Abstract
Cholera toxin is commonly known to induce chloride secretion of the intestine. In recent years, effects on epithelial barrier function have been reported, indicating synergistic co-regulation of transporters and tight junction proteins. Our current study focused on the analysis of cholera toxin effects on transepithelial resistance and on tight junction proteins, the latter known as structural correlates of barrier function. Ligated segments of the rat jejunum were injected with buffered solution containing cholera toxin (1 μg/ml) and incubated for 4 h. Subsequently, selfsame tissue specimens were mounted in Ussing chambers, and cholera toxin (1 μg/ml) was added on the apical side. Transepithelial resistance and permeability of sodium fluorescein (376 Da) were analyzed. Subsequently, tissues were removed, expression and localization of claudins were analyzed, and morphological studies were performed employing transmission electron microscopy and confocal laser scanning microscopy. Cholera toxin induced a marked decrease in transepithelial resistance in the rat jejunal epithelium and an increase in paracellular permeability for sodium fluorescein. Immunoblotting of tight junction proteins revealed an increase in claudin-2 signals, which was verified by confocal laser scanning immunofluorescence microscopy, and a decrease in tricellulin, whereas other tight junction proteins remained unchanged. Transmission electron microscopy showed a reduction in the number of microvilli after incubation with cholera toxin. Moreover, cholera toxin led to a widening of the intercellular space between enterocytes. In accordance with the commonly known prosecretory effect of cholera toxin, our study revealed a complementary effect on small intestinal barrier function and integrity, which might constitute a pathomechanism with high relevance for prevention and therapeutic approaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
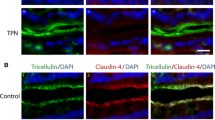
In recent years, studies of epithelial physiology indicate a synergy of ion transport and barrier properties. Transcellular absorption of nutrients or secretion of anions in the small intestinal epithelium is supported by claudin-2 and claudin-15, which allow a back-leakage of sodium ions into the intestinal cavity, thus complementing transcellular transport mechanisms [25,26,27,28]. In contrast, in the epithelium of the colon, the transcellular movement of sodium ions induced by aldosterone is associated with the expression of claudin-8, which prevents the back-leakage of already absorbed Na+ ions into the intestinal cavity [3]. Induction of colonic chloride ion secretion by cholera toxin (Ctx) is paralleled by in an increase in tightening claudin-3 and claudin-4 [16].
The main effect of Ctx on small intestinal epithelial cells is to induce a secretion of chloride ions through cystic fibrosis transmembrane conductance regulator (CFTR) channels [1]. It is generally accepted that in parallel to chloride secretion, sodium ions diffuse along the paracellular pathway. Therefore, CFTR drives an efflux of Cl− ions and the resulting charge promotes a lumen-directed flux of Na+ [9]. Claudin-2 is an important mediator for the latter, providing a selective paracellular channel for small cations and water [2, 23, 28]. Claudin-2 has been reported to be strongly expressed in segments of the small intestine [15]. However, an even higher relevance for paracellular permeability for larger molecules has been attributed to tricellulin [12, 21] To date, analyses of claudin expression in the small intestinal epithelium treated with Ctx are limited.
Moreover, Ctx represents a proven adjuvant for obtaining food allergy [14]. A change in paracellular permeability is considered a likely mechanism for the development of food allergy, implying an increase in the supply of antigens and the direction of the T helper 2 (TH2) cell response [29]. Molecular mechanisms for increasing the permeability of antigens are still limited, though.
As the small intestine provides the main pathophysiological target for diarrhea caused by Ctx due to non-compensable induction of ion secretion and as Ctx is used as an adjuvant for food allergy, this segment merits an in-depth analysis of barrier effects. Therefore, the current study focused on this subject on both functional and molecular levels.
Materials and methods
Chemicals
All chemicals, unless otherwise noted, were purchased from Sigma-Aldrich (St. Louis, MO, USA).
Animals
Male Wistar rats weighing 200–250 g (n = 9) were used in the experiments. The animals were kept in vivarium conditions on a standard diet with free access to food and water. The studies were carried out in accordance with the rules adopted by the organizations for working with laboratory animals FELASA and Rus-LASA and authorized by decision No. 131-03-1 of the ethical committee of St. Petersburg State University on work with animals.
Methods
Experimental study design
Animals were anesthetized by intraperitoneal administration of Zoletil (Virbac, France) at a rate of 100 μg per kilogram of body weight in combination with intramuscular injection of 40 μl of a 0.02% solution of xylazine hydrochloride (Pharmamagist Ltd., Hungary). The intestinal segment was exteriorized without damaging the mesentery. Two segments with a length of about 5 cm were selected on the exposed site, each of which was ligated on both sides. After ligation, 400 μl of Krebs-Ringer’s solution containing Ctx (1 μg/ml) was injected into one of the sections, whereas 400 μl of solution without Ctx was injected in the second section serving as a control. The intestinal segments with ligatures were placed back into the abdominal cavity, and animals were monitored for 4 h. Subsequently, animals were sacrificed by decapitation and the intestine was excised. From each site (control and treatment), a fragment was cut out for the subsequent study of the transepithelial resistance (TER) and permeability to fluorescein using Ussing chambers. Another tissue sample from each segment was harvested for Western blot and transmission electron microscopy.
Electrophysiological measurements
After preparation, jejunal tissue specimens were mounted in Ussing chambers and 5 ml circulating Ringer’s solution was added on each side. The solution contained (in mM) Na+ (140.5), K+ (5.4), Ca2+ (1.2), Mg2+ (1.2), Cl− (123.8), HCO3− (21), HPO42− (2.4), H2PO4− (0.6), and D-glucose (10). During all experiments, the solution was gassed with 95% O2 and 5% CO2 at 37 °C with pH adjusted to 7.4. For measurement of TER in Ussing chambers, a preamplifier (model EVC-3, World Precision Instruments, USA) and a voltage clamp device (EVC-4000, World Precision Instruments, USA) were employed. Specimens of the rat jejunum were incubated with Ctx on the apical side for 1 h.
Paracellular permeability for sodium fluorescein
To detect the contribution of the paracellular pathway to the barrier properties of the epithelium, Na-fluorescein with a molecular mass of 376 Da and a complex size of 4.5 Å was used. According to experimental data, Na-fluorescein diffuses across the paracellular space from both the apical side to the basolateral side and back, regardless of the electrochemical gradient between the apical and basolateral surface of the epithelial cells [19].
Na-fluorescein at a concentration of 100 μmol/l was added from the apical side of the tissue after it was mounted into the Ussing chamber. After completion of the experiment, the solution from the basolateral side was selected to determine the concentration of Na-fluorescein diffused through tissue on a Cary Eclipse Fluorescence Spectrophotometer (Agilent, Santa Clara, CA, USA) at an excitation wavelength of 460 nm and an absorption wavelength of 515 nm. Calculation of the coefficient of permeability for Na-fluorescein was carried out according to the formula:
where dQ / dt is the amount of Na-fluorescein in the solution on the basolateral side at the end of the experiment divided by the length of the flux period (mol/s), A is the exposed area of tissue (cm2), and C0 is the concentration of Na-fluorescein in the solution on the apical side at the beginning of the flux period (M); apparent permeability (Papp) is expressed in centimeter per second.
Immunoblotting
Tissues were homogenized in Tris buffer containing (in mM) Tris (20), MgCl2 (5), EDTA (1), EGTA (0.3), and protease inhibitors (Complete, Boehringer, Mannheim, Germany). Membrane fractions were obtained by two centrifugation steps (5 min at 200×g and 30 min at 43,000×g, 4 °C). Pellets were resuspended in Tris buffer. Total protein contents were determined using a BCA protein assay reagent (Pierce, Rockford, IL, USA) quantified with a plate reader (Tecan, Grodig, Austria). Samples were loaded onto 10% Mini-PROTEAN TGX Stain-Free Protein Gels (Bio-Rad, Munich, Germany) and electrophoresed.
Proteins were assessed by immunoblotting employing rabbit anti-occludin, anti-claudin-1, claudin-2, claudin-3, and claudin-15, and anti-tricellulin primary antibodies in a concentration of 1:100 according to the manufacturer’s protocols (Invitrogen, San Francisco, CA, USA). Signals were visualized by luminescence imaging employing the chemiluminescence detection system Lumi-LightPLUS Western blotting kit (Roche, Mannheim, Germany). Chemiluminescence signals were detected using a ChemiDoc MP (Bio-Rad, Munich, Germany) luminescence imager. For quantification, the Image Lab Software (Bio-Rad, Hercules, USA) was used to perform background subtraction and normalization to the inter-run calibrator, followed by normalization to beta actin as the standard protein.
Confocal laser scanning microscopy
Tissues were fixed in 2% paraformaldehyde and embedded in paraffin as reported recently [16]. Rabbit (polyclonal) anti-claudin-2 and mouse (monoclonal) anti-occludin were employed, respectively (Invitrogen, San Francisco, CA, USA). Antibodies were diluted to 1:100 in blocking solution according to the manufacturer’s recommendations, respectively. Tissues were incubated with the respective antibody solution for 60 min and, after two washes, were incubated with Alexa Fluor goat anti-mouse IgG and Alexa Fluor goat anti-rabbit IgG diluted to 1:500 in blocking solution for 45 min (Molecular Probes, Eugene, OR, USA). Sections were mounted with ProTags MountFluor (BioCyc, Luckenwalde, Germany). Fluorescence images were obtained with microscopes of the Zeiss Meta series (Zeiss, Jena, Germany).
Electron microscopy
Fixation of tissue samples was performed in 2.5% glutaraldehyde and Hanks’ balanced salt solution (pH = 7.0) at 4 °C for 2 h as reported [24]. Subsequently, tissues were postfixed in osmium tetroxide solution (1% OsO4 in Hanks’ solution) at 4 °C for 2 h and block stained with 2% uranyl acetate buffer at 40 °C for 1 h, dehydrated in ethanol and acetone, and embedded in Spurr. Ultrathin sections were obtained employing the ultramicrotome LKB-8800 (LKB, Sweden) and were stained with uranyl acetate and lead citrate. A JEM-100C microscope (JEOL, Tokyo, Japan) was used for examination of the sections. Intercellular spaces were estimated using the suitable common ImageJ default option for surface calculation.
Statistical analysis
Data are expressed as mean ± standard error of the mean (SEM), and the Wilcoxon test and Student’s t test were performed, with n indicating the number of experiments. Paired comparison of data was performed by a one-tailed t test. Statistical significance was defined at p ≤ 0.05.
Results
Ussing chamber experiments
After 4-h incubation of ligated jejunal loops with Ctx, TER was lower than that in control tissue samples (34.2 ± 11.4 versus 55.6 ± 18.2 Ω cm2, respectively; p < 0.05, n = 9; Fig. 1a). This lower TER of Ctx-pretreated samples was still observed after 1 h (34.7 ± 11.3 Ω cm2). Flux measurement employing fluorescein revealed a permeability of 2.8 ± 2.0·10−3 cm/s in control tissue. Ctx induced a significant increase in permeability for fluorescein in jejunal epithelia to 5.4 ± 2.3·10−3 cm/s (p < 0.05, n = 7; Fig. 1b).
Functional permeability measures of isolated jejunal epithelia measured in Ussing chambers following a 4-h pretreatment in vivo without (control) or with Ctx. a Ctx induced a markedly decreased transepithelial resistance (TER) vs. control tissues (p < 0.05, n = 9). b In accordance, permeability for sodium fluorescein was increased (p < 0.05, n = 7)
In contrast, transepithelial voltage and short-circuit current as measures of ion transport were not significantly changed: 1.34 ± 0.12 mV (control) vs. 1.82 ± 0.12 mV (Ctx) and 39.3 ± 13.3 μA (control) vs. 37.5 ± 13.7 μA (Ctx; n = 11 and 9, respectively).
Transmission electron microscopy
Transmission electron microscopy was employed to analyze the ultrastructural changes in jejunal enterocytes. Ultrathin sections of jejunal control tissue revealed elongated enterocytes with characteristic cylindrical shape and oval nuclei in the basal compartment (Fig. 2a). The cells of the surface epithelium, closely adhering to each other, formed a tissue barrier between the intestinal cavity and the intercellular fluid. In the upper part of the lateral region of the plasma membrane, tight junctions were detectable as electron-dense structures with a characteristic apparent fusion of plasma membranes (Fig. 2b). An intercellular space between neighboring cells was not detectable. On the apical part of the enterocytes, tightly adjacent microvilli were visible, forming a brush rim (Fig. 2c).
Transmission electron microscopy of jejunal control tissue. a Sections of control tissue revealed elongated enterocytes with characteristic cylindrical shape closely adhering to each other and oval nuclei at the basal cell. b Tight junctions were detectable as electron-dense structures with a characteristic apparent fusion of plasma membranes. c Tightly adjacent microvilli were visible, forming a brush rim (bars: left panel, 1 μm; right panels, 0.1 μm)
Ctx did not induce a destruction of tight junctions in rat enterocytes, as the integrity of single epithelial cell layers persisted, but Ctx led to an increase in intercellular spaces (Fig. 3a, b). In control tissue specimens, the area of the intercellular space was 0.09 ± 0.03 μm2, while it was increased to 8.5 ± 4.9 μm2 after incubation with Ctx. In addition, Ctx led to a significant decrease in the number of microvilli on the apical surface of enterocytes, compared with the control tissue of the jejunum (Fig. 3c). The density of the microvilli in the control samples was 6.3 ± 0.2 per 1 μm of the apical cell surface. While under the influence of Ctx, this index decreased markedly and was 2.3 ± 0.4 per 1 μm of the apical surface of the cell (p < 0.01, n = 5).
Transmission electron microscopy of the Ctx-incubated jejunum. a While the integrity of single epithelial cell layers was preserved, b Ctx led to an increase in intercellular spaces. c A decrease in the number of microvilli on the apical surface of enterocytes was observed (bars: left panel, 1 μm; right panels, 0.1 μm)
Immunoblots
Immunoblotting was performed detecting major tight junction proteins with relevance for paracellular permeability for ions and molecules, namely occludin, claudin-1, claudin-2, claudin-3, claudin-15, and tricellulin (Fig. 4a). Densitometric analyses of immunoblot signals revealed increased signals of claudin-2 to 175% of controls after incubation with Ctx (n = 5, p < 0.05) and decreased tricellulin to 51% of controls (n = 4, p < 0.05) whereas occludin, claudin-1, claudin-3, and claudin-15 were not significantly changed (n = 4, respectively; Fig. 4b).
Immunoblots detecting occludin (ocln), claudin-1 (cld-1), cld-2, cld-3, cld-15, tricellulin (tric), and beta actin. a Representative immunoblots. b Densitometry. Markedly increased signals of claudin-2 were observed after incubation with Ctx, as well as a decrease in tricellulin, whereas other claudins were not significantly changed (n = 4 to 5, respectively)
Confocal laser scanning microscopy
Confocal laser scanning microscopy after immunostaining with antibodies raised against claudin-2 revealed an increase in signals in the apicolateral membrane of enterocytes after incubation with Ctx (Fig. 5), which was in accordance with the increased abundance of claudin-2 in Western blots; counterstaining with mouse anti-occludin revealed co-localization within tight junction complexes (Fig. 5).
Confocal laser scanning microscopy. Immunofluorescent staining employing antibodies raised against claudin-2 (red) revealed an increase in signals in the apicolateral membrane of enterocytes after incubation with Ctx, in accordance with Western blots in co-localization with occludin (green; bars, 20 μm)
Discussion
In the rat colon, Ctx has been reported to be a regulator of both transport and barrier functions [16]. Since the pathophysiology of cholera is typically linked to small intestinal fluid secretion [5], the current study focused on barrier effects of Ctx on the jejunal epithelium, including an assessment of electrophysiological, ultrastructural, morphological, and molecular parameters. By means of electrophysiological techniques, we found that the effect of Ctx lowers TER of the rat jejunal epithelium and increases the paracellular permeability for solutes. This finding provides important disease-relevant aspects, as the commonly discussed pathophysiological mechanism of Ctx, namely induction of a non-compensable chloride secretion, primarily occurs in the small intestine [9]. This segment is dominated by a Cl− current mediated by apical CFTR channels [5], but for effective net ion and water movement, the permeability of respective counter ions and water is also relevant [8].
Our study reveals that claudin-2 is elevated after Ctx incubation and tricellulin is reduced, both explaining the strong diarrheal effects in this segment. Whereas claudin-2 has been reported to be a selective paracellular pore for the passage of small cations and water [2, 22], tricellulin has been reported to determine the barrier for macromolecules in tricellular cell contact sites [11]. Therefore, a simultaneous increase in claudin-2 and a decrease in tricellulin would explain a synergistic enhancement of paracellular permeability for ions and larger solutes, as detected by TER and fluorescein flux measurements, respectively. In this light, particularly the effects on tricellulin would be in accordance with the common use of Ctx as an adjuvant for obtaining food allergy [14].
In contrast, other main determinants of jejunal epithelial barrier function, namely the sealing tight junction proteins claudin-1 and claudin-3, as well as the Na+ permeability mediating claudin-15 [27], were not changed. This reflects also segment-specific action of Ctx along the longitudinal axis of the gastrointestinal tract [16], in accordance with the distinct expression pattern of tight junction proteins, respectively [15].
Varying results regarding intestinal Ctx effects have been reported recently. In a CFTR-deficient mouse model, it was shown that the intestinal protein level of claudin-2 was elevated compared with wild type, while the expression of tightening claudins was not significantly different [6]. In contrast and in accordance with our current study, in Ctx-treated Caco-2 cells, claudin-2 staining had been reported to induce markedly increased signals compared with untreated cells [10]. However, the latter study also indicated an interaction of chloride channels and a change in tight junction contacts and protein expression, resulting in a functional synergism between the movement of chloride ions through the plasma membrane and the paracellular pathway of cations and water. Moreover, Liu et al. have observed an effect of cholera toxin on claudin-2 in an intestinal allergy mouse model and further analyzed the effect in colonic carcinoma cells, rather uniquely addressing the effect on claudin-2 to a transcellular permeability of macromolecular tracers [13]. Our study now shows the impact on the classic paracellular barrier function, affected by claudin-2 and tricellulin in selfsame tissues of the healthy control jejunum of rats, though.
The functional relationship of CFTR and epithelial barrier properties, provided by tight junction proteins, is currently discussed [4], as an interplay of CFTR and tight junction organization in the cystic fibrosis airway epithelium has been reported. However, among chloride channels, CFTR has not been localized in tight junction complex areas [22]. As Ctx increases the cAMP levels necessary for CFTR function [4], this signaling molecule might be considered a second messenger that also changes the level of claudin expression. A direct evidence for this effect on claudin-2 expression has not been given to date, though. Perhaps the difference in the expression of tight junction proteins is determined by the specific interaction of CFTR with different transports or signaling molecules in these types of epithelial cells including Na-K-ATPase [22]. In turn, ATPase can enter into a functional connection with other ion channels [17]. As effects on tight junction proteins were detected on the protein level, the effects are most likely mediated by gene expression and/or localization. As information on different tight junction protein signaling and CFTR currently still is limited, further interpretation may be addressed soon, though.
The impact of Ctx on cell physiology is impressively shown by TEM, demonstrating major effects on fluid movement and villus architecture, reflecting aberrant morphology. Thus, another possible intracellular mechanism, pointed out by various authors, is associated with the conjugation of CFTR and the actin cytoskeleton [4, 20]. The subject becomes more complex given that depending on crypt/villous localization, different outcomes regarding morphology could be observed [7, 18].
Further studies might reveal the molecular mechanism between CFTR and change of tight junction protein expression and localization, in detail. However, for the understanding of Ctx toxicology and pathophysiology, it is necessary to include a detailed consideration of the paracellular pathway.
References
Alzamora R, O’Mahony F, Harvey BJ (2011) Estrogen inhibits chloride secretion caused by cholera and Escherichia coli enterotoxins in female rat distal colon. Steroids 76:867–876. https://doi.org/10.1016/j.steroids.2011.04.016
Amasheh S, Meiri N, Gitter AH, Schöneberg T, Mankertz J, Schulzke JD, Fromm M (2002) Claudin-2 expression induces cation-selective channels in tight junctions of epithelial cells. J Cell Sci 115(Pt 24:4969–4976. https://doi.org/10.1242/jcs.00165
Amasheh S, Milatz S, Krug SM, Bergs M, Amasheh M, Schulzke JD, Fromm M (2009) Na+ absorption defends from paracellular back-leakage by claudin-8 upregulation. Biochem Biophys Res Commun 378(1):45–50. https://doi.org/10.1016/j.bbrc.2008.10.164
Castellani S, Favia M, Guerra L, Carbone A, Abbattiscianni AC, Di Gioia S, Casavola V, Conese M (2017) Emerging relationship between CFTR, actin and tight junction organization in cystic fibrosis airway epithelium. Histol Histopathol 32(5):445–459. https://doi.org/10.14670/HH-11-842
Clarke LL, Grubb BR, Gabriel SE, Smithies O, Koller BH, Boucher RC (1992) Defective epithelial chloride transport in a gene-targeted mouse model of cystic fibrosis. Science 257(5073):1125–1128
De Lisle RC (2014) Disrupted tight junctions in the small intestine of cystic fibrosis mice. Cell Tissue Res 355(1):131–142. https://doi.org/10.1007/s00441-013-1734-3
DiBona DR, Chen LC, Sharp GW (1974) A study of intercellular spaces in the rabbit jejunum during acute volume expansion and after treatment with cholera toxin. J Clin Invest 53(5):1300–1307
Fan S, Harfoot N, Bartolo RC, Butt AG (2012) CFTR is restricted to a small population of high expresser cells that provide a forskolin-sensitive transepithelial Cl- conductance in the proximal colon of the possum Trichosurus vulpecula. J Exp Biol 215(Pt 7:1218–1230. https://doi.org/10.1242/jeb.061176
Gabriel SE, Brigman KN, Koller BH, Boucher RC, Stutts MJ (1994) Cystic fibrosis heterozygote resistance to cholera toxin in the cystic fibrosis mouse model. Science 266(5182):107–109
Guichard A, Cruz-Moreno B, Aguilar B, van Sorge NM, Kuang J, Kurkciyan AA, Wang Z, Hang S, Pineton de Chambrun GP, McCole DF, Watnick P, Nizet V, Bier E (2013) Cholera toxin disrupts barrier function by inhibiting exocyst-mediated trafficking of host proteins to intestinal cell junctions. Cell Host Microbe 14(3):294–305. https://doi.org/10.1016/j.chom.2013.08.001
Ikenouchi J, Furuse M, Furuse K, Sasaki K, Tsukita S, Tsukita S (2005) Tricellulin constitutes a novel barrier at tricellular contacts of epithelial cells. J Cell Biol 171:939–945. https://doi.org/10.1083/jcb.200510043
Krug SM, Amasheh S, Richter JF, Milatz S, Günzel D, Westphal JK, Huber O, Schulzke JD, Fromm M (2009) Tricellulin forms a barrier to macromolecules in tricellular tight junctions without affecting ion permeability. Mol Biol Cell 20:3713–3724. https://doi.org/10.1091/mbc.e09-01-0080
Liu X, Yang G, Geng XR, Cao Y, Li N, Ma L, Chen S, Yang PC, Liu Z (2013) Microbial products induce claudin-2 to compromise gut epithelial barrier function. PLoS One 8:e68547. https://doi.org/10.1371/journal.pone.0068547
Marinaro M, Staats HF, Hiroi T, Jackson RJ, Coste M, Boyaka PN, Okahashi N, Yamamoto M, Kiyono H, Bluethmann H, Fujihashi K, McGhee JR (1995) Mucosal adjuvant effect of cholera toxin in mice results from induction of T helper 2 (Th2) cells and IL-4. J Immunol 155(10):4621–4629
Markov AG, Veshnyakova A, Fromm M, Amasheh M, Amasheh S (2010) Segmental expression of claudin proteins correlates with tight junction barrier properties in rat intestine. J Comp Physiol B 180(4):591–598. https://doi.org/10.1007/s00360-009-0440-7
Markov AG, Falchuk EL, Kruglova NM, Rybalchenko OV, Fromm M, Amasheh S (2014) Comparative analysis of theophylline and cholera toxin in rat colon reveals an induction of sealing tight junction proteins. Pflugers Arch 466(11):2059–2065. https://doi.org/10.1007/s00424-014-1460-z
Matchkov VV, Krivoi II (2016) Specialized functional diversity and interactions of the Na,K-ATPase. Front Physiol 7:179. https://doi.org/10.3389/fphys.2016.00179
Mathan MM, Chandy G, Mathan VI (1995) Ultrastructural changes in the upper small intestinal mucosa in patients with cholera. Gastroenterology. 109(2):422–430
Molenda N, Urbanova K, Weiser N, Kusche-Vihrog K, Günzel D, Schillers H (2014) Paracellular transport through healthy and cystic fibrosis bronchial epithelial cell lines–do we have a proper model? PLoS One 9(6):e100621. https://doi.org/10.1371/journal.pone.0100621
Nilsson HE, Dragomir A, Lazorova L, Johannesson M, Roomans GM (2010) CFTR and tight junctions in cultured bronchial epithelial cells. Exp Mol Pathol 88(1):118–127. https://doi.org/10.1016/j.yexmp.2009.09.018
Radloff J, Cornelius V, Markov AG, Amasheh S (2019) Caprate modulates intestinal barrier function in porcine Peyer’s patch follicle-associated epithelium. Int J Mol Sci 20(6):E1418. https://doi.org/10.3390/ijms20061418
Rajasekaran SA, Beyenbach KW, Rajasekaran AK (2008) Interactions of tight junctions with membrane channels and transporters. Biochim Biophys Acta 1778(3):757–769
Rosenthal R, Milatz S, Krug SM, Oelrich B, Schulzke JD, Amasheh S, Günzel D, Fromm M (2010) Claudin-2, a component of the tight junction, forms a paracellular water channel. J Cell Sci 123(Pt 11:1913–1921. https://doi.org/10.1242/jcs.060665
Rybalchenko OV, Bondarenko VM, Orlova OG, Markov AG, Amasheh S (2015) Inhibitory effects of Lactobacillus fermentum on microbial growth and biofilm formation. Arch Microbiol 197(8):1027–1032. https://doi.org/10.1007/s00203-015-1140-1
Tamura A, Kitano Y, Hata M, Katsuno T, Moriwaki K, Sasaki H, Hayashi H, Suzuki Y, Noda T, Furuse M, Tsukita S, Tsukita S (2008) Megaintestine in claudin-15-deficient mice. Gastroenterology 134(2):523–534. https://doi.org/10.1053/j.gastro.2007.11.040
Tanaka H, Tamura A, Suzuki K, Tsukita S (2017) Site-specific distribution of claudin-based paracellular channels with roles in biological fluid flow and metabolism. Ann N Y Acad Sci 1405(1):44–52. https://doi.org/10.1111/nyas.13438
Wada M, Tamura A, Takahashi N, Tsukita S (2013) Loss of claudins 2 and 15 from mice causes defects in paracellular Na+ flow and nutrient transport in gut and leads to death from malnutrition. Gastroenterology 144(2):369–380. https://doi.org/10.1053/j.gastro.2012.10.035
Yu AS (2009) Molecular basis for cation selectivity in claudin-2-based pores. Ann N Y Acad Sci 1165:53–57. https://doi.org/10.1111/j.1749-6632.2009.04023.x
Yu W, Hussey Freeland DM, Nadeau KC (2016) Food allergy: immune mechanisms, diagnosis and immunotherapy. Nat Rev Immunol 16:751–765. https://doi.org/10.1038/nri.2016.111
Funding
This research was sponsored by a grant from the Russian Research Foundation (No. 18-15-00043), a grant from the Saint Petersburg State University (No. 0.37.218.2016), a grant from the Deutsche Forschungsgemeinschaft (AM 141/11-1), and the Partnership Program Freie Universität Berlin-Saint Petersburg State University.
Author information
Authors and Affiliations
Contributions
Performed research: AGM, ONV, LSO, AAF, NMK, OVR
Analyzed data: AGM, JRA, SA
Contributed new methods or models: AGM, JRA, SA
Wrote the paper: AGM, JRA, SA
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Markov, A.G., Vishnevskaya, O.N., Okorokova, L.S. et al. Cholera toxin perturbs the paracellular barrier in the small intestinal epithelium of rats by affecting claudin-2 and tricellulin. Pflugers Arch - Eur J Physiol 471, 1183–1189 (2019). https://doi.org/10.1007/s00424-019-02294-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-019-02294-z