibitors of metalloproteinases and chemotactic agents, enhancing the protection of the intestinal barrier. The microbiota of CD patients alters the gene expression of Toll-like Receptor 2, T Toll-like Receptor 9, and the Toll interacting protein, sustaining the pathogenic role of dysbiosis [19]. Moreover, changes in the duodenal microbiota lead to the alteration of the mucosal receptors, thus resulting in increased expression of IL-10 and IFN-γ, which are partly caused by increased TLR9 expression [20]. Furthermore, the gut microbiota components interact and influence the maturation of dendritic cells in the small intestine causing variations in its interactions with epithelial cells [21]. The dysbiosis produced by CD-associated bacteria could be a risk factor for CD, either by promoting the inflammatory response to gluten or, directly, by affecting the mucosal inflammation response [22].
Antibiotic use can lead to intestinal dysbiosis [23]. Marild et al. conducted a study on 2,933 CD patients matched for age and sex with 28,262 controls. A positive correlation between antibiotic use, and subsequently, CD was found [odds ratio (OR) = 1.40; 95% confidence interval (CI) = 1.27–1.53]. Therefore, dysbiosis may play a role in the early pathogenesis of CD [24]. Furthermore, Galipeau et al. conducted a study on mice with the DQ8 human gene revealing that, in subjects with genetic susceptibility, dysbiosis is a risk factor for CD [25]. A more recent study conducted on germ-free C57BL/6 mice colonized with bacteria isolated from CD or healthy subjects showed that Pseudomonas aeruginosa produced better intestinal barrier translocating peptides, thus resulting in activating the gluten specifying T cells from CD patients. On the contrary, Lactobacillus spp. diminished the immunogenicity of both gluten peptides produced by humans and of Pseudomonas aeruginosa proteases by degrading them [26]. A study conducted in 2016 by Caminero et al. focused on how the duodenal bacteria from both healthy and CD patients influence the metabolization of gluten. The study showed that, unlike the germ-free mice, the altered Schaedler flora colonized mice indicated PQP cleavage, thus showing the existence of a correlation between specific bacterial cleavage and the variety of gliadin peptides formed during digestion. Furthermore, Pseudomonas aeruginosa isolated from the duodenum of a CD patient due to elastase activity produces immunogenic peptides P. aeroginosa responsible for the activation of gluten specific T cells in HLA-DQ 2.5 + CD patients. The degradation peptides produced by, although having a shorter chain of amino acids, resulted in the immunogenicity being higher, thus resulting in similar responses as the 33 mer parent peptide. Moreover, the reduced size of the peptides facilitates passing through the epithelial barrier, enhancing the immunogenicity. Furthermore, the role of LasB elastase secreted by P. aeroginosa as a gluten-degrading enzyme has been demonstrated. However, in the presence of Lactobacillus strains, the P. aeroginosa produced peptides are further proteolyzed, resulting in decreased immunogenicity, thus exposing the relationship between probiotics and pathobionts. These findings show how the pathogenic bacteria can influence the CD risk in genetically susceptible individuals. Duodenal dysbiosis influences the host–microbe interactions, including the microbe–macrophage–neuronal communication and diet–microbe–host metabolic exchanges. Therefore, the pathophysiological pathways of CD are complex and still remain unclear [27]. There is a need for more studies in vivo/vitro to clarify the spectrum of interactions between dysbiosis and CD [4, 28, 29].
Characteristics dysbiosis in CD
Virulence features are considered higher in CD patients. For example, the prevalence of virulence genes of the Escherichia coli, such as P fimbriae (papC), capsule K5 (sfaD/E), and haemolysin (hlyA), was higher in CD patients than in healthy subjects [30]. Furthermore, the prevalence of methicillin-resistant (mecA) and adhesion altE virulent genes was higher in Staphylococcus spp isolated from CD patients than in healthy subject [31]. Other bacterial species [32, 33] isolated from CD patients are presented in Table 1.
The microbiota of CD patients is characterized by an increase in Gram-negative bacteria and a decrease in Gram-positive bacteria [34]. As shown in Table 1, many studies [35–38] have shown that there is a difference in the composition of microbiota in healthy and CD patients. However, the gut microbiota is also influenced by other factors. Nistal et al. conducted a study to compare the differences between intestinal bacterial populations in adults and children with or without CD [39]. It was shown that factors, such as age or a gluten-free diet (GFD), influence the microbiota of the CD patients. First, the GFD diet is one of the aspects that must be considered given that a diet without gluten interferes with the gut bacterial population [40]. After a GFD, the gut microbiota is partially restored. However, a decrease has been reported in the diversity of Lactobacillus spp and Bifidobacterium spp in the CD patients going under a GFD [41]. After a GFD, the number of Escherichia coli spp and Staphylococcus spp was restored to normal in CD patients [12]. Furthermore, there were no differences between the fecal pH of patients with CD and healthy subjects. Nonetheless, the lower levels of Bifidobacterium spp in the gut microbial composition of CD patients will promote the pathological process of the disease [42]. In spite of a GFD, persistent gastrointestinal symptoms may be correlated with an unbalanced composition of duodenal microbiota [43]. Moreover, the extra-gastrointestinal symptoms such as dermatitis herpetiformis, and anemia, describe a particular microbiota composition. Wacklin P et al. conducted a study on 33 CD patients with different symptoms and 18 control subjects. The CD patients group was more abundant in Proteobacteria phylum, while the CD patients with dermatitis herpetiformis and controls were more abundant in Firmicutes phylum, suggesting the role of duodenal dysbiosis in disease manifestation [44].
Other significant factors to consider are diet changes, infant infections, and antibiotic use [45]. In infants at risk of developing CD, infections and antibiotic intake in the first 4 months of life are correlated with lymphocyte subpopulations and microbiota alteration [46].
Microbiota as a powerful tool in therapy
Commensal bacterial species are vital to maintain gut immunological homeostasis; therefore, the identification of immunomodulatory species represents a potential tool in reversing gut dysbiosis [47].
Mechanism of action of probiotics
The probiotics are in direct competition with the pathogens not only for nutrients and prebiotics, but also for the adhesion sites (Fig. 2). Therefore, the probiotics are inhibiting the proliferation of pathogens. Furthermore, some probiotics, such as Saccharomyces boulardii, are able to block toxin receptors or have even direct toxin destruction effect [48]. Bifidobacterium and Lactobacillus strains secrete short chain volatile fatty acids, hydrogen peroxide, and antibacterial peptides (lactocidin, acidophilin, and lactacin B). Therefore, the intraluminal pH is reduced and the proliferation of pathogenic bacteria is diminished [49, 50]. Enhanced barrier function is the result of promoting the expression of epithelial growth factor receptor (EGF-R) and heat-shock proteins (hsp 25, hsp 27). Moreover, it has been demonstrated that some strains of probiotics, such as Lactobacillus GG, Bifidobacterium lactis, and Saccharomyces boulardii, are responsible for humoral modulation by inducing the expression of TGFβ, IL-10, and IL-6, which will further promote the B-cell maturation in favor of IgA secretion. In addition to this, probiotics also promote the up-regulation of Ig receptors on the basolateral surface of intestinal epithelial cells, thus increasing the Ig A transcytosis in the gut lumen [50]. However, probiotics produce a series of different effects depending not only on the strain used but also on dosage, route of administration, and frequency. Therefore, strain selection into combined therapies could improve the future aspects in the treatment of bowel diseases [51].
The need for probiotic supplements for CD patients
Iebba et al. conducted a study on 92 pediatric subjects, healthy, or suffering from CD or inflammatory bowel disease or cystic fibrosis, which disclosed that Bdellovibrio bacteriovorus was heavily decreased in patients suffering from CD or inflammatory bowel disease, thus sustaining the role of B. Bacteriovorus as a potential probiotic to restore the gut immunological homeostasis [52]. Latest findings revealed that Lactobacillus spp and Bifidobacterium spp are considered to have a favorable impact on gliadin-damaged epithelial cells [53]. Furthermore, Olivares et al. conducted a double-blind, randomized, placebo-controlled trial on 33 newly diagnosticated pediatric CD patients to assess the beneficial effects of Bifidobacterium longum CECT 7347. It was shown that Bifidobacterium longum CECT 7347 reduced the intestinal inflammatory response supported by the decrease of sIgA in fecal samples [54]. Therefore, Bifidobacterium longum CECT 7347 could improve the intestinal bacterial balance in CD patients. Moreover, Lactobacillus rhamnosus and Lactobacillus paracasei strains isolated from the feces of healthy children could be designed as probiotic supplements to promote the health of CD patients [55]. Another double-blinded, placebo-controlled trial on 46 CD children under GFD divided into two groups and 18 subjects in the control group, conducted by Klemenak M et al. evaluated the anti-inflammatory cytokine interleukin 10 (IL-10) and pro-inflammatory cytokine tumor necrosis factor alpha (TNF-α) serum production after receiving the probiotic strains Bifidobacterium breve BR03 and B632. It has been showed that, after receiving the probiotic strains for 3 months, the serum levels of TNF-α and IL-10 were decreased. Pseudomonas aeruginosa could also represent a potential tool in the therapy of CD [56]. Wei G et al. conducted a study aiming to isolate potential bacteria with gluten-degrading activity, demonstrating the therapeutic role of pseudolysin (lasB) produced by active Pseudomonas aeruginosa strains [57].
Parasite infections and its effects on immunomodulatory responses
Another direction in the management of CD is represented by parasite infections and its effects on immunomodulatory responses [58]. Croese J et al. conducted a study on 12 CD patients inoculated with Necator americanus larvae undergoing a gluten-diet [59]. It was revealed that helminths promote tolerance to gluten among CD patients. Furthermore, hookworms are responsible for the enrichment in bacterial species, aspect that could explain the regulation of gluten-induced inflammation made by hookworms [60].
Gluten-free diet and lifestyle in celiac disease patients
The commensal microbiota is a result of the influence of lifestyle variations, such as developments in food refining process and the presence of various infectious factors. The additives and chemical substances used in food processing have modified the gut microbiota, in favor of more aggressive bacterial strains [61]. Furthermore, a diet high on proteins and saturated fats will reduce the Bacteroidetes:Firmicutes ratio. High fat diets alter the gut microbial composition by decreasing the number of both Gram-positive and Gram-negative bacteria. Studies have shown that non-dietary lifestyle factors, such as smoking, obesity, and sedentariness, influence the gut microbiota. Moreover, stress by influencing the gut-brain axis alters the microbial population of the gut [62]. The therapeutic management of CD implies a strict adherence to GFD. However, studies have shown that in spite of a GFD, fecal, and duodenal dysbiosis is present in both treated and untreated CD patients. The link between oral, intestinal microbiota, and CD has not yet been established; therefore, further studies are needed to improve the content of gluten-free food for a better therapeutic approach towards celiac disease [63].
Conclusions
Dysbiosis and the HLA genotype have a certain role in the pathogenesis of CD. However, the mechanisms are intricate. On one hand, the HLA genotype influences the gut colonization, while the gut microbiota alteration contributes to the risk of developing CD. Moreover, both duodenal and colonic dysbiosis are associated with CD. The most frequent Gram-negative bacterial species isolated from CD patients were: Bacteroides spp, Salmonella spp, Shighella spp, Klebsiella spp, Neisseria spp, and Prevotella spp. Although CD is associated with a decrease in the number of Gram-positive bacteria, pathogenic Gram-positive species, such as Clostridium spp, Staphylococcus spp, and Actinomyces spp, could be isolated from CD patients. Furthermore, bacterial virulence features are considered higher in CD patients. Efforts, to date, on the effect of microbiota in the therapy of CD studies have shown that the use of probiotics for instance, Bdellovibrio bacteriovorus, Lactobacillus spp and Bifidobacterium could improve the management of the patients.
References
Bai JC, Fried M, Corazza GR et al (2013) World Gastroenterology Organisation global guidelines on celiac disease. J Clin Gastroenterol 47:121–126
Frank DN, St Amand AL, Feldman RA et al (2007) Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci USA 104:13780–13785
Jandhyala SM, Talukdar R, Subramanyam C et al (2015) Role of the normal gut microbiota. World J Gastroenterol 21:8787–8803
Nagao-Kitamoto H, Kitamoto S, Kuffa P et al (2016) Pathogenic role of the gut microbiota in gastrointestinal diseases. Intest Res 14:127–138
De Palma G, Capilla A, Nadal I et al (2010) Interplay between human leukocyte antigen genes and the microbial colonization process of the newborn intestine. Curr Issues Mol Biol 12:1–10
Palma GD, Capilla A, Nova E et al (2012) Influence of milk-feeding type and genetic risk of developing coeliac disease on intestinal microbiota of infants: the PROFICEL study. PloS One 7:e30791
Olivares M, Laparra JM, Sanz Y (2013) Host genotype, intestinal microbiota and inflammatory disorders. Br J Nutr 109:S76–S80
Olivares M, Neef A, Castillejo G et al (2015) The HLA-DQ2 genotype selects for early intestinal microbiota composition in infants at high risk of developing coeliac disease. Gut 64:406–417
Kupfer S, Jabri B (2012) Pathophysiology of celiac disease. Gastrointest Endosc Clin N Am 22:639–660
Barker JM, Liu E (2008) Celiac disease: pathophysiology, clinical manifestations and associated autoimmune conditions. Adv Pediatr 55:349–365
Garrote JA, Gómez-González E, Bernardo D et al (2008) Celiac disease pathogenesis: the proinflammatory cytokine network. J Pediatr Gastroenterol Nutr 47:S27–S32
Sarno M, Discepolo V, Troncone R et al (2015) Risk factors for celiac disease. Ital J Pediatr 41:57
Icaza-Chavez ME (2013) Gut microbiota in health and disease. Rev Gastroenterol Mex 78:240–248
Bustos Fernandez LM, Lasa JS et al (2014) Intestinal microbiota: its role in digestive diseases. J Clin Gastroenterol 48:657–666
McLean MH, Dieguez D Jr, Miller LM et al (2015) Does the microbiota play a role in the pathogenesis of autoimmune diseases? Gut 64:332–341
Carding S, Verbeke K, Vipond DT et al (2015) Dysbiosis of the gut microbiota in disease. Microb Ecol Health Dis 26:26191
Ou G, Hedberg M, Horstedt P, Baranov V et al (2009) Proximal small intestinal microbiota and identification of rod-shaped bacteria associated with childhood celiac disease. Am J Gastroenterol 104:3058–3067
Cinova J, De Palma G, Stepankova R et al (2011) Role of intestinal bacteria in gliadin-induced changes in intestinal mucosa: study in germ-free rats. PloS One 6:e16169
Kalliomaki M, Satokari R, Lahteenoja H et al (2012) Expression of microbiota, Toll-like receptors, and their regulators in the small intestinal mucosa in celiac disease. J Pediatr Gastroenterol Nutr 54:727–732
Cheng J, Kalliomaki M, Heilig HG et al (2013) Duodenal microbiota composition and mucosal homeostasis in pediatric celiac disease. BMC Gastroenterol 13:113
De Palma G, Kamanova J, Cinova J et al (2012) Modulation of phenotypic and functional maturation of dendritic cells by intestinal bacteria and gliadin: relevance for celiac disease. J Leukoc Biol 92:1043–1054
Sjoberg V, Sandstrom O, Hedberg M et al (2013) Intestinal T-cell responses in celiac disease - impact of celiac disease associated bacteria. PloS One 8:e53414
Hawrelak J, Myers S (2004) The causes of intestinal dysbiosis: a review. Altern Med Rev 9:180–197
Marild K, Ye W, Lebwohl B et al (2013) Antibiotic exposure and the development of coeliac disease: a nationwide case-control study. BMC Gastroenterol 13:109
Galipeau HJ, McCarville JL, Huebener S et al (2015) Intestinal microbiota modulates gluten-induced immunopathology in humanized mice. Am J Pathol 185:2969–2982
Galipeau HJ, Verdu EF (2014) Gut microbes and adverse food reactions: focus on gluten related disorders. Gut Microbes 5:594–605
Caminero A, Galipeau HJ, McCarville JL et al (2016) Duodenal bacteria from patients with celiac disease and healthy subjects distinctly affect gluten breakdown and immunogenicity. Gastroenterology 151:670–683
Moran C, Sheehan D, Shanahan F (2015) The small bowel microbiota. Curr Opin Gastroenterol 31:130–136
Cenit MC, Olivares M, Codoner-Franch P et al (2015) Intestinal microbiota and celiac disease: cause, consequence or co-evolution? Nutrients 7:6900–6923
Sánchez E, Nadal I, Donat E et al (2008) Reduced diversity and increased virulence-gene carriage in intestinal enterobacteria of coeliac children. BMC Gastroenterol 8:50
Sanchez E, Ribes-Koninckx C, Calabuig M et al (2012) Intestinal Staphylococcus spp. and virulent features associated with coeliac disease. J Clin Pathol 65:830–834
Collado MC, Donat E, Ribes-Koninckx C et al (2009) Specific duodenal and faecal bacterial groups associated with paediatric coeliac disease. J Clin Pathol 62:264–269
Schippa S, Iebba V, Barbato M et al (2010) A distinctive ‘microbial signature’ in celiac pediatric patients. BMC Microbiol 10:175
Di Cagno R, De Angelis M, De Pasquale I et al (2011) Duodenal and faecal microbiota of celiac children: molecular, phenotype and metabolome characterization. BMC Microbiol 11:219
Sanchez E, Donat E, Ribes-Koninckx C et al (2013) Duodenal-mucosal bacteria associated with celiac disease in children. Appl Environ Microbiol 79:5472–5479
Francavilla R, Ercolini D, Piccolo M et al (2014) Salivary microbiota and metabolome associated with celiac disease. Appl Environ Microbiol 80:3416–3425
Giron Fernandez-Crehuet F, Tapia-Paniagua S, Morinigo Gutierrez MA et al (2016) The duodenal microbiota composition in children with active coeliac disease is influenced by the degree of enteropathy. An Pediatr (Barc) 84:224–230
D’Argenio V, Casaburi G, Precone V et al (2016) Metagenomics reveals dysbiosis and a potentially pathogenic N. flavescens strain in duodenum of adult celiac patients. Am J Gastroenterol 111:879–890
Nistal E, Caminero A, Herran AR et al (2012) Differences of small intestinal bacteria populations in adults and children with/without celiac disease: effect of age, gluten diet, and disease. Inflamm Bowel Dis 18:649–656
Bonder MJ, Tigchelaar EF, Cai X et al (2016) The influence of a short-term gluten-free diet on the human gut microbiome. Genome Med 8:45
Nistal E, Caminero A, Vivas S et al (2012) Differences in faecal bacteria populations and faecal bacteria metabolism in healthy adults and celiac disease patients. Biochimie 94:1724–1729
Golfetto L, de Senna FD, Hermes J et al (2014) Lower bifidobacteria counts in adult patients with celiac disease on a gluten-free diet. Arq Gastroenterol 51:139–143
Wacklin P, Laurikka P, Lindfors K et al (2014) Altered duodenal microbiota composition in celiac disease patients suffering from persistent symptoms on a long-term gluten-free diet. Am J Gastroenterol 109:1933–1941
Wacklin P, Kaukinen K, Tuovinen E, et al (2013) The duodenal microbiota composition of adult celiac disease patients is associated with the clinical manifestation of the disease. Inflamm Bowel Dis 2013;19:934–941
Pozo-Rubio T, Olivares M, Nova E et al (2012) Immune development and intestinal microbiota in celiac disease. Clin Dev Immunol 2012:654143
Pozo-Rubio TG, Mujico JR, Olivares M et al (2013) Influence of early environmental factors on lymphocyte subsets and gut microbiota in infants at risk of celiac disease; the PROFICEL study. Nutr Hosp 28:464–473
Ivanov II, Honda K (2012) Intestinal commensal microbes as immune modulators. Cell Host Microbe 12:496–508
Gerald Friedman (2012) Clinical applications of probiotics in gastroenterology: questions and answers, an issue of gastroenterology clinics. Saunders, United States
Fons M, Gomez A (2000) Mechanisms of colonisation and colonisation resistance of the digestive tract. Microbial Ecol Health Dis 12:240–246
Hardy H, Harris J, Lyon E et al (2013) Probiotics, prebiotics and immunomodulation of gut mucosal defences: homeostasis and immunopathology. Nutrients 5:1869–1912
Sherman PM, Ossa JC, Johnson-Henry K (2009) Unraveling mechanisms of action of probiotics. Nutr Clin Pract 24:10–14
Iebba V, Santangelo F, Totino V et al (2013) Higher prevalence and abundance of Bdellovibrio bacteriovorus in the human gut of healthy subjects. PloS One 8:e61608
De Sousa Moraes LF, Grzeskowiak LM, de Sales Teixeira TF et al (2014) Intestinal microbiota and probiotics in celiac disease. Clin Microbiol Rev 27:482–489
Olivares M, Castillejo G, Varea V et al (2014) Double-blind, randomised, placebo-controlled intervention trial to evaluate the effects of Bifidobacterium longum CECT 7347 in children with newly diagnosed coeliac disease. Br J Nutr 112:30–40
Lorenzo Pisarello MJ, Vintini EO, Gonzalez SN et al (2015) Decrease in lactobacilli in the intestinal microbiota of celiac children with a gluten-free diet, and selection of potentially probiotic strains. Can J Microbiol 61:32–37
Klemenak M, Dolinsek J, Langerholc T et al (2015) Administration of bifidobacterium breve decreases the production of TNF-alpha in children with celiac disease. Dig Dis Sci 60:3386–3392
Wei G, Tian N, Valery AC et al (2015) Identification of pseudolysin (lasB) as an aciduric gluten-degrading enzyme with high therapeutic potential for celiac disease. Am J Gastroenterol 110:899–908
Mohammadi R, Hosseini-Safa A, Ehsani Ardakani MJ et al (2015) The relationship between intestinal parasites and some immune-mediated intestinal conditions. Gastroenterol Hepatol Bed Bench 8:123–131
Croese J, Giacomin P, Navarro S et al (2015) Experimental hookworm infection and gluten microchallenge promote tolerance in celiac disease. J Allergy Clin Immunol 135:508–516
Giacomin P, Zakrzewski M, Croese J et al (2015) Experimental hookworm infection and escalating gluten challenges are associated with increased microbial richness in celiac subjects. Sci Rep 5:13797
Kverka M, Tlaskalova-Hogenova H (2013) Two faces of microbiota in inflammatory and autoimmune diseases: triggers and drugs. APMIS 121:403–421
Conlon AM, Bird AR (2015) The impact of diet and lifestyle on gut microbiota and human health. Nutrients 7:17–44
De Angelis M, Vannini L, Di Cagno R et al (2016) Salivary and fecal microbiota and metabolome of celiac children under gluten-free diet. Int J Food Microbiol 19(239):125–132
Acknowledgements
The first author received a grant from the University of Medicine and Pharmacy “Iuliu Hațieganu” Cluj–Napoca 2016, project no. 4995/21/08.03.2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
All authors contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Girbovan, A., Sur, G., Samasca, G. et al. Dysbiosis a risk factor for celiac disease. Med Microbiol Immunol 206, 83–91 (2017). https://doi.org/10.1007/s00430-017-0496-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00430-017-0496-z