Abstract
Fibroblast growth factor 23 (FGF23) levels are elevated in patients with acute kidney injury (AKI). The consequences on renal Ca2+, Mg2+, and Pi regulatory mechanisms are unknown. We hypothesized that renal ischemia-reperfusion (I/R) injury alters the expression of important renal Ca2+, Mg2+, and Pi transport proteins. I/R injury was induced in male C57BL/6 mice by clamping both renal arteries for 27 min. Mice were investigated 18 h later. The mRNA and protein levels of renal Ca2+, Mg2+, and Pi transport proteins were measured by RT-qPCR and western blot analysis. I/R injury-induced hyperphosphatemia and hypermagnesemia were paralleled by a decrease in glomerular filtration rate and an increase in the fractional excretion of Ca2+, Mg2+, and Pi. I/R injury affected the fibroblast growth factor 23 (FGF23)-klotho-vitamin D axis by increasing plasma levels of FGF23 and downregulation of renal klotho expression. Plasma levels of PTH and 1,25-dihydroxyvitamin D3 were unchanged. Further, downregulation of key genes for paracellular reabsorption of Ca2+ and Mg2+ (claudin (Cldn)2, Cldn10b, Cldn16, Cldn19) and for active transcellular transport of Ca2+, Mg2+, and Pi (calbindin-D28K, Ncx1, Pmca4, Cnnm2, Trpm7, NaPi-2a, and NaPi-2c) was observed. However, renal expression of Trpv5 and Trpv6 was increased. In vitro studies support a direct effect of proinflammatory cytokines on the mRNA expression of Cldn16, Cldn19, and Trpv6. Our findings indicate that renal I/R injury increases FGF23 blood levels independent of PTH and 1,25-dihydroxyvitamin D3. This increase is associated with hypermagnesemia, hyperphosphatemia, and increased or decreased expression of specific renal Ca2+, Mg2+, and Pi transporters, respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) is a major clinical problem without effective therapy and may lead to chronic kidney disease (CKD) [66]. Ischemia-reperfusion (I/R) injury causes AKI in various clinical settings including hypotension, sepsis, kidney transplantation, and aortic bypass surgery [6], and is associated with high morbidity and mortality [9]. The clinical consequences of renal I/R injury depend on the severity of the injury, and ranges from minor changes in renal function to a requirement for dialysis or transplantation. Renal I/R injury results from a generalized or localized reduction in renal blood flow leading to hypoxia. As a result, tubular epithelial cell injury with functional impairment of water and electrolyte homeostasis, including calcium (Ca2+), magnesium (Mg2+), and phosphate (Pi) deregulations, develops [5, 11, 20, 62]. However, the underlying mechanisms for electrolyte disturbances have not been fully defined.
Fibroblast growth factor (FGF) 23 was originally described as a bone-derived hormone that mainly affects renal function via the FGF receptor (FGFR). FGF23 is involved in renal phosphate reabsorption, the modulation of the production of parathyroid hormone (PTH) and 1,25-dihydroxyvitamin D3 (1,25(OH)2D3), and in the control of mineral homeostasis. FGF23 and PTH increase renal Pi excretion mainly due to a downregulation of type II sodium-dependent Pi co-transporters (NaPi-2a and NaPi-2c) in proximal tubules [22, 29]. Further, FGF23, PTH, and 1,25(OH)2D3 modulate renal Ca2+ reabsorption by increasing the apical membrane expression of transient receptor potential vanilloid-5 (Trpv5) abundance and activity in distal tubules [5]. In addition, FGF23 suppresses and PTH stimulates renal 1,25(OH)2D3 synthesis, which depends on Cyp24a1 and Cyp27b1 gene expression. Cyp24a1 and Cyp27b1 encode the enzymes 24-hydroxylase and 1α-hydroxylase, respectively, which are responsible for renal 1,25(OH)2D3 degradation and synthesis. Both renal Cyp24a1 and Cyp27b1 are highly regulated: PTH stimulates the expression of Cyp27b1 in the kidney, whereas FGF23 downregulates it, and FGF23 strongly induces the expression of Cyp24a1, whereas PTH reduces its expression [3, 4, 43, 50, 58].
Increased FGF23 levels have been observed after dietary phosphate loading, administration of interleukin-1β (IL-1β), IL-6, PTH, or 1,25(OH)2D3, and most notably during CKD [12, 16, 53]. Subsequently, also non-osseous tissues, including the kidney, for example, have been reported to express and secret FGF23 in response to inflammation or AKI, for example [16, 19, 49]. In proximal and distal renal tubules, the FGFR1 is probably the dominant FGF receptor mediating the effects of FGF23 [21]. Renal FGF23 signaling requires the presence of the co-receptor αKlotho (klotho) on target cells [21]. In CKD, the decrease in klotho expression has been suggested to contribute to renal FGF23 resistance and a maladaptive increase in circulating FGF23, leading to an impaired mineral metabolism [48, 51]. Thus, FGF23 has been implicated in the development of secondary hyperparathyroidism in CKD [48]. Increased levels of FGF23 and decreased levels of klotho also are well-described findings in patients with AKI and in animal models of AKI, and are associated with an adverse outcome [10, 16, 26, 34, 45, 57]. More recently, we found that lipopolysaccharide-induced AKI, which is associated with hypocalcemia and hyperphosphatemia and a disturbed FGF23-klotho-vitamin D signaling, was accompanied by an altered expression of specific renal Ca2+ and Pi transporters [42]. Therefore, one may assume that AKI due to renal I/R injury could also be associated with an impaired FGF23-klotho-vitamin D signaling [23, 26], leading to an alteration in Ca2+ and Pi homeostasis. However, the consequences of such alterations on renal Ca2+ and Pi regulatory mechanisms in response to I/R injury are still unclear. We therefore hypothesized that I/R injury alters the expression of important renal Ca2+ and Pi transport proteins. In addition, we characterized the impact of I/R injury on FGF23-klotho-vitamin D signaling and on renal Mg2+ transport regulation.
Methods
Animals
All animal experiments were conducted according to the National Institutes of Health Guide for the Care and Use of Laboratory Animals and were approved by the local animal protection committee. Male C57BL/6J mice (7 weeks old) were obtained from Charles River (Sulzfeld, Germany), and were acclimated for at least 1 week in the animal facility with free access to standard chow (V1534-300; Ssniff Spezialdäten GmbH Soest, Germany) containing 1.00% Ca2+, 0.22% Mg2+, and 0.70% phosphate and received water ad libitum. Mice were kept in cages in groups of two to four individuals at 23 °C under a 12-h/12-h dark (6 p.m.–6 a.m.)/light (6 a.m.–6 p.m.) cycle.
Induction of renal I/R injury model
Mice were anesthetized with isofluorane and I/R was undertaken as described previously [54]. In brief, mice received subcutaneous injections of 250 μL of 0.9% saline and buprenorphine (0.05 mg/kg) as analgesic substance. Briefly, after visualizing both renal pedicles through a mid-line abdominal incision, the arteries of both kidneys were clamped individually with a non-traumatic microvascular clamp for 27 min. The time of ischemia was chosen to obtain a reversible model of ischemic acute renal failure and to avoid animal mortality [31]. Renal ischemia was confirmed by blanching of kidneys. In sham controls, renal arteries were only touched with forceps. After ischemia, the clamps were released for the kidneys to start the reperfusion. Thereafter, the abdominal wound was sutured and the mouse was kept on a heating pad until it gained full consciousness. Mice were killed after 18 h of reperfusion, blood was collected in tubes containing lithium-heparin, and the kidneys were quickly removed, frozen in liquid nitrogen, and stored at − 80 °C until extraction of total RNA or protein.
In addition, both sham control and I/R injury mice were placed in metabolic cages for 24 h on the day before the surgery for acclimatization. Two hours after the surgery, these mice were replaced in metabolic cages for 16 h to collect urine. No mouse died before the study was finalized.
Histology
Kidneys from sham-operated and I/R-treated mice were fixed in 4% paraformaldehyde solution by retrograde perfusion through the abdominal aorta [55]. The fixed kidneys were then dehydrated, embedded in paraffin, and cut into 5 μm sections. To evaluate morphological damage, paraffin-embedded sections containing all kidney zones were stained with periodic acid-Schiff (PAS) stain according to the manufacturer’s protocol (Sigma-Aldrich, Germany).
Primary proximal tubule and distal tubule cells and mouse kidney thick ascending limb cell line
Primary proximal tubule (PT) cells and distal tubule cells (DTCs) were isolated and cultured as described previously [42, 55]. Mouse kidney thick ascending limb (MKTAL) cells were cultured in DMEM/HAM-F12 (1:1) (Lonza) containing 5% (vol/vol) FCS and 2 mM l-glutamine, at 37 °C in a humidity-controlled incubator with 5% (vol/vol) CO2 [7]. The cells were grown in culture medium until confluent and then in serum- and hormone-free medium for 24 h before use. Thereafter, cells were treated with or without a mixture of TNFα and IL-1β (100 ng/mL each) for 24 h. Murine recombinant cytokines were used for the experiments from PeproTech.
Biochemical and analytical methods
Urea, Pi, and total Mg2+ and Ca2+ levels were measured using colorimetric assays according to the manufacturer’s protocol (ArborAssays, Ann Arbor, MI; BioAssay Systems, Hayward, CA). Plasma creatinine concentrations were determined using a commercially available enzymatic colorimetric assay according to the manufacturer’s protocol (LT-SYS, Labor + Technik, Berlin, Germany). Urine creatinine concentrations were determined using a commercially available colorimetric assay according to the manufacturer’s protocol (ArborAssays, Ann Arbor). Plasma PTH was measured with a mouse PTH 1-84 ELISA kit (Immutopics, San Clemente, CA). Plasma 1,25-dihydroxyvitamin D3 was determined with a mouse 1,25-dihydroxyvitamin D3 ELISA kit (Cusabio Biotech Co., LTD., Wuhan, P.R.China). Plasma levels of FGF23 were determined with a mouse/rat FGF23 (Intact) ELISA kit (Immutopics, San Clemente, CA). FE of Ca2+ was calculated using the formula: ([urine Ca2+] × [serum creatinine] × 100) / ([urine creatinine] × [serum Ca2+]). FE of Mg2+ and Pi were calculated in accordance.
Real-time quantitative PCR
Total tissue and cell RNAs were extracted with TRIzol Reagent (Invitrogen) according to the manufacturer’s instruction. Total RNA was reverse transcribed into cDNA according to standard protocols as described previously [39]. Real-time PCR was performed in a LightCycler 480 (Roche, Mannheim, Germany). All PCR experiments were conducted using the LightCycler DNA Master SYBR Green I kit provided by Roche Molecular Biochemicals (Mannheim, Germany) as described previously [25]. PCR primers are listed in Table 1 or have been described previously by us [42, 54].
Immunoblotting
Protein preparation and immunoblotting were performed as described previously [41]. In brief, protein samples were electrophoretically separated on 15 or 10% polyacrylamide gels and transferred to nitrocellulose membranes, which were blocked overnight in 5% nonfat dry milk diluted in Tris-buffered saline with 0.1% Tween-20, and then incubated for 1 h at room temperature with antibodies against calbindin-D28K (CB300, SWANT, Bellinzona, Switzerland; 1:2000; expected size of ~ 28 kDa), Trpv5 (SC-30187, Santa Cruz Biotechnology, Santa Cruz, CA; 1:1000; expected size of ~ 75 kDa), Trpv6 (CAT11-A, Alpha Diagnostics International, San Antonio, TX; 1:1000; expected size of ~ 85 kDa), Trpm6 (Alomone Labs, ACC-046, 1:1000, expected size ~ 233 kDa), Trpm7 (Alomone Labs, ACC-047, 1:1000, expected size ~ 212 kDa), NCX1 (π 11-13; Swant, 1:1000; expected size of ~ 120 kDa for full length protein and of ~ 70 kDa for active proteolytic fragment), Claudin (Cldn)16 (Zymed Laboratories Inc., 1:500; expected size ~ 34 kDa), Cldn19 (Sigma-Aldrich, SAB2100440, 1:500, expected size ~ 23 kDa), β-actin (A5316, Sigma-Aldrich; 1:5000; expected size of ~ 43 kDa), or klotho (ab75023, Abcam plc, Cambridge, UK; 1:1000; expected size of ~ 116 kDa). After being washed, the membrane was incubated for 2 h with a secondary antibody (Santa Cruz Biotechnology; 1:2000) and subjected to a chemiluminescence detection system. Quantitative assessment of band densities was performed densitometrically using ImageJ Software. The Trpv5 antibody has been used previously by others [37, 47, 52, 65].
Statistical analyses
Results are presented as means ± SEM. Statistical comparisons were made by a two-sided Student’s unpaired t test. A P value < 0.05 was considered significant.
Results
I/R injury worsens renal function
I/R injury did not alter food and water intake, but clearly induced AKI, which is reflected by a decrease in creatinine clearance (Table 2). As expected, sections from sham-operated mice exhibited no evidence of structural damage (Fig. 1a). I/R injury resulted in extensive changes in renal morphology, including destruction of tubules and cast formation (Fig. 1a), and an elevation of plasma creatinine and urea concentration (Fig. 1b). In addition, renal mRNA expression of the tubular injury markers neutrophil gelatinase-associated lipocalin (NGAL) and kidney injury molecule-1 (KIM-1) was increased in the kidneys with I/R injury (Fig. 1c). The increase in tubular injury markers was paralleled by an increase in the renal mRNA expression of interleukin (IL)-1β, IL-6, and tumor necrosis factor (TNF)α (Fig. 1d).
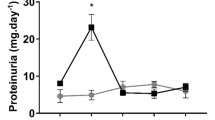
Ischemia-reperfusion (I/R) injury worsened renal function and induced hyperphosphatemia and hypermagnesemia. Effect of I/R injury (18 h) on a renal histological changes (PAS staining of kidneys), plasma levels of b creatinine and urea, c renal NGAL and KIM-1 mRNA, d renal IL-1β, IL-6, and TNFα mRNA expression related to β-actin mRNA expression and on plasma levels of e Pi, f total Ca2+, and g total Mg2+. Values are mean ± SEM for six animals. *P < 0.05 vs. control
I/R injury induces hypermagnesemia and hyperphosphatemia
To investigate the consequences of I/R-induced AKI on electrolyte homeostasis, we determined blood levels and urinary excretion of Ca2+, Mg2+, and Pi. I/R injury caused an increase in plasma levels of Pi (Fig. 1e) and Mg2+ (Fig. 1g). Blood Ca2+ levels were not different from control levels 18 h after induction of I/R injury (Fig. 1f). To investigate the effect of I/R injury on the urinary excretion of Ca2+, Mg2+, and Pi, we placed mice in metabolic cages and collected urine over a period of 16 h. We found that I/R injury increased the FE of Pi, Ca2+, and Mg2+ (Table 2). However, the total urinary excretion of Ca2+ and Mg2+ was decreased in response to I/R injury (Table 2). I/R injury increased total urinary excretion of Pi (Table 2).
I/R injury increases blood levels of fibroblast growth factor 23 and decreases renal klotho expression
In order to determine whether renal I/R results in altered FGF23-klotho signaling, we investigated blood FGF23 levels. FGF23 levels were increased in response to I/R injury (Fig. 2a). Renal mRNA levels of FGF23 and of the primary FGF23 receptor FGFR1 were also increased (Fig. 2b), while klotho expression was decreased (Fig. 2b, c).
Ischemia-reperfusion (I/R) injury and cytokines altered FGF23-klotho-signaling in vivo and in vitro. Effect of renal I/R (18 h) on a plasma levels fibroblast growth factor 23 (FGF23), b renal FGF23, FGFR1, and klotho mRNA expression related to β-actin mRNA expression, and c on renal klotho protein expression related to β-actin protein expression. Effect of a cytokine mixture (Cyto-Mix; IL-1β and TNFα; each 100 ng/mL) on FGFR1 and klotho mRNA expression related to β-actin mRNA expression in d primary proximal tubule cells and e in primary distal tubule cells after 16 h. Shown are representative immunoblots for klotho and β-actin protein. Values are mean ± SEM for six animals or for four independent in vitro experiments. *P < 0.05 vs. control
Proinflammatory cytokines decrease klotho mRNA expression in vitro
To examine a possible direct effect of proinflammatory cytokines, we incubated primary PT cells and DTCs with a combination of TNFα and IL-1β. Addition of the cytokine mixture decreased klotho mRNA expression in PT cells (Fig. 2d) and DTCs (Fig. 2e). Incubation of primary PT cells with cytokines increased the expression of FGFR1 (Fig. 2d). Further, the combination of TNFα with IL-1β did not alter the expression of FGFR1 mRNA in DTCs (Fig. 2e).
I/R injury does not alter blood levels of parathyroid hormone and renal vitamin D synthesis
Next, we investigated the effect of I/R injury on blood levels of major hormones involved in Ca2+ and Pi homeostasis. I/R injury did not alter plasma levels of PTH (Fig. 3a). Similarly, plasma concentration of 1,25(OH)2D3 was not different from controls (Fig. 3b). In accordance with this observation, renal 1,25-dihydroxyvitamin D3 24-hydroxylase (Cyp24a1) mRNA expression was increased and the mRNA expression of the primary vitamin D regulatory enzyme 25-hydroxyvitamin D3 1α-hydroxylase (Cyp27b1) was decreased in response to I/R injury (Fig. 3c).
Ischemia-reperfusion (I/R) injury did not alter plasma levels of PTH and renal vitamin D synthesis. Effect of renal I/R (18 h) on plasma levels of a parathyroid hormone (PTH), b 1,25-dihydroxyvitamin D3 (1,25(OH)2D3), and c renal Cyp27b1 and Cyp24a1 mRNA expression related to β-actin mRNA expression. Values are mean ± SEM for six animals. *P < 0.05 vs. control
I/R injury alters the expression of crucial renal phosphate, calcium, and magnesium transporters
To characterize the impact of renal I/R injury on tubular electrolyte transport regulation, the renal expression of Ca2+, Mg2+, and Pi transporters was determined. I/R injury decreased the renal mRNA expression of NaPi-2a and NaPi-2c (Fig. 4). In contrast, the renal mRNA expression of NaPi-2b and PiT1 was increased, whereas the mRNA abundance of PiT2 was unaltered (Fig. 4). Further, I/R injury increased renal Trpv5 and Trpv6 mRNA abundance (Fig. 5a), whereas renal calbindin-D28K, plasma membrane Ca2+-ATPase (Pmca) 4, and Na+/Ca2+-exchanger (Ncx1) mRNA abundance were decreased (Fig. 5a). The renal mRNA expression level of Pmca1b was unaltered (Fig. 5a). In addition, the increase in renal Trpv5 and Trpv6 expression as well as the decrease in renal Ncx1 and calbindin-D28K expression were confirmed on the protein level (Fig. 5b, c). I/R injury did not alter the renal expression of transient receptor potential channel melastatin (Trpm) 6, but decreased abundance of Trpm7 (Fig. 6a, b). Further, I/R injury decreased the mRNA expression of Na+-Mg2+-exchanger solute carrier family (Slc) 41a3 and of parvalbumin (Fig. 6a). In addition, I/R injury did not alter the renal mRNA expression of Slc41a1, but decreased the mRNA abundance of ancient conserved domain protein 2/cyclin M2 (Cnnm) 2 (Fig. 6a).
Ischemia-reperfusion (I/R) injury altered the renal mRNA expression of tubular calcium transporters. Effect of renal I/R (18 h) on a renal Trpv5, Trpv6, calbindin-D28K, Ncx1, Pmca1b, and Pmca4 mRNA expression related to β-actin mRNA expression. b, c Effect of renal I/R (18 h) on renal Trpv5, Trpv6, Ncx1, and calbindin-D28K protein expression related to β-actin protein expression. Shown are representative immunoblots. Values are mean ± SEM for six animals. *P < 0.05 vs. control
Ischemia-reperfusion (I/R) injury altered the renal expression of tubular magnesium transporters. Effect of renal I/R (18 h) on a renal Trpm6, Trpm7, parvalbumin, Slc4a1, Slc41a3, and Cnnm2 mRNA expression related to β-actin mRNA expression, and b effect of renal I/R injury (18 h) on Trpm6 and Trpm7 protein expression related to β-actin protein expression. Inset shows representative immunoblot. Values are mean ± SEM for six animals. *P < 0.05 vs. control
I/R injury alters the expression profiles of genes involved in paracellular transport of Ca2+ and Mg2+ transport across the thick ascending limb of Henle and the proximal tubule
Next, we examined the renal expression of Ca2+ and Mg2+ transporters involved in passive, paracellular transport. I/R injury decreased the mRNA expression of Cldn2, Cldn10b, Cldn16, and Cldn19 (Fig. 7a), and increased the mRNA expression of Cldn14. Further, the expression levels of NKCC2 and of the Ca2+-sensing receptor (CaSR) were decreased in kidneys with I/R injury (Fig. 7b). We further found that the protein expression of Cldn16 and Cldn19 was decreased in kidneys with I/R injury (Fig. 7c, d).
mRNA expression profiles of genes involved in renal tubular paracellular transport of Ca2+ and Mg2+. Effect of renal I/R (18 h) on renal mRNA abundance of a Claudin (Cldn) 2, Cldn10b, Cldn14 Cldn16, and Cldn19 related to β-actin mRNA expression, b renal sodium-potassium-chloride cotransporter (NKCC2) and Ca2+-sensing receptor (Casr) mRNA expression related to β-actin mRNA expression, and c, d effect of renal I/R injury (18 h) on Cldn16 and Cldn19 protein expression related to β-actin protein expression. Inset shows representative immunoblot. Values are mean ± SEM for six animals. *P < 0.05 vs. control
Proinflammatory cytokines activation decrease Cldn16 and Cldn19 mRNA expression in vitro
To examine a possible regulatory effect of proinflammatory cytokines, we incubated primary DTCs and the MKTAL cell line with a combination of TNFα and IL-1β. Addition of the cytokine mixture decreased Cldn16 and Cldn19 mRNA expression in MKTAL cells (Fig. 8a). Incubation of primary DTCs with cytokines did not alter the expression of Mg2+ transporters (Fig. 8b). Further, the combination of TNFα with IL-1β did not alter the expression of Trpv5, Ncx1, and Pmca1b mRNA, but increased Trpv6 mRNA abundance (Fig. 8c).
Cytokines altered the expression of important renal transporters for magnesium and calcium transport in vitro. Effect of a cytokine mixture (Cyto-Mix; IL-1β and TNFα; each 100 ng/mL) on a claudin (Cldn) 16 and Cldn19 mRNA expression related to β-actin mRNA expression in a mouse kidney thick ascending limb cell line after 16 h, b on transient receptor potential melastatin (Trpm) 6, Trpm7, Na+-Mg2+-exchanger solute carrier family (Slc) 41a1, Slc41a3, and ancient conserved domain protein 2/cyclin M2 (Cnnm) 2 mRNA expression related to β-actin mRNA expression in primary distal tubule cells, and c on Trpv5, Trpv6, Ncx1, and Pmca1b mRNA expression related to β-actin mRNA expression in primary distal tubule cells. Values are mean ± SEM of four independent experiments. *P < 0.05 vs. control
Discussion
In the present study, we characterized the impact of I/R injury on systemic and local renal factors involved in renal Ca2+, Mg2+, and Pi homeostasis. Our data reveal that I/R injury-induced AKI deregulates electrolyte homeostasis in mice, which was paralleled by an increased or decreased expression of renal Ca2+, Mg2+, and Pi transporting proteins, respectively.
Renal I/R injury clearly induced clinical sings of AKI, as reflected by the increase in plasma urea and creatinine concentration, an elevated renal expression of the tubular injury markers NGAL and Kim-1 [56], and an altered renal morphology [30, 31]. Further, renal I/R injury clearly disturbed Pi homeostasis, a common hallmark observed in patients with AKI [28], as reflected by increased Pi blood levels despite an increased urinary excretion of Pi. A decrease in renal function is the most common cause for hyperphosphatemia [5, 20]. Therefore, the decline in GFR in response to I/R injury could likely account for the development of hyperphosphatemia [32]. In addition, I/R injury disturbed Mg2+ homeostasis, as reflected by hypermagnesemia and a decreased urinary Mg2+ excretion despite an increase in FE Mg2+. Because the kidneys play a central role in the control of Mg2+ homeostasis, the impairment of renal function could also be the cause for the increase in Mg2+ blood levels [20]. Taken together, the deterioration of renal function in response to I/R injury may likely account for the observed hyperphosphatemia and hypermagnesemia in our study. However, it should be noted that this study was not designed to specifically address the cause of I/R injury-induced hypermagnesemia and hyperphosphatemia.
Up to now, the functional importance of the FGF23-klotho-vitamin D axis in AKI is not well-defined [45]. It has been found, for example, that the rapid rise in FGF23 blood levels in response to folic acid-induced AKI is due to an increased expression of FGF23 in multiple organs including the bone, thymus, spleen, and heart [19]. The rapid increase in FGF23 blood levels is independent of the action of PTH and 1,25(OH)2D3 [10], two well-known stimulators for FGF23 production [33, 64]. Consistent with this finding, I/R injury was associated with increased FGF23 blood levels and unchanged levels of PTH and 1,25(OH)2D3. Therefore, other mechanisms and regulators of FGF23 are responsible for the observed increase in FGF23 blood levels in our study. Beside increased Pi blood levels [45], the observed increase in proinflammatory cytokines could likely account for the increase in FGF23 blood levels and renal tissue expression, as well as for the decrease in renal klotho expression in response to I/R injury [16, 26, 44, 49, 51]. Renal expression of FGF23 has been reported in animal models of acute and chronic kidney disease [19, 38, 59, 60, 67]. However, the intrarenal localization of FGF23 is still controversial. Zanchi et al., for example, found focal expression of FGF23 in both proximal and distal tubulus cells in a model of diabetic nephropathy [67]. In contrast, we did not clearly detect FGF23 mRNA in primary PT and DTCs. Therefore, our data rather support a more recent study, where FGF23 mRNA was found to be expressed exclusively in cells within the interstitial space [38]. Nevertheless, the observed increase in FGFR1 mRNA favors a possible paracrine signaling of renal-derived FGF23 in response to I/R injury. The observed downregulation of klotho, which may theoretically lead to FGF23 resistance and thus elevated FGF23 levels, may contribute to the FGF23 elevation in response to I/R injury [45]. However, our findings rather suggest that during the acute phase of I/R injury FGF23 resistance seems not to be of major relevance, because the inhibitory effect of FGF23 on the formation of 1,25(OH)2D3 via downregulation of Cyp27b1 expression and upregulation of Cyp24a1 expression was still present [58]. Confirming a human study in patients with AKI [68], but in contrast to other experimental models of AKI, like folic acid- or endotoxin-induced AKI, for example [16, 42], PTH levels were not altered in response to I/R injury in our study. Beside ionized blood Ca2+ levels, PTH secretion is also modulated by Pi, FGF23, and 1,25(OH)2D3 blood levels [35]. Therefore, the inhibitory effect of FGF23 on PTH release could likely account for unchanged PTH blood levels despite an increase in Pi blood levels. In addition, systemic administration of folic acid and/or endotoxin may elicit additional stimulatory effects on PTH secretion, like a fall in free plasma Ca2+ levels, which is the main physiological stimulus for PTH secretion [42]. Therefore, our data may also indicate that acute I/R injury-induced AKI does not cause hypocalcemia. Because FGF23 is filtered by the kidneys, a decrease in GFR could also contribute to increased blood levels of FGF23 in response to I/R injury. However, previous studies suggest that an increased formation rather than decreased excretion accounts for the increase in FGF23 levels in AKI [10].
Taken together, inflammatory stimuli, the decrease in renal kotho expression as well as the decline in renal function are likely responsible for high circulating FGF23 levels, which in turn may inhibit the formation and/or secretion of PTH and 1,25(OH)2D3.
To examine renal adaptive mechanisms of tubular electrolyte regulation in response to I/R injury, the renal expression of major Ca2+, Mg2+, and Pi transporters was investigated. In line with previous reports and with the phosphaturic effect of FGF23, renal I/R injury decreased the renal expression of NaPi-2a and NaPi-2c [22, 32], the principal renal type II sodium-dependent Pi transporters [63]. This downregulation occurred despite a decrease in renal klotho expression, and is likely mediated via activation of FGFR1 [22]. In contrast, NaPi-2b mRNA abundance was clearly increased in response to I/R injury. A low basal expression of NaPi-2b has been reported at the basolateral side of renal epithelial cells and administration of a high phosphate diet strongly increased the NaPi-2b expression. Therefore, it has been assumed that the increased expression of NaPi-2b may further increase tubular phosphate excretion [61]. In line with the observed regulation of NaPi-2 transporters, FE Pi and the urinary excretion of Pi were increased. The increase in PiT1 mRNA expression may be a compensatory mechanism [46], and argues against a global decrease in tubular apical membrane carriers and ion channels in response to I/R injury. However, because I/R injury is associated with renal tubular injury, we cannot completely exclude that the observed changes are also a result of cellular damage [30, 31].
The expression of the Ca2+ transporters Trpv5, the major apical Ca2+ channel in the late distal convoluted and connecting tubule for the initiation of transcellular Ca2+ reabsorption, and Trpv6 was elevated in response to I/R injury. Increased levels of FGF23 as well as proinflammatory cytokines may likely account for this induction [3, 27, 42, 51]. Despite the increase in Trpv5, the intracellular Ca2+ binding protein calbindin-D28K and the basolateral calcium extrusion proteins Pmca4 and Ncx1 were decreased in response to I/R injury, suggesting that the downregulation limits the overall tubular transport of Ca2+. The increase of Trpv5 and the downregulation of calbindin-D28K are peculiar as these two proteins are usually regulated in parallel. However, a very similar regulation has been recently reported for klotho-deficient mice, TRPV5 S682P mutant, adenine-fed mice, and endotoxemic mice [2, 37, 42, 51], suggesting that the decline of klotho and/or other unknown stimuli is involved in the different regulation of renal Ca2+ transport proteins. Further, our in vitro study indicates that proinflammatory cytokines directly increase Trpv6 expression, but have no effect on other Ca2+ transporters. Taken together, FGF23 as well as inflammatory cytokines may influence the expression of Ca2+ transporting proteins. It should be noted that this study was not designed to specifically address the cause of the different regulation of renal Ca2+ transporting proteins. The exact mechanism and signaling pathways have to be addressed in further studies.
The final urinary Mg2+ concentration is determined by an active, transcellular transport in the DCT. Although it has recently been found that the renal expression of Trpm6, the major apical Mg2+ channel in the early distal convoluted tubule for the initiation of transcellular Mg2+ reabsorption, is decreased in response to renal ischemia [17], Trpm6 was not altered in our study confirming a previous report [15]. The effect of I/R injury on the renal expression of Trpm7 is unclear, because increased as well as decreased or unaltered expression levels have been reported [15, 17, 36]. Increased Trpm7 expression has been associated with increased tissue damage [36, 40]. The reason for the variable effect of I/R injury on Trpm7 expression is unclear, but may be due to species differences and different ischemia periods, for example. Further, the intracellular Mg2+ binding protein parvalbumin and the putative basolateral Mg2+ extrusion proteins Cnnm2 and Slc41a3 were decreased in response to I/R injury, suggesting that the downregulation limits the overall tubular transport of Mg2+. Further, the transcellular Mg2+ transport process in the DCT is an electrogenic process [13]. Therefore, the well-described downregulation of the thiazide-sensitive sodium chloride cotransporter (NCC) in response to I/R injury may diminish the driving force for the entry of Mg2+ across the apical membrane, thereby inhibiting the absorption of Mg2+ in the DCT [24].
The observed increase in FE Ca2+ and FE Mg2+ fits with a reduced reuptake of Ca2+ and Mg2+. However, fractional excretion is a parameter that reflects whole tubular handling of Ca2+ and Mg2+, and the major portions of Ca2+ and Mg2+ are reabsorbed in the PT and in the thick ascending limb of Henle (TALH) by paracellular pathways. About 60–70% of the glomerular filtered Ca2+ is reabsorbed in the PT. Although the majority of PT Ca2+ reabsorption occurs via a passive paracellular process, driven by active solute and subsequent water reabsorption, a significant unknown transcellular transport of Ca2+ (~ 30% of the total reabsorption) contributes to PT Ca2+ reabsorption [1]. In contrast to Ca2+, only 10–20% of the filtered Mg2+ load is reabsorbed in the PT via a passive paracellular process [1]. Paracellular Ca2+ and Mg2+ reabsorption in the PT occurs likely via Cldn2, which depends on active, transcellular Na+ reabsorption, driven by the NHE3 and Na+/K+-ATPase. In the TALH, Ca2+ and Mg2+ reabsorption via Cldn16 and Cldn19 requires a lumen-positive transepithelial voltage gradient, which drives paracellular reabsorption of Ca2+ and Mg2+. The driving force for Ca2+ and Mg2+ reabsorption in the TALH is established by sodium absorption via NKCC2 and the activity of the Na+/K+-ATPase. Therefore, an impaired Na+ reabsorption due to decreased levels of NHE3, NKCC2, and Na+/K+-ATPase abundance has to be considered for the increase in FE Ca2+ and FE Mg2+ [24, 30, 32, 54]. Therefore, the I/R-induced downregulation of Cldn16 and Cldn19 in our study likely accounts for the increase in FE Ca2+ and FE Mg2+. The increase in Cldn14 mRNA expression, which blocks Ca2+ reabsorption in the TALH [14], may be a compensatory mechanism, and argues against a global decrease of transporters and channels in the TALH in response to I/R injury. In addition, it should be noted that deletion of Cldn10 rescues Cldn-16-deficient mice from hypomagnesemia and hypercalciuria [8]. Therefore, the decrease in Cldn10b may counteract the decreased passive reabsorption of Ca2+ and Mg2+ due to the decrease in Cldn16 in our study. Further, our in vitro study indicates that proinflammatory cytokines directly decrease Cldn16 and Cldn19 mRNA expression. In addition, an increased concentration of Mg2+ in the pro-urine due to a decreased proximal tubular reabsorption of Mg2+ could also be involved in the downregulation of Cldn16 expression [18]. Despite the increase in FE Ca2+ and FE Mg2+, total urinary excretion of Ca2+ and Mg2+ was decreased in response to I/R injury. It should be noted that FE and total excretion are integrated functions of the whole nephron together with GFR and renal blood flow. Therefore a decline in GFR and an altered renal perfusion, for example, should be taken into account for the observed changes in FE Ca2+ and FE Mg2+ and in the urinary excretion of Ca2+ and Mg2+.
In summary, we provide evidence that acute renal I/R injury is associated with hyperphosphatemia and hypermagnesemia. We found a disturbed FGF23-klotho-vitamin D axis leading to an increased or decreased expression of specific renal Ca2+, Mg2+, and Pi transporters, respectively (Fig. 9). Hormonal as well as inflammatory stimuli mediate this dysregulation via direct and indirect effects.
Simplified summarization of the effects of I/R injury on the renal expression of specific Ca2+, Mg2+, and Pi transporters investigated in this study. Proximal tubule (PT): Pi enters the cell at the apical side through type II sodium-dependent Pi co-transporters (NaPi-2) and type III sodium-dependent phosphate transporter (PiT). The precise renal localization and/or function of PiT1 and NaPi-2b is unknown. Ca2+ and Mg2+ are mainly reabsorbed paracellularly. Whether Cldn2 participates in PT Ca2+ and/or Mg2+ permeability is not entirely clear. Thick ascending limb of Henle (TALH): Ca2+ and Mg2+ are reabsorbed by controlled paracellular pathways involving claudin (Cldn) 16, Cldn19, and Cldn14. The driving force is initiated by sodium reabsorption via the sodium-potassium-chloride cotransporter (NKCC2 or Slc12a1). Activation of the basolateral Ca2+-sensing receptor (Casr) reduces NKCC2 activity and modulates paracellular Ca2+ permeability in response to increased interstitial Ca2+ concentrations. Distal convoluted tubule (DCT): Luminal Mg2+ uptake from the pro-urine is mediated by transient receptor potential channel melastatin (Trpm) 6/7 channels. Subsequently, Mg2+ binds to intracellular parvalbumin (Pvalb) and exits the cell at the basolateral side via the Na+-Mg2+-exchanger solute carrier family (Slc) 41a1 and the ancient conserved domain protein 2/cyclin M2 (Cnnm2). Mitochondria serve as intracellular Mg2+ stores. Intramitochondrial Mg2+ concentration is determined by Slc41a3. Ca2+ enters the cell at the apical side through transient receptor potential channel vanilloid (Trpv) 5/6 channels, subsequently binds to intracellular calbindin-D28K (CB28), and exits the cell at the basolateral side via the Na+/Ca2+-exchanger 1 (Ncx1) and the Ca2+ ATPases Pmca1b and Pmca4. Arrows indicate increased (↑), decreased (↓), or unaltered (↔) expression in response to I/R injury
References
Alexander RT, Dimke H (2017) Effect of diuretics on renal tubular transport of calcium and magnesium. Am J Physiol Renal Physiol 312:F998–F1015. https://doi.org/10.1152/ajprenal.00032.2017
Alexander RT, Woudenberg-Vrenken TE, Buurman J, Dijkman H, van der Eerden BC, van Leeuwen JP, Bindels RJ, Hoenderop JG (2009) Klotho prevents renal calcium loss. J Am Soc Nephrol 20:2371–2379. https://doi.org/10.1681/ASN.2008121273
Andrukhova O, Smorodchenko A, Egerbacher M, Streicher C, Zeitz U, Goetz R, Shalhoub V, Mohammadi M, Pohl EE, Lanske B, Erben RG (2014) FGF23 promotes renal calcium reabsorption through the TRPV5 channel. EMBO J 33:229–246. https://doi.org/10.1002/embj.201284188
Bikle DD (2014) Vitamin D metabolism, mechanism of action, and clinical applications. Chem Biol 21:319–329. https://doi.org/10.1016/j.chembiol.2013.12.016
Blaine J, Chonchol M, Levi M (2015) Renal control of calcium, phosphate, and magnesium homeostasis. Clin J Am Soc Nephrol 10:1257–1272. https://doi.org/10.2215/CJN.09750913
Bonventre JV, Yang L (2011) Cellular pathophysiology of ischemic acute kidney injury. J Clin Invest 121:4210–4221. https://doi.org/10.1172/JCI45161
Bourgeois S, Rossignol P, Grelac F, Chalumeau C, Klein C, Laghmani K, Chambrey R, Bruneval P, Duong JP, Poggioli J, Houillier P, Paillard M, Kellermann O, Froissart M (2003) Differentiated thick ascending limb (TAL) cultured cells derived from SV40 transgenic mice express functional apical NHE2 isoform: effect of nitric oxide. Pflugers Arch 446:672–683. https://doi.org/10.1007/s00424-003-1108-x
Breiderhoff T, Himmerkus N, Drewell H, Plain A, Gunzel D, Mutig K, Willnow TE, Muller D, Bleich M (2018) Deletion of claudin-10 rescues claudin-16-deficient mice from hypomagnesemia and hypercalciuria. Kidney Int 93:580–588. https://doi.org/10.1016/j.kint.2017.08.029
Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW (2005) Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol 16:3365–3370. https://doi.org/10.1681/ASN.2004090740
Christov M, Waikar SS, Pereira RC, Havasi A, Leaf DE, Goltzman D, Pajevic PD, Wolf M, Juppner H (2013) Plasma FGF23 levels increase rapidly after acute kidney injury. Kidney Int 84:776–785. https://doi.org/10.1038/ki.2013.150
Claure-Del Granado R, Bouchard J (2012) Acid-base and electrolyte abnormalities during renal support for acute kidney injury: recognition and management. Blood Purif 34:186–193. https://doi.org/10.1159/000341723
David V, Martin A, Isakova T, Spaulding C, Qi L, Ramirez V, Zumbrennen-Bullough KB, Sun CC, Lin HY, Babitt JL, Wolf M (2016) Inflammation and functional iron deficiency regulate fibroblast growth factor 23 production. Kidney Int 89:135–146. https://doi.org/10.1038/ki.2015.290
de Baaij JH (2015) The art of magnesium transport. Magnes Res 28:85–91. https://doi.org/10.1684/mrh.2015.0388
Dimke H, Desai P, Borovac J, Lau A, Pan W, Alexander RT (2013) Activation of the Ca(2+)-sensing receptor increases renal claudin-14 expression and urinary Ca(2+) excretion. Am J Physiol Renal Physiol 304:F761–F769. https://doi.org/10.1152/ajprenal.00263.2012
Dokuyucu R, Gogebakan B, Yumrutas O, Bozgeyik I, Gokce H, Demir T (2014) Expressions of TRPM6 and TRPM7 and histopathological evaluation of tissues in ischemia reperfusion performed rats. Ren Fail 36:932–936. https://doi.org/10.3109/0886022X.2014.900405
Durlacher-Betzer K, Hassan A, Levi R, Axelrod J, Silver J, Naveh-Many T (2018) Interleukin-6 contributes to the increase in fibroblast growth factor 23 expression in acute and chronic kidney disease. Kidney Int 94:315–325. https://doi.org/10.1016/j.kint.2018.02.026
Dusmez D, Cengiz B, Yumrutas O, Demir T, Oztuzcu S, Demiryurek S, Tutar E, Bayraktar R, Bulut A, Simsek H, Dagli SN, Kilic T, Bagci C (2014) Effect of verapamil and lidocaine on TRPM and NaV1.9 gene expressions in renal ischemia-reperfusion. Transplant Proc 46:33–39. https://doi.org/10.1016/j.transproceed.2013.10.036
Efrati E, Hirsch A, Kladnitsky O, Rozenfeld J, Kaplan M, Zinder O, Zelikovic I (2010) Transcriptional regulation of the claudin-16 gene by Mg2+ availability. Cell Physiol Biochem 25:705–714. https://doi.org/10.1159/000315090
Egli-Spichtig D, Zhang MYH, Perwad F (2018) Fibroblast growth factor 23 expression is increased in multiple organs in mice with folic acid-induced acute kidney injury. Front Physiol 9:1494. https://doi.org/10.3389/fphys.2018.01494
Elin RJ (1988) Magnesium metabolism in health and disease. Dis Mon 34:161–218
Erben RG (2018) Physiological actions of fibroblast growth factor-23. Front Endocrinol (Lausanne) 9:267. https://doi.org/10.3389/fendo.2018.00267
Gattineni J, Bates C, Twombley K, Dwarakanath V, Robinson ML, Goetz R, Mohammadi M, Baum M (2009) FGF23 decreases renal NaPi-2a and NaPi-2c expression and induces hypophosphatemia in vivo predominantly via FGF receptor 1. Am J Physiol Renal Physiol 297:F282–F291. https://doi.org/10.1152/ajprenal.90742.2008
Goncalves JG, de Braganca AC, Canale D, Shimizu MH, Sanches TR, Moyses RM, Andrade L, Seguro AC, Volpini RA (2014) Vitamin D deficiency aggravates chronic kidney disease progression after ischemic acute kidney injury. PLoS One 9:e107228. https://doi.org/10.1371/journal.pone.0107228
Gong H, Wang W, Kwon TH, Jonassen T, Li C, Ring T, Froki AJ, Nielsen S (2004) EPO and alpha-MSH prevent ischemia/reperfusion-induced down-regulation of AQPs and sodium transporters in rat kidney. Kidney Int 66:683–695. https://doi.org/10.1111/j.1523-1755.2004.00791.x
Hocherl K, Schmidt C, Kurt B, Bucher M (2010) Inhibition of NF-kappaB ameliorates sepsis-induced downregulation of aquaporin-2/V2 receptor expression and acute renal failure in vivo. Am J Physiol Renal Physiol 298:F196–F204. https://doi.org/10.1152/ajprenal.90607.2008
Hu MC, Shi M, Zhang J, Quinones H, Kuro-o M, Moe OW (2010) Klotho deficiency is an early biomarker of renal ischemia-reperfusion injury and its replacement is protective. Kidney Int 78:1240–1251. https://doi.org/10.1038/ki.2010.328
Ikeda S, Yamamoto H, Masuda M, Takei Y, Nakahashi O, Kozai M, Tanaka S, Nakao M, Taketani Y, Segawa H, Iwano M, Miyamoto K, Takeda E (2014) Downregulation of renal type IIa sodium-dependent phosphate cotransporter during lipopolysaccharide-induced acute inflammation. Am J Physiol Renal Physiol 306:F744–F750. https://doi.org/10.1152/ajprenal.00474.2013
Jung SY, Kwon J, Park S, Jhee JH, Yun HR, Kim H, Kee YK, Yoon CY, Chang TI, Kang EW, Park JT, Yoo TH, Kang SW, Han SH (2018) Phosphate is a potential biomarker of disease severity and predicts adverse outcomes in acute kidney injury patients undergoing continuous renal replacement therapy. PLoS One 13:e0191290. https://doi.org/10.1371/journal.pone.0191290
Kempson SA, Lotscher M, Kaissling B, Biber J, Murer H, Levi M (1995) Parathyroid hormone action on phosphate transporter mRNA and protein in rat renal proximal tubules. Am J Phys 268:F784–F791. https://doi.org/10.1152/ajprenal.1995.268.4.F784
Kristensen ML, Kierulf-Lassen C, Nielsen PM, Krag S, Birn H, Nejsum LN, Norregaard R (2016) Remote ischemic perconditioning attenuates ischemia/reperfusion-induced downregulation of AQP2 in rat kidney. Physiol Rep 4:e12865. https://doi.org/10.14814/phy2.12865
Kumar S, Allen DA, Kieswich JE, Patel NS, Harwood S, Mazzon E, Cuzzocrea S, Raftery MJ, Thiemermann C, Yaqoob MM (2009) Dexamethasone ameliorates renal ischemia-reperfusion injury. J Am Soc Nephrol 20:2412–2425. https://doi.org/10.1681/ASN.2008080868
Kwon TH, Frokiaer J, Han JS, Knepper MA, Nielsen S (2000) Decreased abundance of major Na(+) transporters in kidneys of rats with ischemia-induced acute renal failure. Am J Physiol Renal Physiol 278:F925–F939. https://doi.org/10.1152/ajprenal.2000.278.6.F925
Lavi-Moshayoff V, Wasserman G, Meir T, Silver J, Naveh-Many T (2010) PTH increases FGF23 gene expression and mediates the high-FGF23 levels of experimental kidney failure: a bone parathyroid feedback loop. Am J Physiol Renal Physiol 299:F882–F889. https://doi.org/10.1152/ajprenal.00360.2010
Leaf DE, Wolf M, Stern L (2010) Elevated FGF-23 in a patient with rhabdomyolysis-induced acute kidney injury. Nephrol Dial Transplant 25:1335–1337. https://doi.org/10.1093/ndt/gfp682
Lederer E (2014) Regulation of serum phosphate. J Physiol 592:3985–3995. https://doi.org/10.1113/jphysiol.2014.273979
Liu A, Wu J, Yang C, Wu Y, Zhang Y, Zhao F, Wang H, Yuan L, Song L, Zhu T, Fan Y, Yang B (2018) TRPM7 in CHBP-induced renoprotection upon ischemia reperfusion-related injury. Sci Rep 8:5510. https://doi.org/10.1038/s41598-018-22852-2
Loh NY, Bentley L, Dimke H, Verkaart S, Tammaro P, Gorvin CM, Stechman MJ, Ahmad BN, Hannan FM, Piret SE, Evans H, Bellantuono I, Hough TA, Fraser WD, Hoenderop JG, Ashcroft FM, Brown SD, Bindels RJ, Cox RD, Thakker RV (2013) Autosomal dominant hypercalciuria in a mouse model due to a mutation of the epithelial calcium channel, TRPV5. PLoS One 8:e55412. https://doi.org/10.1371/journal.pone.0055412
Mace ML, Gravesen E, Nordholm A, Hofman-Bang J, Secher T, Olgaard K, Lewin E (2017) Kidney fibroblast growth factor 23 does not contribute to elevation of its circulating levels in uremia. Kidney Int 92:165–178. https://doi.org/10.1016/j.kint.2017.01.015
Matzdorf C, Kurtz A, Hocherl K (2007) COX-2 activity determines the level of renin expression but is dispensable for acute upregulation of renin expression in rat kidneys. Am J Physiol Renal Physiol 292:F1782–F1790. https://doi.org/10.1152/ajprenal.00513.2006
Meng Z, Wang X, Yang Z, Xiang F (2012) Expression of transient receptor potential melastatin 7 up-regulated in the early stage of renal ischemia-reperfusion. Transplant Proc 44:1206–1210. https://doi.org/10.1016/j.transproceed.2011.11.068
Meurer M, Ebert K, Schweda F, Hocherl K (2018) The renal vasodilatory effect of prostaglandins is ameliorated in isolated-perfused kidneys of endotoxemic mice. Pflugers Arch 470:1691–1703. https://doi.org/10.1007/s00424-018-2183-3
Meurer M, Hocherl K (2019) Endotoxaemia differentially regulates the expression of renal Ca(2+) transport proteins in mice. Acta Physiol (Oxf) 225:e13175. https://doi.org/10.1111/apha.13175
Moor MB, Bonny O (2016) Ways of calcium reabsorption in the kidney. Am J Physiol Renal Physiol 310:F1337–F1350. https://doi.org/10.1152/ajprenal.00273.2015
Moreno JA, Izquierdo MC, Sanchez-Nino MD, Suarez-Alvarez B, Lopez-Larrea C, Jakubowski A, Blanco J, Ramirez R, Selgas R, Ruiz-Ortega M, Egido J, Ortiz A, Sanz AB (2011) The inflammatory cytokines TWEAK and TNFalpha reduce renal klotho expression through NFkappaB. J Am Soc Nephrol 22:1315–1325. https://doi.org/10.1681/ASN.2010101073
Neyra JA, Moe OW, Hu MC (2015) Fibroblast growth factor 23 and acute kidney injury. Pediatr Nephrol 30:1909–1918. https://doi.org/10.1007/s00467-014-3006-1
Nowik M, Picard N, Stange G, Capuano P, Tenenhouse HS, Biber J, Murer H, Wagner CA (2008) Renal phosphaturia during metabolic acidosis revisited: molecular mechanisms for decreased renal phosphate reabsorption. Pflugers Arch 457:539–549. https://doi.org/10.1007/s00424-008-0530-5
Olauson H, Lindberg K, Amin R, Jia T, Wernerson A, Andersson G, Larsson TE (2012) Targeted deletion of klotho in kidney distal tubule disrupts mineral metabolism. J Am Soc Nephrol 23:1641–1651. https://doi.org/10.1681/ASN.2012010048
Olauson H, Vervloet MG, Cozzolino M, Massy ZA, Urena Torres P, Larsson TE (2014) New insights into the FGF23-klotho axis. Semin Nephrol 34:586–597. https://doi.org/10.1016/j.semnephrol.2014.09.005
Onal M, Carlson AH, Thostenson JD, Benkusky NA, Meyer MB, Lee SM, Pike JW (2018) A novel distal enhancer mediates inflammation-, PTH-, and early onset murine kidney disease-induced expression of the mouse Fgf23 gene. JBMR Plus 2:32–47. https://doi.org/10.1002/jbm4.10023
Perwad F, Azam N, Zhang MY, Yamashita T, Tenenhouse HS, Portale AA (2005) Dietary and serum phosphorus regulate fibroblast growth factor 23 expression and 1,25-dihydroxyvitamin D metabolism in mice. Endocrinology 146:5358–5364. https://doi.org/10.1210/en.2005-0777
Pulskens WP, Verkaik M, Sheedfar F, van Loon EP, van de Sluis B, Vervloet MG, Hoenderop JG, Bindels RJ, Consortium N (2015) Deregulated renal calcium and phosphate transport during experimental kidney failure. PLoS One 10:e0142510. https://doi.org/10.1371/journal.pone.0142510
Radhakrishnan VM, Ramalingam R, Larmonier CB, Thurston RD, Laubitz D, Midura-Kiela MT, McFadden RM, Kuro OM, Kiela PR, Ghishan FK (2013) Post-translational loss of renal TRPV5 calcium channel expression, Ca(2+) wasting, and bone loss in experimental colitis. Gastroenterology 145:613–624. https://doi.org/10.1053/j.gastro.2013.06.002
Rodriguez-Ortiz ME, Rodriguez M (2015) FGF23 as a calciotropic hormone. F1000Res 4. https://doi.org/10.12688/f1000research.7189.1
Schmidt C, Hocherl K, Schweda F, Kurtz A, Bucher M (2007) Regulation of renal sodium transporters during severe inflammation. J Am Soc Nephrol 18:1072–1083. https://doi.org/10.1681/ASN.2006050454
Schreiber A, Theilig F, Schweda F, Hocherl K (2012) Acute endotoxemia in mice induces downregulation of megalin and cubilin in the kidney. Kidney Int 82:53–59. https://doi.org/10.1038/ki.2012.62
Schrezenmeier EV, Barasch J, Budde K, Westhoff T, Schmidt-Ott KM (2017) Biomarkers in acute kidney injury—pathophysiological basis and clinical performance. Acta Physiol (Oxf) 219:554–572. https://doi.org/10.1111/apha.12764
Seo MY, Yang J, Lee JY, Kim K, Kim SC, Chang H, Won NH, Kim MG, Jo SK, Cho W, Kim HK (2015) Renal klotho expression in patients with acute kidney injury is associated with the severity of the injury. Korean J Intern Med 30:489–495. https://doi.org/10.3904/kjim.2015.30.4.489
Shimada T, Hasegawa H, Yamazaki Y, Muto T, Hino R, Takeuchi Y, Fujita T, Nakahara K, Fukumoto S, Yamashita T (2004) FGF-23 is a potent regulator of vitamin D metabolism and phosphate homeostasis. J Bone Miner Res 19:429–435. https://doi.org/10.1359/JBMR.0301264
Smith ER, Tan SJ, Holt SG, Hewitson TD (2017) FGF23 is synthesised locally by renal tubules and activates injury-primed fibroblasts. Sci Rep 7:3345. https://doi.org/10.1038/s41598-017-02709-w
Spichtig D, Zhang H, Mohebbi N, Pavik I, Petzold K, Stange G, Saleh L, Edenhofer I, Segerer S, Biber J, Jaeger P, Serra AL, Wagner CA (2014) Renal expression of FGF23 and peripheral resistance to elevated FGF23 in rodent models of polycystic kidney disease. Kidney Int 85:1340–1350. https://doi.org/10.1038/ki.2013.526
Suyama T, Okada S, Ishijima T, Iida K, Abe K, Nakai Y (2012) High phosphorus diet-induced changes in NaPi-IIb phosphate transporter expression in the rat kidney: DNA microarray analysis. PLoS One 7:e29483. https://doi.org/10.1371/journal.pone.0029483
Vallon V (2016) Tubular transport in acute kidney injury: relevance for diagnosis, prognosis and intervention. Nephron 134:160–166. https://doi.org/10.1159/000446448
Wagner CA, Rubio-Aliaga I, Biber J, Hernando N (2014) Genetic diseases of renal phosphate handling. Nephrol Dial Transplant 29(Suppl 4):iv45–iv54. https://doi.org/10.1093/ndt/gfu217
Wesseling-Perry K, Pereira RC, Sahney S, Gales B, Wang HJ, Elashoff R, Juppner H, Salusky IB (2011) Calcitriol and doxercalciferol are equivalent in controlling bone turnover, suppressing parathyroid hormone, and increasing fibroblast growth factor-23 in secondary hyperparathyroidism. Kidney Int 79:112–119. https://doi.org/10.1038/ki.2010.352
Yang SS, Hsu YJ, Chiga M, Rai T, Sasaki S, Uchida S, Lin SH (2010) Mechanisms for hypercalciuria in pseudohypoaldosteronism type II-causing WNK4 knock-in mice. Endocrinology 151:1829–1836. https://doi.org/10.1210/en.2009-0951
Zager RA (2014) Progression from acute kidney injury to chronic kidney disease: clinical and experimental insights and queries. Nephron Clin Pract 127:46–50. https://doi.org/10.1159/000363726
Zanchi C, Locatelli M, Benigni A, Corna D, Tomasoni S, Rottoli D, Gaspari F, Remuzzi G, Zoja C (2013) Renal expression of FGF23 in progressive renal disease of diabetes and the effect of ACE inhibitor. PLoS One 8:e70775. https://doi.org/10.1371/journal.pone.0070775
Zhang M, Hsu R, Hsu CY, Kordesch K, Nicasio E, Cortez A, McAlpine I, Brady S, Zhuo H, Kangelaris KN, Stein J, Calfee CS, Liu KD (2011) FGF-23 and PTH levels in patients with acute kidney injury: a cross-sectional case series study. Ann Intensive Care 1:21. https://doi.org/10.1186/2110-5820-1-21
Acknowledgements
The technical assistance provided by Ramona Mogge and Andrea Agli is gratefully acknowledged.
Funding
This study was supported by a grant from the Deutsche Forschungsgemeinschaft (DFG, SFB699/B5).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All animal experiments were conducted according to the National Institutes of Health Guide for the Care and Use of Laboratory Animals and were approved by the local animal protection committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Organ Physiology
Rights and permissions
About this article
Cite this article
Meurer, M., Höcherl, K. Renal ischemia-reperfusion injury impairs renal calcium, magnesium, and phosphate handling in mice. Pflugers Arch - Eur J Physiol 471, 901–914 (2019). https://doi.org/10.1007/s00424-019-02255-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-019-02255-6