Abstract
Hyperuricemia, defined as elevated serum concentrations of uric acid (UA) above 416 µmol L−1, is related to the development of cardiometabolic disorders, probably via induction of endothelial dysfunction. Hyperuricemia causes endothelial dysfunction via induction of cell apoptosis, oxidative stress, and inflammation; however, it's interfering with insulin signaling and decreased endothelial nitric oxide (NO) availability, resulting in the development of endothelial insulin resistance, which seems to be a major underlying mechanism for hyperuricemia-induced endothelial dysfunction. Here, we elaborate on how hyperuricemia induces endothelial insulin resistance through the disruption of insulin-stimulated endothelial NO synthesis. High UA concentrations decrease insulin-induced NO synthesis within the endothelial cells by interfering with insulin signaling at either the receptor or post-receptor levels (i.e., proximal and distal steps). At the proximal post-receptor level, UA impairs the function of the insulin receptor substrate (IRS) and phosphatidylinositol 3-kinase (PI3K)/protein kinase B (Akt) in the insulin signaling pathway. At the distal level, high UA concentrations impair endothelial NO synthase (eNOS)-NO system by decreasing eNOS expression and activity as well as by direct inactivation of NO. Clinically, UA-induced endothelial insulin resistance is translated into impaired endothelial function, impaired NO-dependent vasodilation, and the development of systemic insulin resistance. UA-lowering drugs may improve endothelial function in subjects with hyperuricemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Uric acid (UA), the end product of purine catabolism in humans, is synthesized from xanthine through the action of the xanthine oxidoreductase (XOR) enzyme system [63]. In addition to being the primary cause of gout [64], hyperuricemia is a risk factor for cardiometabolic disorders [33, 48, 55, 99] and mortality [52, 100]. Meta-analyses of cohort studies report a 24% attributable risk of high-serum UA for incidence of type 2 diabetes mellitus (T2DM) with each 59.48 μmol L−1 (1 mg dL−1) increase in circulating UA concentration increases the risk of T2DM by 6–17% [50, 60]. Although still controversial, increased circulating levels of UA are considered to be a causative factor for developing T2DM [50, 60].
High UA concentrations can be a predisposing factor in the onset of T2DM. This is potentially due to induction of pancreatic β-cell death and impairment of insulin secretion [31, 59] and/or blunting of insulin signaling in various cells, including cardiomyocytes [115], skeletal muscle cells [109], adipocytes [9], hepatocytes [116], and endothelial cells [20] that is consequently reflected as systemic insulin resistance [2, 65].
Hyperuricemia induces endothelial dysfunction primarily by decreasing nitric oxide (NO) bioavailability [66], which is considered to be the primary factor coupling endothelial dysfunction with insulin resistance [19]. Hyperuricemia inhibits insulin-induced activation and expression of endothelial NO synthase (eNOS) and therefore decreases NO production in the endothelial cells, resulting in endothelial insulin resistance [20, 77, 97]. The critical role of endothelial-derived NO in insulin homeostasis is greatly supported by experiments in which eNOS-deficient animals display insulin resistance [18, 25].
This review aims to elaborate on how hyperuricemia induces endothelial insulin resistance by disrupting the endothelial NO system.
UA metabolism
Uric acid (C5H4N4O3, 7,9-dihydro-1 H-purine2,6,8(3 H)-trione, molecular mass 168 Da) is a weak hydrogenated organic acid with pKa1 of 5.75 and pKa2 of 10.3. Under physiological conditions (i.e., pH 7.4 and 37 °C), UA predominantly circulates (~ 98–99%) in the plasma and synovial fluid in its mono-deprotonated ionic form (urate anion) [72]. Figure 1 summarizes the biosynthesis and catabolism of UA, indicating how an imbalance in UA metabolism leads to hyperuricemia and contributing to the development of gout and cardiometabolic disorders. The whole-body homeostasis of UA depends on the balance between its production and catabolism [91]. UA is originated from the catabolism of adenine- and guanine-based purines arising from endogenous (i.e., de novo purine biosynthesis and cell and tissue turnover) and exogenous (i.e., dietary purines occurring in the seafood, meats, and legumes) sources [40, 102, 103]. The liver is the major site of UA production, while other organs such as the intestine, myocardium, kidney, and endothelium also synthesize UA to a lesser extent [26]. About two-thirds of UA is eliminated by the kidneys in the urine [92] and approximately one-third to one-fourth is eliminated via the gastrointestinal tract [14, 63].
Uric acid (UA) biosynthesis/catabolism pathways in humans and determinants of its whole-body homeostasis. The xanthine oxidoreductase (XOR) is the key and rate-limiting enzyme in the biosynthesis of UA that converts hypoxanthine (HPX) to xanthine (XN) and UA. Mammalian XOR has two interconvertible forms: dehydrogenase (XDH) and oxidase (XO) forms. The kidneys eliminate about two-thirds (62.8–69.8%) of UA in urine, and one-third to one-fourth (16–22%) is eliminated via the gastrointestinal tract and excreted in the feces as intact UA and allantoin (i.e., produced by bacterial uricase activity). The voltage-driven urate transporter 1 (URATv1), working together with URAT1, organic anion transporter 1 (OAT1), and OAT3, regulates renal urate handling, and ATP-binding cassette G2 (ABCG2) is known as the main one for intestinal UA transport regulation. Serum UA in humans is regulated mainly by ABCG2 (a secretion transporter) and URAT1 and URATv1 (urate reabsorption transporters). About 10% of hyperuricemia is attributed to UA overproduction, more than 80% to decreased UA renal excretion, and 10% to combined overproduction-underexcretion
Many enzymes are involved in metabolizing purines (adenine and guanine) to UA; adenosine monophosphate (AMP) is converted to inosine via nucleotidase and adenosine deaminase, whereas guanine monophosphate (GMP) is converted to guanosine by nucleotidase [63]. Both nucleosides (inosine and guanosine) are subjected to further processes to convert to hypoxanthine (HPX) and guanine, respectively, by the act of purine nucleoside phosphorylase [63]. The guanine is then deaminated to form xanthine via guanine deaminase [63]. The XOR is the key and rate-limiting enzyme in purine metabolism [63] that converts HPX to xanthine and then to UA [63]. Mammalian XOR has two interconvertible forms, a dehydrogenase form (XDH, EC 1.17.1.4) and an oxidase form (XO, EC 1.17.3.2) [36]. The XDH-XO transition occurs either irreversibly via partial proteolysis or reversibly via the chemical or enzymatic oxidation of thiol groups [12]. The XDH is predominantly the intracellular form, whereas XO is the post-transcriptionally modified circulating form and is highly expressed in pathological conditions (e.g., hypoxia and ischemia [119]) that generate toxic levels of superoxide anion and hydrogen peroxide [3, 11]. NO can modify XOR activity; exogenous NO and also NO produced by XOR-induced reduction of nitrite to NO inactivate XOR by NO-induced conversion of XO to its desulfo-form [32, 39].
Normal plasma concentrations of UA are 155–357 µmol L−1 in women and 208–428 µmol L−1 in men [23]. A threshold level of < 360 µmol L−1 has been suggested to be a cut-off value to identify healthy subjects [23]; however, hyperuricemia is commonly defined as plasma UA concentration of greater than 416 µmol L−1, which is related to an increased size of exchangeable UA pool by about twofold (from 1200 to 2027 mg) and hyperuricosuria (urinary excretion of UA > 800 mg day−1 in men and > 750 mg day−1 in women) [14, 102].
Physiological functions of UA
Although physiological functions of UA have been poorly documented, both in vitro and in vivo studies indicate that physiological concentrations of UA can exert antioxidant [13], anti-inflammatory, and chondroprotective effects [54]. UA is also essential for endothelial function (see the “Physiologic functions of UA in the endothelial cells” section), immune response, and defense against neurological and autoimmune diseases [13, 26]. As discussed by Johnson et al. [42], UA may act as a “physiological alarm signal” in response to modern lifestyle. The lack of uricase is responsible for a higher level of UA in human blood (180–720 μmol L−1) compared to other mammals that have uricase (30–120 μmol L−1) [42]. It has been hypothesized that uricase mutation (occurred in early hominoid evolution) led to higher serum UA concentrations, might have been a compensatory response to the loss of L-gluconolactone oxidase (the enzyme responsible for ascorbic acid synthesis) that acted as an antioxidant system, improved innate immune function, maintained blood pressure during periods of environmental stress, and increased life span [5, 41].
Emerging high UA levels in modern humans have been interpreted as an adaptive response. UA retained in the circulation in an attempt to offset disease-associated oxidative stress [15]. Uric acid is as effective as ascorbate at inhibiting lipid peroxidation [5] or more effective than ascorbate at neutralizing peroxynitrite [53]. The higher circulating level of UA compared to ascorbate (300 vs. 60–90 µmol L−1) makes it the major antioxidant in humans. About half of the plasma total antioxidant capacity in humans has been attributed to circulating UA [5, 13]; UA comprises ~ 10–15% of hydroxyl radical-scavenging capacity and 30–65% of the peroxyl radical-scavenging capacity of plasma [13]. The oxidative damage of biological molecules (i.e., protein, DNA, and lipids), induced by 2,2′-azobis-(2-amidinopropane)-dihydrochloride, is effectively prevented by UA [71]. Physiological concentrations of UA inhibit the oxo-heme oxidant formed by peroxide reaction with hemoglobin, and protect erythrocyte membrane against lipid peroxidation, and erythrocytes from peroxidative damage and lysis [5, 46]. Uric acid also dose-dependently inhibits oxidation of human low-density lipoprotein at concentrations of 5–100 µmol L−1 [88]; at a concentration of 100 µmol L−1, UA reduces consumption of other antioxidants (i.e., α-tocopherol and β-carotene), by ~ 50% and effectively suppresses oxidation of polyunsaturated fatty acids [88].
At physiologic concentrations (15–60 μg/ml), UA inhibits activator protein-1 (AP-1) and extracellular signal-regulated kinase (ERK) signaling pathways as well as expression of tumor necrosis factor-α- and interleukin-induced inducible NOS, cyclooxygenase-2, and matrix metalloproteinase-13 in joint tissues [54].
Pathological effects of high concentrations of UA
Epidemiological evidence indicates that hyperuricemia is associated with incidence of cardiovascular diseases [16, 27] and development of atherosclerosis [34]. A meta-analysis of prospective cohort studies showed that hyperuricemia was related to the risk of major adverse cardiovascular events [relative risk (RR) = 1.72, 95% confidence interval (CI) = 1.28–2.33) [112]. The pooled estimated effect size of hyperuricemia for the risk of coronary heart disease mortality and all-cause mortality was 1.14 (95% CI = 1.06–1.23) and 1.20 (95% CI = 1.13–1.28), respectively. Each 59.48 μmol L−1 increase in serum UA concentration increased risk of coronary heart disease and all-cause mortalities by 20% and 9%, respectively [118]. A meta-analysis of 11 studies indicated that each 59.48 μmol L−1 increase in serum UA increases risk of metabolic syndrome and non-alcoholic fatty liver disease by 30% and 21%, respectively [110]. High-serum UA levels also contribute to the development of hypertension and can lead to renal dysfunction by increasing renal vascular resistance and decreasing renal blood flow [86, 87]. High UA concentration induces vascular dysfunction, by activating the nuclear factor kappa-B (NF-κB) signaling pathway [57], as well as decreases cell viability, by activating NF-κB and ERK signaling pathways [58], inducing oxidative stress, and activating renin-angiotensin system [108].
Endothelial insulin resistance
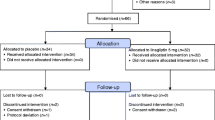
The endothelium is an important insulin target tissue [10]; despite not regulating metabolism, insulin regulates endothelial cell homeostasis [82] via two main signaling pathways [47]. First, the phosphatidylinositol 3-kinase (PI3K)-protein kinase B (Akt) pathway, and second, the Ras/Raf/mitogen-activated protein kinase (MAPK) pathway (Fig. 2).
Insulin signaling pathways in the endothelial cells. Insulin regulates endothelial cell homeostasis via two main signaling pathways: (1) phosphatidylinositol 3-kinase (PI3K)-protein kinase B (Akt) pathway and (2) Ras/Raf/mitogen-activated protein kinase (MAPK) pathway. IRS, insulin receptor substrate; PDK, phosphoinositide-dependent kinase; eNOS, endothelial nitric oxide (NO) synthase; ROS, reactive oxygen species; NADPH, the reduced form of nicotinamide adenine dinucleotide phosphate; PKC, protein kinase C; NF-κB, nuclear factor kappa-B; Ang-II, angiotensin II; ET-1, endothelin1; VCAM-1, vascular cell adhesion molecule-1; GRB2, growth factor receptor binding protein-2; SHC, Src (sarcoma) homology collagen-like-1; SOS, son of sevenless; Ras, rat sarcoma; Raf, rat fibrosarcoma; MAPK, MEK, mitogen-activated ERK kinase; ERK, extracellular-regulated kinase; MAPK, mitogen-activated protein kinase. Sp1, specificity protein 1; AP-1, activator protein 1
Through the PI3K-Akt pathway, insulin stimulates endothelial NO production by inducing eNOS phosphorylation at Ser1177 (as stimulatory site) and eNOS dephosphorylation at Thr495 (as inhibitory site), which is constitutively phosphorylated in the endothelial cells [6]. In addition, insulin increases eNOS gene expression and transcription via PI3K-induced binding of transcriptional factors Sp1 (specificity protein 1) and AP-1 to the eNOS gene [28]. Insulin can also suppress inflammation in the endothelial cells, probably through the PI3K-Akt pathway, as loss of insulin signaling in the endothelial cells (induced by endothelial-specific elimination of the insulin receptor) leads to increased inflammation and expression of the vascular cell adhesion molecule-1 (VCAM-1) [83]. Furthermore, through induction of the PI3K-Akt pathway and phosphorylation of caspase-9, insulin suppresses caspase-9-induced endothelial cell apoptosis [35]. Insulin also inhibits NADPH oxidase-dependent superoxide production in the endothelial cells, probably via the PI3K-Akt pathway [24].
Through the Ras/Raf/MAPK pathway, insulin regulates mitogenesis, growth, and differentiation of the endothelial cells. Also, it mediates vasoconstrictor actions of insulin by stimulating the production of endothelin-1 (ET-1) and angiotensin II (Ang-II) [68, 73, 79]. In the hyperinsulinemic or insulin resistance states, insulin promotes VCAM-1 expression in the endothelial cells by activating the p38-MAPK pathway, an effect that is intensified by blocking the PI3K-Akt pathway [61]. Insulin signaling in the endothelial cells may be complicated by a network of multiple feedback loops and cross-talk between two major pathways [69]; for example, inhibition of the PI3K-Akt pathway leads to enhanced mitogenic action of insulin [68].
Although the concept of endothelial insulin resistance is not clinically established nevertheless, at the cellular level, it has been characterized as an impaired responsiveness of the cell to insulin’s actions through inactivation of both PI3K-Akt and MAPK pathways. This notion is supported by using the endothelial cell insulin receptor knockout mouse model, where both eNOS and ET-1 were observed to be decreased [98]. However, some evidence emphasizes that endothelial insulin resistance in the PI3K-Akt pathway does not necessarily coincide with resistance in the other signaling pathway [22, 111] and a selective reduction in the ability of insulin to stimulate the PI3K-Akt pathway alongside with augmented insulin-induced MAPK pathway occurs in endothelial insulin resistance [69]. In support, both in vitro and in vivo models of endothelial insulin resistance (i.e., induced by high-fat diet and high-glucose concentrations, respectively) indicate decreased insulin-stimulated NO production with increased Ang-II concentrations [111]. In addition, in a high-glucose-induced model of endothelial insulin resistance, insulin cannot activate the PI3K-Akt-eNOS pathway. In contrast, the Ras/Raf/MAPK pathway responds to insulin through up-regulation of extracellular signal-regulated kinase-1/2 (ERK1/2), p38, and JNK (c-Jun N-terminal kinase) phosphorylation [22].
Impaired insulin-stimulated NO synthesis has been suggested to be the hallmark of endothelial insulin resistance [70, 89]. Following exposure to insulin, freshly isolated peripheral venous endothelial cells obtained from patients with T2DM displayed decreased Ser1177 eNOS phosphorylation (which increases eNOS activity) and increased Thr495 eNOS phosphorylation (which decreases eNOS activity) when compared to the cells obtained from healthy subjects [94].
UA and the endothelial cells
Uric acid enters into the endothelial cells via uric acid transporters (UAT) and is also synthesized from HPX within the cells. The major physiological NO-related function of UA in the endothelial cells seems to be increased NO availability.
Uric acid transporters in the endothelial cells
Uric acid transporters are classified as reabsorbing and excretory transporters; URAT1 (SLC22A12, solute carrier family 22, member 12) is a reabsorbing transporter, expressed in both the luminal and basolateral membranes of the renal proximal tubular cells [105]. The organic acid transporter 1 (OAT1/SLC22A6), OAT3 (SLC22A8), multidrug resistance-associated protein 4 [(MRP4); also called ATP-binding cassette transporter C4 (ABCC4)], ABCG2, and voltage-driven urate transporter 1 [(URATv1); also called glucose transporter 9 (GLUT9) or SLC2A9] are excretory transporters [105].
Expression of UAT has been widely reported in the kidneys and intestine, however, little is known about their distribution in other tissues. Among the known UAT, mRNA expressions of MCT9 (monocarboxylate transporter 9)/SLC16A9, URATv1, BCRP (breast cancer resistance protein; also called ABCG2), MRP4, and OAT10 have been documented in the human umbilical vein endothelial cells (HUVECs) [51, 58, 67, 93]. In addition, expression of URAT1 has also been reported in the HUVEC cells [58] and in the human vascular smooth muscle cells, where it enters UA into the cells [80]. However, others have reported that URAT1, OAT1, OAT3, NPT1 (sodium-dependent phosphate cotransporter), and NPT4 are not expressed in the HUVEC cells [67, 93]. To the best of our knowledge, there is no report to address the distribution of UAT in the endothelial cells of different vascular beds and this issue needs further investigation.
Among UAT in the endothelial cells, URATv1 (GLUT9) and MCT9 are involved in the entry of UA into the cells; in the presence of high UA concentrations, they act as influx transporters [67], and BCRP and MRP4 act as efflux UA transporters [51]. High UA concentration disturbs UA efflux in the HUVECs; UA (595 and 892 μmol L−1 vs. 300 μmol L−1) decreases Akt phosphorylation and therefore inhibits intracellular BCRP translocation to the cell surface, resulting in intracellular accumulation of UA [51]. It has been suggested that hyperuricemia-induced activation of URATv1 (GLUT9) contributes more to UA-induced impaired NO production in the endothelial cells [67] (Fig. 3).
Intracellular source of uric acid (UA) in the endothelial cell. Uric acid enters into the endothelial cells via uric acid transporters (UAT); UA is also synthesized in the endothelial cells from its precursor, hypoxanthine (HPX) by xanthine oxidoreductase (XOR), which exist in two interconvertible forms: dehydrogenase (XDH) and oxidase (XO) forms. eNOS, endothelial nitric oxide (NO) synthase; ONOO-, peroxynitrite; for details and abbreviations of UA transporters, see the “Uric acid transporters in the endothelial cells” section
Uric acid synthesis in the endothelial cells
In addition to its entry into the endothelial cells via UATs [58, 67, 93], UA is also synthesized in the endothelial cells from its precursor, HPX, via XOR activity [76] (Fig. 3). Hypoxanthine enters into the endothelial cells via a nucleoside transporter, characterized as nitrobenzylthioinosine-insensitive equilibrative nucleoside transporter (NBMPR-insensitive transporter with a medium affinity for the purine, with a Km 320 ± 10 µmol L−1) [74]; HPX influx is saturable and Na+-independent [74]. XOR is located both within the cytoplasm of the endothelial cells (with higher intensity in the perinuclear region) and on the outside surface of the endothelial cell membrane [84]. Circulating XO released from XO-rich tissues under pathophysiological conditions interacts with glycosaminoglycans on the surface of the endothelial cells and is endocytosed into intracellular compartments [38]. Extracellular UA negatively regulates XOR activity, as blockage of UA transporters (due to mutations or inhibitors, e.g., probenecid) promotes XOR activity [29, 81]. Moderate hypoxia and inflammatory cytokines induce XOR expression and activity in the endothelial cells [45, 78]; conversion of XOR to XO, in response to inflammatory conditions, leads to superoxide anion and hydrogen peroxide production, which negatively impact endothelial function by decreased NO bioavailability [4, 8].
Physiologic functions of UA in the endothelial cells
Although UA’s physiologic functions in the endothelial cells have not been fully understood [66], some evidence indicates that normal concentrations of UA in the endothelial cells can preserve NO-dependent endothelial function by increasing NO availability. UA increases NO availability by increasing eNOS expression and NO production in HUVECs [37] and also by decreasing oxidative stress–induced NO inactivation [21, 37, 93]; the latter is probably done by preventing eNOS uncoupling, reacting with peroxynitrite, and preventing oxidant-induced inactivation of extracellular superoxide dismutase [30, 63].
In support of this notion that normal levels of UA help NO-dependent endothelial function, it has been reported that mutations in the URAT1, encoded by the SLC22A12 gene, are associated with lower flow-mediated dilation, which is an index of endothelium-dependent vasodilatation [93]. Extremely low levels of serum UA (< 47.5 µmol L−1), observed in subjects who were homozygote and compound-heterozygous for URAT1 mutations, are related to decreased flow-mediated dilation (homozygous = 2.7 ± 2.3%, compound-heterozygous = 4.7 ± 2.8%, heterozygous = 9.3 ± 7.2%, and mutation free = 7.0 ± 2.3%). In contrast, nitrate-mediated dilation remained unchanged [93], indicating the normal response of vascular smooth muscle to NO. Furthermore, in type 1 diabetic patients with low-serum UA levels (264 vs. 322 µmol L−1 compared to controls), impaired acetylcholine-induced forearm blood flow response was restored following intravenous infusion of 1000 mg UA [101].
UA has an inhibitory feedback effect on XOR activity (Ki UA for XOR = 70 μM, in the presence of 50 μM xanthine and 210 μM oxygen) and therefore regulates XOR-induced reactive oxygen species (ROS) production [81, 95]. It is therefore tempting to assume that in a similar way to plasma, normal levels of UA suppress oxidative stress in the endothelial cells; in human plasma, UA at concentrations of 150 and 300 μmol L−1 decreases the oxidation of xanthine to UA and formation of superoxide anion (37.5 ± 5.6 and 48.9 ± 6.1%, and 23.2 ± 1.9 and 32.0 ± 2.3%, respectively) [95]. Indeed, moderate and severe short-term hypouricemia (plasma UA ~ 126 and 18 µmol L−1), induced by administration of febuxostat per se and febuxostat + rasburicase, increases lipid peroxidation in healthy humans [21].
To sum up, at concentrations near to normal human plasma levels (< 300 μmol L−1), UA seems to be essential for NO-dependent endothelial function.
Uric acid and endothelial insulin resistance
Both clinical and experimental studies indicate that exposure of the endothelial cells to high UA concentrations may cause endothelial dysfunction. In clinical studies, endothelium-dependent vasodilation was inversely related to serum UA levels [44, 117]; for each 59.48 μmol L−1 increase in serum UA concentration, there was a 41% higher risk of endothelial dysfunction [117]. The reactive hyperemia index, considered an index of endothelial function of the microvasculature, was negatively associated with serum UA concentrations [75]. Flow-mediated dilation but not nitrate-mediated dilation was significantly impaired in subjects with serum UA levels of 488 ± 11.9 µmol L−1 compared with those who had UA levels of 357 ± 11.9 µmol L−1; similarly, acetylcholine-induced but not nitrate-induced forearm blood flow was impaired in subjects with UA levels greater than 327 µmol L−1 [117]. Such data may imply that a selective impairment of the endothelial NO-dependent vasodilation in the absence of overt structural vascular disease occurs in hyperuricemic subjects [44].
Table 1 summarizes the underlying mechanisms (i.e., inducing cell apoptosis, increasing oxidative stress, and inflammation) by which high UA levels induce endothelial dysfunction. In brief, high UA concentrations (300–900 μmol L−1), occurring by either induction of intracellular XO or hyperuricemia, result in endothelial dysfunction and higher concentrations of UA (~ 1070–1190 μmol L−1) cause endothelial cell death.
Among the underlying mechanisms explaining endothelial dysfunction induced by high UA concentrations, impaired insulin-stimulated PI3K-Akt-eNOS pathway, and decreased endothelial NO availability, resulting in the development of endothelial insulin resistance, may be the most important ones. This notion is supported by the in vivo evidence indicating hyperuricemia (induced by the uricase inhibitor, allantoxanamide, in rats) disrupts the insulin-stimulated but not acetylcholine-stimulated eNOS phosphorylation in endothelium-intact aortic rings and NO-dependent vasodilation [20]. In the following sections, we focus on the UA-induced mechanisms targeting insulin signaling and NO bioavailability in the endothelial cells.
Underlying mechanisms of UA-induced insulin resistance
A high UA concentration interferes with insulin signaling in the endothelial cells at the receptor and post-receptor levels; at the post-receptor level, both proximal (IRS and PI3K-Akt components) and distal (eNOS-NO system) steps within the insulin signaling pathway are affected by UA (Fig. 4). Other mechanisms summarized in Table 1, including high UA-induced oxidative stress, inflammation, and cell apoptosis, may also contribute to the development of insulin resistance in the endothelial cells.
Interfering of high uric acid (UA) levels with insulin signaling at the receptor and post-receptor levels in the endothelial cells; at the post-receptor level, both proximal (IRS and PI3K-Akt components) and distal (eNOS-NO system) steps within the insulin signaling pathway are affected by UA. ENPP1, ectonucleotide pyrophosphatase/phosphodiesterase 1; Ang-II, angiotensin II; IRS, insulin receptor substrate; PI3K, phosphatidylinositol 3-kinase; Akt, protein kinase B; Sp1, specificity protein 1; AP-1, activator protein 1; eNOS, endothelial nitric oxide (NO) synthase; ROS, reactive oxygen species; CaM, calmodulin; PKC, protein kinase C
Insulin receptor level
Uric acid increases recruitment and binding of ectonucleotide pyrophosphatase/phosphodiesterase 1 (ENPP1), a plasma membrane enzyme that regulates nucleotide metabolism, to α-subunit of the insulin receptor in HUVECs; this binding impairs tyrosine-kinase activity and autophosphorylation of the β-subunit, which results in the inhibition of insulin signaling [1]. Through this inhibition, the Ser473 phosphorylation of Akt and the Ser1177 phosphorylation of eNOS is decreased in the endothelial cells [97]. Inhibition of UA entry into the cell (using probenecid at a dose of 1 mmol L−1 for 30 min) restored these effects [97]. In addition, exposing HUVECs to UA at a dose of 200 µmol L−1 decreases tyrosine phosphorylation of the β-subunit in the insulin receptor and decreases insulin-induced PI3K/Akt/eNOS-mediated NO production [20].
High UA concentrations may also interfere with insulin signaling at the receptor level by increasing Ang-II levels in the endothelial cells. This notion is supported by evidence indicating that UA is a potent activator of the renin-angiotensin system in endothelial cells [107, 108]. At a dose of 535 µmol L−1, intracellular concentrations of Ang-II increased by about threefold in HUVECs over a 24-h period; this increase was due to up-regulation of the pro-renin receptor [107], increased mRNA expressions of angiotensin-converting enzyme, and angiotensinogen [108]. Ang-II inhibits insulin-stimulated tyrosine phosphorylation of the insulin receptor at its β-subunit [7]. Exposing HUVECs to Ang-II at a dose of 200 nM had shown to decrease insulin-stimulated Tyr phosphorylation (Tyr1158/Tyr1162/Tyr1163) of the receptor by 65% [7].
To sum up, these data indicate that in the endothelial cells, high concentrations of UA can directly interfere with the insulin signaling pathway at the receptor level and can contribute to the development of endothelial insulin resistance.
Post insulin receptor level
Proximal signaling pathway (IRS and PI3K-Akt components)
Exposing HUVECs to UA at a dose of 200 µmol L−1 decreases the percent of p-IRS-1/IRS-1 [20]. It has been shown that UA can cause oxidase stress–induced activation of protein kinase C (PKC) in HUVECs [56]. PKC activation inhibits the PI3K-Akt signaling pathway of insulin in bovine aortic endothelial cells; this effect is partly due to inhibition of insulin-induced Tyr phosphorylation of IRS2 [62] but not IRS1, which is functionally more important in the endothelial cells [62]. PKC phosphorylates Thr86 on p85α subunit of PI3K and therefore decreases binding of p85α to IRS1, resulting in a decrease in the insulin-induced activation of PI3K activity [62]. UA also interferes with the insulin signaling pathway at the IRS-1 level in the endothelial cells by increasing intracellular levels of Ang-II [108], which increases phosphorylation of Ser312 and Ser616 (as negative regulatory sites) at IRS-1, leading to decreased ability of IRS-1 to be phosphorylated on Tyr612 and Tyr632 (i.e., essential sites for engaging the p85 subunit of PI3K) [7]. Quantitatively, Ang-II (at a dose of 100 nM) reduces insulin-stimulated binding of IRS-1 to the p85 subunit of PI3K by about 30%, resulting in decreased insulin-induced Akt-Ser473 and eNOS-Ser1177 phosphorylation in HUVECs by 60% and 45%, respectively [7]. This effect is mediated by increasing JNK and ERK 1/2 activity [7]. Ang-II also induces Ser/Thr phosphorylation of p85α/β subunit of PI3K, through the activation and translocation of PKCα/β/δ, from the cytosol to the membrane. The predominant effect of Ang-II is on the PKCα isoform, which effectively phosphorylates Thr86 of p85/ PI3K [62].
In HUVECs, UA (50–200 µmol L−1) inhibits insulin-stimulated eNOS phosphorylation at Ser1177 (IC50 of 51.0 µmol L−1) by inhibiting insulin-stimulated Akt phosphorylation (IC50 = 21.97 µmol L−1), as transfection of the cells with p110, a class I PI3K catalytic subunit, restored the inhibitory effects of UA on Akt and eNOS phosphorylation [20]. UA can also trigger disruption of the PI3K-Akt pathway by increasing PKC phosphorylation and activity [56]. Activated PKC phosphorylates Thr86 of p85 subunit of PI3K, resulting in decreased p-Akt at Ser473 and p-eNOS at Ser1177 [62]. At a dose of 714 μmol L−1, UA increases intracellular p-PKC/PKC ratio, resulting in phosphorylation of eNOS at Thr495 and decreased production of NO [56].
High UA concentrations are also able to counteract PI3K-Akt activity through the induction of oxidative stress and inflammation. UA (at concentrations of 357 and 535 µmol L−1) increases intracellular levels of C-reactive protein (by 7.2-fold at 1 h, and 6.5-fold at 3 h) through activation of p38 and ERK44/42 MAPK signaling pathways, leading to decreased NO production in HUVECs by 80% [43]. High- C-reactive protein levels in the endothelial cell blunt insulin-induced Akt phosphorylation, via the immunoreceptor tyrosine–based inhibition motif of FcγRIIB and SHIP-1 (Src homology 2 domain-containing inositol 5′-phosphatase 1) [96].
Distal signaling pathway (eNOS-NO system)
High UA concentrations can impair the eNOS-NO system by decreasing eNOS expression, reducing eNOS activity, and by direct inactivation of NO. UA-induced decrease in eNOS activity is achieved in several ways: (1) diminishing the insulin-induced Ser1177 phosphorylation of eNOS, (2) reducing insulin-induced Thr495 dephosphorylation of eNOS, (3) decreasing interaction between eNOS and calmodulin, and (4) reducing the availability of substrate for eNOS via (a) decreased intracellular L-arginine concentrations and (b) increased arginase activity.
Incubation of HUVECs with a high dose of UA (1190 µmol L−1) decreases eNOS expression and the amount of NO released by HUVECs (by threefold, from ~ 30 to 10 µmol L−1) [28]. Incubation of HUVECs with high UA concentrations (≥ 600 µmol L−1) switches the direction of mitochondrial Na+/Ca2+ exchanger, resulting in an influx of calcium into the mitochondria, causing an overload in mitochondrial calcium [37]. Elevated mitochondrial calcium levels upregulate mitochondrial ROS production and therefore increased intracellular ROS, which decreases eNOS protein expression and NO synthesis [37]. Blockage of mitochondrial Na+/Ca2+ exchanger inhibits UA-induced reduction in eNOS protein expression and NO production [37]. These effects are against the actions of insulin, which stimulates eNOS gene expression and transcription via PI3K-induced binding of transcriptional factors, Sp1 and AP-1, to the eNOS gene [28].
In HUVECs, UA at concentrations ranged 50–200 µmol L−1 had neither an effect on the expression nor the phosphorylation of Ser1177 within eNOS, meanwhile insulin-stimulated eNOS phosphorylation was blunted by the same doses (with an IC50 of 51.0 µmol L−1) [20]. This data indicates that the effects of UA on eNOS expression/phosphorylation in the endothelial cells, at least in part, are mediated by the insulin signaling pathway. Indeed, UA causes ROS-induced PKC activation, which increases eNOS phosphorylation at Thr495 and decreases eNOS activity by decreasing calmodulin binding to eNOS [56]. On the other hand, insulin through the PI3K-Akt pathway dephosphorylates eNOS at Thr495 and increases eNOS activity [6]. UA (at a dose of 714 µmol L−1 for 24 h) can also decrease eNOS activity and NO production by reducing the interaction of eNOS with calmodulin (as an eNOS activator) [77].
UA (at concentrations of 297 and 446 μmol L−1) decreases stimulated NO production in pig pulmonary arterial endothelial cells by increasing arginase activity; this effect is due to an increase in affinity of arginase for L-arginine (Km = 1.1 mmol L−1 vs. 0.6 mmol L−1 in the presence of 446 μmol L−1 UA) without neither affecting Vmax of the enzyme not changing the gene expression of arginase II (as predominant endothelial isoform of arginase) [113]. Furthermore, UA suppresses eNOS activity via decreasing cellular L-arginine uptake; this effect is not mediated through manipulating the L-arginine transporter (cationic amino acid transporter-1) content or affecting the post-translational modification by PKCa [90].
Uric acid can also react directly with NO (in both human plasma and aortic endothelial cell lysates) through a rapid, irreversible reaction leading to the formation of 6-aminouracil and depletion of NO [30].
Conclusion and future perspective
Uric acid can act as a Janus-faced molecule in the endothelial cells because of its highly contrasting features at varying concentrations. At low concentration, UA is essential for eNOS expression, NO synthesis and availability, and NO-dependent endothelial functions. Meanwhile, at high concentrations, UA can cause endothelial dysfunction. This is so because high-intracellular UA concentrations decrease the responsiveness of the endothelial cells to insulin, resulting in the development of endothelial insulin resistance. Intracellular high UA targets the IRS-PI3K-Akt-eNOS pathway at different steps, including the insulin receptor binding capacity to its downstream signaling events, finally translating to decreased eNOS expression and activity. As a caution, it should be noted that most data that associate hyperuricemia and endothelial insulin resistance are from in vitro studies and needs to be verified through in vivo models. In addition to interfering with insulin signaling pathways and NO synthesis, other unknown mechanisms may also be involved in the development of hyperuricemia-induced endothelial insulin resistance.
Current data provides not only new insights into the complex mechanisms of endothelial insulin resistance in relation to hyperuricemia but also addresses potential therapeutic targets. Since hyperuricemia-induced endothelial insulin resistance is a risk factor for developing systemic insulin resistance, T2DM, and cardiovascular diseases, treating asymptomatic patients with hyperuricemia and maintaining their serum UA within the normal range could potentially protect against cardiometabolic disorders. However, well-designed clinical trials are needed to confirm this assumption.
Data availability
Not applicable.
Code availability
Not applicable.
Abbreviations
- ABC:
-
ATP-binding cassette transporter
- Ang-II:
-
Angiotensin II
- AP-1:
-
Activator protein-1
- BCRP:
-
Breast cancer resistance protein
- CI:
-
Confidence interval
- eNOS:
-
Endothelial nitric oxide synthase
- ENPP1:
-
Ectonucleotide pyrophosphatase/phosphodiesterase 1
- ERK:
-
Extracellular signal-regulated kinase
- ET-1:
-
Endothelin-1
- GLUT:
-
Glucose transporter
- HPX:
-
Hypoxanthine
- HUVEC:
-
Human umbilical vein endothelial cell
- IRS:
-
Insulin receptor substrate
- JNK:
-
C-Jun N-terminal kinase
- MAPK:
-
Mitogen-activated protein kinase
- MCT:
-
Monocarboxylate transporter
- MRP:
-
Multidrug resistance-associated protein
- NF-κB:
-
Nuclear factor kappa-B
- NO:
-
Nitric oxide
- OAT:
-
Organic anion transporter
- PI3K:
-
Phosphatidylinositol 3-kinase
- PKC:
-
Protein kinase C
- ROS:
-
Reactive oxygen species
- RR:
-
Relative risk
- SLC:
-
Solute carrier family
- T2DM:
-
Type 2 diabetes mellitus
- UA:
-
Uric acid
- UAT:
-
Uric acid transporter
- URATv1:
-
Voltage-driven urate transporter 1
- VCAM-1:
-
Vascular cell adhesion molecule-1
- XDH:
-
Xanthine dehydrogenase
- XO:
-
Xanthine oxidase
- XOR:
-
Xanthine oxidoreductase
References
Abate N, Chandalia M, Di Paola R, Foster DW, Grundy SM, Trischitta V (2006) Mechanisms of disease: ectonucleotide pyrophosphatase phosphodiesterase 1 as a ‘gatekeeper’ of insulin receptors. Nat Clin Pract Endocrinol Metab 2:694–701. https://doi.org/10.1038/ncpendmet0367
Adachi SI, Yoshizawa F, Yagasaki K (2017) Hyperuricemia in type 2 diabetic model KK-A(y)/Ta mice: a potent animal model with positive correlation between insulin resistance and plasma high uric acid levels. BMC Res Notes 10:577. https://doi.org/10.1186/s13104-017-2897-x
Agarwal A, Banerjee A, Banerjee UC (2011) Xanthine oxidoreductase: a journey from purine metabolism to cardiovascular excitation-contraction coupling. Crit Rev Biotechnol 31:264–280. https://doi.org/10.3109/07388551.2010.527823
Amaya Y, Yamazaki K, Sato M, Noda K, Nishino T, Nishino T (1990) Proteolytic conversion of xanthine dehydrogenase from the NAD-dependent type to the O2-dependent type. Amino acid sequence of rat liver xanthine dehydrogenase and identification of the cleavage sites of the enzyme protein during irreversible conversion by trypsin. J Biol Chem 265:14170–14175
Ames BN, Cathcart R, Schwiers E, Hochstein P (1981) Uric acid provides an antioxidant defense in humans against oxidant- and radical-caused aging and cancer: a hypothesis. Proc Natl Acad Sci USA 78:6858–6862. https://doi.org/10.1073/pnas.78.11.6858
Andreozzi F, Laratta E, Procopio C, Hribal ML, Sciacqua A, Perticone M, Miele C, Perticone F, Sesti G (2007) Interleukin-6 impairs the insulin signaling pathway, promoting production of nitric oxide in human umbilical vein endothelial cells. Mol Cell Biol 27:2372–2383. https://doi.org/10.1128/mcb.01340-06
Andreozzi F, Laratta E, Sciacqua A, Perticone F, Sesti G (2004) Angiotensin II impairs the insulin signaling pathway promoting production of nitric oxide by inducing phosphorylation of insulin receptor substrate-1 on Ser312 and Ser616 in human umbilical vein endothelial cells. Circ Res 94:1211–1218. https://doi.org/10.1161/01.res.0000126501.34994.96
Aslan M, Ryan TM, Adler B, Townes TM, Parks DA, Thompson JA, Tousson A, Gladwin MT, Patel RP, Tarpey MM, Batinic-Haberle I, White CR, Freeman BA (2001) Oxygen radical inhibition of nitric oxide-dependent vascular function in sickle cell disease. Proc Natl Acad Sci USA 98:15215–15220. https://doi.org/10.1073/pnas.221292098
Baldwin W, McRae S, Marek G, Wymer D, Pannu V, Baylis C, Johnson RJ, Sautin YY (2011) Hyperuricemia as a mediator of the proinflammatory endocrine imbalance in the adipose tissue in a murine model of the metabolic syndrome. Diabetes 60:1258–1269
Barrett EJ, Liu Z (2013) The endothelial cell: an “early responder” in the development of insulin resistance. Rev Endocr Metab Disord 14:21–27. https://doi.org/10.1007/s11154-012-9232-6
Battelli MG, Bolognesi A, Polito L (2014) Pathophysiology of circulating xanthine oxidoreductase: new emerging roles for a multi-tasking enzyme. Biochem Biophys Acta 1842:1502–1517. https://doi.org/10.1016/j.bbadis.2014.05.022
Battelli MG, Polito L, Bortolotti M, Bolognesi A (2016) Xanthine oxidoreductase in drug metabolism: beyond a role as a detoxifying enzyme. Curr Med Chem 23:4027–4036. https://doi.org/10.2174/0929867323666160725091915
Becker BF (1993) Towards the physiological function of uric acid. Free Radical Biol Med 14:615–631. https://doi.org/10.1016/0891-5849(93)90143-I
Benn CL, Dua P, Gurrell R, Loudon P, Pike A, Storer RI, Vangjeli C (2018) Physiology of hyperuricemia and urate-lowering treatments. Front Med 5:160. https://doi.org/10.3389/fmed.2018.00160
Bobulescu IA, Moe OW (2012) Renal transport of uric acid: evolving concepts and uncertainties. Adv Chronic Kidney Dis 19:358–371. https://doi.org/10.1053/j.ackd.2012.07.009
Bos MJ, Koudstaal PJ, Hofman A, Witteman JC, Breteler MM (2006) Uric acid is a risk factor for myocardial infarction and stroke: the Rotterdam study. Stroke 37:1503–1507. https://doi.org/10.1161/01.STR.0000221716.55088.d4
Cai W, Duan X-M, Liu Y, Yu J, Tang Y-L, Liu Z-L, Jiang S, Zhang C-P, Liu J-Y, Xu J-X (2017) Uric acid induces endothelial dysfunction by activating the HMGB1/RAGE signaling pathway. Biomed Res Int 2017:4391920–4391920. https://doi.org/10.1155/2017/4391920
Carlstrom M, Larsen FJ, Nystrom T, Hezel M, Borniquel S, Weitzberg E, Lundberg JO (2010) Dietary inorganic nitrate reverses features of metabolic syndrome in endothelial nitric oxide synthase-deficient mice. Proc Natl Acad Sci USA 107:17716–17720. https://doi.org/10.1073/pnas.1008872107
Cersosimo E, DeFronzo RA (2006) Insulin resistance and endothelial dysfunction: the road map to cardiovascular diseases. Diabetes Metab Res Rev 22:423–436. https://doi.org/10.1002/dmrr.634
Choi YJ, Yoon Y, Lee KY, Hien TT, Kang KW, Kim KC, Lee J, Lee MY, Lee SM, Kang DH, Lee BH (2014) Uric acid induces endothelial dysfunction by vascular insulin resistance associated with the impairment of nitric oxide synthesis. FASEB J Off Publ Fed Am Soc Exp Biol 28:3197–3204. https://doi.org/10.1096/fj.13-247148
De Becker B, Coremans C, Chaumont M, Delporte C, Van Antwerpen P, Franck T, Rousseau A, Zouaoui Boudjeltia K, Cullus P, van de Borne P (2019) Severe hypouricemia impairs endothelium-dependent vasodilatation and reduces blood pressure in healthy young men: a randomized, placebo-controlled, and crossover study. J Am Heart Assoc 8:e013130. https://doi.org/10.1161/jaha.119.013130
De Nigris V, Pujadas G, La Sala L, Testa R, Genovese S, Ceriello A (2015) Short-term high glucose exposure impairs insulin signaling in endothelial cells. Cardiovasc Diabetol 14:114. https://doi.org/10.1186/s12933-015-0278-0
Desideri G, Castaldo G, Lombardi A, Mussap M, Testa A, Pontremoli R, Punzi L, Borghi C (2014) Is it time to revise the normal range of serum uric acid levels? Eur Rev Med Pharmacol Sci 18:1295–1306
Duncan ER, Crossey PA, Walker S, Anilkumar N, Poston L, Douglas G, Ezzat VA, Wheatcroft SB, Shah AM, Kearney MT (2008) Effect of endothelium-specific insulin resistance on endothelial function in vivo. Diabetes 57:3307–3314. https://doi.org/10.2337/db07-1111
Duplain H, Burcelin R, Sartori C, Cook S, Egli M, Lepori M, Vollenweider P, Pedrazzini T, Nicod P, Thorens B, Scherrer U (2001) Insulin resistance, hyperlipidemia, and hypertension in mice lacking endothelial nitric oxide synthase. Circulation 104:342–345
El Ridi R, Tallima H (2017) Physiological functions and pathogenic potential of uric acid: a review. J Adv Res 8:487–493. https://doi.org/10.1016/j.jare.2017.03.003
Fang J, Alderman MH (2000) Serum uric acid and cardiovascular mortality the NHANES I epidemiologic follow-up study, 1971–1992. National Health and Nutrition Examination Survey. JAMA 283:2404–2410. https://doi.org/10.1001/jama.283.18.2404
Fisslthaler B, Benzing T, Busse R, Fleming I (2003) Insulin enhances the expression of the endothelial nitric oxide synthase in native endothelial cells: a dual role for Akt and AP-1. Nitric Oxide 8:253–261. https://doi.org/10.1016/s1089-8603(03)00042-9
George J, Carr E, Davies J, Belch JJ, Struthers A (2006) High-dose allopurinol improves endothelial function by profoundly reducing vascular oxidative stress and not by lowering uric acid. Circulation 114:2508–2516. https://doi.org/10.1161/circulationaha.106.651117
Gersch C, Palii SP, Kim KM, Angerhofer A, Johnson RJ, Henderson GN (2008) Inactivation of nitric oxide by uric acid. Nucleosides Nucleotides Nucleic Acids 27:967–978. https://doi.org/10.1080/15257770802257952
Ghasemi A (2021) Uric acid-induced pancreatic β-cell dysfunction. BMC Endocr Disord 21:24. https://doi.org/10.1186/s12902-021-00698-6
Godber BL, Doel JJ, Sapkota GP, Blake DR, Stevens CR, Eisenthal R, Harrison R (2000) Reduction of nitrite to nitric oxide catalyzed by xanthine oxidoreductase. J Biol Chem 275:7757–7763. https://doi.org/10.1074/jbc.275.11.7757
Grayson PC, Kim SY, LaValley M, Choi HK (2011) Hyperuricemia and incident hypertension: a systematic review and meta-analysis. Arthritis Care Res 63:102–110. https://doi.org/10.1002/acr.20344
Hao L, Zhou Y, Xu H (2019) A study of the correlation between vitamin D uric acid levels and senile acute cerebral infarction. Int J Clin Exp Med 12:9343–9350
Hermann C, Assmus B, Urbich C, Zeiher AM, Dimmeler S (2000) Insulin-mediated stimulation of protein kinase Akt: a potent survival signaling cascade for endothelial cells. Arterioscler Thromb Vasc Biol 20:402–409. https://doi.org/10.1161/01.atv.20.2.402
Hille R, Nishino T (1995) Xanthine oxidase and xanthine dehydrogenase. FASEB J 9:995–1003. https://doi.org/10.1096/fasebj.9.11.7649415
Hong Q, Qi K, Feng Z, Huang Z, Cui S, Wang L, Fu B, Ding R, Yang J, Chen X, Wu D (2012) Hyperuricemia induces endothelial dysfunction via mitochondrial Na+/Ca2+ exchanger-mediated mitochondrial calcium overload. Cell Calcium 51:402–410. https://doi.org/10.1016/j.ceca.2012.01.003
Houston M, Estevez A, Chumley P, Aslan M, Marklund S, Parks DA, Freeman BA (1999) Binding of xanthine oxidase to vascular endothelium. Kinetic characterization and oxidative impairment of nitric oxide-dependent signaling. J Biol Chem 274:4985–4994. https://doi.org/10.1074/jbc.274.8.4985
Ichimori K, Fukahori M, Nakazawa H, Okamoto K, Nishino T (1999) Inhibition of xanthine oxidase and xanthine dehydrogenase by nitric oxide. Nitric oxide converts reduced xanthine-oxidizing enzymes into the desulfo-type inactive form. J Biol Chem 274:7763–7768. https://doi.org/10.1074/jbc.274.12.7763
Jakše B, Jakše B, Pajek M, Pajek J (2019) Uric acid and plant-based nutrition. Nutrients 11:1736. https://doi.org/10.3390/nu11081736
Johnson RJ, Gaucher EA, Sautin YY, Henderson GN, Angerhofer AJ, Benner SA (2008) The planetary biology of ascorbate and uric acid and their relationship with the epidemic of obesity and cardiovascular disease. Med Hypotheses 71:22–31. https://doi.org/10.1016/j.mehy.2008.01.017
Johnson RJ, Sautin YY, Oliver WJ, Roncal C, Mu W, Gabriela Sanchez-Lozada L, Rodriguez-Iturbe B, Nakagawa T, Benner SA (2009) Lessons from comparative physiology: could uric acid represent a physiologic alarm signal gone awry in western society? J Comp Physiol [B] 179:67–76. https://doi.org/10.1007/s00360-008-0291-7
Kang DH, Park SK, Lee IK, Johnson RJ (2005) Uric acid-induced C-reactive protein expression: implication on cell proliferation and nitric oxide production of human vascular cells. J Am Soc Nephrol 16:3553–3562. https://doi.org/10.1681/asn.2005050572
Kato M, Hisatome I, Tomikura Y, Kotani K, Kinugawa T, Ogino K, Ishida K, Igawa O, Shigemasa C, Somers VK (2005) Status of endothelial dependent vasodilation in patients with hyperuricemia. Am J Cardiol 96:1576–1578. https://doi.org/10.1016/j.amjcard.2005.07.068
Kelley EE, Hock T, Khoo NK, Richardson GR, Johnson KK, Powell PC, Giles GI, Agarwal A, Lancaster JR Jr, Tarpey MM (2006) Moderate hypoxia induces xanthine oxidoreductase activity in arterial endothelial cells. Free Radical Biol Med 40:952–959. https://doi.org/10.1016/j.freeradbiomed.2005.11.008
Kellogg EW 3rd, Fridovich I (1977) Liposome oxidation and erythrocyte lysis by enzymically generated superoxide and hydrogen peroxide. J Biol Chem 252:6721–6728
Kim J-a, Montagnani M, Koh KK, Quon MJ (2006) Reciprocal relationships between insulin resistance and endothelial dysfunction. Circulation 113:1888–1904. https://doi.org/10.1161/CIRCULATIONAHA.105.563213
Kim SY, Guevara JP, Kim KM, Choi HK, Heitjan DF, Albert DA (2010) Hyperuricemia and coronary heart disease: a systematic review and meta-analysis. Arthritis Care Res 62:170–180. https://doi.org/10.1002/acr.20065
Ko J, Kang HJ, Kim DA, Kim MJ, Ryu ES, Lee S, Ryu JH, Roncal C, Johnson RJ, Kang DH (2019) Uric acid induced the phenotype transition of vascular endothelial cells via induction of oxidative stress and glycocalyx shedding. FASEB J Off Publ Fed Am Soc Exp Biol 33:13334–13345. https://doi.org/10.1096/fj.201901148R
Kodama S, Saito K, Yachi Y, Asumi M, Sugawara A, Totsuka K, Saito A, Sone H (2009) Association between serum uric acid and development of type 2 diabetes. Diabetes Care 32:1737–1742. https://doi.org/10.2337/dc09-0288
Komori H, Yamada K, Tamai I (2018) Hyperuricemia enhances intracellular urate accumulation via down-regulation of cell-surface BCRP/ABCG2 expression in vascular endothelial cells. Biochim Biophys Acta 1860:973–980. https://doi.org/10.1016/j.bbamem.2018.01.006
Konta T, Ichikawa K, Kawasaki R, Fujimoto S, Iseki K, Moriyama T, Yamagata K, Tsuruya K, Narita I, Kondo M, Shibagaki Y, Kasahara M, Asahi K, Watanabe T (2020) Association between serum uric acid levels and mortality: a nationwide community-based cohort study. Sci Rep 10:6066. https://doi.org/10.1038/s41598-020-63134-0
Kuzkaya N, Weissmann N, Harrison DG, Dikalov S (2005) Interactions of peroxynitrite with uric acid in the presence of ascorbate and thiols: implications for uncoupling endothelial nitric oxide synthase. Biochem Pharmacol 70:343–354. https://doi.org/10.1016/j.bcp.2005.05.009
Lai J-H, Luo S-F, Hung L-F, Huang C-Y, Lien S-B, Lin L-C, Liu F-C, Yen BL, Ho L-J (2017) Physiological concentrations of soluble uric acid are chondroprotective and anti-inflammatory. Sci Rep 7:2359. https://doi.org/10.1038/s41598-017-02640-0
Li L, Yang C, Zhao Y, Zeng X, Liu F, Fu P (2014) Is hyperuricemia an independent risk factor for new-onset chronic kidney disease?: A systematic review and meta-analysis based on observational cohort studies. BMC Nephrol 15:122–122. https://doi.org/10.1186/1471-2369-15-122
Li P, Zhang L, Zhang M, Zhou C, Lin N (2016) Uric acid enhances PKC-dependent eNOS phosphorylation and mediates cellular ER stress: a mechanism for uric acid-induced endothelial dysfunction. Int J Mol Med 37:989–997. https://doi.org/10.3892/ijmm.2016.2491
Liang WY, Zhu XY, Zhang JW, Feng XR, Wang YC, Liu ML (2015) Uric acid promotes chemokine and adhesion molecule production in vascular endothelium via nuclear factor-kappa B signaling. Nutr Metab Cardiovasc Dis 25:187–194. https://doi.org/10.1016/j.numecd.2014.08.006
Liu S, Yuan Y, Zhou Y, Zhao M, Chen Y, Cheng J, Lu Y, Liu J (2017) Phloretin attenuates hyperuricemia-induced endothelial dysfunction through co-inhibiting inflammation and GLUT9-mediated uric acid uptake. J Cell Mol Med 21:2553–2562. https://doi.org/10.1111/jcmm.13176
Lu J, He Y, Cui L, Xing X, Liu Z, Li X, Zhang H, Li H, Sun W, Ji A, Wang Y, Yin H, Li C (2020) Hyperuricemia pedisposes to the onset of diabetes via promoting pancreatic β-cell death in uricase-deficient male mice. Diabetes 69:1149–1163. https://doi.org/10.2337/db19-0704
Lv Q, Meng XF, He FF, Chen S, Su H, Xiong J, Gao P, Tian XJ, Liu JS, Zhu ZH, Huang K, Zhang C (2013) High serum uric acid and increased risk of type 2 diabetes: a systemic review and meta-analysis of prospective cohort studies. PLoS ONE 8:e56864. https://doi.org/10.1371/journal.pone.0056864
Madonna R, Pandolfi A, Massaro M, Consoli A, De Caterina R (2004) Insulin enhances vascular cell adhesion molecule-1 expression in human cultured endothelial cells through a pro-atherogenic pathway mediated by p38 mitogen-activated protein-kinase. Diabetologia 47:532–536. https://doi.org/10.1007/s00125-004-1330-x
Maeno Y, Li Q, Park K, Rask-Madsen C, Gao B, Matsumoto M, Liu Y, Wu IH, White MF, Feener EP, King GL (2012) Inhibition of insulin signaling in endothelial cells by protein kinase C-induced phosphorylation of p85 subunit of phosphatidylinositol 3-kinase (PI3K). J Biol Chem 287:4518–4530. https://doi.org/10.1074/jbc.M111.286591
Maiuolo J, Oppedisano F, Gratteri S, Muscoli C, Mollace V (2016) Regulation of uric acid metabolism and excretion. Int J Cardiol 213:8–14. https://doi.org/10.1016/j.ijcard.2015.08.109
Martillo MA, Nazzal L, Crittenden DB (2014) The crystallization of monosodium urate. Curr Rheumatol Rep 16:400–400. https://doi.org/10.1007/s11926-013-0400-9
Martínez-Sánchez FD, Vargas-Abonce VP, Guerrero-Castillo AP, Santos-Villavicencio ML, Eseiza-Acevedo J, Meza-Arana CE, Gulias-Herrero A, Gómez-Sámano M (2020) Serum Uric Acid concentration is associated with insulin resistance and impaired insulin secretion in adults at risk for Type 2 Diabetes. Prim Care Diabetes. https://doi.org/10.1016/j.pcd.2020.10.006
Maruhashi T, Hisatome I, Kihara Y, Higashi Y (2018) Hyperuricemia and endothelial function: from molecular background to clinical perspectives. Atherosclerosis 278:226–231. https://doi.org/10.1016/j.atherosclerosis.2018.10.007
Mishima M, Hamada T, Maharani N, Ikeda N, Onohara T, Notsu T, Ninomiya H, Miyazaki S, Mizuta E, Sugihara S (2016) Effects of uric acid on the NO production of HUVECs and its restoration by urate lowering agents. Drug Research 66:270–274
Montagnani M, Golovchenko I, Kim I, Koh GY, Goalstone ML, Mundhekar AN, Johansen M, Kucik DF, Quon MJ, Draznin B (2002) Inhibition of phosphatidylinositol 3-kinase enhances mitogenic actions of insulin in endothelial cells. J Biol Chem 277:1794–1799. https://doi.org/10.1074/jbc.M103728200
Muniyappa R, Chen H, Montagnani M, Sherman A, Quon MJ (2020) Endothelial dysfunction due to selective insulin resistance in vascular endothelium: insights from mechanistic modeling. Am J Phys Endocrinol Metab 319:E629–E646. https://doi.org/10.1152/ajpendo.00247.2020
Muniyappa R, Iantorno M, Quon MJ (2008) An integrated view of insulin resistance and endothelial dysfunction. Endocrinol Metab Clin North Am 37:685–x. https://doi.org/10.1016/j.ecl.2008.06.001
Muraoka S, Miura T (2003) Inhibition by uric acid of free radicals that damage biological molecules. Pharmacol Toxicol 93:284–289. https://doi.org/10.1111/j.1600-0773.2003.pto930606.x
Ndrepepa G (2018) Uric acid and cardiovascular disease. Clin Chim Acta Int J Clin Chem 484:150–163. https://doi.org/10.1016/j.cca.2018.05.046
Oliver FJ, De la Rubia G, Feener E, Lee M, Loeken M, Shiba T, Quertermous T, King G (1991) Stimulation of endothelin-1 gene expression by insulin in endothelial cells. J Biol Chem 266:23251–23256
Osses N, Pearson JD, Yudilevich DL, Jarvis SM (1996) Hypoxanthine enters human vascular endothelial cells (ECV 304) via the nitrobenzylthioinosine-insensitive equilibrative nucleoside transporter. Biochem J 317(Pt 3):843–848. https://doi.org/10.1042/bj3170843
Otani N, Toyoda S, Sakuma M, Hayashi K, Ouchi M, Fujita T, Anzai N, Tanaka A, Node K, Uemura N, Inoue T (2018) Effects of uric acid on vascular endothelial function from bedside to bench. Hypertens Res 41:923–931. https://doi.org/10.1038/s41440-018-0095-4
Panus PC, Wright SA, Chumley PH, Radi R, Freeman BA (1992) The contribution of vascular endothelial xanthine dehydrogenase/oxidase to oxygen-mediated cell injury. Arch Biochem Biophys 294:695–702. https://doi.org/10.1016/0003-9861(92)90743-g
Park J-H, Jin YM, Hwang S, Cho D-H, Kang D-H, Jo I (2013) Uric acid attenuates nitric oxide production by decreasing the interaction between endothelial nitric oxide synthase and calmodulin in human umbilical vein endothelial cells: a mechanism for uric acid-induced cardiovascular disease development. Nitric Oxide 32:36–42. https://doi.org/10.1016/j.niox.2013.04.003
Partridge CA, Blumenstock FA, Malik AB (1992) Pulmonary microvascular endothelial cells constitutively release xanthine oxidase. Arch Biochem Biophys 294:184–187. https://doi.org/10.1016/0003-9861(92)90155-P
Potenza MA, Marasciulo FL, Chieppa DM, Brigiani GS, Formoso G, Quon MJ, Montagnani M (2005) Insulin resistance in spontaneously hypertensive rats is associated with endothelial dysfunction characterized by imbalance between NO and ET-1 production. Am J Physiol Heart Circ Physiol 289:H813-822. https://doi.org/10.1152/ajpheart.00092.2005
Price KL, Sautin YY, Long DA, Zhang L, Miyazaki H, Mu W, Endou H, Johnson RJ (2006) Human vascular smooth muscle cells express a urate transporter. J Am Soc Nephrol 17:1791–1795. https://doi.org/10.1681/asn.2006030264
Radi R, Tan S, Prodanov E, Evans RA, Parks DA (1992) Inhibition of xanthine oxidase by uric acid and its influence on superoxide radical production. Biochim Biophys Acta Protein Struct Mol Enzymol 1122:178–182. https://doi.org/10.1016/0167-4838(92)90321-4
Rask-Madsen C, King GL (2013) Vascular complications of diabetes: mechanisms of injury and protective factors. Cell Metab 17:20–33. https://doi.org/10.1016/j.cmet.2012.11.012
Rask-Madsen C, Li Q, Freund B, Feather D, Abramov R, Wu IH, Chen K, Yamamoto-Hiraoka J, Goldenbogen J, Sotiropoulos KB, Clermont A, Geraldes P, Dall’Osso C, Wagers AJ, Huang PL, Rekhter M, Scalia R, Kahn CR, King GL, (2010) Loss of insulin signaling in vascular endothelial cells accelerates atherosclerosis in apolipoprotein E null mice. Cell Metab 11:379–389. https://doi.org/10.1016/j.cmet.2010.03.013
Rouquette M, Page S, Bryant R, Benboubetra M, Stevens CR, Blake DR, Whish WD, Harrison R, Tosh D (1998) Xanthine oxidoreductase is asymmetrically localised on the outer surface of human endothelial and epithelial cells in culture. FEBS Lett 426:397–401. https://doi.org/10.1016/s0014-5793(98)00385-8
Sánchez-Lozada LG, Lanaspa MA, Cristóbal-García M, García-Arroyo F, Soto V, Cruz-Robles D, Nakagawa T, Yu MA, Kang DH, Johnson RJ (2012) Uric acid-induced endothelial dysfunction is associated with mitochondrial alterations and decreased intracellular ATP concentrations. Nephron Exp Nephrol 121:e71–e78. https://doi.org/10.1159/000345509
Sánchez-Lozada LG, Soto V, Tapia E, Avila-Casado C, Sautin YY, Nakagawa T, Franco M, Rodríguez-Iturbe B, Johnson RJ (2008) Role of oxidative stress in the renal abnormalities induced by experimental hyperuricemia. Am J Physiol Renal Physiol 295:F1134-1141. https://doi.org/10.1152/ajprenal.00104.2008
Sánchez-Lozada LG, Tapia E, Santamaría J, Avila-Casado C, Soto V, Nepomuceno T, Rodríguez-Iturbe B, Johnson RJ, Herrera-Acosta J (2005) Mild hyperuricemia induces vasoconstriction and maintains glomerular hypertension in normal and remnant kidney rats. Kidney Int 67:237–247. https://doi.org/10.1111/j.1523-1755.2005.00074.x
Schlotte V, Sevanian A, Hochstein P, Weithmann KU (1998) Effect of uric acid and chemical analogues on oxidation of human low density lipoprotein in vitro. Free Radical Biol Med 25:839–847. https://doi.org/10.1016/s0891-5849(98)00160-9
Schulman IH, Zhou MS (2009) Vascular insulin resistance: a potential link between cardiovascular and metabolic diseases. Curr Hypertens Rep 11:48–55. https://doi.org/10.1007/s11906-009-0010-0
Schwartz IF, Grupper A, Chernichovski T, Grupper A, Hillel O, Engel A, Schwartz D (2011) Hyperuricemia attenuates aortic nitric oxide generation, through inhibition of arginine transport, in rats. J Vasc Res 48:252–260. https://doi.org/10.1159/000320356
So A, Thorens B (2010) Uric acid transport and disease. J Clin Investig 120:1791–1799. https://doi.org/10.1172/jci42344
Sorensen LB (1965) Role of the intestinal tract in the elimination of uric acid. Arthritis Rheum Off J Am Coll Rheumatol 8:694–706
Sugihara S, Hisatome I, Kuwabara M, Niwa K, Maharani N, Kato M, Ogino K, Hamada T, Ninomiya H, Higashi Y, Ichida K, Yamamoto K (2015) Depletion of uric acid due to SLC22A12 (URAT1) loss-of-function mutation causes endothelial dysfunction in hypouricemia. Circ J 79:1125–1132. https://doi.org/10.1253/circj.CJ-14-1267
Tabit CE, Shenouda SM, Holbrook M, Fetterman JL, Kiani S, Frame AA, Kluge MA, Held A, Dohadwala MM, Gokce N, Farb MG, Rosenzweig J, Ruderman N, Vita JA, Hamburg NM (2013) Protein kinase C-β contributes to impaired endothelial insulin signaling in humans with diabetes mellitus. Circulation 127:86–95. https://doi.org/10.1161/circulationaha.112.127514
Tan S, Radi R, Gaudier F, Evans RA, Rivera A, Kirk KA, Parks DA (1993) Physiologic levels of uric acid inhibit xanthine oxidase in human plasma. Pediatr Res 34:303–307. https://doi.org/10.1203/00006450-199309000-00013
Tanigaki K, Mineo C, Yuhanna IS, Chambliss KL, Quon MJ, Bonvini E, Shaul PW (2009) C-reactive protein inhibits insulin activation of endothelial nitric oxide synthase via the immunoreceptor tyrosine-based inhibition motif of FcgammaRIIB and SHIP-1. Circ Res 104:1275–1282. https://doi.org/10.1161/circresaha.108.192906
Tassone EJ, Cimellaro A, Perticone M, Hribal ML, Sciacqua A, Andreozzi F, Sesti G, Perticone F (2018) Uric acid impairs insulin signaling by promoting Enpp1 binding to insulin receptor in human umbilical vein endothelial cells. Front Endocrinol (Lausanne) 9:98–98. https://doi.org/10.3389/fendo.2018.00098
Vicent D, Ilany J, Kondo T, Naruse K, Fisher SJ, Kisanuki YY, Bursell S, Yanagisawa M, King GL, Kahn CR (2003) The role of endothelial insulin signaling in the regulation of vascular tone and insulin resistance. J Clin Investig 111:1373–1380. https://doi.org/10.1172/JCI15211
Wang J, Qin T, Chen J, Li Y, Wang L, Huang H, Li J (2014) Hyperuricemia and risk of incident hypertension: a systematic review and meta-analysis of observational studies. PLoS ONE 9:e114259. https://doi.org/10.1371/journal.pone.0114259
Wang R, Song Y, Yan Y, Ding Z (2016) Elevated serum uric acid and risk of cardiovascular or all-cause mortality in people with suspected or definite coronary artery disease: a meta-analysis. Atherosclerosis 254:193–199. https://doi.org/10.1016/j.atherosclerosis.2016.10.006
Waring WS, McKnight JA, Webb DJ, Maxwell SRJ (2006) Uric acid restores endothelial function in patients with type 1 diabetes and regular smokers. Diabetes 55:3127–3132. https://doi.org/10.2337/db06-0283
Williams AW, Wilson DM (1990) Uric acid metabolism in humans. Semin Nephrol 10:9–14
Wright AF, Rudan I, Hastie ND, Campbell H (2010) A ‘complexity’ of urate transporters. Kidney Int 78:446–452. https://doi.org/10.1038/ki.2010.206
Xie H, Sun J, Chen Y, Zong M, Li S, Wang Y (2015) EGCG attenuates uric acid-induced inflammatory and oxidative stress responses by medicating the NOTCH pathway. Oxid Med Cell Longev 2015:214836–214836. https://doi.org/10.1155/2015/214836
Xu L, Shi Y, Zhuang S, Liu N (2017) Recent advances on uric acid transporters. Oncotarget 8:100852–100862. https://doi.org/10.18632/oncotarget.20135
Yang B, Li S, Zhu J, Huang S, Zhang A, Jia Z, Ding G, Zhang Y (2020) MiR-214 protects against uric acid-induced endothelial cell apoptosis. Front Med 7:411
Yang X, Gu J, Lv H, Li H, Cheng Y, Liu Y, Jiang Y (2019) Uric acid induced inflammatory responses in endothelial cells via upregulating (pro)renin receptor. Biomed Pharmacother 109:1163–1170. https://doi.org/10.1016/j.biopha.2018.10.129
Yu MA, Sánchez-Lozada LG, Johnson RJ, Kang DH (2010) Oxidative stress with an activation of the renin-angiotensin system in human vascular endothelial cells as a novel mechanism of uric acid-induced endothelial dysfunction. J Hypertens 28:1234–1242
Yuan H, Hu Y, Zhu Y, Zhang Y, Luo C, Li Z, Wen T, Zhuang W, Zou J, Hong L, Zhang X, Hisatome I, Yamamoto T, Cheng J (2017) Metformin ameliorates high uric acid-induced insulin resistance in skeletal muscle cells. Mol Cell Endocrinol 443:138–145. https://doi.org/10.1016/j.mce.2016.12.025
Yuan H, Yu C, Li X, Sun L, Zhu X, Zhao C, Zhang Z, Yang Z (2015) Serum uric acid levels and risk of metabolic syndrome: a dose-response meta-analysis of prospective studies. J Clin Endocrinol Metab 100:4198–4207
Zhang Y, Zhan RX, Chen JQ, Gao Y, Chen L, Kong Y, Zhong XJ, Liu MQ, Chu JJ, Yan GQ, Li T, He M, Huang QR (2015) Pharmacological activation of PPAR gamma ameliorates vascular endothelial insulin resistance via a non-canonical PPAR gamma-dependent nuclear factor-kappa B trans-repression pathway. Eur J Pharmacol 754:41–51. https://doi.org/10.1016/j.ejphar.2015.02.004
Zhao L, Cao L, Zhao TY, Yang X, Zhu XX, Zou HJ, Wan WG, Xue Y (2020) Cardiovascular events in hyperuricemia population and a cardiovascular benefit-risk assessment of urate-lowering therapies: a systematic review and meta-analysis. Chin Med J 133:982–993. https://doi.org/10.1097/cm9.0000000000000682
Zharikov S, Krotova K, Hu H, Baylis C, Johnson RJ, Block ER, Patel J (2008) Uric acid decreases NO production and increases arginase activity in cultured pulmonary artery endothelial cells. Am J Physiol Cell Physiol 295:C1183-1190. https://doi.org/10.1152/ajpcell.00075.2008
Zhen H, Gui F (2017) The role of hyperuricemia on vascular endothelium dysfunction. Biomed Rep 7:325–330. https://doi.org/10.3892/br.2017.966
Zhi L, Yuzhang Z, Tianliang H, Hisatome I, Yamamoto T, Jidong C (2016) High uric acid induces insulin resistance in cardiomyocytes in vitro and in vivo. PLoS ONE 11:e0147737. https://doi.org/10.1371/journal.pone.0147737
Zhu Y, Hu Y, Huang T, Zhang Y, Li Z, Luo C, Luo Y, Yuan H, Hisatome I, Yamamoto T, Cheng J (2014) High uric acid directly inhibits insulin signalling and induces insulin resistance. Biochem Biophys Res Commun 447:707–714. https://doi.org/10.1016/j.bbrc.2014.04.080
Zoccali C, Maio R, Mallamaci F, Sesti G, Perticone F (2006) Uric acid and endothelial dysfunction in essential hypertension. J Am Soc Nephrol 17:1466–1471. https://doi.org/10.1681/asn.2005090949
Zuo T, Liu X, Jiang L, Mao S, Yin X, Guo L (2016) Hyperuricemia and coronary heart disease mortality: a meta-analysis of prospective cohort studies. BMC Cardiovasc Disord 16:207. https://doi.org/10.1186/s12872-016-0379-z
Zweier JL, Kuppusamy P, Lutty GA (1988) Measurement of endothelial cell free radical generation: evidence for a central mechanism of free radical injury in postischemic tissues. Proc Natl Acad Sci 85:4046–4050
Funding
This study has been supported by Shahid Beheshti University of Medical Sciences (Grant Number 25401), Tehran, Iran.
Author information
Authors and Affiliations
Contributions
Idea and conceptualization: Asghar Ghasemi and Zahra Bahadoran
Writing, reviewing, and editing: Zahra Bahadoran, Asghar Ghasemi, Khosrow Kashfi, Parvin Mirmiran
Literature research: Zahra Bahadoran, Asghar Ghasemi, Khosrow Kashfi, Parvin Mirmiran
Figure conceptualization and design: Zahra Bahadoran and Asghar Ghasemi
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the special issue on pathophysiological mechanisms of cardiometabolic diseases in Pflügers Archiv—European Journal of Physiology
Rights and permissions
About this article
Cite this article
Bahadoran, Z., Mirmiran, P., Kashfi, K. et al. Hyperuricemia-induced endothelial insulin resistance: the nitric oxide connection. Pflugers Arch - Eur J Physiol 474, 83–98 (2022). https://doi.org/10.1007/s00424-021-02606-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-021-02606-2