Abstract
Given that most malignant tumors are derived from epithelium, developing a strategy for treatment of epithelium-derived cancers (i.e., carcinomas) is a pivotal issue in cancer therapy. Carcinomas, including ovarian, breast, prostate, and pancreatic cancers, are known to overexpress various claudins (CLDNs); in particular, CLDN-3 and -4 are frequently overexpressed in malignant case. The generation of CLDN binders is a key for expanding CLDN-targeted cancer therapy but has been delayed due to the small size of CLDN extracellular domains (approximately 50 amino acids for the first domain and 15 amino acids for the second) and their high homology among species. Interestingly, however, the receptors for Clostridium perfringens enterotoxin (CPE), a foodborne toxin in humans, happen to be identical to CLDN-3 and -4. Thus, the first CLDN binder, CPE, has provided us CLDN-targeted cancer therapy from a concept into a potential reality. In this review, we describe roles of CPE technology in cancer therapy and discuss future directions in the CLDN-targeting concept-to-therapy process.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The tight junction (TJ) is critical for the epithelial barrier protecting our cells, organs, and body systems from pathogens and other harmful agents [23]. These structures reside in the most apical region of the lateral membranes, where they function as both gates and fences. As gates, TJs create selective barriers between tissue spaces. As fences, TJs inhibit the diffusion of lipids and membrane proteins between the apical and basolateral membrane domains, thus maintaining cell polarity. However, epithelial carcinogenesis often introduces aberrations into the proteins that form the TJs, consequently disrupting their gate and fence functions [64]. Thus, TJ proteins are attractive candidate targets for cancer therapy [48].
One group of proteins that is integral to TJs and to their gate and fence functions are the claudins (CLDNs) [19]. Each of the 27 mammalian members of the CLDN family is a tetra-transmembrane protein that contains 2 extracellular loop domains and N- and C-terminal intracellular domains [55]. The expression pattern of CLDNs differs among tissues [23]. A series of gene and histological analysis has revealed that abnormal expression patterns of CLDNs are observed in many cancers (Table 1). These findings indicate that CLDN binders might be potent therapeutic and diagnostic molecules for cancer therapy.
Clostridium perfringens enterotoxin (CPE) is responsible for the diarrhea and abdominal cramps of C. perfringens type A food poisoning, which is the second most common foodborne illness in the USA [21]. The receptors for CPE were identified in 1997—before the “discovery” of CLDNs—and, in 1999, the CPE receptors were found to be identical to CLDN-3 and -4 [18, 31, 32, 58]. Thus, by being identified as the first CLDN binder, CPE became an important nexus between the concept of CLDN-targeted cancer therapy and, through its application as a model for drug discovery, the reality of this treatment modality. In this review, we overview the journey to CLDN-targeted cancer therapy with CPE technology.
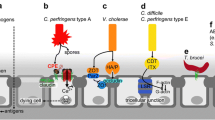
CPE and its receptor-binding domain
The CPE protein comprises 319 amino acids and has two domains: the N-terminal cytotoxic domain, which is involved in oligomerization and pore formation, and the C-terminal receptor-binding domain (Fig. 1a, b) [35]. To elicit the high cytotoxic activity of the N-terminal domain requires digestion of the extreme N-terminal residues by intestinal protease [36]. The CPE oligomerization domain corresponds to amino acids 45–53, and residues 80–106 are responsible for the insertion of CPE into the membrane and for pore formation [10, 36]. The C-terminal fragment of CPE (corresponding to amino acids 184–319) is the receptor-binding domain [31, 32]. CLDN-3 and -4 were the first recognized CPE receptors, with the second extracellular loop domain considered to be the CPE receptor domain [17, 79]. CPE typically binds to CLDNs that are “free” on the cell surface and only infrequently binds to CLDNs that are incorporated into TJs [42, 94]. After interacting with CLDNs, CPE first becomes a small (∼90 kDa) complex consisting of CPE and a cell surface CLDN, followed by oligomerization of six of these small complexes into a large (∼450 kDa) complex. This large complex forms a permeable pore, causing a robust influx of Ca2+, and the subsequent disruption of the cellular osmotic equilibrium and activation of Ca2+-dependent protease cause rapid cell lysis (Fig. 2) [9]. In this context, CPE is the first CLDN-targeted cytotoxic molecule. Numerous binding studies have revealed that CPE strongly binds to CLDN-3, -4, -6, -7, and -9 and weakly binds to CLDN-8, -14, and -19 [17, 71, 94].
Structure of Clostridium perfringens enterotoxin (CPE). a Structure of CPE (PDB code, 3AM2) by X-ray crystallography. The N-terminal domain is shown in green, and the C-terminal domain is turquoise. Regions involved in oligomerization (red), pore formation (pink), and claudin binding (navy) are indicated. b Schematic diagram of the roles of the CPE domains. Amino acids shown in blue are particularly important for claudin binding
CPE-mediated cytolysis. This schematic diagram illustrates the mechanism underlying CPE-mediated cytolysis. In brief, CPE binds to CLDNs to form a hexameric complex in the membrane. This complex creates a pore through which Ca2+ enters the cell. The rapid influx of Ca2+ triggers Ca2+-dependent protease, leading to necrosis
Recombinant C-terminal fragments of CPE (C-CPE), corresponding to amino acids 184–319 or 194–319, bind to CLDNs [79, 89, 91]. Treatment of epithelial cell sheets with C-CPE disrupts the intercellular seal function of TJs without inducing cytotoxicity [39, 85, 89]. Functional domain-mapping studies indicate that the minimal CLDN-binding domain comprises amino acids 290–319 in the C-terminus and that Y306, Y310, Y312, and L315 are critical for the interaction of C-CPE with CLDN-4 [24, 84].
The role of CPE for cancer therapy
Ovarian cancers have been studied most frequently as targets for CPE and its derivatives. A large-scale serial analysis of gene expression revealed that CLDN-3 and -4 are overexpressed (83- and 109-fold, respectively) in several cases of ovarian cancers compared with normal epithelium [29]. In addition, DNA microarray analysis has shown that CLDN-3 and -4 are two of the top five differentially expressed genes in ovarian cancers [75]. CLDN-6 and -7 are also overexpressed in ovarian cancers [13, 87]. This means that the expression of several CPE-sensitive CLDNs (that is, those that strongly bind CPE) is frequently increased in ovarian cancers [74]. Moreover, the expression levels of CLDN-3 and -4 were higher in chemotherapy-resistant or recurrent ovarian cancers than in chemotherapy-sensitive ovarian cancers [74, 95]. Intraperitoneal injection of CPE into intraperitoneal mouse xenografts models of chemotherapeutic-resistant primary ovarian cancer cells attenuated tumor growth without apparent side effects [8, 74].
In studies comparing primary breast carcinoma and normal mammary epithelial tissues, CLDN-3 and -4 were overexpressed in 62 and 26 % of breast cancers, respectively, and CLDN-7 gene expression was increased in breast cancers [38, 60]. Furthermore, CPE has been shown to be cytotoxic in freshly resected samples of breast cancer tissue [38]. However, 5–10 % of breast cancers comprise a “CLDN-low” subtype that shows decreased expression of CLDN-3, -4, and -7 [25].
Among the CLDNs, both CLDN-3 and -4 are strongly expressed in prostate cancers [51, 82]. In particular, a cDNA microarray analysis of prostate cancer cell lines and normal prostate cell lines showed that CLDN-4 mRNA has the greatest upregulation among 51 upregulated genes in prostate cancer cells, and an immunohistologic study indicated that CLDN-4 is highly expressed in primary prostate cancers and at the secondary sites of metastatic prostate cancers and is moderately expressed in benign prostatic hyperplasia [43]. Although intratumoral injection of CPE inhibited tumor growth in mice bearing PC-3 prostate cancer cells, the possibility of side effects of this treatment scheme should be considered, given that CLDN-3 is strongly expressed in normal prostate tissues [51, 52].
A Northern blot analysis demonstrated frequent high CLDN-4 expression in pancreatic cancer tissues, whereas CLDN-4 expression was low or absent in normal pancreatic tissue [54]. In addition, immunohistologic analysis using tissue samples from patients with pancreatic cancers revealed that expression of CLDN-4 was increased in primary and metastatic pancreatic cancer cells compared with normal pancreatic duct epithelial cells [63]. Intratumoral injection of CPE in mice carrying Panc-1 xenografts (pancreatic cancer cells) completely inhibited tumor growth and induced widespread tumor necrosis without causing any adverse effects [54].
One of the hurdles to the clinical application of human induced pluripotent stem cells for regenerative medicine is the risk of teratoma formation from contaminating undifferentiated cells [46]. In this context, CLDN-6 has been shown to be present in pluripotent-undifferentiated cells and germ cell tumors but not in differentiated cells [3, 90]. Although transplantation of a mixture of undifferentiated and differentiated cells into mice led to teratoma formation, treatment of the cell mixture with CPE prior to transplantation prevented this consequence [3]. Of note, CLDN-6-deficient mice showed a normal phenotype, indicating that CLDN-6 is dispensable for the self-renewal and survival of pluripotent cells [1].
The role of C-CPE as an adjunct to chemotherapy
An increasing tumor mass causes an increase in tumor interstitial fluid pressure and thus hampers the uptake and penetration of anti-tumor drugs [2]. This situation prompted the search for a strategy to increase the tissue penetration of anti-tumor drugs by opening epithelial junctions, given that intercellular junctions, including TJs, are not fully compromised in cancer cells [53]. C-CPE can be used as such an enhancer of anti-tumor drug penetration (Fig. 3a) [37]. In particular, C-CPE induced morphologic changes in ovarian cancer cells (causing them to become spheroids) and repeated combined intraperitoneal administration of paclitaxel and C-CPE that yielded significant synergic anti-tumor effects in mice implanted with subcutaneous tumors [20]. Another molecule, a categorized enhancer of anti-tumor drug penetration, increased the therapeutic efficacy of paclitaxel, protein-bound paclitaxel, doxorubicin, and a monoclonal antibody [4, 5].
The biological roles of CLDNs in cancer cells are still not fully understood, but several reports suggest that the suppression of CLDNs in cancer cells increased their sensitivity to anti-tumor drugs. Knockdown of CLDN-4 in ovarian cancer cells enhanced the cellular uptake of cisplatin and thus their sensitivity to this drug [95]. Samples of ovarian cancer tissue resected from cisplatin-resistant patients consistently showed significantly higher CLDN-4 expression than did those resected from cisplatin-sensitive patients [95]. CLDNs recruit various membrane proteins to the plasma membrane and regulate others at the gene-expression level, suggesting that the loss of CLDN-4 might affect the recruitment or expression of a drug influx or efflux transporter [41, 83, 97]. Moreover, knockdown of CLDN-7 in pancreatic cancer cells increased their cisplatin sensitivity by reducing the expression of anti-apoptotic proteins [88]. Because C-CPE treatment causes the degradation of CLDN-4 proteins, C-CPE might enhance the sensitivity to anti-tumor drugs by increasing their cellular uptake (Fig. 3b) [79]. In an example of an alternative mechanism, CLDN-4 associates with the cisplatin influx transporter CTR1 and knockdown of CLDN-4 in ovarian cancer cells hampered the internalization of cisplatin by reducing CTR1 mRNA [76]. The cell type-specific biological functions of CLDNs should be considered for the utility of CLDN binders as adjunct therapeutics.
The role of C-CPE in cancer diagnosis
CLDNs are targets not only for cancer therapeutics but also for cancer diagnosis. C-CPE is a non-toxic CLDN binder, and concepts for CLDN-targeted cancer diagnosis have been proven by using C-CPE (Fig. 3c).
Intravenous injection of fluorescent dye-conjugated C-CPE into mice intraperitoneally grafted with OSPC-ARK-1 cells (intraperitoneal metastatic ovarian cancer cells) detected tumor tissues as small as 1 mm2 in area, which went undetected by conventional visual observation [12]. C-CPE-mediated detection of peritoneal micrometastases and CPE-mediated cytolysis have been useful in the treatment of uterine serous cancers, which are gynecologic cancers showing high expression of CLDN-3 and -4 [12, 73].
SPECT imaging using 111In-conjugated glutathione S-transferase–C-CPE showed significantly increased accumulation of the radioactive tracer in the tumor tissues of MDA-MB-468 xenografts (CLDN-4-positive breast cancer cells) compared with CLDN-4-negative xenografts [59]. This SPECT imaging technique also detected aplastic lesions in genetically engineered mice that spontaneously developed breast cancer (Balb/neuT mouse). As another example, the accumulation of fluorescein-conjugated C-CPE was greater in Capan-1 xenografts (CLDN-4-positive pancreatic cancer cells) than in CLDN-4 negative xenografts [62]. In addition, the C-CPE conjugate accumulated more strongly in spontaneously developed pancreatic intraepithelial neoplasms than in normal pancreatic tissues [62]. Together, these findings suggest a potential application of C-CPE in the detection of precursor lesions in some cancers.
Safety evaluation of CPE and C-CPE
Because CLDN-3 and -4 are expressed in normal tissues, including lung, thyroid, liver, kidney, and intestines, damage to these tissues is inevitable once CPE or C-CPE-conjugated drugs are applied. C-CPE was distributed in thyroid, liver, kidney, and intestines after intravenous injection [49]. For instance, a single intraperitoneal injection of CPE in excess of 0.75 mg/kg was lethal to mice [93]. Similarly, a single intravenous injection of more than 10 μg/kg of C-CPE conjugated with protein synthesis inhibitory factor, which is the exotoxin derived from Pseudomonas aeruginosa, induced hepatic injury and loss of body weight in mice [49]. The high systemic toxicity of CPE limits the administration route and dose of CPE and C-CPE-conjugated drugs. Indeed, CPE injected directly into xenografted tumors or into the peritoneal cavity of mice with peritoneal metastatic cancer inhibited tumor growth in the absence of systemic effects [8, 52, 54, 74]. To reduce the systemic cytotoxicity of CPE and its derivative, one group designed a CPE-based protoxin [69]. The protoxin comprised two domains: CPE and the CPE-binding motif derived from the second extracellular domain of CLDN-3. The two domains were connected by flexible linker that contained a cleavage site for prostate-specific antigen (PSA). PSA is an enzyme secreted from prostate cancer cells and is activated in tumor microenvironments because serum protease inhibitors bind to (and thus inactivate) PSA in the systemic circulation [15]. This CPE-based protoxin was cytotoxic to cells that expressed both CLDN-3 and -4, and PSA yet showed reduced adverse effects.
Because CPE is a bacterial protein, it induces an immune response. This immunogenicity limits the clinical application of native CPE and its derivatives because the resulting antibody response may complicate the prediction of their pharmacokinetic–pharmacodynamic profiles and because the immunogenic compounds might induce complement- or IgE-mediated hypersensitivity [44]. A previous domain-mapping analysis of CPE revealed amino acids 16–65, 91–170, and 286–305 as antigenic epitopes, but the minimal CLDN-binding domain of CPE (amino acids 290–319) is considered to have low antigenicity [80]. Subsequent conjugation of this 30 amino acid peptide with tumor necrosis factor alpha increased its CLDN-targeting ability and its specific cytotoxicity against cells that express CLDN-3 and -4 [96]. In another study, screening of a phage display library yielded two CLDN-4-binding 12 residue peptides whose amino-acid motifs were similar to the minimal binding domain of C-CPE [50]. Future efforts focused on minimizing the CLDN-binding domain of CPE might overcome its antigenicity.
The role of C-CPE as a template for creating new CLDN binders
Native CPE binds to a broad range of CLDNs, leading to a risk of systemic toxicity. Consequently, a CLDN-4-specific CPE derivative might lack hepatotoxic effects, because CLDN-4 is not expressed in liver [51]. Similarly a CLDN-6-specific CPE mutant might accumulate preferentially in tumor tissues because normal differentiated cells do not express CLDN-6 [3]. To generate new C-CPE derivatives with narrow CLDN-specificity, several groups have applied a mutagenesis approach; the resulting CPE mutants N309A/S313A, L254A/S256A/I258A/D284A, L223A/D225A/R227A, and Y306W/S313H showed high affinity for CLDN-4 and high specificity for CLDN-4, -3, and -5, respectively [66, 86, 92]. In addition, recent findings regarding the structure of mouse CLDN-15 (Protein Data Bank [PDB] code, 4P79) and of the mouse CLDN-19–C-CPE complex (PDB code, 3X29) indicate that C-CPE actually binds to both the first and second extracellular domains of CLDNs and not solely to the second extracellular domain of CLDNs, as had been thought initially (Fig. 4a) [17, 71, 81, 94]. Currently the N-P-(V/L)-(V/L/T)-(P/A) motif in the second extracellular domain of CLDN is considered to determine the sensitivity of CLDNs for CPE, whereas the (A/N/S)-I-(I/L/V)-(T/V) motif in the first extracellular domain of CLDN is thought to support the interaction between CLDNs and CPE by enlarging the hydrophobic contact area [71]. In this regard, mutations within the (A/N/S)-I-(I/L/V)-(T/V) motif of mouse CLDN-19 clearly attenuated its interaction with C-CPE to the same extent as mutation in the N-P-(V/L)-(V/L/T)-(P/A) motif [71]. Further knowledge regarding the structures of other CLDNs and CLDNs–C-CPE complexes will enable the generation mono-CLDN-specific C-CPEs and their derivatives.
Structure of the C-CPE:CLDN-19 complex. a The structure of the C-CPE:CLDN-19 complex (PDB code, 3X29) by X-ray crystallography. The regions of CLDN-19 that are involved in binding CPE (red) and those of C-CPE that are involved in binding CLDN-19 (blue) are shown. b A schematic diagram of CLDN structure. Regions involved in the interaction with C-CPE are circled
Conclusion
Since its discovery as a CLDN binder, CPE has connected the dots leading from the conceptualization of CLDN-targeted cancer therapy to its potential realization as a novel therapeutic and diagnostic modality. Many studies have shown that CPE-mediated cytolysis can be an effective anti-tumor treatment for CPE-sensitive CLDN-overexpressing cancers, regardless of whether the lesions are chemotherapy-sensitive or -resistant. In particular, CLDN-3, -4, -6, and -7 are CPE-sensitive and frequently overexpressed in various cancers. In addition, C-CPE is a useful adjunct cancer therapy because it enhances the permeability of anti-tumor drugs into tumor tissues and increases the sensitivity to such drugs at the single-cell level. Alternatively, probe-conjugated C-CPE efficiently detects micrometastatic cancers and hyperplastic lesions. However, despite these diverse potential applications, neither CPE itself nor any CPE-based derivative is currently under study in a clinical trial. To advance CPE-based cancer diagnosis and therapy, new CLDN binders with high druggability need to be developed.
References
Anderson WJ, Zhou Q, Alcalde V, Kaneko OF, Blank LJ, Sherwood RI, Guseh JS, Rajagopal J, Melton DA (2008) Genetic targeting of the endoderm with Claudin-6(CreER). Dev Dynam 237:504–512
Baronzio G, Parmar G, Baronzio M (2015) Overview of methods for overcoming hindrance to drug delivery to tumors, with special attention to tumor interstitial fluid. Front Oncol 5:165
Ben-David U, Nudel N, Benvenisty N (2013) Immunologic and chemical targeting of the tight-junction protein claudin-6 eliminates tumorigenic human pluripotent stem cells. Nat Commun 4
Beyer I, Cao H, Persson J, Song H, Richter M, Feng Q, Yumul R, van Rensburg R, Li Z, Berenson R, Carter D, Roffler S, Drescher C, Lieber A (2012) Coadministration of epithelial junction opener JO-1 improves the efficacy and safety of chemotherapeutic drugs. Clin Cancer Res 18:3340–3351
Beyer I, van Rensburg R, Strauss R, Li Z, Wang H, Persson J, Yumul R, Feng Q, Song H, Bartek J, Fender P, Lieber A (2011) Epithelial junction opener JO-1 improves monoclonal antibody therapy of cancer. Cancer Res 71:7080–7090
Blanchard AA, Skliris GP, Watson PH, Murphy LC, Penner C, Tomes L, Young TL, Leygue E, Myal Y (2009) Claudins 1, 3, and 4 protein expression in ER negative breast cancer correlates with markers of the basal phenotype. Virchows Arch 454:647–656
Borlak J, Meier T, Halter R, Spanel R, Spanel-Borowski K (2005) Epidermal growth factor-induced hepatocellular carcinoma: gene expression profiles in precursor lesions, early stage and solitary tumours. Oncogene 24:1809–1819
Casagrande F, Cocco E, Bellone S, Richter CE, Bellone M, Todeschini P, Siegel E, Varughese J, Arin-Silasi D, Azodi M, Rutherford TJ, Pecorelli S, Schwartz PE, Santin AD (2011) Eradication of chemotherapy-resistant CD44+ human ovarian cancer stem cells in mice by intraperitoneal administration of Clostridium perfringens enterotoxin. Cancer-. Am Cancer Soc 117:5519–5528
Chakrabarti G, McClane BA (2005) The importance of calcium influx, calpain and calmodulin for the activation of CaCo-2 cell death pathways by Clostridium perfringens enterotoxin. Cell Microbiol 7:129–146
Chen J, Theoret JR, Shrestha A, Smedley JG 3rd, McClane BA (2012) Cysteine-scanning mutagenesis supports the importance of Clostridium perfringens enterotoxin amino acids 80 to 106 for membrane insertion and pore formation. Infect Immun 80:4078–4088
Cheung ST, Leung KL, Ip YC, Chen X, Fong DY, Ng IO, Fan ST, So S (2005) Claudin-10 expression level is associated with recurrence of primary hepatocellular carcinoma. Clin Cancer Res 11:551–556
Cocco E, Shapiro EM, Gasparrini S, Lopez S, Schwab CL, Bellone S, Bortolomai I, Sumi NJ, Bonazzoli E, Nicoletti R, Deng Y, Saltzman WM, Zeiss CJ, Centritto F, Black JD, Silasi DA, Ratner E, Azodi M, Rutherford TJ, Schwartz PE, Pecorelli S, Santin AD (2015) Clostridium perfringens enterotoxin C-terminal domain labeled to fluorescent dyes for in vivo visualization of micrometastatic chemotherapy-resistant ovarian cancer. Int J Cancer 137:2618–2629
Davidson B, Zhang Z, Kleinberg L, Li M, Florenes VA, Wang TL, Shih IM (2006) Gene expression signatures differentiate ovarian/peritoneal serous carcinoma from diffuse malignant peritoneal mesothelioma. Clin Cancer Res 12:5944–5950
de Oliveira SS, de Oliveira IM, De Souza W, Morgado-Diaz JA (2005) Claudins upregulation in human colorectal cancer. FEBS Lett 579:6179–6185
DeFeo-Jones D, Garsky VM, Wong BK, Feng DM, Bolyar T, Haskell K, Kiefer DM, Leander K, McAvoy E, Lumma P, Wai J, Senderak ET, Motzel SL, Keenan K, Van Zwieten M, Lin JH, Freidinger R, Huff J, Oliff A, Jones RE (2000) A peptide-doxorubicin prodrug activated by prostate-specific antigen selectively kills prostate tumor cells positive for prostate-specific antigen in vivo. Nat Med 6:1248–1252
dos Reis PP, Bharadwaj RR, Machado J, MacMillan C, Pintilie M, Sukhai MA, Perez-Ordonez B, Gullane P, Irish J, Kamel-Reid S (2008) Claudin 1 overexpression increases invasion and is associated with aggressive histological features in oral squamous cell carcinoma. Cancer-Am Cancer Soc 113:3169–3180
Fujita K, Katahira J, Horiguchi Y, Sonoda N, Furuse M, Tsukita S (2000) Clostridium perfringens enterotoxin binds to the second extracellular loop of claudin-3, a tight junction integral membrane protein. FEBS Lett 476:258–261
Furuse M, Fujita K, Hiiragi T, Fujimoto K, Tsukita S (1998) Claudin-1 and -2: novel integral membrane proteins localizing at tight junctions with no sequence similarity to occludin. J Cell Biol 141:1539–1550
Furuse M, Sasaki H, Fujimoto K, Tsukita S (1998) A single gene product, claudin-1 or -2, reconstitutes tight junction strands and recruits occludin in fibroblasts. J Cell Biol 143:391–401
Gao Z, Xu X, McClane B, Zeng Q, Litkouhi B, Welch WR, Berkowitz RS, Mok SC, Garner EI (2011) C terminus of Clostridium perfringens enterotoxin downregulates CLDN4 and sensitizes ovarian cancer cells to taxol and carboplatin. Clin Cancer Res 17:1065–1074
Grass JE, Gould LH, Mahon BE (2013) Epidemiology of foodborne disease outbreaks caused by Clostridium perfringens, United States, 1998–2010. Foodborne Pathog Dis 10:131–136
Grone J, Weber B, Staub E, Heinze M, Klaman I, Pilarsky C, Hermann K, Castanos-Velez E, Ropcke S, Mann B, Rosenthal A, Buhr HJ (2007) Differential expression of genes encoding tight junction proteins in colorectal cancer: frequent dysregulation of claudin-1, -8 and -12. Int J Color Dis 22:651–659
Gunzel D, Fromm M (2012) Claudins and other tight junction proteins. Compr Physiol 2:1819–1852
Hanna PC, Mietzner TA, Schoolnik GK, Mcclane BA (1991) Localization of the receptor-binding region of clostridium-perfringens enterotoxin utilizing cloned toxin fragments and synthetic peptides—the 30 C-terminal amino-acids define a functional binding region. J Biol Chem 266:11037–11043
Herschkowitz JI, Simin K, Weigman VJ, Mikaelian I, Usary J, Hu ZY, Rasmussen KE, Jones LP, Assefnia S, Chandrasekharan S, Backlund MG, Yin YZ, Khramtsov AI, Bastein R, Quackenbush J, Glazer RI, Brown PH, Green JE, Kopelovich L, Furth PA, Palazzo JP, Olopade OI, Bernard PS, Churchill GA, Van Dyke T, and Perou CM (2007) Identification of conserved gene expression features between murine mammary carcinoma models and human breast tumors. Genome Biol 8:
Higashi Y, Suzuki S, Sakaguchi T, Nakamura T, Baba S, Reinecker HC, Nakamura S, Konno H (2007) Loss of claudin-1 expression correlates with malignancy of hepatocellular carcinoma. J Surg Res 139:68–76
Hofmann HS, Bartling B, Simm A, Murray R, Aziz N, Hansen G, Silber RE, Burdach S (2006) Identification and classification of differentially expressed genes in non-small cell lung cancer by expression profiling on a global human 59.620-element oligonucleotide array. Oncol Rep 16:587–595
Hornsby CD, Cohen C, Amin MB, Picken MM, Lawson D, Yin-Goen QQ, Young AN (2007) Claudin-7 immunohistochemistry in renal tumors—a candidate marker for chromophobe renal cell carcinoma identified by gene expression profiling. Arch Pathol Lab Med 131:1541–1546
Hough CD, Sherman-Baust CA, Pizer ES, Montz FJ, Im DD, Rosenshein NB, Cho KR, Riggins GJ, Morin PJ (2000) Large-scale serial analysis of gene expression reveals genes differentially expressed in ovarian cancer. Cancer Res 60:6281–6287
Karanjawala ZE, Illei PB, Ashfaq R, Infante JR, Murphy K, Pandey A, Schulick R, Winter J, Sharma R, Maitra A, Goggins M, Hruban RH (2008) New markers of pancreatic cancer identified through differential gene expression analyses: claudin 18 and annexin A8. Am J Surg Pathol 32:188–196
Katahira J, Inoue N, Horiguchi Y, Matsuda M, Sugimoto N (1997) Molecular cloning and functional characterization of the receptor for Clostridium perfringens enterotoxin. J Cell Biol 136:1239–1247
Katahira J, Sugiyama H, Inoue N, Horiguchi Y, Matsuda M, Sugimoto N (1997) Clostridium perfringens enterotoxin utilizes two structurally related membrane proteins as functional receptors in vivo. J Biol Chem 272:26652–26658
Kim TH, Huh JH, Lee S, Kang H, Kim GI, An HJ (2008) Down-regulation of claudin-2 in breast carcinomas is associated with advanced disease. Histopathology 53:48–55
Kinugasa T, Huo Q, Higash D, Shibaguchi H, Kuroki M, Tanaka T, Futami K, Yamashita Y, Hachimine K, Maekawa S, Nabeshima K, Iwasaki H, Kuroki M (2007) Selective up-regulation of claudin-1 and claudin-2 in colorectal cancer. Anticancer Res 27:3729–3734
Kitadokoro K, Nishimura K, Kamitani S, Fukui-Miyazaki A, Toshima H, Abe H, Kamata Y, Sugita-Konishi Y, Yamamoto S, Karatani H, Horiguchi Y (2011) Crystal structure of Clostridium perfringens enterotoxin displays features of beta-pore-forming toxins. J Biol Chem 286:19549–19555
Kokai-Kun JF, Benton K, Wieckowski EU, McClane BA (1999) Identification of a Clostridium perfringens enterotoxin region required for large complex formation and cytotoxicity by random mutagenesis. Infect Immun 67:5634–5641
Kominsky SL (2006) Claudins: emerging targets for cancer therapy. Expert Rev Mol Med 8:1–11
Kominsky SL, Vali M, Korz D, Gabig TG, Weitzman SA, Argani P, Sukumar S (2004) Clostridium perfringens enterotoxin elicits rapid and specific cytolysis of breast carcinoma cells mediated through tight junction proteins claudin 3 and 4. Am J Pathol 164:1627–1633
Kondoh M, Masuyama A, Takahashi A, Asano N, Mizuguchi H, Koizumi N, Fujii M, Hayakawa T, Horiguchi Y, Watanbe Y (2005) A novel strategy for the enhancement of drug absorption using a claudin modulator. Mol Pharmacol 67:749–756
Konecny GE, Agarwal R, Keeney GA, Winterhoff B, Jones MB, Mariani A, Riehle D, Neuper C, Dowdy SC, Wang HJ, Morin PJ, Podratz KC (2008) Claudin-3 and claudin-4 expression in serous papillary, clear-cell, and endometrioid endometrial cancer. Gynecol Oncol 109:263–269
Kuhn S, Koch M, Nubel T, Ladwein M, Antolovic D, Klingbeil P, Hildebrand D, Moldenhauer G, Langbein L, Franke WW, Weitz J, Zoller M (2007) A complex of EpCAM, claudin-7, CD44 variant isoforms, and tetraspanins promotes colorectal cancer progression. Mol Cancer Res 5:553–567
Kyuno D, Yamaguchi H, Ito T, Kono T, Kimura Y, Imamura M, Konno T, Hirata K, Sawada N, Kojima T (2014) Targeting tight junctions during epithelial to mesenchymal transition in human pancreatic cancer. World J Gastroentero 20:10813–10824
Landers KA, Samaratunga H, Teng L, Buck M, Burger MJ, Scells B, Lavin MF, Gardiner RA (2008) Identification of claudin-4 as a marker highly overexpressed in both primary and metastatic prostate cancer. Brit. J Cancer 99:491–501
Leach MW, Rottman JB, Hock MB, Finco D, Rojko JL, Beyer JC (2014) Immunogenicity/hypersensitivity of biologics. Toxicol Pathol 42:293–300
Lechpammer M, Resnick MB, Sabo E, Yakirevich E, Greaves WO, Sciandra KT, Tavares R, Noble LC, DeLellis RA, Wang LJ (2008) The diagnostic and prognostic utility of claudin expression in renal cell neoplasms. Modern Pathol 21:1320–1329
Lee AS, Tang C, Rao MS, Weissman IL, Wu JC (2013) Tumorigenicity as a clinical hurdle for pluripotent stem cell therapies. Nat Med 19:998–1004
Lee JW, Lee SJ, Seo J, Song SY, Ahn G, Park CS, Lee JH, Kim BG, Bae DS (2005) Increased expressions of claudin-1 and claudin-7 during the progression of cervical neoplasia. Gynecol Oncol 97:53–59
Leech AO, Cruz RG, Hill AD, Hopkins AM (2015) Paradigms lost-an emerging role for over-expression of tight junction adhesion proteins in cancer pathogenesis. Ann Transl Med 3:184
Li XR, Saeki R, Watari A, Yagi K, Kondoh M (2014) Tissue distribution and safety evaluation of a claudin-targeting molecule, the C-terminal fragment of Clostridium perfringens enterotoxin. Eur J Pharm Sci 52:132–137
Ling J, Liao H, Clark R, Wong MS, Lo DD (2008) Structural constraints for the binding of short peptides to claudin-4 revealed by surface plasmon resonance. J Biol Chem 283:30585–30595
Long HY, Crean CD, Lee WH, Cummings OW, Gabig TG (2001) Expression of Clostridium perfringens enterotoxin receptors claudin-3 and claudin-4 in prostate cancer epithelium. Cancer Res 61:7878–7881
Maeda T, Murata M, Chiba H, Takasawa A, Tanaka S, Kojima T, Masumori N, Tsukamoto T, Sawada N (2012) Claudin-4-targeted therapy using Clostridium perfringens enterotoxin for prostate cancer. Prostate 72:351–360
Marcucci F, Corti A (2012) Improving drug penetration to curb tumor drug resistance. Drug Discov Today 17:1139–1146
Michl P, Buchholz M, Rolke M, Kunsch S, Lohr M, McClane B, Tsukita S, Leder G, Adler G, Gress TM (2001) Claudin-4: a new target for pancreatic cancer treatment using Clostridium perfringens enterotoxin. Gastroenterology 121:678–684
Mineta K, Yamamoto Y, Yamazaki Y, Tanaka H, Tada Y, Saito K, Tamura A, Igarashi M, Endo T, Takeuchi K, Tsukita S (2011) Predicted expansion of the claudin multigene family. FEBS Lett 585:606–612
Moldvay J, Jackel M, Paska C, Soltesz I, Schaff Z, Kiss A (2007) Distinct claudin expression profile in histologic subtypes of lung cancer. Lung Cancer 57:159–167
Montgomery E, Mamelak AJ, Gibson M, Maitra A, Sheikh S, Amr SS, Yang S, Brock M, Forastiere A, Zhang S, Murphy KM, Berg KD (2006) Overexpression of claudin proteins in esophageal adenocarcinoma and its precursor lesions. Appl Immunohisto M M 14:24–30
Morita K, Furuse M, Fujimoto K, Tsukita S (1999) Claudin multigene family encoding four-transmembrane domain protein components of tight junction strands. P Natl Acad Sci USA 96:511–516
Mosley M, Knight J, Neesse A, Michl P, Iezzi M, Kersemans V, Cornelissen B (2015) Claudin-4 SPECT imaging allows detection of aplastic lesions in a mouse model of breast cancer. J Nucl Med 56:745–751
Nacht M, Ferguson AT, Zhang W, Petroziello JM, Cook BP, Gao YH, Maguire S, Riley D, Coppola G, Landes GM, Madden SL, Sukumar S (1999) Combining serial analysis of gene expression and array technologies to identify genes differentially expressed in breast cancer. Cancer Res 59:5464–5470
Nakanishi K, Ogata S, Hiroi S, Tominaga S, Aida S, Kawai T (2008) Expression of occludin and claudins 1, 3, 4, and 7 in urothelial carcinoma of the upper urinary tract. Am J Clin Pathol 130:43–49
Neesse A, Hahnenkamp A, Griesmann H, Buchholz M, Hahn SA, Maghnouj A, Fendrich V, Ring J, Sipos B, Tuveson DA, Bremer C, Gress TM, Michl P (2013) Claudin-4-targeted optical imaging detects pancreatic cancer and its precursor lesions. Gut 62:1034–1043
Nichols LS, Ashfaq R, Iacobuzio-Donahue CA (2004) Claudin 4 protein expression in primary and metastatic pancreatic cancer—support for use as a therapeutic target. Am J Clin Pathol 121:226–230
Oliveira SS, Morgado-Diaz JA (2007) Claudins: multifunctional players in epithelial tight junctions and their role in cancer. Cell Mol Life Sci 64:17–28
Park JY, Park KH, TY O, Hong SP, Jeon TJ, Kim CH, Park SW, Chung JB, Song SY, Bang S (2007) Up-regulated claudin 7 expression in intestinal-type gastric carcinoma. Oncol Rep 18:377–382
Protze J, Eichner M, Piontek A, Dinter S, Rossa J, Blecharz KGZ, Vajkoczy P, Piontek J, Krause G (2015) Directed structural modification of Clostridium perfringens enterotoxin to enhance binding to claudin-5. Cell Mol Life Sci 72:1417–1432
Resnick MB, Gavilanez M, Newton E, Konkin T, Bhattacharya B, Britt DE, Sabo E, Moss SF (2005) Claudin expression in gastric adenocarcinomas: a tissue microarray study with prognostic correlation. Hum Pathol 36:886–892
Resnick MB, Konkin T, Routhier J, Sabo E, Pricolo VE (2005) Claudin-1 is a strong prognostic indicator in stage II colonic cancer: a tissue microarray study. Modern Pathol 18:511–518
Romanov V, Whyard TC, Waltzer WC, Gabig TG (2014) A claudin 3 and claudin 4-targeted Clostridium perfringens protoxin is selectively cytotoxic to PSA-producing prostate cancer cells. Cancer Lett 351:260–264
Sahin U, Koslowski M, Dhaene K, Usener D, Brandenburg G, Seitz G, Huber C, Tureci O (2008) Claudin-18 splice variant 2 is a pan-cancer target suitable for therapeutic antibody development. Clin Cancer Res 14:7624–7634
Saitoh Y, Suzuki H, Tani K, Nishikawa K, Irie K, Ogura Y, Tamura A, Tsukita S, Fujiyoshi Y (2015) Structural insight into tight junction disassembly by Clostridium perfringens enterotoxin. Science 347:775–778
Sanada Y, Oue N, Mitani Y, Yoshida K, Nakayama H, Yasui W (2006) Down-regulation of the claudin-18 gene, identified through serial analysis of gene expression data analysis, in gastric cancer with an intestinal phenotype. J Pathol 208:633–642
Santin AD, Bellone S, Siegel ER, McKenney JK, Thomas M, Roman JJ, Burnett A, Tognon G, Bandiera E, Pecorelli S (2007) Overexpression of Clostridium perfringens enterotoxin receptors claudin-3 and claudin-4 in uterine carcinosarcomas. Clin Cancer Res 13:3339–3346
Santin AD, Cane S, Bellone S, Palmieri M, Siegel ER, Thomas M, Roman JJ, Burnett A, Cannon MJ, Pecorelli S (2005) Treatment of chemotherapy-resistant human ovarian cancer xenografts in C.B-17/SCID mice by intraperitoneal administration of Clostridium perfringens enterotoxin. Cancer Res 65:4334–4342
Santin AD, Zhan FH, Bellone S, Palmieri M, Cane S, Bignotti E, Anfossi S, Gokden M, Dunn D, Roman JJ, O’Brien TJ, Tian EM, Cannon MJ, Shaughnessy J, Pecorelli S (2004) Gene expression profiles in primary ovarian serous papillary tumors and normal ovarian epithelium: identification of candidate molecular markers for ovarian cancer diagnosis and therapy. Int J Cancer 112:14–25
Shang X, Lin X, Manorek G, Howell SB (2013) Claudin-3 and claudin-4 regulate sensitivity to cisplatin by controlling expression of the copper and cisplatin influx transporter CTR1. Mol Pharmacol 83:85–94
Sobel G, Paska C, Szabo I, Kiss A, Kadar A, Schaff Z (2005) Increased expression of claudins in cervical squamous intraepithelial neoplasia and invasive carcinoma. Hum Pathol 36:162–169
Soini Y, Talvensaari-Mattila A (2006) Expression of claudins 1, 4, 5, and 7 in ovarian tumors of diverse types. Int J Gynecol Pathol 25:330–335
Sonoda N, Furuse M, Sasaki H, Yonemura S, Katahira J, Horiguchi Y, Tsukita S (1999) Clostridium perfringens enterotoxin fragment removes specific claudins from tight junction strands: evidence for direct involvement of claudins in tight junction barrier. J Cell Biol 147:195–204
Sugii S (1994) Analysis of multiple antigenic determinants of clostridium-perfringens enterotoxin as revealed by use of different synthetic peptides. J Vet Med Sci 56:1047–1050
Suzuki H, Nishizawa T, Tani K, Yamazaki Y, Tamura A, Ishitani R, Dohmae N, Tsukita S, Nureki O, Fujiyoshi Y (2014) Crystal structure of a claudin provides insight into the architecture of tight junctions. Science 344:304–307
Szasz AM, Nyirady P, Majoros A, Szendroi A, Szucs M, Szekely E, Tokes AM, Romics I, Kulka J (2010) Beta-catenin expression and claudin expression pattern as prognostic factors of prostatic cancer progression. BJU Int 105:716–722
Tabaries S, Dong Z, Annis MG, Omeroglu A, Pepin F, Ouellet V, Russo C, Hassanain M, Metrakos P, Diaz Z, Basik M, Bertos N, Park M, Guettier C, Adam R, Hallett M, Siegel PM (2011) Claudin-2 is selectively enriched in and promotes the formation of breast cancer liver metastases through engagement of integrin complexes. Oncogene 30:1318–1328
Takahashi A, Komiya E, Kakutani H, Yoshida T, Fujii M, Horiguchi Y, Mizuguchi H, Tsutsumi Y, Tsunoda S, Koizumi N, Isoda K, Yagi K, Watanabe Y, Kondoh M (2008) Domain mapping of a claudin-4 modulator, the C-terminal region of C-terminal fragment of Clostridium perfringens enterotoxin, by site-directed mutagenesis. Biochem Pharmacol 75:1639–1648
Takahashi A, Kondoh M, Masuyama A, Fujii M, Mizuguchi H, Horiguchi Y, Watanabe Y (2005) Role of C-terminal regions of the C-terminal fragment of Clostridium perfringens enterotoxin in its interaction with claudin-4. J Control Release 108:56–62
Takahashi A, Kondoh M, Uchida H, Kakamu Y, Hamakubo T, Yagi K (2011) Mutated C-terminal fragments of Clostridium perfringens enterotoxin have increased affinity to claudin-4 and reversibly modulate tight junctions in vitro. Biochem Biophys Res Commun 410:466–470
Tassi RA, Bignotti E, Falchetti M, Ravanini M, Calza S, Ravaggi A, Bandiera E, Facchetti F, Pecorelli S, Santin AD (2008) Claudin-7 expression in human epithelial ovarian cancer. Int J Gynecol Cancer 18:1262–1271
Thuma F, Zoller M (2013) EpCAM-associated claudin-7 supports lymphatic spread and drug resistance in rat pancreatic cancer. Int J Cancer 133:855–866
Uchida H, Kondoh M, Hanada T, Takahashi A, Hamakubo T, Yagi K (2010) A claudin-4 modulator enhances the mucosal absorption of a biologically active peptide. Biochem Pharmacol 79:1437–1444
Ushiku T, Shinozaki-Ushiku A, Maeda D, Morita S, Fukayama M (2012) Distinct expression pattern of claudin-6, a primitive phenotypic tight junction molecule, in germ cell tumours and visceral carcinomas. Histopathology 61:1043–1056
Van Itallie CM, Betts L, Smedley JG 3rd, McClane BA, Anderson JM (2008) Structure of the claudin-binding domain of Clostridium perfringens enterotoxin. J Biol Chem 283:268–274
Veshnyakova A, Piontek J, Protze J, Waziri N, Heise I, Krause G (2012) Mechanism of Clostridium perfringens enterotoxin interaction with claudin-3/-4 protein suggests structural modifications of the toxin to target specific claudins. J Biol Chem 287:1698–1708
Wallace FM, Mach AS, Keller AM, Lindsay JA (1999) Evidence for Clostridium perfringens enterotoxin (CPE) inducing a mitogenic and cytokine response in vitro and a cytokine response in vivo. Curr Microbiol 38:96–100
Winkler L, Gehring C, Wenzel A, Muller SL, Piehl C, Krause G, Blasig IE, Piontek J (2009) Molecular determinants of the interaction between Clostridium perfringens enterotoxin fragments and claudin-3. J Biol Chem 284:18863–18872
Yoshida H, Sumi T, Zhi X, Yasui T, Honda KI, Ishiko O (2011) Claudin-4: a potential therapeutic target in chemotherapy-resistant ovarian cancer. Anticancer Res 31:1271–1277
Yuan X, Lin X, Manorek G, Kanatani I, Cheung LH, Rosenblum MG, Howell SB (2009) Recombinant CPE fused to tumor necrosis factor targets human ovarian cancer cells expressing the claudin-3 and claudin-4 receptors. Mol Cancer Ther 8:1906–1915
Zheng JY, Yu D, Foroohar M, Ko E, Chan J, Kim N, Chiu R, Pang S (2003) Regulation of the expression of the prostate-specific antigen by claudin-7. J Membrane Biol 194:187–197
Acknowledgments
We thank all of the members of our laboratory for their useful comments. This work was supported by a Health and Labour Sciences Research Grant from the Ministry of Health, Labour, and Welfare of Japan; a research grant from the Japan Agency for Medical Research and Development (AMED); a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology of Japan [grant number 24390042]; and funds from the Adaptable and Seamless Technology Transfer Program through Target-driven R&D Agency; Platform for Drug Discovery, Informatics, and Structural Life Science from the Ministry of Education, Culture, Sports, Science and Technology, Japan; and the Takeda Science Foundation. Y.H. is supported by a Research Fellowship for Young Scientists from the Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hashimoto, Y., Yagi, K. & Kondoh, M. Roles of the first-generation claudin binder, Clostridium perfringens enterotoxin, in the diagnosis and claudin-targeted treatment of epithelium-derived cancers. Pflugers Arch - Eur J Physiol 469, 45–53 (2017). https://doi.org/10.1007/s00424-016-1878-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-016-1878-6