Abstract
Purpose
Although there have been many reports on learning curves for robotic surgery, it is unclear how surgeons’ conventional laparoscopic surgical skills influence their ability in performing robotic surgery for colorectal cancer (CRC). The aim of this study was to determine the surgical outcomes of robotic surgery for CRC during the induction phase by skilled laparoscopic surgeons.
Methods
Surgical outcomes of consecutive CRC cases between January 2021 and March 2023 following the skilled phase of laparoscopic surgery and introductory phase of robotic surgery performed by three skilled laparoscopic surgeons were compared.
Results
Overall, 77 consecutive patients diagnosed with sigmoid colon or rectosigmoid cancer were analysed, including 50 in the laparoscopy group (LAP) and 27 in the robotic group (Ro). Patient characteristics, including age, sex, body mass index, and tumour progression, did not differ between the groups. The median operation time was 204 min in the robotic group and 170 min in the laparoscopic group (p < 0.001). Blood loss was significantly lower in the robotic group (p = 0.0059). The incidence of grade 2 or higher complications did not differ between the two groups (LAP, 10.0% vs. Ro, 7.4%, p = 1). In the robotic group, the time required for lymph node dissection had a greater impact on operative duration.
Conclusion
Skills acquired from performing conventional laparoscopic surgery may contribute to the safe and reliable performance of robotic surgery for CRC.
Trial registration
UMIN000050923.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most common cancer worldwide [1]. Minimally invasive surgery (MIS) has been widely performed for CRC, and its safety and usefulness have been reported. Conventional laparoscopic surgery was introduced in 1980 and has continuously been developed [2]. The types of MIS that surgeons should learn include laparoscopic and robotic surgeries. Additionally, surgeons should strive to improve their surgical skills. Robotic surgery in CRC is characterised by improved operability compared to conventional laparoscopic surgery by utilising an articulated arm from the viewpoint of ergonomics [3–5]. It has been reported that a learning curve exists even with this state-of-the-art technology [6–8]. However, there is no clear evidence that robotic surgery can be performed safely by surgeons in the early stages of implementation, and it is unknown how surgeons’ experience and skills in laparoscopic surgery will affect their transition to performing robotic surgery.
In Japan, an objective evaluation system for the quality of conventional laparoscopic surgery was introduced in 2004 by the Japan Society for Endoscopic Surgery (JSES), contributing to the improvement of surgical skills of young surgeons[9, 10]. The number of successful applicants in the field of CRC using this evaluation system has been somewhat low (21–34% in the last 10 years) as it is a high-level evaluation system. Surgeons certified under this system have been objectively evaluated as having a certain level of laparoscopic surgical skill. However, it remains to be seen whether robotic surgery can be safely performed by certified laparoscopic surgeons. Although several reports have examined the learning curve required for successfully robotic surgery, there is no evidence of how experience with laparoscopic surgery influences a surgeon’s ability in performing robotic surgery.
Therefore, we aimed to determine how being certified as a “skilled laparoscopic surgeon (SLS)” is related to surgical outcomes following robotic colorectal surgery.
Patients and methods
This multicentre retrospective cohort study was conducted by the Yokohama City University Medical Centre (Yokohama, Japan). This study was conducted in accordance with the Declaration of Helsinki. Because of the retrospective nature of the study, written informed consent was not required, and subjects were given the opportunity to refuse to participate in the study using an opt-out method. This study was approved by the Institutional Review Board of Yokohama City University Medical Centre (Number F230300043) and registered in the Japanese Clinical Trials Registry as UMIN000050923.
Patients who underwent laparoscopic or robotic surgery for CRC at two high-volume centres (Yokohama City University Hospital and Yokohama City University Medical Centre) between January 2021 and March 2023 were selected for this study. Patient data, including clinical and pathological information, were extracted from their medical records. The Union for International Cancer Control TNM classification (eighth edition) was used to identify tumour progression [11].
The laparoscopic skill evaluation system in colorectal surgery covers laparoscopic surgery for sigmoid colon or rectosigmoid colon cancer. Under this system, a surgeon’s laparoscopic video is evaluated by several colorectal surgeons to determine the SLS certification.
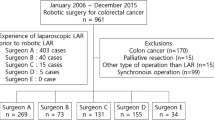
Between January 2021 and March 2023, three independent and young colorectal surgeons from two high-volume centres performed conventional laparoscopic surgery for sigmoid colon or rectosigmoid cancer. As a result, the three young surgeons were simultaneously certified as SLS by the JSES in April 2022. After the SLS qualification, the three surgeons also began performing robotic surgery. All surgeons were trained using the da Vinci Surgical Skills Simulator (Intuitive Surgical Inc., Sunnyvale, CA, USA) prior to the introduction of robotic surgery. We compared the outcomes of conventional laparoscopic surgery performed by the three surgeons immediately prior to SLS certification with those of robotic surgery in the induction phase immediately after certification (Fig. 1).
Patient selection
The inclusion criteria were as follows: (1) patients who underwent laparoscopic or robotic surgery for sigmoid colon or rectosigmoid cancer performed by any of the three surgeons, and (2) patients who underwent D2 or D3 lymph node dissection. Patients with ulcerative colitis-associated colorectal cancer, a history of colectomy, and those who underwent emergency surgery were excluded. Patients requiring splenic flexure mobilisation were also excluded because it increases the risk of splenic injury, increases operative difficulty, and prolongs operation time. In this study, the definition of tumour localisation was determined with reference to sagittal images, such as those from computed tomography, magnetic resonance imaging, or irrigoscopy. The height of the sacral promontory was defined as the rectosigmoid junction (RSJ) and was used as an anatomic landmark. Sigmoid colon and rectosigmoid cancer were defined as tumours arising from the proximal and distal RSJ, respectively (Fig. 2). Cases wherein the inferior margin of the tumour exceeded the second sacral vertebra were excluded from cases of rectosigmoid cancer.
Surgical procedure
The same procedures and techniques were employed in all cases, including anastomosis and mesenteric dissection, in both laparoscopic and robotic surgery. Conventional laparoscopic resection was performed using five trocars (Fig. 3a). Robotic surgery was performed using the da Vinci Xi surgical system (Intuitive Surgical Inc., Sunnyvale, CA, USA), with four dedicated robotic ports for the tip-up grasper, monopolar curved scissors, fenestrated bipolar forceps, and camera. Additionally, one assistant port used by the assistant surgeon was placed in the upper abdomen (Fig. 3b).
The surgical procedure was as follows: (1) sigmoid mesenteric mobilization through the medial approach, (2) resection of the inferior mesenteric artery (IMA) with apical lymph node dissection, (3) resection of the inferior mesenteric vein and the left colic artery (LCA), (4) lateral approach, (5) rectal mobilization, (6) rectal resection on the anal side of the tumour by linear stapler, and (7) anastomosis.
D3 lymph node dissection was the protocol; however, D2 dissection was performed in some patients, including elderly patients and those with several comorbidities. For D3 dissection, the apical lymph nodes were dissected, and the IMA was clipped at the origin and divided (Fig. 4a). In D2 dissection, the apical nodes were not dissected, and the IMA was clipped peripherally after the LCA bifurcation (Fig. 4b). In the present case, blood perfusion to the LCA was preserved. Subsequently, the lateral approach began at the lateral peritoneal fold near the descending sigmoid flexure and was continuous with the dissected layer of the medial approach. The tumour-specific mesorectal excision concept was then used to dissect the presacral space in the order of midline, right side, and left side while protecting the hypogastric nerves. The endpoint of the distal dissection was approximately 5 cm below the tumour in cases of rectosigmoid cancer and 10 cm in cases of sigmoid colon cancer. Therefore, the techniques for sigmoid colon and rectosigmoid cancer were almost identical. The rectum was then transected using a linear stapler.
The specimen was extracted by extending the umbilical incision by 3–5 cm. Before anastomosis, anastomotic perfusion was evaluated using indocyanine green fluorescence imaging or intraoperative visual judgment based on clinical findings such as colour and pulsation. Anastomosis was performed intracorporeally using the double stapling technique.
Interest of outcomes
The primary endpoint of this study was the incidence of perioperative complications. The Clavien–Dindo (CD) classification was used to evaluate complications, and grade 2 or higher complications were considered major complications [12]. The secondary endpoints were operation time, blood loss, and console time. Additionally, the minimally invasive surgical duration (MID) required for each part of the surgery was analysed for each group. In accordance with our surgical procedures, we categorised procedures into the following: Sect. 1, from the start of the medial approach to IMA ligation (lymph node dissection); Sect. 2, continuation of the medial approach to the end of the lateral approach; Sect. 3, rectal mobilisation; and Sect. 4, mesorectal dissection and rectal resection with a stapler. To compare the time required for each part, the start of the procedure was defined as the beginning of the incision of the medial approach and the end of the rectal dissection with the stapler.
Statistical analyses
All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). The Mann–Whitney U test was used to compare continuous variables. Differences between categorical variables were identified using the Fisher’s exact probability test. Additionally, the ratio of MID for each of the four sections to the total MID and their correlation were analysed in the laparoscopic and robotic groups using Spearman’s rank correlation coefficient. All statistical analyses were two-tailed, and p-values < 0.05 were considered statistically significant.
Results
Demographic and clinicopathological characteristics of patients who underwent minimally invasive surgery
Overall, 77 consecutive patients diagnosed with sigmoid colon or rectosigmoid cancer were included in the study, including 50 in the laparoscopy group and 27 in the robotic group. Patient characteristics, such as age, sex, body mass index, American Society of Anesthesiologists physical status, Eastern Cooperative Oncology Group Performance Status Scale, and tumour progression, did not differ between the two groups (Table 1). Sigmoid colon cancer was significantly more common in the laparoscopic group (80.0% vs. 37.0%, p < 0.001).
Summary of surgical outcomes for the laparoscopic and robotic groups
The short-term surgical outcomes in each group are summarised in Table 2. The median operation time was 204 and 170 min in the robotic and laparoscopic groups, respectively (p < 0.001). Histograms of the operation time in both groups are shown in Fig. 5. The operation time tended to be more equalised in the robotic group than in the laparoscopic group. Additionally, blood loss was significantly lower in the robotic group (p = 0.0059). There was no difference in the extent of lymph node dissection or number of retrieved lymph nodes between the two groups. The perioperative complications developed in five patients in the laparoscopy group (10%), including two with surgical site infections, one with dysuria, one with anastomotic bleeding, and one with bowel obstruction. Patients with bowel obstruction due to port-site hernia required reoperation. In contrast, two patients in the robotic group had pneumonia; there were no intra-abdominal complications. There were no intraoperative complications, such as intraoperative equipment failure, organ damage, iatrogenic tumour perforation, or massive bleeding, in the robotic group. The median postoperative hospital stay was 7 days in both groups, and no surgery-related deaths occurred.
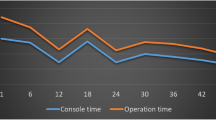
Comparison of time required for each part of the minimally invasive procedures
The MID of the four sections is summarised in Table 3. The median total MID was 86.0 min (IQR: 73.0–95.5 min) and 129.0 min (IQR: 119.0–136.5 min) in the laparoscopic and robotic groups, respectively (p < 0.001). From Sects. 1 to 4, all parts took significantly longer to perform in the robotic group. The correlation of the MID required for each section with the total MID is presented in Table 4. In the laparoscopy group, the correlation coefficients in Sects. 1–3 were almost constant, but in the robotic group, the time spent in Sect. 1 had the greatest impact on the total MID.
Discussion
The present study revealed the safety and feasibility of performing robotic surgery after being certified as a skilled laparoscopic surgeon. Although the robot induction phase prolonged the operation time, blood loss was reduced, and postoperative complications were comparable between laparoscopic and robotic surgeries. Proficiency in laparoscopic surgery suggests that robotic surgery can be safely initiated. Additionally, we compared the time required for each surgical procedure and found that improving the surgical technique up to lymph node dissection may be an important issue for the mastery of robotic surgery.
Approaches to colorectal cancer have changed over time from open surgery to laparoscopic surgery to robotic surgery, and each technique has its own advantages and disadvantages [13–15]. Generally, in robotic surgery, the roles of the main and assistant surgeons in laparoscopic surgery are performed by a single robotic surgeon, reflecting the skill of the individuals.
Robotic surgery for colorectal cancer has rapidly expanded from conventional laparoscopic surgery [16–18]. The advantages of robotic surgery include a faster learning curve and the ability to perform procedures safely and easily in confined spaces by making full use of the multi-joint function [19]. On the other hand, adapting existing surgical skills acquired from performing open and conventional laparoscopic surgery to robotic surgery is an important clinical issue.
Park et al. reported that the learning curve for robotic surgery for low anterior resection was 44 cases, while that for laparoscopic surgery was 41 cases, which were similar [20]. In contrast, De’Angelis et al. reported a faster learning curve for robotic surgery for right-sided colon cancer (16 cases for robotic surgery vs. 25 cases for laparoscopic surgery) [21]. Additionally, a systematic review of learning curves in colorectal cancer surgery by Flynn et al. pointed out the possible influence of surgeon experience on the correlation between platform selection and operation time [22]. Thus, there have been many reports on robotic surgery proficiency. However, most of them do not consider “the objective surgical skill” of the surgeon.
In their review of learning curves in robotic surgery, Wong et al. pointed out factors that may be related to the operation time, including surgical case mix, hybrid technique, operating room team, case complexity, and laparoscopic and open colorectal surgery experience [23]. Odermatt et al. also analysed the robotic total mesocolic resection proficiency process of two surgeons with different levels of laparoscopic surgery experience (206 laparoscopic and 43 robotic vs. 88 laparoscopic and 47 robotic) using propensity score matching and cumulative sum (CUSUM) charts[24]. They revealed that for the more experienced surgeon, the CUSUM curve did not show a clear learning process compared to his laparoscopic surgical standard. In contrast, less experienced surgeons reported a learning process after 15 cases and generally reached their goals. Although robotic surgery is considered a useful platform in minimally invasive surgical procedures, understanding the surgical anatomy and procedures is no different from open or conventional laparoscopic surgery. In this study, we examined the safety and usefulness of robotic surgery performed by an SLS, who was evaluated using an objective evaluation system. The results of the present study showed that the surgical time during the robotic introduction phase was longer, but blood loss was less, and the complication rate was the same, indicating that the same results can be achieved during the robotic introduction phase if the surgeon is skilled in laparoscopic surgery. The ROLARR trial, one of the most well-known randomised control trials of robot-assisted rectal cancer surgery, reported an intraoperative complication rate of 15.3%, including organ damage, significant haemorrhage, anastomotic complication, equipment failure, and iatrogenic tumour perforation [25]. In the present study, however, none of these intraoperative complications were observed in the robotic surgery group. This indicates that robotic surgery can be safely performed by a surgeon proficient in laparoscopic surgery. Additionally, in CRC surgery, the concept of radical resection of the cancer is similar regardless of platform, and proficiency in laparoscopic surgery will help surgeons to master the surgical procedure and anatomy, which will contribute to the introduction of safe robotic surgery.
This study also evaluated the surgical time by dividing the procedure into four parts. In the robotic group, the time from the medial approach to central vascular ligation had a greater impact on total MID than that during laparoscopic surgery. In contrast to conventional laparoscopic surgery, in robotic surgery, one surgeon performs the three roles of main surgeon, assistant and scopist, and may not be familiar with the operation of the third arm in the early stages of implementation. In addition, during the introduction of the robot, more time may have been required for perivascular dissection, such as for inferior mesenteric artery dissection, which requires delicate forceps manipulation. In other words, improving one’s skills during central lymph node dissection may contribute to the learning curve of performing robotic colorectal surgery.
The present study had some limitations. First, the sample size was small with low statistical power. However, the present study examined robotic surgical procedures started “at the same time” by technically certified laparoscopic surgeons who started “the same procedure at the same time,” and because the procedures were homogenised, it is thought to be a clearer representation of the results of the induction phase of robotic surgery compared to the previous report. Second, only cases with localisation in the sigmoid colon or rectum were included. These localisations require relatively less complicated procedures during minimally invasive surgery, and the results of surgery for right-sided colon cancer, transverse colon cancer, and lower rectal cancer, which require delicate dissection around the vein, have not been examined. However, in the introductory phase of robotic surgery, cases with relatively standardised procedures are often selected, as in this study, and are considered more in line with clinical practice. Future studies on the performance of robotic surgery for relatively difficult cases, such as transverse colon cancer and splenic flexure cancer, are needed.
In conclusion, when training for robotic surgery, proficiency in laparoscopic surgery may contribute to the safe and reliable performance of robotic surgery. Additionally, it was suggested that improving one’s technique during central lymph node dissection may be important in the introduction phase of robotic surgery for colorectal cancer.
References
1. Sung H, Ferlay J, Siegel RL, et al (2021) Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 71:209–249. https://doi.org/10.3322/caac.21660
2. Spaner SJ, Warnock GL (1997) A brief history of endoscopy, laparoscopy, and laparoscopic surgery. J Laparoendosc Adv Surg Tech - Part A 7:369–373. https://doi.org/10.1089/lap.1997.7.369
3. Armijo PR, Huang CK, High R, et al (2019) Ergonomics of minimally invasive surgery: an analysis of muscle effort and fatigue in the operating room between laparoscopic and robotic surgery. Surg Endosc 33:2323–2331. https://doi.org/10.1007/s00464-018-6515-3
4. Wong SW, Crowe P (2023) Visualisation ergonomics and robotic surgery. J. Robot. Surg.
5. Wong SW, Ang ZH, Yang PF, Crowe P (2022) Robotic colorectal surgery and ergonomics. J. Robot. Surg. 16:241–246
6. Jiménez-Rodríguez RM, Rubio-Dorado-Manzanares M, Díaz-Pavón JM, et al (2016) Learning curve in robotic rectal cancer surgery: current state of affairs. Int. J. Colorectal Dis. 31:1807–1815
7. Sugishita T, Tsukamoto S, Imaizumi J, et al (2022) Evaluation of the learning curve for robot-assisted rectal surgery using the cumulative sum method. Surg Endosc 36:5947–5955. https://doi.org/10.1007/s00464-021-08960-7
8. Kawai K, Hata K, Tanaka T, et al (2018) Learning Curve of Robotic Rectal Surgery With Lateral Lymph Node Dissection: Cumulative Sum and Multiple Regression Analyses. J Surg Educ 75:1598–1605. https://doi.org/10.1016/j.jsurg.2018.04.018
9. Tanigawa N, Lee SW, Kimura T, et al (2011) The Endoscopic Surgical Skill Qualification System for gastric surgery in Japan. Asian J Endosc Surg 4:112–115. https://doi.org/10.1111/j.1758-5910.2011.00082.x
10. Mori T, Kimura T, Kitajima M (2010) Skill accreditation system for laparoscopic gastroenterologic surgeons in Japan. Minim. Invasive Ther. Allied Technol. 19:18–23
11. Brierley J, Gospodarowicz MD, Wittekind CT (2017) TNM Classification of Malignant Tumors International Union Against Cancer. 8th. Oxford, England: Wiley; 2017. Wiley pp57-62
12. Dindo D, Demartines N, Clavien P-A (2004) Classification of Surgical Complications. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
13. Kim MJ, Park SC, Park JW, et al (2018) Robot-assisted Versus Laparoscopic Surgery for Rectal Cancer: A Phase II Open Label Prospective Randomized Controlled Trial. In: Annals of Surgery. Ann Surg, pp 243–251
14. Sheng S, Zhao T, Wang X (2018) Comparison of robot-assisted surgery, laparoscopic-assisted surgery, and open surgery for the treatment of colorectal cancer A network meta-analysis. Med. (United States) 97
15. Feng Q, Yuan W, Li T, et al (2022) Robotic versus laparoscopic surgery for middle and low rectal cancer (REAL): short-term outcomes of a multicentre randomised controlled trial. Lancet Gastroenterol Hepatol 7:991–1004. https://doi.org/10.1016/S2468-1253(22)00248-5
16. Pai A, Marecik SJ, Park JJ, et al (2015) Oncologic and clinicopathologic outcomes of robot-assisted total mesorectal excision for rectal cancer. Dis Colon Rectum 58:659–667. https://doi.org/10.1097/DCR.0000000000000385
17. Park EJ, Cho MS, Baek SJ, et al (2015) Long-term oncologic outcomes of robotic low anterior resection for rectal cancer. Ann Surg 261:129–137. https://doi.org/10.1097/SLA.0000000000000613
18. Biffi R, Luca F, Bianchi P Pietro, et al (2016) Dealing with robot-assisted surgery for rectal cancer: Current status and perspectives. World J. Gastroenterol. 22:546–556
19. Zaepfel S, Marcovei R, Fernandez-de-Sevilla E, et al (2023) Robotic-assisted surgery for mid and low rectal cancer: a long but safe learning curve. J Robot Surg. https://doi.org/10.1007/s11701-023-01624-9
20. Park EJ, Kim CW, Cho MS, et al (2014) Is the learning curve of robotic low anterior resection shorter than laparoscopic low anterior resection for rectal cancer?: A comparative analysis of clinicopathologic outcomes between robotic and laparoscopic surgeries. Med (United States) 93:. https://doi.org/10.1097/MD.0000000000000109
21. De’Angelis N, Lizzi V, Azoulay D, Brunetti F (2016) Robotic Versus Laparoscopic Right Colectomy for Colon Cancer: Analysis of the Initial Simultaneous Learning Curve of a Surgical Fellow. J Laparoendosc Adv Surg Tech 26:882–892. https://doi.org/10.1089/lap.2016.0321
22. Flynn J, Larach JT, Kong JCH, et al (2021) The learning curve in robotic colorectal surgery compared with laparoscopic colorectal surgery: a systematic review. Color. Dis. 23:2806–2820
23. Wong SW, Crowe P (2022) Factors affecting the learning curve in robotic colorectal surgery. J. Robot. Surg. 16:1249–1256
24. Odermatt M, Ahmed J, Panteleimonitis S, et al (2017) Prior experience in laparoscopic rectal surgery can minimise the learning curve for robotic rectal resections: a cumulative sum analysis. Surg Endosc 31:4067–4076. https://doi.org/10.1007/s00464-017-5453-9
25. Jayne D, Pigazzi A, Marshall H, et al (2017) Effect of robotic-assisted vs conventional laparoscopic surgery on risk of conversion to open laparotomy among patients undergoing resection for rectal cancer the rolarr randomized clinical trial. JAMA - J Am Med Assoc 318:1569–1580. https://doi.org/10.1001/jama.2017.7219
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
This study was not supported by any external funding.
Author information
Authors and Affiliations
Contributions
Drs. KI, MN, AS, KS, YA, KK, NS, TS, YR, and AS contributed to the conception and design of the study. KI, KS, and YA prepared data collection. KI wrote the main manuscript text. All authors reviewed the manuscript and accepted the final version.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Institutional Review Board of Yokohama City University Medical Centre (Number F230300043).
Conflict of interest
All authors declare no conflicts of interest in association with the present study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Iguchi, K., Numata, M., Sugiyama, A. et al. Influence of proficiency in conventional laparoscopic surgery in colorectal cancer on the introduction of robotic surgery. Langenbecks Arch Surg 409, 189 (2024). https://doi.org/10.1007/s00423-024-03380-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-024-03380-2