Abstract
Historically, papillary renal cell carcinoma (PRCC) was divided into two types, type 1 and type 2, based solely on morphology. However, it is apparent that PRCC is far more complex and represents a histological, clinical, and molecular spectrum. There has been a significant evolution in our understanding of PRCC, highlighted by the recognition of new and molecularly defined entities that were previously included in PRCC type 2. This contemporary review addresses the evolving concepts regarding the PRCC, including why it is no longer needed to subtype PRCC, the current molecular landscape, prognostic parameters, and PRCC variants, including biphasic PRCC, papillary renal neoplasm with reverse polarity, and Warthin-like PRCC. Pathologists should also be aware of the potential mimickers of both low-grade and high-grade PRCCs as well as some new and emerging entities that may show papillary growth that should be excluded in the diagnostic workup. The evolving knowledge of PRCC biomarkers, morphologic patterns, and PRCC variants could also have important implications for clinical management. Lastly, the heterogeneity within the PRCC spectrum needs to be further studied, aiming to better stratify PRCC for appropriate clinical management and systemic therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Papillary renal cell carcinoma (PRCC) is the second most prevalent type of adult carcinomas of renal tubular origin, accounting for ~15% of all adult RCCs [1]. The current 5th edition of WHO defines PRCC as a circumscribed tumor with papillary or tubulopapillary architecture that lacks the specific features of other RCCs presenting with papillary architecture [2]. In 1976, Mancilla-Jimenez et al. described PRCC initially as a tumor with a papillary or tubulopapillary morphology that is avascular or hypovascular on imaging, frequently displays marked cystic and degenerative changes with necrosis, and is encased by a fibrous capsule [3]. Even at this early stage, PRCC was noted to have a heterogeneous morphology. The papillary lining ranged from a single-cell layer to a more complex pseudostratified lining. Cytology of the cells varied from small size with scant cytoplasm to large eosinophilic with abundant cytoplasm and cellular atypia. An association with foamy macrophages, often infiltrating the papillary stalks was also described, and often, these were associated with calcifications [3]. In fact, this initial description of PRCC holds accurately to this day, including the predominant papillary or tubulopapillary morphology, specific gross features with frequent necrosis, and a spectrum of heterogeneity, that is, the hallmark and the differential diagnostic dilemma in PRCC.
Subtypes of PRCC and why subtyping is no longer recommended
In 1997, Delahunt and Eble proposed a classification which dichotomized PRCC tumors into type 1 and type 2 [4]. Type 1 PRCC was lined by a single layer of small cells with scant pale cytoplasm, small bland nuclei, and inconspicuous nucleoli. Type 2 PRCC, in contrast, was characterized by cellular pseudostratification, abundant eosinophilic cytoplasm, and larger nuclei with prominent nucleoli. Type 2 carcinomas were often larger tumors and were associated with higher-stage disease. Interestingly, positive cytokeratin (CK) 7 immunohistochemical (IHC) staining was more frequent in the type 1 tumors and was often absent (or “null”) in the type 2 ones. Their study classified 64% of the PRCCs as type 1 and 36% as type 2 [4]. Multiple subsequent studies showed a consistent theme of PRCC type 2 being associated with more aggressive disease, including higher histologic grade and stage, and worse overall survival (OS) [5,6,7,8]. However, many studies also found that PRCC subtyping loses its significance in a multivariate analysis, particularly when controlling for grade and stage [5, 9,10,11]. Indeed, when using the contemporary WHO/ISUP grading, PRCC type 2 is at least a WHO/ISUP grade 3 disease, because of the prominent nucleoli, which could explain why it loses its significance when adjusted for grade.
In 2015, The Cancer Genome Atlas (TCGA) published its landmark study showing a significant heterogeneity in the PRCC type 2 group [12], which was divided into 3 different molecular classes. They also found cases originally lumped in the type 2 group that were MiT family translocation RCCs, RCCs with fumarate hydratase (FH) mutations, and cases with an FH signature [CIMP (CpG island methylator phenotype) group]. As about 1/3 of these cases included within PRCC type 2 represented potential outliers, this further questioned the rationale for maintaining PRCC type 2 as a homogenous PRCC type.
Another important challenge in PRCC typing was the substantial lack of inter-observer agreement on subtyping, as a significant number of PRCCs show in-between or mixed features between type 1 and type 2. Studies that have addressed this phenomenon found that if strict type 1 and type 2 criteria are applied, approximately half (45–48%) of the cases do not fit into these categories [13,14,15,16]. Authors used different terminologies to describe such PRCC cases, including “unclassified” [12], “overlapping” [13], “not otherwise specified” (NOS) [14, 15], and “mixed” [16]. This lack of consensus on the subtyping of a large portion of PRCC cases has likely influenced inconsistent results regarding the clinical significance of PRCC subtypes. Many studies indeed found that typing was not a significant parameter when adjusting for histological grade and stage [5, 7,8,9,10,11, 17, 18]. For example, a recent study showed that PRCC with mixed type 1 and “type 2” features are similar to type 1 PRCC at the clinicopathologic and molecular level [16]. Meanwhile, some authors found that typing does maintain its significance in multivariate analysis [7, 19], but the mounting evidence against it was one of the main reasons that pushed the current practice toward the “no typing” approach.
Finally, the Genitourinary Pathology Society (GUPS) in its review update on existing renal entities in 2021 formally recommended abandoning the PRCC typing [20], which was subsequently endorsed by the WHO 5th edition of the Classification of Urinary and Male Genital Tumors [2].
PRCC represents a spectrum of disease—evidence from TCGA
So what does the in-between PRCC category (i.e., neither type 1 nor type 2) represent—are we encountering a disease spectrum or several distinct entities? We and others [12, 16, 21] have tried to answer this question—and in our opinion, after removing specific outliers previously labeled as type 2, PRCC seems to represent a spectrum of morphologies. The classic type 1 morphology occupies the low-grade end of the spectrum, while the classic type 2 morphology represents the high-grade end of the spectrum, and a significant proportion of PRCC tumors lie in the middle of that spectrum [16] (Fig. 1).
PRCC represents a disease spectrum, when outliers from what was previously labeled “type 2” are removed. PRCC tumor spectrum includes classic low-grade/type 1–like at one end, classic high-grade/type 2–like at the other end, and NOS/mixed/ overlapping cases lie in the middle. Tumors at the opposite ends are defined by specific morphological, IHC, chromosomal, molecular, and clinical features, whereas in-between cases display variable and overlapping profiles
A good start to examine the evidence is the TCGA study on PRCC [12]. The TCGA identified four molecular classes of PRCCs: C1, C2a, C2b, and C2c (CIMP) group. C1 was enriched in type 1 tumors, while the other three classes were enriched in type 2. The CIMP included a group of nine cases in TCGA cohort, five of which were FH-mutant, while four had an FH-altered molecular signature (Fig. S1). A recent study by Wang et al. [22] found that the CIMP group originated from the collecting duct/distal tubular cells; in contrast, the majority of PRCCs originated from the proximal tubular cells [22]. We further investigated these nine cases of the CIMP group, using the available TCGA data [12], and we found that they highly expressed the markers of distal tubular origin, such as GATA3 and L1CAM [23], while showing low expression of α-methylacyl-CoA racemase (AMACR), a marker of both PRCC and proximal renal tubules [24] (Fig. S1e). Although the available morphology of these cases showed a papillary/tubulopapillary component, they also exhibited other morphologies that would not be readily classified as PRCC currently (Fig. S1a-d). In our opinion, these cases should not be considered PRCCs and should not have been factored into the cohort analysis.
The remaining three PRCC groups of the remaining TCGA cohort, C1, C2a, and C2b, point toward a continuum along a morphologic spectrum. C1 was enriched in type 1 PRCC cases, while C2b was exclusively formed of type 2 PRCCs and few unclassified cases. C2a represented an “in-between” group in the middle of the spectrum enriched in type 2 but also had about 30% of type 1 PRCC or unclassified cases. C2a also showed a consistent “in-between” molecular and clinical profiles and C2a clustered with the C1 group on methylation profiling, while it clustered with C2b on mRNA profiling. Based on the copy number analysis, C2a cases were more heterogeneous, with some clustering with the C1 group and others clustering with C2b. Clinically, C2a also had an intermediate overall survival (OS) between C1 and C2b, further supporting the disease spectrum paradigm.
Another important piece of evidence supporting that PRCC is a single entity that exhibits a spectrum is the uniform origin of the majority of PRCCs. Wang et al. performed chromatin accessibility analysis and single-cell sorting of normal kidney cells to identify the PRCC cell of origin and confirmed that the origin of PRCC is the proximal tubular cell [22]. If CIMP cases and the MiT family translocation RCCs are excluded from TCGA cohort, then only ~ 7% of PRCCs have a potentially distal tubular origin. However, it is important to note that TCGA cohort also harbors other non-PRCC cases, including papillary renal neoplasm of reverse polarity (PRNRP), urothelial carcinoma, NF2-mutant carcinomas, and ALK-rearranged RCCs [12]. As these cases all harbor a type 2–like morphology, they were likely mischaracterized as PRCC in TCGA cohort. Therefore, after a critical analysis, it appears that the great majority of TCGA PRCC cohort has a uniform origin from the proximal tubular cells.
Need for better PRCC stratification—the ABCC2 story
In 2015, we started a search for a molecular/biological-based biomarker that could stratify the unclassified PRCC cases that neither fit the type 1 nor the type 2 PRCC [14]. First, we found, similar to others [13, 16], that 47% of evaluated PRCC cases lacked consensus regarding type 1 versus 2 (we called this group PRCC NOS) [14, 15]. By utilizing the TCGA KIRP cohort, we found that ATP-binding cassette subfamily C member 2 (ABCC2), also known as multidrug resistance protein 2 (MRP2), is significantly overexpressed in the classic PRCC type 2 in comparison to type 1 [14]. ABCC2 is a transmembrane protein transporter that is normally involved in active drug transportation through an efflux mechanism [25]. In a non-tumor kidney, ABCC2 is naturally localized at the apical brush border membrane of proximal renal tubules [25].
ABCC2 was the only biomarker, when considering other potential biomarkers, that successfully dichotomized the PRCC NOS group into two groups with significant survival differences, in both univariate and multivariate analyses for disease-free survival (DFS) and OS [14, 15, 26, 27]. We assessed ABCC2 in four PRCC cohorts, with more than 500 cases, using both gene/transcript expression [14, 27] and IHC expression [26, 27]. High ABCC2 expression, manifested by brush border IHC staining, independently predicted a more aggressive PRCC group, as illustrated in Fig. 2. Additionally, we found that ABCC2 outperformed the WHO/ISUP nucleolar grade, which is currently the only available histologic parameter used to predict PRCC aggressive potential. ABCC2 also showed significant survival differences in PRCCs representing small renal masses (< 4 cm) and stage pT1a disease, which could be useful to guide clinical management decisions regarding active surveillance versus surgery in this PRCC group [26, 27].
PRCC (H&E) with corresponding ABCC2 IHC patterns: a, b PRCC with negative ABCC2 staining (inset; proximal renal tubules serve as positive internal control and glomeruli as a negative internal control). c, d PRCC with cytoplasmic pattern, characterized by the presence of weak granular cytoplasmic staining. e, f PRCC with brush border < 50% staining and g, h PRCC with brush border ≥ 50% staining. Brush border pattern is defined by distinct staining on the apical end of tumor cells with or without cytoplasmic staining
The high ABCC2 expression in more aggressive PRCCs is likely owing to the NRF2-ARE pathway enrichment in high-grade/type 2–like PRCCs, as ABCC2 represents a downstream target of NRF2-ARE activation [12, 15]. ABCC2 is also thought to have a chemoresistance effect; however, more recent studies show that ATP transporters are involved in cancer aggressiveness beyond the drug efflux [28]. Additionally, using preclinical models, we found that blocking ABCC2 in PRCC delays tumor growth [29]. Hence, there is potential for utilizing ABCC2 in future studies as a possible therapeutic target.
We have also consistently found that ABCC2 expression reflects the biological spectrum of PRCC [14, 15, 26, 27]. In our 2017 study [15], we studied the “in-between” group that we designated PRCC “type 3.” The PRCC “type 3” or “in-between” group (demonstrating ABCC2 brush border expression < 50% [26, 27]) provided confirmatory evidence for the PRCC disease spectrum. Morphologically, this group was enriched in NOS/overlapping/mixed cases, had an intermediate expression of ABCC2 [26, 27], and consistently had an intermediate DFS and OS [15, 26].
Papillary adenoma—PRCC and their relationship with end-stage renal disease
PRCCs, similar to clear cell RCCs, are believed to originate from the proximal tubular epithelial cells [30,31,32,33,34]. Papillary adenoma (PA) is considered a precursor lesion of PRCC, because it has an identical morphology, immunoprofile, and molecular signature to PRCC. However, PAs are limited to ≤ 15 mm in size and are deemed benign based on studies that show no risk of metastasis associated with this cut-off [35]. End-stage renal disease (ESRD) patients also have an increased risk of developing PRCCs, which tend to be multifocal and bilateral, and they also commonly harbor PAs [31,32,33]. Hes et al. found chromosomal changes that included gains in chromosomes 7 and 17 and loss of Y in the non-neoplastic parenchyma of ESRD, similar to the chromosomal changes found both in PA and PRCC [34]. A study by Lindgren et al. isolated a progenitor-like cell population in the proximal renal tubules that were expanded upon renal injury and were transcriptionally similar to PRCC [33]. In our previous work on PRCC [36], we investigated this potential progenitor-like cell, and we also found a cell population that was biologically similar to PA, which was significantly increased in ESRD. A recent single-cell sorting study by Wang et al. [22] confirmed that the majority of PRCCs specifically originate from proximal tubule–related progenitor cells [31,32,33,34]. This body of evidence conclusively connects the PRCC and PA to a progenitor-like cell population in the proximal renal tubules, which becomes enriched upon kidney injury.
Molecular/cytogenetic landscape of PRCC and MET pathway alterations
The spectrum of clinical and morphological heterogeneity of PRCC extends as well to the molecular and cytogenetic levels [12, 14]. Tumors with low-grade/“type 1” morphology often harbor gains of chromosomes 7 and 17, loss of Y, and also frequent gains of chromosomes 12, 16, and 20 [12, 37]. In comparison, fewer high-grade tumors retain the whole gains of chromosomes 7 and 17 and more commonly retain partial gains of chromosomes 17 [38], gains of 16 and 20, and a wide array of other chromosomal alterations [12, 37, 38].
MET alterations are more common in low-grade/“type 1” PRCCs [12, 39]. MET proto-oncogene is a tyrosine kinase receptor at chromosome 7q31.3, and MET-activating mutations are defining molecular events in hereditary PRCC, characterized by multifocal and bilateral PRCCs, autosomal dominant inheritance, and high penetrance [40]. MET is involved not only in tumor proliferation and invasiveness, but also plays a role in resistance to anti-tumor therapies [41]. Initially, MET mutations were identified as germline-activating mutations in hereditary PRCC [42], but MET mutations were also found in 10–15% of low-grade PRCCs. Generally, MET mRNA and protein expression were noted to be significantly increased in low-grade PRCC versus the high-grade/“type 2” group. The TCGA study attributed this overexpression to MET dysregulation by mutations, splice variants, gene fusions, or an increase in chromosome 7 copy numbers; collectively, these changes occur in ~ 80% of the “type 1” PRCCs [12].
The high-grade/“type 2” PRCCs represent a molecularly heterogeneous and diverse group. They are associated with alterations in cell cycle checkpoint genes, such as CDKN2A and TP53, as well as MYC and NRF2-ARE pathway activation [12, 43]. Chromatin modifier pathways are also commonly implicated in all PRCCs with mutations in SETD2, BAP1, and PBRM1 being more common in the “type 2” PRCC group [12].
We would like to highlight two important points regarding the molecular aspects of PRCC. First, there are no definitive hallmark molecular alterations diagnostic of PRCC. Chromosome 7 and 17 gains are only present in a portion of PRCCs and are primarily enriched in the low-grade/“type 1” group. Hence, the diagnosis of PRCC remains primarily a morphologic one, supported by the IHC profile, and by exclusion of outliers. The second important point is that the molecular characteristics of low-grade/“type 1” PRCCs are different from the high-grade/“type 2” tumors, and the underlying molecular PRCC signatures are heterogenous in the spectrum from low-grade to high-grade PRCCs, with the “in-between” PRCCs showing overlapping molecular profiles with both. This implies that a metastatic disease of low-grade/“type 1”–like and high-grade/“type 2”–like PRCC may be clinically and molecularly different and may respond differently to therapies, which could explain the poor response to systemic therapies in clinical trials [1].
Histologic prognostic parameters and WHO/ISUP nucleolar grade in PRCC
The WHO/ISUP grading has been widely accepted as a main prognostic factor for PRCC in the current practice [2]. It is based on nucleolar prominence for grades 1–3 and prominent nuclear pleomorphism or sarcomatoid and rhabdoid differentiation for grade 4 [2, 44]. Several studies have demonstrated that the four-tiered tumor grading provides superior prognostication compared to the histologic subtyping [10, 17, 18, 45]. Currently, WHO/ISUP nucleolar grading is recommended, and it should be included in pathology reports alongside stage, lymphovascular invasion, and rhabdoid or sarcomatoid histology, given their established association with aggressive behavior in PRCC [44, 46]. However, it is essential to acknowledge that the grading system, despite its better prognostic utility in PRCC, is not without limitations. Some studies have yielded varying results regarding its prognostic value including its lack of significance in multivariate analysis [11, 26, 27]. In addition, assigning grades on biopsy can be inaccurate in over a third of PRCCs, particularly in cases with mixed morphology [47].
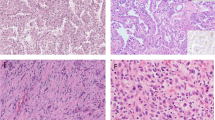
More recently, several histologic architectures have been reported to be associated with adverse outcomes in PRCC [16, 17, 48] (Fig. 3). Yang et al. investigated whether the specific growth patterns, such as solid, hobnail, and micropapillary, are associated with unfavorable prognosis [17]. In a PRCC cohort of 185 cases, micropapillary features were identified in 10 (5.4%) tumors, while hobnail and solid architectures were observed in 9 (4.9%) and 3 (10%) cases, respectively. All three patterns showed worse prognoses in univariate analysis, but only the micropapillary pattern retained statistical significance in multivariate analysis. The solid pattern is somewhat controversial as another study reported a more favorable clinical course among PRCCs with solid architecture [49]; however, the cases reported in this previous study were mostly composed of tightly compressed tubular structures rather than true solid sheets, as proposed by Yang et al. [17]. A recent study by Chan et al. found that the microcystic pattern is another histologic pattern associated with worse PRCC outcomes [48]. Notably, this pattern was present in a subset of historically classified type 1 PRCCs that demonstrated a propensity for extrarenal involvement and metastatic disease [48]. In addition, the study noted that the microcystic pattern had superior inter-observer reproducibility compared to the other patterns [48]. Of note, a cut-off of > 5% of the overall tumor area was considered for a particular growth pattern [17, 48]. More studies and larger cohorts are, however, needed to validate the association of these morphologic patterns with aggressive PRCC disease and to better define the cut -off proportions for these patterns.
Unfavorable architectures in PRCC, as reported in previous studies: a Hobnail: tumors cells characterized by apically protruding nuclei and eosinophilic or clear cytoplasm. b Micropapillary: clusters of 3–10 tumor cells with no lumen or fibrovascular core; more than 4 tumor buds are required to call it a micropapillary pattern. c, d Microcystic: cysts lined by neoplastic cells containing tumor papillae and separated by fibrotic stroma. These adverse histologic patterns often co-occur with other patterns, and a cut-off of > 5% of the overall tumor area is considered positive for a particular growth pattern
Recognition of PRCC variants—do they all belong to PRCC?
In recent years, several studies have identified specific PRCC variants with unique architectural and cytological patterns. In some variants, the unique morphology is associated with specific clinical behavior and molecular profiles. These variants/patterns include biphasic PRCC, papillary renal neoplasm with reverse polarity (PRNRP), and Warthin-like PRCC.
Biphasic PRCC, labeled initially as “biphasic alveolosquamoid” [50] and “biphasic squamoid alveolar” PRCC [51], is composed of two-cell populations that include clusters of larger eosinophilic cells with higher nuclear grade, surrounded by smaller, amphophilic cells with lower nuclear grade, forming alveolar or glomeruloid structures (Fig. 4a) [50]. In fact, such PRCC cases were likely considered in older studies as a “solid variant of PRCC,” showing “micronodular formations” that in some cases resembled abortive papillae [52]. Biphasic PRCC frequently shows emperipolesis or cytophagocytosis within the larger cells (Fig. 4a) [51]. On IHC, the large cells demonstrate immunoreactivity to cyclin D1 (Fig. 4b) [51]. An important clinicopathological aspect related to this variant is that it harbors a higher prevalence of MET mutations than the conventional PRCC (30–60%) [53,54,55], which in the right clinical setting can raise suspicion for a hereditary PRCC syndrome with a germline MET mutation. The biphasic PRCC had incidences of metastasis of 5–10% and may present with a higher-stage disease [56]. Additionally, this variant has been associated with frequent multifocal lesions in about 30% of the cases [56]. This variant is included within the PRCC spectrum, due to the consistent immunoprofile and the cytogenetic and molecular profiles overlapping with the classic type 1 PRCC [51, 53, 54].
PRCC variants: a, b Biphasic PRCC is composed of clusters of large, squamoid cells with high-grade nuclei often with emperipolesis (inset), surrounded by smaller, low nuclear grade cells (a). The large cell population is typically positive for cyclin D1 (b). c, d PRNRP is characterized by papillae lined by a single row of eosinophilic cells with apically located, low-grade nuclei (c). PRNRP consistently shows GATA3 nuclear immunoreactivity (d)
PRNRP has been referred to in some earlier studies as an “oncocytic PRCC” or “oncocytic PRCC with low-grade nuclei,” although the descriptions and images from these studies indicate that this was a heterogenous group that also harbored some traditional “type 2” PRCCs [57,58,59]. In 2017, we evaluated a subset of PRCCs with delicate papillary architecture that had an oncocytic morphology, characterized by low-grade nuclei (WHO/ISUP grade 1 or 2), which were linearly arranged opposite the basement membrane (Fig. 4c) and stained positive for GATA3 (Fig. 4d) [15]. Several subsequent studies by Al-Obaidy et al. further characterized this variant and identified positivity to L1CAM by IHC, weak or absent staining for AMACR and vimentin, and frequent KRAS mutations in 80–90% of these tumors [23, 60, 61]. Over 100 cases of PRNRP have been reported to date demonstrating uniform indolent behavior and without evidence of disease recurrence or metastasis [23, 60,61,62,63,64]. PRNRPs are usually small neoplasms, the majority being < 4 cm in size. It is important to accurately distinguish this entity from other eosinophilic PRCCs, which are often associated with aggressive behavior [63]. In our opinion, PRNRP likely represents a distinct entity and not a PRCC variant, primarily because the evidence points toward its origin from the distal nephron (distal renal tubules/collecting ducts). GATA3 and L1CAM are both distal nephron markers and are IHC hallmarks of PRNRP [23]. In addition, AMACR is uniformly expressed in PRCC and normal proximal tubules by IHC, but it is typically negative or underexpressed in PRNRP. Tong et al. also showed that PRNRPs shared a similar gene expression profile with the distal renal tubules [64], which further supports the conclusion that PRNRP is a separate entity that does not belong to the PRCC spectrum.
With only twelve reported cases to date [65, 66], Warthin-like PRCC is a rare variant of PRCC characterized by eosinophilic papillary morphology, WHO/ISUP nucleolar grade 2 to 3 [65], and typically admixed with dense stromal lymphocytic infiltrates [65]. However, this variant shows similar IHC and molecular profiles to PRCC [65]. Notably, among the eleven cases with available follow-up, three exhibited an aggressive clinical course [65, 66], and therefore, additional well-documented cases are needed to further characterize the biology of this variant.
Differential diagnosis of PRCC versus other renal entities with papillary morphology
According to the latest WHO 2022 classification, PRCC is defined as a malignant neoplasm exhibiting papillary or tubulopapillary growth patterns without specific features of other RCCs with papillary morphology [2]. This definition underscores the importance of distinguishing PRCC from other histologic mimickers. To date, there is no molecular or IHC marker that is specific for PRCC. PRCC tumors are typically reactive for PAX8, AE1/AE3, Cam5.2, CD10, vimentin, AMACR, and CK7, while they are negative for CD117 (KIT). AMACR and CK7 are the most valuable IHC markers to differentiate PRCC from other renal tumor types. AMACR is a sensitive marker of PRCC, albeit it is not entirely specific [67]. CK7 tends to be more positive in lower-grade PRCCs (up to 100%) than in higher-grade tumors (up to 27%) [4, 13]. This profile is also repeatedly observed in lower- versus higher-grade areas within the same tumor [13]. Thus, a proper diagnostic workup requires careful histological assessment with a judicial IHC workup and occasional molecular studies to rule out other renal entities that may mimic PRCC.
Low-grade renal entities with papillary morphology
Tumors that may exhibit features similar to low-grade PRCC include clear cell papillary renal cell tumor (CCPRCT), metanephric adenoma (MA), and mucinous tubular and spindle cell carcinoma (MTSCC). Figure 5a outlines the diagnostic algorithm of PRCC with low-grade morphology.
CCPRCTs display papillary or tubulopapillary architecture lined by clear cells with low-grade nuclei (WHO/ISUP grades 1–2) with linear arrangement opposite to the basement membrane, i.e., reverse polarity [68]. CCPRCT also typically exhibits diffuse CK7 staining and CAIX positivity in a cup-like pattern [68, 69] and is also frequently positive for GATA3 [70]. However, CCPRCT is usually negative for AMACR and CD10, both of which are expressed in PRCC [68, 69].
MA can also demonstrate focal or more prominent papillary growth, but typically, it is a small blue cell tumor that is positive for WT1 and often for CD57 on IHC, as well as for BRAF V600E [71, 72]. CK7 and AMACR are usually negative in MA.
MTSCC can be differentiated from PRCC primarily by the absence of a recognizable papillary growth pattern. MTSCC exhibits tubular and spindle cell morphology, with focal mucin deposition [73, 74]. Of note, focal mucin deposition has also been reported in rare PRCCs [75]. Although there is a significant overlap between the IHC profiles of MTSCC and PRCC, VSTM2A has been reported as a sensitive and specific in situ hybridization marker for MTSCC that can reliably distinguish it from PRCC [76]. MTSCC also shows multiple chromosomal losses, most frequently involving chromosomes 1, 4, 6, 8, 9, 13, 14, 15, and 22 while lacking trisomy 7 or 17 [77].
High-grade renal entities with papillary morphology
The real challenge lies in the differential diagnosis of high-grade PRCCs (prior “type 2”) from the respective renal mimickers. The two most important entities in this regard are MiT family translocation RCC and FH-deficient RCC, both of which can present with a predominant high-grade papillary morphology. Figure 5b outlines the systematic approach to high-grade PRCC.
Trpkov et al., in their study of FH-deficient RCC, found that 3% of cases previously diagnosed as PRCC type 2 harbor FH deficiency [78]. However, FH-deficient RCC often shows other non-papillary architectural patterns including solid, tubulocystic, tubular, and cribriform components [79]. Although FH-deficient RCC often shows large cherry-red nucleoli surrounded by a halo, this feature is not entirely specific to FH-deficient RCC and can be seen in other RCC types including high-grade PRCC [2, 78, 79]. Loss of FH immunoexpression and/or positive staining for 2-succino-cysteine (2SC) indicate FH aberrant mutations that can be helpful for the correct diagnosis. Typically, PRCC exhibits FH+/2SC− immunoprofile, which is opposite from FH-deficient RCC (FH−/2SC+) [78, 80, 81]. Rare cases with FH missense mutations are associated with heterogenous and patchy FH IHC expression, but these are usually positive for 2SC [82]. In difficult diagnostic scenarios, molecular testing showing either germline or sporadic FH mutations is diagnostic for this entity [78]. Additionally, FH-deficient RCCs can be positive for GATA3 IHC, which is consistent with the TCGA CIMP group data suggesting a possible distal nephron origin [83]. The diagnosis of FH-deficient RCC carries important clinical implications, because these patients often present with advanced and metastatic disease necessitating aggressive treatment, as well as genetic counseling and testing for their family members [84].
MiT family translocation RCC, particularly TFE3-rearranged RCC and TFEB-altered RCC, can also present with a dominant high-grade papillary morphology [85]. Morphologic clues, such as an admixture of other architectural patterns, including solid, nested, and tubular, and the coexistence of clear and eosinophilic cell components, should raise suspicion for this entity [20, 85]. IHC markers that can aid in that differential diagnosis include reactivity for TFE3, cathepsin K, HMB-45, and Melan-A, as well as TFEB expression in TFEB-altered RCC. Of note, cathepsin K, while a relatively specific marker for TFEB-altered RCC, is only positive in ~ 30% of TFE3-rearranged cases, mostly in PRCC::TFE3 t(X;1)(p11.2;q21) [85]. HMB-45 and Melan-A are also rarely positive in TFE3-rearranged RCCs and are more common in TFEB-altered RCCs. Epithelial markers, such as EMA, AE1/AE3, CK7, and Cam 5.2 are frequently patchy to negative in the TFE3-rearranged RCC [86]. PAX8 and cytokeratins are useful IHCs to differentiate RCCs from TFE3-rearranged melanotic neoplasms/PEComas [87]. Although TFE3 IHC is helpful, it does have limitations in practice and may show false-negative or false-positive expression, depending on the TFE3 clone and IHC platform used [85]. Thus, it is helpful to have strong nuclear TFE3 labeling in a clean background. A positive result, as well as an ambiguous result (e.g., focal nuclear positivity), requires molecular confirmation, either by FISH or NGS for RNA fusion [20, 88]. GPNMB (glycoprotein nonmetastatic B) has recently emerged as a promising IHC screening marker with reactivity in all TFE3-rearranged and TFEB-altered RCCs while demonstrating consistently low expression in PRCC [89].
Other exceedingly rare entities may present with focal papillary architecture with high-grade nuclei, as SDH-deficient RCCs, particularly those with SDHA mutation. The papillary component, however, is often seen in combination with other growth patterns including solid, cribriform, and desmoplastic [90,91,92,93]. This tumor demonstrates negative to focal positive staining for pancytokeratin and CK7 [20, 94]. Loss of SDHB on IHC can confirm the bi-allelic inactivation of any of the four SDH genes, including SDHA [20, 94]. Also, in the context of a very high-grade PRCC, collecting duct carcinoma (CDC) should also be considered, as it can exhibit a papillary or tubulopapillary component [20, 95]. However, CDC typically shows infiltrative growth, predominantly tubular pattern, and desmoplastic stroma. The key to the diagnosis of CDC lies in meticulously excluding other high-grade RCCs (e.g., FH-deficient RCC and SMARCB1-deficient renal medullary carcinoma), urothelial carcinoma, and metastasis through adequate gross sampling and the use of IHC panel [20, 95].
Novel and emerging renal entities with papillary morphology
Other renal entities that could be considered in the differential diagnosis of PRCC include two novel renal entities in the WHO 2022 classification—eosinophilic solid and cystic (ESC) RCC and anaplastic lymphoma kinase (ALK)-rearranged RCC [20, 96, 97] and one recently described, emerging renal entity, designated as “biphasic hyalinizing psammomatous” (BHP) RCC [20, 98].
ESC RCC may rarely show focal papillary morphology (< 10% cases) and scattered foamy histiocytic aggregates, which may bring PRCC in the differential, but it typically exhibits solid and cystic growth, with recognizable cytoplasmic stippling (granularity), and IHC reactivity for CK20, in the absence of CK7 [99, 100]. Sporadic ESC RCCs have shown recurrent, somatic bi-allelic losses or mutations in TSC2 and TSC1 and lack trisomy 7 and 17 [101]. These genetic changes result in dysregulation of the mTOR signaling pathway in ESC RCC.
ALK-rearranged RCC, another new renal entity, also frequently exhibits papillary growth, often admixed with other growth patterns, including solid, tubular, trabecular cystic, cribriform, and signet-ring cells [97, 102]. A mucinous component (intracellular or interstitial) is frequently found. Therefore, screening for ALK by IHC (for example, by monoclonal ALK antibody 5A4) or by molecular methods (FISH or NGS) should be performed in all renal tumors with variable patterns or unusual morphologies or containing a mucinous component [102].
BHP RCC is an emerging renal entity with a limited number of reported cases, usually exhibiting a prominent tubulopapillary architecture, fibrotic and hyalinized stroma, psammomatous microcalcification, a nonspecific IHC profile, often with CK7 reactivity, and frequent NF2 mutations [20, 103]. The differential diagnosis of BHP RCC is, however, broad and may include PRCC. Currently, it is uncertain whether NF2 abnormalities represent a specific feature in a group of related tumors or if they are a nonspecific finding, as they have been found in other RCC subtypes with various morphologies, including some advanced PRCCs [103].
Finally, if after careful diagnostic workup and exclusion of mimickers, the diagnosis of a papillary renal lesion is indeed PRCC with high-grade, former type 2–like morphology, this should be simply reported as a PRCC and graded according to current WHO/ISUP criteria.
Current paradigms in PRCC treatment and why does it matter
PRCC tumors limited to the kidney can be managed with partial or radical nephrectomy, ablation, or active surveillance [104]. Small renal masses (≤ 4 cm) exhibit minimal metastatic propensity, making active surveillance a viable option [105], with renal biopsy representing a crucial diagnostic tool in dictating the management of this subset. In PRCC cases with mixed morphology due the intratumoral heterogeneity, grading on renal biopsy might be inaccurate [47], and other markers such as ABCC2 could be supplemented for prognostication.
For locally advanced and metastatic PRCCs, the latest NCCN [104] and ESMO [105] guidelines recommend cabozantinib as the preferred option with savolitinib, sunitinib, and pembroluzimab as alternatives. Cabozantinib [106] and savolitinib [107], both targeting MET, have shown better responses than sunitinib. Additionally, MET status was reported to be predictive of treatment responses to MET inhibitors [107, 108]. Nonetheless, about 60% of locally advanced and metastatic diseases do not harbor MET alterations [109]; thus, MET-targeted therapies might not be optimal for MET-independent PRCC tumors, and targeting alternative pathways like NRF2-ARE could be more effective in treating these tumors. Pembrolizumab, a PD1 inhibitor, has shown promising results among PRCC patients [110]. High PD-L1 expression (combined positive score ≥ 1) correlates with better clinical response [110], but further studies are needed to validate its predictive value in PRCC immunotherapy. In addition, the tumor microenvironment of metastatic PRCCs appears to be diverse [111, 112] suggesting potential variability in response to such immunotherapy.
Data availability
No original research findings were presented in this article; it only reviewed and discussed findings from previously published research articles.
References
Angori S, Lobo J, Moch H (2022) Papillary renal cell carcinoma: current and controversial issues. Curr Opin Urol 32(4):344–351. https://doi.org/10.1097/MOU.0000000000001000
Williamson SR, Hartmann A, Hes O et al (2022) Papillary renal cell carcinoma. In: WHO classification of tumours editorial board. Urinary and male genital tumours, vol 8, 5th edn. International Agency for Research on Cancer, Lyon (France), pp 47–49 https://publications.iarc.fr/610
Mancilla-Jimenez R, Stanley RJ, Blath RA (1976) Papillary renal cell carcinoma: a clinical, radiologic, and pathologic study of 34 cases. Cancer 38:2469–2480. https://doi.org/10.1002/1097-0142(197612)38:6<2469::aid-cncr2820380636>3.0.co;2-r
Delahunt B, Eble JN (1997) Papillary renal cell carcinoma: a clinicopathologic and immunohistochemical study of 105 tumors. Mod Pathol 10:537–544
Mejean A, Hopirtean V, Bazin JP et al (2003) Prognostic factors for the survival of patients with papillary renal cell carcinoma: meaning of histological typing and multifocality. J Urol 170(3):764–767. https://doi.org/10.1097/01.ju.0000081122.57148.ec
Allory Y, Ouazana D, Boucher E et al (2003) Papillary renal cell carcinoma. Prognostic value of morphological subtypes in a clinicopathologic study of 43 cases. Virchows Arch 442(4):336–342. https://doi.org/10.1007/s00428-003-0787-1
Delahunt B, Eble JN, McCredie MR et al (2001) Morphologic typing of papillary renal cell carcinoma: comparison of growth kinetics and patient survival in 66 cases. Hum Pathol 32(6):590–595. https://doi.org/10.1053/hupa.2001.24984
Klatte T, Pantuck AJ, Said JW et al (2009) Cytogenetic and molecular tumor profiling for type 1 and type 2 papillary renal cell carcinoma. Clin Cancer Res 15(4):1162–1169. https://doi.org/10.1158/1078-0432.CCR-08-1229
Sukov WR, Lohse CM, Leibovich BC et al (2012) Clinical and pathological features associated with prognosis in patients with papillary renal cell carcinoma. J Urol 187(1):54–59. https://doi.org/10.1016/j.juro.2011.09.053
Le X, Wang X-B, Zhao H et al (2020) Comparison of clinicopathologic parameters and oncologic outcomes between type 1 and type 2 papillary renal cell carcinoma. BMC Urol 20(1):148. https://doi.org/10.1186/s12894-020-00716-0
Polifka I, Agaimy A, Herrmann E et al (2019) High proliferation rate and TNM stage but not histomorphological subtype are independent prognostic markers for overall survival in papillary renal cell carcinoma. Hum Pathol 83:212–223. https://doi.org/10.1016/j.humpath.2018.08.006
Linehan WM, Spellman P, Ricketts C et al (2016) Comprehensive molecular characterization of papillary renal-cell carcinoma. N Engl J Med 374(2):135–145. https://doi.org/10.1056/NEJMoa1505917
Chevarie-Davis M, Riazalhosseini Y, Arseneault M et al (2014) The morphologic and immunohistochemical spectrum of papillary renal cell carcinoma: study including 132 cases with pure type 1 and type 2 morphology as well as tumors with overlapping features. Am J Surg Pathol 38(7):887–894. https://doi.org/10.1097/PAS.0000000000000247
Saleeb RM, Plant P, Tawedrous E et al (2018) Integrated phenotypic/genotypic analysis of papillary renal cell carcinoma subtypes: identification of prognostic markers, cancer-related pathways, and implications for therapy. Eur Urol Focus 4(5):740–748. https://doi.org/10.1016/j.euf.2016.09.002
Saleeb RM, Brimo F, Farag M et al (2017) Toward biological subtyping of papillary renal cell carcinoma with clinical implications through histologic, immunohistochemical, and molecular analysis. Am J Surg Pathol 41(12):1618–1629. https://doi.org/10.1097/PAS.0000000000000962
Murugan P, Jia L, Dinatale RG et al (2022) Papillary renal cell carcinoma: a single institutional study of 199 cases addressing classification, clinicopathologic and molecular features, and treatment outcome. Mod Pathol 35(6):825–835. https://doi.org/10.1038/s41379-021-00990-9
Yang C, Shuch B, Kluger H et al (2020) High WHO/ISUP grade and unfavorable architecture, rather than typing of papillary renal cell carcinoma, may be associated with worse prognosis. Am J Surg Pathol 44:582–593. https://doi.org/10.1097/PAS.0000000000001455
Xiong S, Zhu W, Li X et al (2021) Whether histologic subtyping affect the oncological outcomes of patients with papillary renal cell carcinoma: evidence from a systematic review and meta-analysis. Transl Androl Urol 10(8):3255–3266. https://doi.org/10.21037/tau-21-329
Pignot G, Elie C, Conquy S et al (2007) Survival analysis of 130 patients with papillary renal cell carcinoma: prognostic utility of type 1 and type 2 subclassification. Urology 69(2):230–235. https://doi.org/10.1016/j.urology.2006.09.052
Trpkov K, Hes O, Williamson SR et al (2021) New developments in existing WHO entities and evolving molecular concepts: the Genitourinary Pathology Society (GUPS) update on renal neoplasia. Mod Pathol 34(7):1392–1424. https://doi.org/10.1038/s41379-021-00779-w
Przybycin CG (2024) Papillary renal cell carcinoma: evolving classification by combined morphologic and molecular means. Adv Anat Pathol 31(3):147–156. https://doi.org/10.1097/PAP.0000000000000434
Wang Q, Zhang Y, Zhang B et al (2022) Single-cell chromatin accessibility landscape in kidney identifies additional cell-of-origin in heterogenous papillary renal cell carcinoma. Nat Commun 13(1):31. https://doi.org/10.1038/s41467-021-27660-3
Al-Obaidy KI, Saleeb RM, Trpkov K et al (2022) Recurrent KRAS mutations are early events in the development of papillary renal neoplasm with reverse polarity. Mod Pathol 35(9):1279–1286. https://doi.org/10.1038/s41379-022-01018-6
Molinié V, Balaton A, Rotman S et al (2006) Alpha-methyl CoA racemase expression in renal cell carcinomas. Hum Pathol 37(6):698–703. https://doi.org/10.1016/j.humpath.2006.01.012
Jedlitschky G, Hoffmann U, Kroemer HK (2006) Structure and function of the MRP2 (ABCC2) protein and its role in drug disposition. Expert Opin Drug Metabol Toxicol 2:351–366. https://doi.org/10.1517/17425255.2.3.351
Saleeb RM, Brimo F, Gao Y et al (2022) ABCC2 expression in papillary renal cell carcinoma provides better prognostic stratification than WHO/ISUP nucleolar grade. Hum Pathol 120:57–70. https://doi.org/10.1016/j.humpath.2021.12.006
Castillo VF, Masoomian M, Trpkov K et al (2023) ABCC2 brush-border expression predicts outcome in papillary renal cell carcinoma: a multi-institutional study of 254 cases. Histopathology 83(6):949–958. https://doi.org/10.1111/his.15042
Muriithi W, Macharia LW, Heming CP et al ABC transporters and the hallmarks of cancer: roles in cancer aggressiveness beyond multidrug resistance. Cancer Biol Med 17(2):253–269. https://doi.org/10.20892/j.issn.2095-3941.2019.0284
Saleeb RM, Farag M, Lichner Z et al (2018) Modulating ATP binding cassette transporters in papillary renal cell carcinoma type 2 enhances its response to targeted molecular therapy. Mol Oncol 12(10):1673–1688. https://doi.org/10.1002/1878-0261.12346
Ishihara H, Yamashita S, Liu Y-Y et al (2020) Genetic and epigenetic profiling indicates the proximal tubule origin of renal cancers in end-stage renal disease. Cancer Sci 111(11):4276–4287. https://doi.org/10.1111/cas.14633
Wang KL, Weinrach DM, Luan C et al (2007) Renal papillary adenoma--a putative precursor of papillary renal cell carcinoma. Hum Pathol 38(2):239–246. https://doi.org/10.1016/j.humpath.2006.07.016
Jones TD, Eble JN, Wang M et al (2005) Molecular genetic evidence for the independent origin of multifocal papillary tumors in patients with papillary renal cell carcinomas. Clin Cancer Res 11(20):7226–7233. https://doi.org/10.1158/1078-0432.CCR-04-2597
Lindgren D, Boström A-K, Nilsson K et al (2011) Isolation and characterization of progenitor-like cells from human renal proximal tubules. Am J Pathol 178(2):828–837. https://doi.org/10.1016/j.ajpath.2010.10.026
Hes O, Síma R, Nemcová J et al (2008) End-stage kidney disease: gains of chromosomes 7 and 17 and loss of Y chromosome in non-neoplastic tissue. Virchows Arch 453(4):313–319. https://doi.org/10.1007/s00428-008-0661-2
Hartmann A, Cheville J, Hes O et al (2022) Renal papillary adenoma. In: WHO Classification of Tumours Editorial Board. Urinary and male genital tumours, vol 8, 5th edn. International Agency for Research on Cancer, Lyon (France), pp 47–49 https://publications.iarc.fr/610
Saleeb RM, Farag M, Ding Q et al (2019) Integrated molecular analysis of papillary renal cell carcinoma and precursor lesions unfolds evolutionary process from kidney progenitor-like cells. Am J Pathol 189(10):2046–2060. https://doi.org/10.1016/j.ajpath.2019.07.002
Pitra T, Pivovarcikova K, Alaghehbandan R et al (2019) Chromosomal numerical aberration pattern in papillary renal cell carcinoma: review article. Ann Diagn Pathol 40:189–199. https://doi.org/10.1016/j.anndiagpath.2017.11.004
Marsaud A, Dadone B, Ambrosetti D et al (2015) Dismantling papillary renal cell carcinoma classification: the heterogeneity of genetic profiles suggests several independent diseases: Heterogeneity of Papillary Renal Cell Carcinomas. Genes Chromosomes Cancer 54(6):369–382. https://doi.org/10.1002/gcc.22248
Lubensky IA, Schmidt L, Zhuang Z et al (1999) Hereditary and sporadic papillary renal carcinomas with c-met mutations share a distinct morphological phenotype. Am J Pathol 155(2):517–526. https://doi.org/10.1016/S0002-9440(10)65147-4
Yang Y, Ricketts CJ, Vocke CD et al (2021) Characterization of genetically defined sporadic and hereditary type 1 papillary renal cell carcinoma cell lines. Genes Chromosomes Cancer 60(6):434–446. https://doi.org/10.1002/gcc.22940
Wood GE, Hockings H, Hilton DM et al (2021) The role of MET in chemotherapy resistance. Oncogene 40(11):1927–1941. https://doi.org/10.1038/s41388-020-01577-5
Haas NB, Nathanson KL (2014) Hereditary kidney cancer syndromes. Adv Chronic Kidney Dis 21(1):81–90. https://doi.org/10.1053/j.ackd.2013.10.001
Bailey ST, Smith AM, Kardos J et al (2017) MYC activation cooperates with Vhl and Ink4a/Arf loss to induce clear cell renal cell carcinoma. Nat Commun 8(1):15770. https://doi.org/10.1038/ncomms15770
Delahunt B, Cheville JC, Martignoni G et al (2013) The International Society of Urological Pathology (ISUP) grading system for renal cell carcinoma and other prognostic parameters. Am J Surg Pathol 37(10):1490–1504. https://doi.org/10.1097/PAS.0b013e318299f0fb
Cornejo KM, Dong F, Zhou AG et al (2015) Papillary renal cell carcinoma: correlation of tumor grade and histologic characteristics with clinical outcome. Hum Pathol 46(10):1411–1417. https://doi.org/10.1016/j.humpath.2015.07.001
Srigley J, Paner G, Zhou M, et al (2021) Protocol for the examination of specimens from patients with invasive carcinoma of renal tubular origin, version 4.1.0.0. College of American Pathologists. https://documents.cap.org/protocols/Kidney_4.1.0.0.REL_CAPCP.pdf?_gl=1*1hx8iia*_ga*MjA3NzY1ODg4Ni4xNzE3NDE5NjE0*_ga_97ZFJSQQ0X*MTcxNzQxOTYxNC4xLjEuMTcxNzQxOTgxNi4wLjAuMA. Accessed 03 June 2024
Prendeville S, Richard PO, Jewett MAS et al (2019) Accuracy of renal tumour biopsy for the diagnosis and subtyping of papillary renal cell carcinoma: analysis of paired biopsy and nephrectomy specimens with focus on discordant cases. J Clin Pathol 72(5):363–367. https://doi.org/10.1136/jclinpath-2018-205655
Chan E, Stohr BA, Butler RS et al (2022) Papillary renal cell carcinoma with microcystic architecture is strongly associated with extrarenal invasion and metastatic disease. Am J Surg Pathol 46(3):392–403. https://doi.org/10.1097/PAS.0000000000001802
Ulamec M, Skenderi F, Trpkov K et al (2016) Solid papillary renal cell carcinoma: clinicopathologic, morphologic, and immunohistochemical analysis of 10 cases and review of the literature. Ann Diagn Pathol 23:51–57. https://doi.org/10.1016/j.anndiagpath.2016.04.008
Petersson F, Bulimbasic S, Hes O et al (2012) Biphasic alveolosquamoid renal carcinoma: a histomorphological, immunohistochemical, molecular genetic, and ultrastructural study of a distinctive morphologic variant of renal cell carcinoma. Ann Diagn Pathol 16(6):459–469. https://doi.org/10.1016/j.anndiagpath.2012.08.007
Hes O, Condom Mundo E, Peckova K et al (2016) Biphasic squamoid alveolar renal cell carcinoma: a distinctive subtype of papillary renal cell carcinoma? Am J Surg Pathol 40(5):664–675. https://doi.org/10.1097/PAS.0000000000000639
Renshaw AA, Zhang H, Corless CL et al (1997) Solid variants of papillary (chromophil) renal cell carcinoma: clinicopathologic and genetic features. Am J Surg Pathol 21(10):1203–1209. https://doi.org/10.1097/00000478-199710000-00011
Chartier S, Méjean A, Richard S et al (2017) Biphasic squamoid alveolar renal cell carcinoma: 2 cases in a family supporting a continuous spectrum with papillary type I renal cell carcinoma. Am J Surg Pathol 41(7):1011–1012. https://doi.org/10.1097/PAS.0000000000000870
Denize T, Just PA, Sibony M et al (2021) MET alterations in biphasic squamoid alveolar papillary renal cell carcinomas and clinicopathological features. Mod Pathol 34(3):647–659. https://doi.org/10.1038/s41379-020-0645-6
Nova-Camacho LM, Acosta AM, Akgul M et al (2024) Biphasic papillary (biphasic squamoid alveolar) renal cell carcinoma: a clinicopathologic and molecular study of 17 renal cell carcinomas including 10 papillary adenomas. Virchows Arch 484(3):441–449. https://doi.org/10.1007/s00428-024-03768-x
Trpkov K, Athanazio D, Magi-Galluzzi C et al (2018) Biphasic papillary renal cell carcinoma is a rare morphological variant with frequent multifocality: a study of 28 cases. Histopathology 72(5):777–785. https://doi.org/10.1111/his.13432
Kunju LP, Wojno K, Wolf JS Jr et al (2008) Papillary renal cell carcinoma with oncocytic cells and nonoverlapping low grade nuclei: expanding the morphologic spectrum with emphasis on clinicopathologic, immunohistochemical and molecular features. Hum Pathol 39(1):96–101. https://doi.org/10.1016/j.humpath.2007.05.016
Han G, Yu W, Chu J et al (2017) Oncocytic papillary renal cell carcinoma: a clinicopathological and genetic analysis and indolent clinical course in 14 cases. Pathol Res Pract 213(1):1–6. https://doi.org/10.1016/j.prp.2016.04.009
Park B-H, Ro JY, Park WS et al (2009) Oncocytic papillary renal cell carcinoma with inverted nuclear pattern: distinct subtype with an indolent clinical course. Pathol Int 59(3):137–146. https://doi.org/10.1111/j.1440-1827.2009.02341.x
Al-Obaidy KI, Eble JN, Cheng L et al (2019) Papillary renal neoplasm with reverse polarity: a morphologic, immunohistochemical, and molecular study. Am J Surg Pathol 43(8):1099–1111. https://doi.org/10.1097/PAS.0000000000001288
Al-Obaidy KI, Eble JN, Nassiri M et al (2020) Recurrent KRAS mutations in papillary renal neoplasm with reverse polarity. Mod Pathol 33(6):1157–1164. https://doi.org/10.1038/s41379-019-0362-1
Wei S, Kutikov A, Patchefsky AS et al (2022) Papillary renal neoplasm with reverse polarity is often cystic: report of 7 cases and review of 93 cases in the literature. Am J Surg Pathol 46(3):336–343. https://doi.org/10.1097/PAS.0000000000001773
Castillo VF, Trpkov K, Van der Kwast T et al (2024) Papillary renal neoplasm with reverse polarity is biologically and clinically distinct from eosinophilic papillary renal cell carcinoma. Pathol Int 74(4):222–226. https://doi.org/10.1111/pin.13417
Tong K, Zhu W, Fu H et al (2020) Frequent KRAS mutations in oncocytic papillary renal neoplasm with inverted nuclei. Histopathology 76(7):1070–1083. https://doi.org/10.1111/his.14084
Skenderi F, Ulamec M, Vanecek T et al (2017) Warthin-like papillary renal cell carcinoma: clinicopathologic, morphologic, immunohistochemical and molecular genetic analysis of 11 cases. Ann Diagn Pathol 27:48–56. https://doi.org/10.1016/j.anndiagpath.2017.01.005
Li XF, Wang ZJ, Zhang HM et al (2023) Warthin-like papillary renal cell carcinoma: a case report. World J Clin Cases 11(30):7450–7456. https://doi.org/10.12998/wjcc.v11.i30.7450
Tretiakova MS, Sahoo S, Takahashi M et al (2004) Expression of alpha-methylacyl-CoA racemase in papillary renal cell carcinoma. Am J Surg Pathol 28(1):69–76. https://doi.org/10.1097/00000478-200401000-00007
Cheville J, Helenon O, Hes O et al (2022) Clear cell papillary renal cell tumour. In: WHO Classification of Tumours Editorial Board. Urinary and male genital tumours, vol 8, 5th edn. International Agency for Research on Cancer, Lyon (France), pp 61–62 https://publications.iarc.fr/610
Weng S, DiNatale RG, Silagy A et al (2021) The clinicopathologic and molecular landscape of clear cell papillary renal cell carcinoma: implications in diagnosis and management. Eur Urol 79(4):468–477. https://doi.org/10.1016/j.eururo.2020.09.027
Mantilla JG, Antic T, Tretiakova M (2017) GATA3 as a valuable marker to distinguish clear cell papillary renal cell carcinomas from morphologic mimics. Hum Pathol 66:152–158. https://doi.org/10.1016/j.humpath.2017.06.016
Argani P, Cheng L, Hartmann A et al (2022) Metanephric adenoma. In: WHO Classification of Tumours Editorial Board. Urinary and male genital tumours, vol 8, 5th edn. International Agency for Research on Cancer, Lyon (France), pp 87–89 https://publications.iarc.fr/610
Kinney SN, Eble JN, Hes O et al (2015) Metanephric adenoma: the utility of immunohistochemical and cytogenetic analyses in differential diagnosis, including solid variant papillary renal cell carcinoma and epithelial-predominant nephroblastoma. Mod Pathol 28(9):1236–1248. https://doi.org/10.1038/modpathol.2015.81
Chen YB, Hes O, Kuroda N et al (2022) Mucinous tubular and spindle cell carcinoma. In: WHO Classification of Tumours Editorial Board. Urinary and male genital tumours, vol 8, 5th edn. International Agency for Research on Cancer, Lyon (France), pp 63–64 https://publications.iarc.fr/610
Peckova K, Martinek P, Sperga M et al (2015) Mucinous spindle and tubular renal cell carcinoma: analysis of chromosomal aberration pattern of low-grade, high-grade, and overlapping morphologic variant with papillary renal cell carcinoma. Ann Diagn Pathol 19(4):226–231. https://doi.org/10.1016/j.anndiagpath.2015.04.004
Pivovarcikova K, Peckova K, Martinek P et al (2016) “Mucin”-secreting papillary renal cell carcinoma: clinicopathological, immunohistochemical, and molecular genetic analysis of seven cases. Virchows Arch 469(1):71–80. https://doi.org/10.1007/s00428-016-1936-7
Wang L, Zhang Y, Chen Y-B et al (2018) VSTM2A overexpression is a sensitive and specific biomarker for mucinous tubular and spindle cell carcinoma (MTSCC) of the kidney. Am J Surg Pathol 42(12):1571–1584. https://doi.org/10.1097/PAS.0000000000001150
Ren Q, Wang L, Al-Ahmadie HA et al (2018) Distinct genomic copy number alterations distinguish mucinous tubular and spindle cell carcinoma of the kidney from papillary renal cell carcinoma with overlapping histologic features. Am J Surg Pathol 42(6):767–777. https://doi.org/10.1097/PAS.0000000000001038
Trpkov K, Hes O, Agaimy A et al (2016) Fumarate hydratase-deficient renal cell carcinoma is strongly correlated with fumarate hydratase mutation and hereditary leiomyomatosis and renal cell carcinoma syndrome. Am J Surg Pathol 40:865–875. https://doi.org/10.1097/PAS.0000000000000617
Moch H, Ohashi R, Gandhi JS et al (2018) Morphological clues to the appropriate recognition of hereditary renal neoplasms. Semin Diagn Pathol 35:184–192. https://doi.org/10.1053/j.semdp.2018.01.005
Muller M, Guillaud-Bataille M, Salleron J et al (2018) Pattern multiplicity and fumarate hydratase (FH)/S-(2-succino)-cysteine (2SC) staining but not eosinophilic nucleoli with perinucleolar halos differentiate hereditary leiomyomatosis and renal cell carcinoma-associated renal cell carcinomas from kidney tumors without FH gene alteration. Mod Pathol 31:974–983. https://doi.org/10.1038/s41379-018-0017-7
Chen YB, Brannon AR, Toubaji A et al (2014) Hereditary leiomyomatosis and renal cell carcinoma syndrome-associated renal cancer: recognition of the syndrome by pathologic features and the utility of detecting aberrant succination by immunohistochemistry. Am J Surg Pathol 38:627–637. https://doi.org/10.1097/PAS.0000000000000163
Anderson WJ, Tsai HK, Sholl LM et al (2022) A clinicopathological and molecular analysis of fumarate hydratase (FH)-deficient renal cell carcinomas with heterogeneous loss of FH expression. Int J Surg Pathol 30(6):606–615. https://doi.org/10.1177/10668969221074600
Liu Y, Dong Y, Gu Y et al (2022) GATA3 aids in distinguishing fumarate hydratase-deficient renal cell carcinoma from papillary renal cell carcinoma. Ann Diagn Pathol 60:152007. https://doi.org/10.1016/j.anndiagpath.2022.152007
Wyvekens N, Valtcheva N, Mischo A et al (2020) Novel morphological and genetic features of fumarate hydratase deficient renal cell carcinoma in HLRCC syndrome patients with a tailored therapeutic approach. Genes Chromosomes Cancer 59(11):611–619. https://doi.org/10.1002/gcc.22878
Tretiakova MS (2022) Chameleon TFE3-translocation RCC and how gene partners can change morphology: accurate diagnosis using contemporary modalities. Adv Anat Pathol 29(3):131–140. https://doi.org/10.1097/PAP.0000000000000332
Argani P, Hicks J, De Marzo AM et al (2010) Xp11 translocation renal cell carcinoma (RCC): extended immunohistochemical profile emphasizing novel RCC markers. Am J Surg Pathol 34(9):1295–1303. https://doi.org/10.1097/PAS.0b013e3181e8ce5b
Saleeb RM, Srigley JR, Sweet J et al (2017) Melanotic MiT family translocation neoplasms: expanding the clinical and molecular spectrum of this unique entity of tumors. Pathol Res Pract 213(11):1412–1418. https://doi.org/10.1016/j.prp.2017.08.004
Green W, Yonescu R, Morsberger L et al (2013) Utilization of a TFE3 break-apart FISH assay in a renal tumor consultation service. Am J Surg Pathol 37:1150–1163. https://doi.org/10.1097/PAS.0b013e31828a69ae
Salles DC, Asrani K, Woo J et al (2022) GPNMB expression identifies TSC1/2/mTOR-associated and MiT family translocation-driven renal neoplasms. J Pathol 257(2):158–171. https://doi.org/10.1002/path.5875
Yakirevich E, Ali SM, Mega A et al (2015) A novel SDHA-deficient renal cell carcinoma revealed by comprehensive genomic profiling. Am J Surg Pathol 39(6):858–863. https://doi.org/10.1097/PAS.0000000000000403
Ozluk Y, Taheri D, Matoso A et al (2015) Renal carcinoma associated with a novel succinate dehydrogenase A mutation: a case report and review of literature of a rare subtype of renal carcinoma. Hum Pathol 46(12):1951–1955. https://doi.org/10.1016/j.humpath.2015.07.027
Jiang Q, Zhang Y, Zhou Y-H et al (2015) A novel germline mutation in SDHA identified in a rare case of gastrointestinal stromal tumor complicated with renal cell carcinoma. Int J Clin Exp Pathol 8(10):12188–12197
McEvoy CR, Koe L, Choong DY et al (2018) SDH-deficient renal cell carcinoma associated with biallelic mutation in succinate dehydrogenase A: comprehensive genetic profiling and its relation to therapy response. NPJ Precis Oncol 2:9. https://doi.org/10.1038/s41698-018-0053-2
Hes O, Gill AJ, Jimenez RE et al (2022) Succinate dehydrogenase-deficient renal cell carcinoma. In: WHO Classification of Tumours Editorial Board. Urinary and male genital tumours, vol 8, 5th edn. International Agency for Research on Cancer, Lyon (France), pp 80–81 https://publications.iarc.fr/610
Chen YB, Colecchia M, Comperat EM et al (2022) Collecting duct carcinoma. In: WHO Classification of Tumours Editorial Board. Urinary and male genital tumours, vol 8, 5th edn. International Agency for Research on Cancer, Lyon (France), pp 59–60 https://publications.iarc.fr/610
Argani P, Hartmann A, Hes O et al (2022) Eosinophilic solid and cystic renal cell carcinoma. In: WHO Classification of Tumours Editorial Board. Urinary and male genital tumours, vol 8, 5th edn. International Agency for Research on Cancer, Lyon (France), pp 69–70 https://publications.iarc.fr/610
Argani P, Inamura K, Williamson SR et al (2022) ALK-rearranged renal cell carcinoma. In: WHO Classification of Tumours Editorial Board. Urinary and male genital tumours, vol 8, 5th edn. International Agency for Research on Cancer, Lyon (France), pp 82–83 https://publications.iarc.fr/610
Argani P, Reuter VE, Eble JN et al (2020) Biphasic hyalinizing psammomatous renal cell carcinoma (BHP RCC): a distinctive neoplasm associated with somatic NF2 mutations. Am J Surg Pathol 44(7):901–916. https://doi.org/10.1097/PAS.0000000000001467
Trpkov K, Hes O, Bonert M et al (2016) Eosinophilic, solid, and cystic renal cell carcinoma: clinicopathologic study of 16 unique, sporadic neoplasms occurring in women. Am J Surg Pathol 40(1):60–71. https://doi.org/10.1097/PAS.0000000000000508
Trpkov K, Abou-Ouf H, Hes O et al (2017) Eosinophilic solid and cystic renal cell carcinoma (ESC RCC): further morphologic and molecular characterization of ESC RCC as a distinct entity. Am J Surg Pathol 41(10):1299–1308. https://doi.org/10.1097/PAS.0000000000000838
Mehra R, Vats P, Cao X et al (2018) Somatic bi-allelic loss of TSC genes in eosinophilic solid and cystic renal cell carcinoma. Eur Urol 74(4):483–486. https://doi.org/10.1016/j.eururo.2018.06.007
Kuroda N, Trpkov K, Gao Y et al (2020) ALK rearranged renal cell carcinoma (ALK-RCC): a multi-institutional study of twelve cases with identification of novel partner genes CLIP1, KIF5B and KIAA1217. Mod Pathol 33(12):2564–2579. https://doi.org/10.1038/s41379-020-0578-0
Yakirevich E, Pavlick DC, Perrino CM et al (2021) NF2 tumor suppressor gene inactivation in advanced papillary renal cell carcinoma. Am J Surg Pathol 45(5):716–718. https://doi.org/10.1097/PAS.0000000000001586
Motzer RJ, Jonasch E, Agarwal N et al (2022) Kidney cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 20(1):71–90. https://doi.org/10.6004/jnccn.2022.0001
Powles T, Albiges L, Bex A et al (2021) ESMO clinical practice guideline update on the use of immunotherapy in early stage and advanced renal cell carcinoma. Ann Oncol 32(12):1511–1519. https://doi.org/10.1016/j.annonc.2021.09.014
Pal SK, Tangen CM, Thompson IM et al (2017) A randomized, phase II efficacy assessment of multiple MET kinase inhibitors in metastatic papillary renal carcinoma (PRCC): SWOG S1500. J Clin Oncol 35(15). https://doi.org/10.1200/JCO.2017.35.15_suppl.TPS459
Choueiri TK, Plimack E, Arkenau HT et al (2017) Biomarker-based Phase II trial of savolitinib in patients with advanced papillary renal cell cancer. J Clin Oncol 35:2993–3001. https://doi.org/10.1200/JCO.2017.72.2967
Choueiri TK, Vaishampayan U, Rosenberg JE et al (2013) Phase II and biomarker study of the dual MET/VEGFR2 inhibitor foretinib in patients with papillary renal cell carcinoma. J Clin Oncol 31:181e6. https://doi.org/10.1200/JCO.2012.43.3383
Albiges L, Heng DYC, Lee JL et al (2022) Impact of MET status on treatment outcomes in papillary renal cell carcinoma: a pooled analysis of historical data. Eur J Cancer 170:158–168. https://doi.org/10.1016/j.ejca.2022.04.021
McDermott DF, Lee JL, Ziobro M et al (2021) Open-label, single-arm, Phase II study & of pembrolizumab monotherapy as first-line therapy in patients with advanced non-clear cell renal cell carcinoma. J Clin Oncol 39:1029–1039. https://doi.org/10.1200/JCO.20.02365
de Vries-Brilland M, Rioux-Leclercq N, Meylan M et al (2023) Comprehensive analyses of immune tumor microenvironment in papillary renal cell carcinoma. J Immunother Cancer 11(11):e006885–e006885. https://doi.org/10.1136/jitc-2023-006885
Castillo V, van der Kwast T, Trpkov K et al (2024) Immune landscape and PD-L1 expression of papillary renal cell carcinoma with ABCC2 brush border reactivity. USCAP abstracts: Genitourinary pathology (including renal tumors). Lab Invest 104(3):S917–S918. https://doi.org/10.1016/j.labinv.2024.101057
Funding
RS received support from the Ontario Institute for Cancer Research through funding provided by the government of Ontario (grant number IA-1-024).
Author information
Authors and Affiliations
Contributions
RS conceptualized the review topic and outlined the structure of the article. VC, KT, and RS contributed to the literature review and analysis. VC drafted the manuscript and prepared the figures. RS and KT provided critical revisions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This is a review article that did not use tissue samples or involve human subjects; therefore, ethical approval was not necessary.
Informed consent
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 3733 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Castillo, V.F., Trpkov, K. & Saleeb, R. Contemporary review of papillary renal cell carcinoma—current state and future directions. Virchows Arch 485, 391–405 (2024). https://doi.org/10.1007/s00428-024-03865-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-024-03865-x