Abstract
In isolated segments of the rat proximal colon, the dopamine reuptake inhibitor GBR 12909 (GBR) causes a dilatation, while the D1-like receptor antagonist SCH 23390 (SCH) induces a tonic constriction, suggesting that neurally released dopamine tonically stimulates enteric inhibitory efferent neurons. Here, the targets of the enteric dopaminergic neurons were investigated. Cannulated segments of rat proximal colon were bathed in physiological salt solution and luminally perfused with 0.9% saline, while all drugs were applied to the bath. Spatio-temporal maps of colonic motility were constructed from video recordings of peristaltic contractions, and the maximum diameter was measured as an index of colonic contractility. GBR (1 μM)-induced dilatations of colonic segments were prevented by SCH (5 μM), L-nitro arginine (L-NA; 100 μM), a nitric oxide synthase inhibitor, or tetrodotoxin (0.6 μM). In contrast, constrictions induced by a higher concentration of SCH (20 μM) were unaffected by either L-NA or tetrodotoxin. The vasoactive intestinal peptide (VIP) receptor antagonist VIP10-28 (3 μM) or P2Y1 receptor antagonist MRS 2500 (1 μM) had no effect on either the GBR-induced dilatation or the SCH-induced constriction. In colonic segments that had been pretreated with 6-hydroxydopamine (100 μM, 3 h) to deplete enteric dopamine, GBR failed to increase the colonic diameter, while SCH was still capable of constricting colonic segments. Enteric dopaminergic neurons appear to project to nitrergic neurons to dilate the proximal colon by activating neuronal D1-like receptors. In addition, constitutively activated D1-like receptors expressed in cells yet to be determined may provide a tonic inhibition on colonic constrictions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The enteric nervous system (ENS), where a complex network of afferent and efferent neurons is functionally modulated by interneurons, plays pivotal roles in regulating intestinal peristalsis. Excitatory efferent neurons release acetylcholine or substance P to contract smooth muscle cells, while their relaxation is mediated by nitric oxide (NO), vasoactive intestinal peptide (VIP), or purines released from inhibitory efferents [8, 15]. In the proximal colon, dopamine released from interneurons appears to bind to dopamine D1-like receptors, including D1 and D5 receptors [24], expressed in both nitrergic and cholinergic neurons to modulate colonic motility [1, 18, 19, 27].
In isolated colonic segments, GBR 12909 (GBR), a selective dopamine reuptake inhibitor, increases the maximum diameter with a reduction in the frequency of peristaltic waves as does sodium nitroprusside, an NO donor. SCH 23390 (SCH), a D1-like receptor antagonist, decreases the maximum diameter and slows or prevents colonic peristalsis, as is also the case upon the blockade of nitrergic transmission using L-nitro arginine (L-NA), an NO synthase (NOS) inhibitor. Thus, neurally released dopamine appears to predominantly stimulate nitrergic neurons, while having a lesser effect of cholinergic neurons [27]. Yet, the precise target neurons of enteric dopaminergic neurons in colonic segments remain to be determined.
In colonic muscle strips, exogenous dopamine attenuates cholinergic nerve-mediated contractions by activating D1-like receptors that are presumably located in nitrergic and purinergic neurons [2]. However, SCH-induced enlargement of spontaneous or cholinergic nerve-mediated contractions is not inhibited by either tetrodotoxin (TTX), a NOS inhibitor or a P2Y1 receptor antagonist [2], suggesting that constitutively active D1-like receptors may also be expressed in a population of cells within the colonic wall exerting tonic inhibition of colonic contractility.
In this study, the cellular target(s) of enteric dopaminergic neurons was further investigated by analyzing the motility of isolated segments of the rat proximal colon using spatio-temporal mapping techniques. Since dopaminergic neurons exert inhibitory effects on the colonic motility, the cellular target(s) was explored with a particular focus on nitrergic, VIP or purinergic neurons. In addition, the effects of neuronal dopamine depletion with 6-hydroxydopamine (6-OHDA) on the colonic motility was examined to explore if constitutively active D1-like receptors may contribute to dopaminergic inhibition of the colonic motility [31].
Materials and methods
Ethical approval
Male Wistar rats (Japan SLC, Shizuoka, Japan) were housed under a 12:12 h light/dark cycle at 23 ± 1 °C with free access to food and water. The experimental procedures were performed according to the guidelines for the care and use of laboratory animals approved by The Experimental Animal Committee of the Nagoya City University Graduate School of Medical Sciences (Approval no: H30M-27).
Video imaging of colonic motility
Rats aged 6–7 weeks were used for a series of experiments. All rats were decapitated, segments of the proximal colon with a length of approximately 5–6 cm were removed and immersed in physiological salt solution (PSS). Luminal contents in the colonic segments were emptied by PSS flushing, and then the segments were placed in a 30 mL volume of organ bath that was continuously perfused with warmed (36 °C) and oxygenated (95% O2 + 5% CO2) PSS at 3.5 mL min−1. The oral ends of the colonic segments were cannulated via an L-shaped attachment, and luminally perfused with degassed 0.9% saline at 1.5 mL min−1 using a peristaltic pump. The aboral ends of the colonic segments were cannulated to another L-shaped attachment, and its outlet was connected to a one-way valve to prevent backflow of saline. The level of outflow was set to 4 cm above the colonic segments to provide a suitable backpressure. Colonic segments were initially allowed to develop stable peristaltic contractions for about 1 h, and then only a single experimental protocol in which the drug was applied in the bath solution was conducted on individual colonic segments. All experiments were performed during the light period.
Wall motion of colonic segments was recorded using a digital video camera (HDR-XR500V; Sony, Tokyo, Japan), positioned above the segment. The videos were converted into spatio-temporal maps of diameter changes (DMaps) using custom-made software [5, 26]. The initial 1 cm of the oral end and 1.5 cm of the aboral end were excluded for making the DMaps. Regions of maximum diameter (dilatation) were represented on DMaps as black pixels, whereas that of minimum diameter (contraction) was represented as white pixels.
6-OHDA lesion model
The 6-OHDA lesion model rats were prepared using a method modified from previously published protocols [11, 23]. Briefly, the total dose of 6-OHDA remained unchanged (300 mg kg−1), while the treatment period was increased from 1 to 4 weeks to avoid interfering with body weight loss. Rats aged 3 weeks were administered intraperitoneally with 6-OHDA (100 mg kg−1) or vehicle 3 times, on day 0, day 7, and day 14. Experiments were performed on days 28–30 (7-week-old).
Solutions
The composition of PSS was (in mM) as follows: Na+, 137.5; K+, 5.9; Ca2+, 2.5; Mg2+, 1.2; HCO3−, 15.5; H2PO4−, 1.2; Cl−, 134 and glucose, 11.5. The drugs used were GBR, dopamine (Tokyo Chemical Industry, Tokyo, Japan), SCH, L-NA, propranolol, phentolamine, guanethidine (Sigma-Aldrich, St. Louis, MO, USA), VIP10-28 (AnyGen Co., Ltd, Gwang-ju, Korea), MRS 2500 (MRS; Tocris Bioscience, Bristol, UK), TTX, desipramine (Wako Pure Chemical Industries, Osaka, Japan), and 6-OHDA (LKT Laboratories, Inc., St. Paul, MN, USA). 6-OHDA was dissolved in 0.1% ascorbic acid in 0.9% saline. Other drugs were dissolved in deionized water.
Concentrations of GBR (1 μM) [27], SCH (5 or 20 μM) [27], VIP10-28 (3 μM) [13], MRS (1 μM) [15], dopamine (3 μM) [27], 6-OHDA (100 μM) [22], or desipramine (0.1 μM) [7] were chosen based on previous studies.
Data analysis
Data are expressed as mean ± SD (where n is number of preparations as well as animals). One- or two-way repeated-measures analysis of variance (RM-ANOVA) followed by post hoc Bonferroni multiple comparisons test, unpaired Student’s t-test or Fisher’s exact test was used to examine the effects of drugs. P-values < 0.05 were considered to be statistically significant. Control parameters, namely, the maximum diameter and frequency of peristalsis, were measured for 5-min periods immediately prior to drug application. Effects of the drugs on the parameters were analyzed for 5-min periods 5 min after drug application, except for the treatment with GBR for 30 min or 6-OHDA for 3 h. The peristaltic waves were defined as contractile waves originated at the oral end of the DMaps that propagated along its entire length to the aboral end. Peristaltic contractions were defined as the regions where the colonic diameter was reduced to less than 75% of its basal values in the measured 5-min period (Supplemental Fig. 1).
Results
In isolated colonic segments with a maximum diameter of 9.21 ± 0.54 mm, peristaltic waves propagated from the oral to aboral end were periodically generated at a frequency, 2.8 ± 0.9 5 min−1 (n = 97 animals). Since the inhibition of nitrergic neurons invariably disrupted or abolished peristaltic contractions [27], changes in the maximum diameters but not the frequency of peristaltic waves were used as a primary index of the colonic contractility. To adjust variations in the basal diameter among samples, after one- or two-way RM-ANOVA using raw data of the maximum diameter, the comparisons among multiple groups were performed using normalized data (% of max diameter).
Consistent with our previous report [27], the inhibition of neuronal dopamine reuptake with bath-applied GBR (1 μM, 5–10 min) increased the basal diameter of colonic segments without changing the frequency of peristaltic waves (Fig. 1a-d). Prolonged application of GBR further increased the colonic diameter over time periods of 15–20 min and 25–30 min (Fig. 1a-c) and reduced the peristaltic frequency during 15–20 min period (Fig. 1d). In the following experiments, the colonic dilatation induced by 5–10 min application of GBR was subject to analysis.
Effects of GBR 12909 (GBR) and SCH 23990 (SCH) on colonic motility in the proximal colon of rats. A series of spatio-temporal maps of diameter changes showed time-dependent effects of bath-applied GBR (1 μM, up to 30 min) on colonic motility (a). Arrowheads indicated peristalsis. Time-dependent effects of GBR on the maximum diameter (b), % of maximum diameter (c), and frequency of peristalsis (d) were summarized (mean ± SD, n = 8, *P < 0.05, NS: not significant). A series of spatio-temporal maps showed that SCH (5 μM) did not change the maximum diameter but reduced the frequency of peristalsis. Pre-treatment of SCH (5 μM) blocked the dilatation of colonic segments induced by a subsequent 10 min application of GBR (1 μM, e). Effects of SCH (5 μM) alone and SCH plus GBR (1 μM) on the maximum diameter (f), % of maximum diameter (g), and frequency of peristalsis (h) were summarized (n = 5). A series of spatio-temporal maps showed that GBR (1 μM) dilated without changing the frequency of peristaltic waves. Subsequent bath-applied SCH (20 μM) reversed the GBR-induced dilatation and prevented the generation of peristaltic waves (i). Effects of GBR alone and GBR plus SCH on the maximum diameter (j), % of maximum diameter (k), and frequency of peristalsis (l) were summarized (n = 11)
In our previous study, the blockade of D1-like dopamine receptors with SCH at a dose of 20 μM but not 5 μM reduced the colonic diameter [27]. Consistently, bath-applied SCH (5 μM) alone did not decrease the colonic diameter (Fig. 1e-g), while reducing the frequency of peristaltic waves (Fig. 1e, h). In the presence of SCH (5 μM), a 5–10 min application of GBR (1 μM) failed to dilate colonic segments (Fig. 1e–g), suggesting that GBR exerted its dilatory actions via D1–like receptors. In preparations where GBR (1 μM) application for 5–10 min had induced a colonic dilatation, subsequent application of a higher dose of SCH (20 μM) decreased the maximum diameter and largely reduced the frequency of peristaltic waves or abolished their generation (Fig. 1i-l).
Neither GBR (1 μM) nor SCH (5 μM) affected the velocity of peristaltic waves (Supplemental Fig. 2a-c).
Roles of nitrergic, VIP, and purinergic neurons in the GBR-induced dilatation of the colonic segment
Since the neuronal dopamine reuptake inhibitor GBR that is expected to enhance dopaminergic transmission resulted in colonic dilatations, neurally released dopamine may stimulate nitrergic, VIP, or purinergic neurons.
Inhibition of nitrergic transmission with L-NA (100 μM) decreased the colonic diameter and reduced the frequency of peristaltic waves or abolished their generation (Fig. 2a–d). In the colonic segments that had been pretreated with L-NA (100 μM), GBR (1 μM) failed to increase the maximum diameter (Fig. 2a–c).
Effects of an inhibition of inhibitory efferent signals on the GBR-induced dilatation in the proximal colon of rats. A series of spatio-temporal maps of diameter changes showed effects of bath-applied L-nitro arginine (L-NA, 100 μM, a), vasoactive intestinal peptide 10–28 (VIP10-28, 3 μM, e), and MRS 2500 (MRS, 1 μM, i) on the GBR (1 μM)-induced dilatation in colonic segments. Arrowheads indicate peristalsis. Effects of bath-applied GBR plus L-NA (n = 7), VIP10-28 (n = 5), and MRS (n = 5) on the maximum diameter (b, f, j), % of maximum diameter (c, g, k) and frequency of peristalsis (d, h, l) were summarized (mean ± SD, *P < 0.05, NS: not significant)
VIP10-28 (3 μM), a VIP receptor antagonist, alone had no effect on either the maximum diameter or the frequency of peristaltic waves (Fig. 2e–h). In the presence of VIP10-28 (3 μM), GBR (1 μM) was still capable of causing colonic dilatation (Fig. 2e–g).
MRS (1 μM), a P2Y1 receptor antagonist, itself tended to decrease the colonic diameter with a reduction in the frequency of peristaltic waves (Fig. 2i–l). MRS (1 μM) failed to prevent GBR (1 μM)-induced colonic dilatation (Fig. 2i–k).
Roles of nitrergic, VIP, and purinergic neurons in the SCH-induced constriction of the colonic segment
Since the blockade of nitrergic transmission with L-NA prevented GBR-induced colonic dilatations, SCH-induced colonic constrictions may be attributable to the suppression of basal activity of nitrergic neurons. However, SCH (20 μM) was capable of further reducing the maximum diameter in colonic segments where L-NA (100 μM) had caused a colonic constriction (Fig. 3a, b). Since L-NA (100 μM) alone abolished the generation of peristaltic contractions (see Fig. 2a), it was not possible to examine whether SCH (20 μM) reduced peristalsis in the absence of nitrergic transmission.
Effects of an inhibition of inhibitory efferent signals on the SCH-induced constriction in the proximal colon of rats. Effects of bath-applied SCH (20 μM) plus L-NA (100 μM, n = 5; a, b), VIP10-28 (3 μM, n = 5; d, e), and MRS (1 μM, n = 5; h, i) on the maximum diameter and % of maximum diameter were summarized (mean ± SD, * P < 0.05, NS: not significant). A series of spatio-temporal maps of diameter changes showed effects of bath-applied VIP10-28 (c) and MRS (g) on the SCH-induced constriction in colonic segments. Arrowheads indicate peristalsis. Effects of bath-applied SCH plus VIP10-28 (n = 5, f) and MRS (n = 5, j) on the frequency of peristalsis were summarized
Pre-treatment of the colonic segment with VIP10-28 (3 μM) or MRS (1 μM) also failed to prevent SCH (20 μM)-induced colonic constrictions (Fig. 3c–j).
Effects of TTX on the colonic diameter change
To explore if SCH (20 μM)-induced colonic constrictions may be mediated by the suppression of non-nitrergic, non-VIP and non-purinergic neurons, the effects of TTX, a neural excitation blocker, were examined.
TTX (0.6 μM) alone decreased the maximum diameter and prevented the generation of peristaltic waves (Fig. 4a). In the colonic segments that had been pretreated with TTX (0.6 μM), SCH (20 μM) further decreased the maximum diameter (Fig. 4a–c), while GBR (1 μM)-induced increases in the colonic diameter were effectively prevented (Fig. 4d, e). In the TTX-pretreated segments, bath-applied dopamine (3 μM) increased the colonic diameter (Fig. 4f, g), suggesting dopamine is able to exert its dilatory actions independently of neuronal action potentials.
Effects of a neural blocker on the diameter change in the proximal colon of rats. A series of spatio-temporal maps of diameter changes demonstrated that pretreatment of tetrodotoxin (TTX, 0.6 μM) failed to block the SCH (20 μM)-induced constriction in colonic segments (a). Arrowheads indicate peristalsis. Effects of bath-applied TTX plus SCH (n = 5; b, c), GBR (1 μM, n = 5; d, e) and dopamine (3 μM, n = 6; f, g) on the maximum diameter and % of maximum diameter were summarized (mean ± SD, *P < 0.05, NS: not significant)
Effects of GBR and SCH on the diameter change in 6-OHDA-treated colonic segments
TTX prevented the relaxing actions of GBR that appear to result from endogenous dopamine-induced stimulation of D1-like receptors in nitrergic neurons but not the constrictor actions of SCH. Thus, D1-like receptors may also be constitutively expressed in other population(s) of cells [31]. To eliminate the contribution of enteric dopaminergic neurons, colonic segments were treated with 6-OHDA, a dopaminergic neurotoxin, to deplete neuronal dopamine.
Bath application of 6-OHDA (100 μM) for 1 h increased the colonic diameter with an abolition of peristaltic waves (Fig. 5a–d). During continuous application of 6-OHDA (100 μM) for 2 h, the maximum diameter was partially returned towards its original values (Fig. 5a–c). Peristaltic waves were also restored, although their frequency was a lower frequency than control values (Fig. 5a, d). After 3 h of 6-OHDA treatment, peristaltic waves were further slowed or abolished without changing the maximum diameter (Fig. 5a–d). In the segments that had been pretreated with 6-OHDA (100 μM) for 3 h, GBR (1 μM) failed to increase the maximum diameter, but subsequent SCH (20 μM) was still capable of decreasing the colonic diameter (Fig. 5e).
Effects of bath-applied 6-hydroxydopamine (6-OHDA) on colonic motility in the proximal colon of rats. A series of spatio-temporal maps of diameter changes showed time-dependent effects of bath-applied 6-OHDA (100 μM, up to 3 h) on colonic motility (a). Arrowheads indicate peristalsis. Effects of vehicle (n = 7) or 6-OHDA (n = 10) on the maximum diameter (b), % of maximum diameter (c) and frequency of peristalsis (d) were summarized (mean ± SD, *P < 0.05, NS: not significant,.#P < 0.05 vs. vehicle). Effects of GBR alone and GBR plus SCH on % of maximum diameter in segments that had been pretreated with 6-OHDA (100 μM) for 3 h were summarized (e, n = 10)
Effects of in vivo 6-OHDA treatment on the actions of GBR and SCH were also examined. Intraperitoneal injection of 6-OHDA (100 mg kg−1) transiently reduced body weight in rats at day 1, but body weights increased constantly thereafter (Supplemental Fig. 3a). Body weight gain of 6-OHDA-injected rats was lower than that of vehicle-injected rats at days 0–1 but not at days 7–8 or days 14–15 (Supplemental Fig. 3b).
In 12 out of 13 colonic segments isolated from vehicle-treated rats, GBR (1 μM) increased the maximum diameter (Supplemental Fig. 3c, e, and f), while GBR (1 μM) dilated 4 out of 8 segments isolated from 6-OHDA-treated rats (Supplemental Fig. 3d-f). The incidence rate of GBR-induced dilatation was reduced in the segments isolated from 6-OHDA-treated rats compared to vehicle-treated rats (P < 0.05), suggesting that dopaminergic neurons were disrupted by in vivo 6-OHDA treatment. In colonic segments isolated from 6-OHDA-treated rats, subsequent SCH (20 μM) was still capable of constricting colonic segments (Supplemental Fig. 3d-f). In both vehicle- and 6-OHDA-treated segments, the frequency of peristaltic waves was unaffected by GBR (1 μM), but their generation was prevented by subsequent SCH (20 μM) (Supplemental Fig. 3c, d, and g).
The maximum diameter and frequency of peristaltic waves in colonic segments isolated from 6-OHDA-treated rats were unexpectedly comparable to that of vehicle-treated rats (Supplemental Fig. 3e and g, P > 0.05).
Effects of a facilitation and inhibition of noradrenergic signaling on colonic motility
Despite the fact that 6-OHDA denervates not only dopaminergic but also noradrenergic nerves [11, 23], desipramine (0.1 μM), a selective noradrenaline reuptake inhibitor, had no effect on the colonic diameter or the frequency of peristaltic waves (Fig. 6a–c), while subsequent application of GBR (1 μM) increased the colonic diameter without changing the peristaltic frequency (Fig. 6a–c). Bath-applied propranolol (1 μM), a β-adrenoceptor antagonist, and subsequently applied phentolamine (1 μM), an α-adrenoceptor antagonist, also had no effect on the colonic diameter or the frequency of peristaltic waves (Fig. 6d–f). Guanethidine (10 μM), an adrenergic neuron blocker, had no effect on the maximum diameter but decreased the frequency of peristaltic waves (Fig. 6g–j). Subsequent administration of GBR (1 μM) but not desipramine (0.1 μM) increased the colonic diameter without changing the frequency (Fig. 6g–j).
Effects of a facilitation and inhibition of noradrenergic signaling on colonic motility in the proximal colon of rats. Effects of bath-applied desipramine (0.1 μM) and subsequent bath-applied GBR (1 μM) on the maximum diameter (a), % of maximum diameter (b), and frequency of peristalsis (c) were summarized (mean ± SD, n = 5, *P < 0.05, NS: not significant). Effects of bath-applied propranolol (1 μM) and subsequent bath-applied phentolamine (1 μM) on the maximum diameter (d), % of maximum diameter (e), and frequency of peristalsis (f) were summarized (n = 6). A series of spatio-temporal maps of diameter changes showed effects of bath-applied guanethidine (10 μM) and subsequent bath-applied desipramine (0.1 μM) and GBR (1 μM) on colonic motility (g). Arrowheads indicated peristalsis. Effects of guanethidine, desipramine and GBR on the maximum diameter (h), % of maximum diameter (i), and frequency of peristalsis (j) were summarized (n = 5)
Discussion
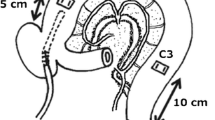
Neural targets of endogenous dopamine in the proximal colon were investigated. In addition, the contribution of constitutively active D1-like receptors to dopaminergic inhibition of the colonic motility was explored. Our principal findings were as follows: (i) the inhibition of dopamine reuptake with GBR that would increase synaptic dopamine concentrations dilated segments of rat proximal colon via the stimulation of D1-like receptors, (ii) the blockade of D1-like receptor with SCH constricted colonic segments, (iii) the effects of GBR but not SCH on the colonic motility were inhibited by L-NA or TTX, and (iv) the colonic segments in which neuronal dopamine is expected to be depleted by 6-OHDA were unresponsive to GBR but constricted by SCH. These findings suggested that enteric dopaminergic nerves stimulate nitrergic neurons expressing D1-like receptors to inhibit the colonic contractile activity. Constitutively active D1-like receptors that are expressed in cells yet to be determined, presumably non-neuronal, cells contribute to tonic dilatation of the proximal colon that is essential for the generation of coordinated peristalsis (Fig. 7).
Proposed roles of enteric dopaminergic neurons and D1-like receptors in regulating motility in the proximal colon. Dopamine released from enteric neurons stimulates nitrergic neurons via the activation of D1-like receptors to dilate the proximal colon. Undetermined cells expressing constitutive active D1-like receptors also contribute to relax smooth muscle cells to suppress non-propagating contractions for the generation of coordinated peristalsis
Neuronal target of dopaminergic neurons to inhibit colonic contractility
GBR-induced dilatations of the colonic segments were prevented by SCH and absent in the 6-OHDA-treated colonic segment, indicating that GBR exerts its actions by specifically increasing synaptic dopamine concentration. The inhibitory actions of GBR were prevented by L-NA but not the VIP receptor antagonist VIP10-28 or the P2Y1 receptor antagonist MRS, suggesting that dopaminergic neurons primarily project to nitrergic rather than VIP or purinergic neurons for interneuronal regulation of colonic motility.
Consistently, our previous immunohistochemical study demonstrated that D1 receptor immunoreactivity is co-localized with the nitrergic nerve marker neuronal NOS in the ENS [27]. Since D1-like receptors are coupled to the Gs protein [24], D1-like receptor-mediated activation of the adenylyl cyclase-cAMP-protein kinase A pathway would enhance NO release from nitrergic neurons by phosphorylating neuronal NOS [9]. Thus, GBR-induced enhancement of dopaminergic neurotransmission appears to result in the stimulation of nitrergic neurons.
Roles of apo-D1-like receptors in the regulation of colonic motility
SCH-induced constrictions of colonic segments were not blocked by either L-NA, VIP10-28 or MRS, suggesting that the constrictions were not due to the removal of inhibitory neuronal activity. In accordance with a previous study [2], the blockade of neuronal activity with TTX also failed to inhibit the excitatory actions of SCH, suggesting that SCH acts on D1-like receptors expressed in non-neuronal cells.
Bath-applied 6-OHDA initially abolished the generation of colonic peristalsis with a colonic dilatation presumably due to an acute, massive leakage of neuronal dopamine. During prolonged exposure to 6-OHDA for 2 h, the diameter was partially returned towards its original level, presumably due the removal of the leaked dopamine by its diffusion and/or degradation. Peristalsis was also restored at a lower frequency than control conditions, suggesting that some residual dopaminergic nerves may still be capable of releasing dopamine to partially restore peristalsis. However, further exposure to 6-OHDA for 3 h eventually abolished peristalsis presumably due to a total lesion of dopaminergic nerves. The lack of colonic dilatation with GBR in 6-OHDA-treated colonic segments supported the notion that enteric dopaminergic neurons are not functional. In this condition, SCH was capable of constricting 6-OHDA-treated colonic segments, suggesting that constitutively active D1-like receptors may be expressed in a population of cells, presumably non-neuronal cells, as in the case of serotonin 5-HT3/4 receptors in the colon [29, 31]. SCH-induced constrictions of colonic segments taken from in vivo 6-OHDA-treated rats also supported this notion.
In our previous immunohistochemical study [27], the expression of D1 receptors was not detected in colonic smooth muscle cells, interstitial cells of Cajal or platelet-derived growth factor receptor α-positive cells that form an integrated postjunctional network, referred to as the SIP syncytium [6]. Transcriptome analyses has also demonstrated that gene expression of dopamine receptors are nearly absent in the SIP syncytium [10, 16, 17]. Since the D5 receptor gene is expressed in colonic residential macrophages [20], constitutive active D1-like receptors in these residential macrophages may well be modulating colonic contractile activity [21, 25].
Roles of noradrenergic neurons in the regulation of motility in isolated colonic preparations
Noradrenaline released by electrical stimulation of sympathetic nerves inhibits colonic migrating motor complexes in isolated colonic segments of mice [14]. In our isolated rat colonic preparations, the selective noradrenaline reuptake inhibitor desipramine, β-adrenoceptor antagonist propranolol or the α-adrenoceptor antagonist phentolamine did not affect the colonic motility, suggesting that constitutively released noradrenaline has a negligible role in regulating the motility. Nevertheless, the adrenergic neuron blocker guanethidine reduced the frequency of colonic peristalsis. The guanethidine-induced inhibition of peristalsis could be attributable to its transient stimulation of noradrenaline releases, but subsequent desipramine did not enhance the inhibitory action. In guanethidine-treated segments, GBR was capable of dilating the colonic segments, suggesting that enteric dopamine was not depleted. Since P2Y1 receptor blockade with MRS reduced the frequency of colonic peristalsis, guanethidine-induced inhibition of peristalsis could be due to the blockade of purines that could be released from sympathetic nerves as co-transmitter(s).
Pathological implications
In patients with Parkinson’s disease, in whom dopaminergic neurons are reduced in the both central and enteric nervous systems, constipation is a commonly seen non-motor symptom [12, 28, 30]. While the degeneration of central dopaminergic neurons also results in the impairment of colonic contractile activity [4], reductions in daily fecal output occurred at 3 weeks after the lesion of nigrostriatal dopaminergic neurons, presumably due to enteric neuronal dysfunction secondary to central dopaminergic neural loss [3]. Thus, dysfunction of enteric dopamine rather than central dopamine may have an impact on constipation in the prodromal stage of Parkinson’s disease [12, 28]. Since peristaltic contractions in colonic segments in which neuronal dopamine is expected be chronically depleted with the 4-week-6-OHDA treatment remained comparable to those of normal colonic segments, compensatory mechanisms may have substituted for dopaminergic neurons to maintain normal colonic motility. Thus, subsequent neuronal loss of central dopaminergic neurons may contribute to late stage constipation in Parkinson’s disease patients.
Conclusions
Dopaminergic neurons appear to facilitate nitrergic neurons expressing D1-like receptors to dilate the proximal colon, contributing the maintenance of regular peristaltic waves. Constitutively activated enteric D1-like receptors may also contribute to basal dilatation of the colon.
Data availability
Data is available on demand from Dr. Hiroyuki Nakamori in whose laboratory this research was undertaken.
References
Anlauf M, Schäfer MK, Eiden L, Weihe E (2003) Chemical coding of the human gastrointestinal nervous system: cholinergic, VIPergic, and catecholaminergic phenotypes. J Comp Neurol 459:90–111. https://doi.org/10.1002/cne.10599
Auteri M, Zizzo MG, Amato A, Serio R (2016) Dopamine induces inhibitory effects on the circular muscle contractility of mouse distal colon via D1- and D2-like receptors. J Physiol Biochem 73:395–404. https://doi.org/10.1007/s13105-017-0566-0
Blandini F, Balestra B, Levandis G, Cervio M, Greco R, Tassorelli C, Colucci M, Faniglione M, Bazzini E, Nappi G, Clavenzani P, Vigneri S, De Giorgio R, Tonini M (2009) Functional and neurochemical changes of the gastrointestinal tract in a rodent model of Parkinson’s disease. Neurosci Lett 467:203–207. https://doi.org/10.1016/j.neulet.2009.10.035
Chai XY, Diwakarla S, Pustovit RV, McQuade RM, Di Natale M, Ermine CM, Parish CL, Finkelstein DI, Furness JB (2020) Investigation of nerve pathways mediating colorectal dysfunction in Parkinson’s disease model produced by lesion of nigrostriatal dopaminergic neurons. Neurogastroenterol Motil 32:e13893. https://doi.org/10.1111/nmo.13893
Costa M, Wiklendt L, Simpson P, Spencer NJ, Brookes SJ, Dinning PG (2015) Neuromechanical factors involved in the formation and propulsion of fecal pellets in the guinea-pig colon. Neurogastroenterol Motil 27:1466–1477. https://doi.org/10.1111/nmo.12646
Durnin L, Kurahashi M, Sanders KM, Mutafova-Yambolieva VN (2020) Extracellular metabolism of the enteric inhibitory neurotransmitter β-nicotinamide adenine dinucleotide (β-NAD) in the murine colon. J Physiol 598:4509–4521. https://doi.org/10.1113/JP280051
Fujii H, Takatori S, Zamami Y, Hashikawa-Hobara N, Miyake N, Tangsucharit P, Mio M, Kawasaki H (2012) Adrenergic stimulation-released 5-HT stored in adrenergic nerves inhibits CGRPergic nerve-mediated vasodilatation in rat mesenteric resistance arteries. Br J Pharmacol 166:2084–2094. https://doi.org/10.1111/j.1476-5381.2012.01935.x
Grider JR (2003) Neurotransmitters mediating the intestinal peristaltic reflex in the mouse. J Pharmacol Exp Ther 307:460–467. https://doi.org/10.1124/jpet.103.053512
Guerra DD, Bok R, Lorca RA, Hurt KJ (2020) Protein kinase A facilitates relaxation of mouse ileum via phosphorylation of neuronal nitric oxide synthase. Br J Pharmacol 177:2765–2778. https://doi.org/10.1111/bph.15001
Ha SE, Lee MY, Kurahashi M, Wei L, Jorgensen BG, Park C, Park PJ, Redelman D, Sasse KC, Becker LS, Sanders KM, Ro S (2017) Transcriptome analysis of PDGFRα+ cells identifies T-type Ca2+ channel CACNA1G as a new pathological marker for PDGFRα+ cell hyperplasia. PLoS One 12:e0182265. https://doi.org/10.1371/journal.pone.0182265
Jiao YY, Guo SY, Umezawa T, Okada M, Hisamitsu T (2002) The sympathetic nervous system is involved in the inhibitory effect of morphine on the colon motility in rats. Auton Neurosci 100:27–31. https://doi.org/10.1016/S1566-0702(02)00137-6
Kalia LV, Lang AE (2015) Parkinson’s disease. Lancet 386:896–912. https://doi.org/10.1016/S0140-6736(14)61393-3
Kishi M, Takeuchi T, Suthamnatpong N, Ishii T, Nishio H, Hata F, Takewaki T (1996) VIP- and PACAP-mediated nonadrenergic, noncholinergic inhibition in longitudinal muscle of rat distal colon: involvement of activation of charybdotoxin- and apamin-sensitive K+ channels. Br J Pharmacol 119:623–630. https://doi.org/10.1111/j.1476-5381.1996.tb15719.x
Kurahashi M, Kito Y, Baker SA, Jennings LK, Dowers JGR, Koh SD, Sanders KM (2020) A novel postsynaptic signal pathway of sympathetic neural regulation of murine colonic motility. FASEB J 34:5563–5577. https://doi.org/10.1096/fj.201903134R
Kurahashi M, Mutafova-Yambolieva V, Koh SD, Sanders KM (2014) Platelet-derived growth factor receptor-α-positive cells and not smooth muscle cells mediate purinergic hyperpolarization in murine colonic muscles. Am J Physiol Cell Physiol 307:C561–C570. https://doi.org/10.1152/ajpcell.00080.2014
Lee MY, Ha SE, Park C, Park PJ, Fuchs R, Wei L, Jorgensen BG, Redelman D, Ward SM, Sanders KM, Ro S (2017) Transcriptome of interstitial cells of Cajal reveals unique and selective gene signatures. PLoS One 12:e0176031. https://doi.org/10.1371/journal.pone.0176031
Lee MY, Park C, Berent RM, Park PJ, Fuchs R, Syn H, Chin A, Townsend J, Benson CC, Redelman D, Shen TW, Park JK, Miano JM, Sanders KM, Ro S (2015) Smooth muscle cell genome browser: enabling the identification of novel serum response factor target genes. PLoS One 10:e0133751. https://doi.org/10.1371/journal.pone.0133751
Li Z, Chalazonitis A, Huang YY, Mann JJ, Margolis KG, Yang QM, Kim DO, Côté F, Mallet J, Gershon MD (2011) Essential roles of enteric neuronal serotonin in gastrointestinal motility and the development/survival of enteric dopaminergic neurons. J Neurosci 31:8998–9009. https://doi.org/10.1523/JNEUROSCI.6684-10.2011
Li ZS, Pham TD, Tamir H, Chen JJ, Gershon MD (2004) Enteric dopaminergic neurons: definition, developmental lineage, and effects of extrinsic denervation. J Neurosci 24:1330–1339. https://doi.org/10.1523/JNEUROSCI.3982-03.2004
Liu L, Wu Y, Wang B, Jiang Y, Lin L, Li X, Yang S (2021) DA-DRD5 signaling controls colitis by regulating colonic M1/M2 macrophage polarization. Cell Death Dis 12:500. https://doi.org/10.1038/s41419-021-03778-6
Luo J, Qian A, Oetjen LK, Yu W, Yang P, Feng J, Xie Z, Liu S, Yin S, Dryn D, Cheng J, Riehl TE, Zholos AV, Stenson WF, Kim BS, Hu H (2018) TRPV4 channel signaling in macrophages promotes gastrointestinal motility via direct effects on smooth muscle cells. Immunity 49:107-119.e4. https://doi.org/10.1016/j.immuni.2018.04.021
Massari CM, Castro AA, Dal-Cim T, Lanznaster D, Tasca CI (2016) In vitro 6-hydroxydopamine-induced toxicity in striatal, cerebrocortical and hippocampal slices is attenuated by atorvastatin and MK-801. Toxicol In Vitro 37:162–168. https://doi.org/10.1016/j.tiv.2016.09.015
McCafferty DM, Wallace JL, Sharkey KA (1997) Effects of chemical sympathectomy and sensory nerve ablation on experimental colitis in the rat. Am J Physiol 272:G272–G280. https://doi.org/10.1152/ajpgi.1997.272.2.G272
Missale C, Nash SR, Robinson SW, Jaber M, Caron MG (1998) Dopamine receptors: from structure to function. Physiol Rev 78:189–225. https://doi.org/10.1152/physrev.1998.78.1.189
Muller PA, Koscsó B, Rajani GM, Stevanovic K, Berres ML, Hashimoto D, Mortha A, Leboeuf M, Li XM, Mucida D, Stanley ER, Dahan S, Margolis KG, Gershon MD, Merad M, Bogunovic M (2014) Crosstalk between muscularis macrophages and enteric neurons regulates gastrointestinal motility. Cell 158:1210. https://doi.org/10.1016/j.cell.2014.08.002
Nakamori H, Iida K, Hashitani H (2021) Mechanisms underlying the prokinetic effects of endogenous glucagon-like peptide-1 in the rat proximal colon. Am J Physiol Gastrointest Liver Physiol 321:G617–G627. https://doi.org/10.1152/ajpgi.00175.2021
Nakamori H, Noda K, Mitsui R, Hashitani H (2021) Role of enteric dopaminergic neurons in regulating peristalsis of rat proximal colon. Neurogastroenterol Motil 33:e14127. https://doi.org/10.1111/nmo.14127
Schapira AHV, Chaudhuri KR, Jenner P (2017) Non-motor features of Parkinson disease. Nat Rev Neurosci 18:435–450. https://doi.org/10.1038/nrn.2017.62
Sia TC, Whiting M, Kyloh M, Nicholas SJ, Oliver J, Brookes SJ, Dinning PG, Wattchow DA, Spencer NJ (2013) 5-HT3 and 5-HT4 antagonists inhibit peristaltic contractions in guinea-pig distal colon by mechanisms independent of endogenous 5-HT. Front Neurosci 7:136. https://doi.org/10.3389/fnins.2013.00136
Singaram C, Ashraf W, Gaumnitz EA, Torbey C, Sengupta A, Pfeiffer R, Quigley EM (1995) Dopaminergic defect of enteric nervous system in Parkinson’s disease patients with chronic constipation. Lancet 346:861–864. https://doi.org/10.1016/S0140-6736(95)92707-7
Zhang B, Albaker A, Plouffe B, Lefebvre C, Tiberi M (2014) Constitutive activities and inverse agonism in dopamine receptors. Adv Pharmacol 70:175–214. https://doi.org/10.1016/B978-0-12-417197-8.00007-9
Acknowledgements
The authors thank Dr Richard Lang (Monash University) for critically reading the manuscript.
Funding
The present study was supported by a research grant from the Nitto Foundation and Grant-in-Aid for Young Scientists (JP20K16964) from Japan Society for the Promotion of Science (JSPS) to HN.
Author information
Authors and Affiliations
Contributions
HN and HH were responsible for the conception and design of the experiments. HN was responsible for the collection, analysis, and interpretation of data. HN and HH were responsible for drafting the article or revising it critically for important intellectual content. HN and HH have read and approved the final manuscript submitted for publication and are accountable for all aspects of the work. All persons designated as authors qualify for authorship, and all those who qualify are listed.
Corresponding author
Ethics declarations
Ethics approval
The experimental procedures were performed according to the guidelines for the care and use of laboratory animals approved by the Experimental Animal Committee of the Nagoya City University Graduate School of Medical Sciences (Approval no: H30M-27).
Consent to participate
“Not applicable” as human study is not included in this work.
Consent for publication
The authors hereby consent to publication of the Work in Pflügers Archiv European Journal of Physiology.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nakamori, H., Hashitani, H. Neural targets of the enteric dopaminergic system in regulating motility of rat proximal colon. Pflugers Arch - Eur J Physiol 475, 1315–1327 (2023). https://doi.org/10.1007/s00424-023-02849-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-023-02849-1