Abstract
Purpose
Methods to preoperatively stratify oncological risks associated with gastric cancer (GC) are limited. Host inflammatory parameters, i.e., serum C-reactive protein (CRP) and albumin levels, are known to be associated with outcomes. We examined the relationships between disease-specific mortality and four CRP-albumin–based indices (CRP-albumin ratio [CAR], modified Glasgow prognostic score [mGPS], Osaka prognostic score [OPS], and NUn score) preoperatively measured in cases with resectable GC.
Methods
Survival outcomes of 1290 consecutive GC patients with oncological gastrectomy were reviewed. Predictive significances of preoperative CAR, mGPS, OPS, and NUn scores were assessed with time-dependent receiver operating characteristic curves and Cox regression analyses.
Results
Median follow-up was 107 months. Area under the curve for predicting overall and disease-specific survivals (OS/DSS) for the preoperative NUn score was clearly superior to those of the other parameters. On univariate Cox regression analysis, preoperative CAR, mGPS, OPS, and the NUn score all correlated significantly with OS/DSS. On multivariate Cox regression analysis, the preoperative NUn score, as a continuous variable, showed an independent relationship with OS (hazard ratio [HR] 1.32, 95% confidence interval [CI] 1.16–1.50, per 1-unit increase, P < 0.001) and even DSS (HR 1.23, 95% CI 1.02–1.49, P = 0.032). The other three markers failed to maintain independence for DSS.
Conclusions
Preoperative NUn scores are stably associated with outcomes, including disease-specific mortality, possibly serving as a simple measure to define the likelihood of progression to systemic disease after meticulous surgery for GC, which may contribute to identifying patients who would benefit from additional modalities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer (GC) is the fifth most common malignancy worldwide, accounting for approximately 770,000 deaths annually [1]. It has been a major contributor to the global malignant burden, and optimization of the treatment strategy is thus of major interest [2]. Oncological gastrectomy is the mainstay of curative therapy for GC without detectable distant metastases. Furthermore, additional multidisciplinary approaches including perioperative chemotherapy/radiotherapy are options for the population susceptible to disease recurrence [3]. Therefore, objective tools for stratifying oncological risks associated with resectable GC prior to treatment, focusing especially on cancer-related mortality, are of clinical value for guiding individualized management strategies.
Inflammation-related hematological parameters have been advocated as easily available prognostic factors in solid tumors including GC. C-reactive protein (CRP) is an acute-phase reactant sensitive to systemic inflammatory responses and is among the most common inflammation markers used in clinical settings. Serum albumin is also an inflammation-related nutritional biomarker and is known to be a potent prognostic factor [4]. Several previous studies documented that serum CRP and albumin levels were clearly linked to outcomes, and combinations of these metrics can be utilized to predict clinical outcomes in patients with several distinct solid tumors. These factors include the CRP-albumin ratio (CAR) [5], the modified Glasgow prognostic score (mGPS) [6], the Osaka prognostic score (OPS) [7], and the NUn score [8]. However, the association between survival outcomes and these parameters in GC cases has yet to be adequately investigated, in particular regarding disease-specific mortality. Although GC recurrence risk persists far beyond 5 years after surgical resection [9], follow-up periods were not sufficient in previous investigations of cancer-related survivals.
We herein aimed to retrospectively assess the relationships between cancer-specific survival outcomes and preoperative parameters employing combinations of CRP and albumin concentrations (CAR, mGPS, OPS, and NUn score) in patients undergoing radical surgery for GC with long-term surveillance.
Patients and methods
Study population
From a database prospectively constructed by the Department of Gastrointestinal Surgery, the University of Tokyo Hospital, 1880 consecutive patients in total were identified who underwent elective gastrectomy with regional lymphadenectomy for GC between July 1999 and December 2014. Of these, 509 cases were excluded for the following reasons: preoperative chemo-/chemoradio-therapy (n = 98), R1/R2 resection (n = 146), preoperative endoscopic resection (n = 153), synchronous malignant diseases (n = 58), hematological disorders, liver cirrhosis, inflammatory or collagen diseases (n = 21), and/or an insufficient follow-up period (< 6 months) (n = 33). Of the remaining 1371 patients, complete clinicopathological information and preoperative laboratory data, in principle measured within a week before surgery, were available for 1290 (94.1%). These cases were retrospectively investigated and included in the analyses conducted for the present study. This study was carried out in accordance with the Declaration of Helsinki and the ethical guidelines for clinical studies in Japan under approval of the Institutional Review Board at the faculty of medicine at the University of Tokyo (No. 3962).
Clinicopathological data
CAR was calculated by dividing the serum CRP level (mg/L) by the albumin level (g/L), as previously described [5]. Baseline mGPS was determined as follows [6]. Cases with both higher CRP (> 10 mg/L) and hypoalbuminemia (< 35 g/L) were allocated a score of 2. Those with only an elevated CRP (> 10 mg/L) were given a score of 1. Patients without CRP elevation were given a score of 0. The OPS was formulated according to the sum of CRP > 10 mg/L (1 point), albumin < 35 g/L (1 point), and total lymphocyte count < 1600/µL (1 point) [7]. The patients were divided into four groups according to their total scores (0, 1, 2, 3). The NUn score was calculated from the individual values of CRP and albumin, with the white blood cell count (WCC): 11.3894 + 0.005 (CRP [mg/L]) + 0.186 (WCC [/µL]) − 0.174 (albumin [g/L]) [8].
The disease staging was determined as per the eighth edition of the TNM classification by the UICC [10]. Lauren histology definitions were as follows [11]: intestinal type, cohesive tumor cells with gland-like solid structures; diffuse type, non-cohesive scattered tumor cells without cell-to-cell interactions; mixed type, non-homogenous mixtures of intestinal/diffuse type carcinomas. Postoperative complications were defined as those with a grade II or greater according to the Clavien-Dindo classification [12].
All subjects had undergone follow-up surveillance for at least 5 years postoperatively or until death, from any cause, in accordance with the guidelines of the Japanese Gastric Cancer Association [13]. For patients who failed to attend regular outpatient visits, telephone surveys were carried out to determine the tumor relapse and/or survival status. Follow-up of all patients in the current study was completed in August 2023.
Statistical analysis
Statistical analyses were carried out using JMP Pro version 17.0.0 (SAS Institute, Cary, NC, USA) and R version 4.3.2 (R Foundation for Statistical Computing, Vienna, Austria). Statistical analyses were two-tailed and P values < 0.05 were considered to indicate a statistically significant association.
Continuous values were compared using Wilcoxon’s rank-sum test. Categorical variables were compared using the Fisher exact test or the chi-square test, as appropriate. Overall survival (OS) was calculated from date of surgery to the date of death from any cause. Disease-specific survival (DSS) was calculated from the date of surgery to the date of death from primary GC. Survival curves were plotted using the Kaplan–Meier functions with the log-rank test. The factors contributing to survival were identified by means of univariate Cox regression analysis. Multivariate Cox proportional hazards models were used to examine the effects of preoperative indices on OS and DSS after adjusting for known confounders: age at surgery, adjuvant chemotherapy, tumor depth, nodal metastasis, tumor location [14], type of gastrectomy [15], and postoperative complications [16]. Time-dependent receiver operating characteristic curves (ROCs) for the survival estimations based on CAR, mGPS, OPS, and the NUn score were generated using the R package “timeROC” function.
Results
Associations between clinicopathological factors and four preoperative indices
The relationships of the four preoperative indices with clinicopathological features are presented in Table 1. Age at surgery, tumor depth (pT category), nodal metastasis (pN category), lymphatic/venous involvement, and postoperative complications all showed significant correlations with preoperative CAR, mGPS, OPS, and the NUn score.
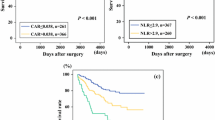
Survival curve analyses
The median follow-up period was 107 months for the survivors in our cohort. To evaluate whether the four preoperative indices reflected the outcomes of our patients, Kaplan–Meier analyses and log-rank tests were carried out. With regard to CAR and the NUn score, the patients were divided into four strata according to the following quartiles: CAR cut-offs 0.010, 0.030, and 0.077; NUn score cut-offs 5.094, 5.550, and 6.097. OS curves are shown in Fig. 1. The survival curves were clearly separated with statistical significance, especially in those of the NUn score (P < 0.001). These findings were similar to those obtained when DSS curves were determined (Fig. 2). The DSS curves correlated highly with the quartiles of the NUn score (P < 0.001).
Time-dependent ROC analyses
The time-dependent ROC curves were constructed, and area under the curve values of each index were chronologically plotted to compare their outcome-predicting performance (Fig. 3). The prognostic relevance of the preoperative NUn score, as regards both OS and DSS, was superior to those of CAR, mGPS, and OPS at all timepoints examined.
Univariate and multivariate Cox regression analyses
Next, we carried out Cox regression analyses for OS and DSS. As the most common inflammatory parameters, prognostic power of preoperative neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) were also alongside examined. In these analyses, mGPS and OPS were treated as categorical variables, while CAR, the NUn score, NLR, and PLR were taken to be continuous values rather than using arbitrary cut-off values [17]. Preoperative CAR, mGPS, OPS, and the NUn score all correlated significantly with both OS and DSS in univariate estimations (Table 2). Subsequent multivariate Cox regression analyses were conducted with adjustment of the model for age (≥ 70 years), main tumor location (upper/middle/lower third), tumor depth (pT1), nodal metastasis (pN0), type of gastrectomy (total gastrectomy), adjuvant chemotherapy, and postoperative complications. To avoid any collinearity issues, we used separate models for each score. In these multivariate analyses, the preoperative NUn score independently predicted OS (hazard ratio [HR] 1.32, 95% confidence interval [CI] 1.16–1.50, per 1-unit increase, P < 0.001) and even DSS (HR 1.23, 95% CI 1.02–1.49, P = 0.032) as well as NLR and PLR (Table 3). Preoperative OPS maintained independence for OS (P = 0.021), but not DSS. Preoperative CAR and mGPS were not independent prognostic factors for OS/DSS in the multivariate assessment.
Discussion
Recent results of large-scale clinical trials have promoted a trend favoring multidisciplinary therapy for GC [18]. Given this situation, tools to screen GC patients who have a high propensity for disease recurrence and subsequent mortality will be necessary to find a cure for this entity. In the current study, we examined the prognostic value of four pre-gastrectomy laboratory data indices, formulated based on routinely available CRP and albumin levels. We ultimately demonstrated the NUn score before surgery to be the most stably involved in OS and even in DSS following curative resection of GC, being superior to the other well-established CRP-albumin–based parameters (CAR, mGPS and OPS) [5,6,7]. Ours is the first study to elucidate the survival relevance of the NUn score measured preoperatively for a specific solid tumor, i.e., GC.
The NUn score, advocated by Noble and Underwood in 2011 [8], is a logistic regression model determined with CRP, WCC, and albumin values. It was originally developed as an easily obtained predictor of anastomotic leakage after esophagectomy. CRP and albumin, along with WCC, are all linked to systemic inflammatory responses resulting from tissue damage. Dvorak suggested a clear relationship between inflammation and tumorigenic processes, insightfully designating tumors as “wounds that do not heal” [19]. Since then, the idea that systemic host responses to neoplasms have parallels with inflammatory status has been widely accepted. Bodies of evidence have suggested the onset and progression of cancer to be in direct relation to inflammatory processes, on the basis of molecular pathophysiological mechanisms such as cytokine release [20]. Accordingly, considerable research has been devoted to reporting the serum levels of inflammatory parameters, represented by CRP and albumin, serving as parameters reflecting the progression of cancers including GC [21]. Albumin, being synthesized in the liver and binding to certain inflammatory factors, can play an immunoregulatory role, along with CRP [22]. The albumin concentration is currently regarded as a supportive proxy measure of the degree of inflammation rather than malnutrition [23]. As to our results, the NUn score system appeared to be a very good combination of systemic inflammatory response parameters for predicting survival, even though this score is relatively difficult to determine as compared with the others. GC patients with impaired NUn scores should be alerted to the possibility of metastasis, independent of the degree of tumor load, and surgery alone may not be sufficient to cure the malignancy in this patient population. Consequently, the NUn score may help oncological care-givers in deciding whether to give priority to neoadjuvant therapy in individuals who are considered to be borderline candidates based on conventional imaging modalities. This score has the potential to guide tailored treatment selections and follow-up strategies (e.g., meticulous monitoring for cases with lower NUn scores) and might thereby ultimately improve survival.
The reason for the NUn score achieving the most substantial impact on OS and DSS among all tested indices was uncertain. We hypothesized that the NUn score is related to the host’s sarcopenic status, which is known to be a key prognostic factor in GC [24], and thus examined the relationship between the NUn score and the skeletal muscle index calculated using pretreatment abdominal computed tomography images. Such data was available for 95 cases in our cohort, and no marked tendency was recognized (data not shown). A plausible explanation for the survival impact of the NUn score has yet to be obtained and this issue merits further exploration.
The present study has limitations. First, its retrospective nature and its single-institution analysis design can produce inherent selection bias. Second, the year of surgery in our eligible cases covered a rather long period (1999–2014) and treatment strategies may thus not have been consistent among the cases. Such differences might have influenced the results even after multivariate adjustments. However, the current analyses were based on a prospectively constructed dataset (n = 1290), and our survival estimations were based on a very long follow-up period of the cohort (median 107 months). As GC can recur far beyond 5 years after radical surgery (over 10 years in stage IIIB/IIIC cases) [9], survival outcome analyses for this entity may well require qualified surveillance information. Our data, supported by the results of long-duration follow-up, may have the potential to serve as a rationale for further research aimed at increasing external validity.
Conclusion
We herein clarified, for the first time, that the preoperative NUn score as a continuous variable independently predicted OS and DSS in cases with resectable GC. The NUn score has potential to distinguish GC patients at oncological risk who require specific management strategies and may facilitate providing optimally tailored therapeutic options.
Data availability
The present data are not available for other studies.
Abbreviations
- CAR:
-
C-reactive protein to albumin ratio
- CRP:
-
C-reactive protein
- DSS:
-
Disease-specific survival
- GC:
-
Gastric cancer
- mGPS:
-
Modified Glasgow prognostic score
- NLR:
-
Neutrophil-to-lymphocyte ratio
- OPS:
-
Osaka prognostic score
- OS:
-
Overall survival
- PLR:
-
Platelet-to-lymphocyte ratio
- ROC:
-
Receiver operating characteristic
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
Morgan E, Arnold M, Camargo MC, Gini A, Kunzmann AT, Matsuda T et al (2022) The current and future incidence and mortality of gastric cancer in 185 countries, 2020–2040: a population-based modelling study. EClinicalMedicine 47:101404
Goetze OT, Al-Batran SE, Chevallay M, Mönig SP (2018) Multimodal treatment in locally advanced gastric cancer. Updates Surg 70(2):173–179
Oñate-Ocaña LF, Aiello-Crocifoglio V, Gallardo-Rincón D, Herrera-Goepfert R, Brom-Valladares R, Carrillo JF et al (2007) Serum albumin as a significant prognostic factor for patients with gastric carcinoma. Ann Surg Oncol 14(2):381–389
Saito H, Kono Y, Murakami Y, Shishido Y, Kuroda H, Matsunaga T et al (2018) Prognostic significance of the preoperative ratio of c-reactive protein to albumin and neutrophil-lymphocyte ratio in gastric cancer patients. World J Surg 42(6):1819–1825
Jiang X, Hiki N, Nunobe S, Kumagai K, Kubota T, Aikou S et al (2012) Prognostic importance of the inflammation-based Glasgow prognostic score in patients with gastric cancer. Br J Cancer 107(2):275–279
Fujino S, Myoshi N, Saso K, Sasaki M, Ishikawa S, Takahashi Y et al (2020) The inflammation-nutrition score supports the prognostic prediction of the TNM stage for colorectal cancer patients after curative resection. Surg Today 50(2):163–170
Noble F, Curtis N, Harris S, Kelly JJ, Bailey IS, Byrne JP et al (2012) Risk assessment using a novel score to predict anastomotic leak and major complications after oesophageal resection. J Gastrointest Surg 16(6):1083–1095
Yago A, Haruta S, Ueno M, Hamada Y, Ogawa Y, Ohkura Y et al (2021) Adequate period of surveillance in each stage for curatively resected gastric cancer: analyzing the time and rates of recurrence. Gastric Cancer 24(3):752–761
Brierley JD, Gospodarowicz MK, Wittekind C (2017) TNM classification of malignant tumours, 8th edn. Wiley-Blackwell, Oxford, UK
Lauren P (1965) The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand 64:31–49
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Japanese Gastric Cancer Association (2021) Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer 24(1):1–21
Kattan MW, Karpeh MS, Mazumdar M, Brennan MF (2003) Postoperative nomogram for disease-specific survival after an R0 resection for gastric carcinoma. J Clin Oncol 21(19):3647–3650
Katai H, Ishikawa T, Akazawa K, Isobe Y, Miyashiro I, Oda I et al (2018) Five-year survival analysis of surgically resected gastric cancer cases in Japan: a retrospective analysis of more than 100,000 patients from the nationwide registry of the Japanese Gastric Cancer Association (2001–2007). Gastric Cancer 21(1):144–154
Kubota T, Hiki N, Sano T, Nomura S, Nunobe S, Kumagai K et al (2014) Prognostic significance of complications after curative surgery for gastric cancer. Ann Surg Oncol 21(3):891–898
Altman DG, Royston P (2006) The cost of dichotomising continuous variables. BMJ 332(7549):1080
Alsina M, Arrazubi V, Diez M, Tabernero J (2023) Current developments in gastric cancer: from molecular profiling to treatment strategy. Nat Rev Gastroenterol Hepatol 20(3):155–170
Dvorak HF (1986) Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N Engl J Med 315(26):1650–1659
McMillan DC (2009) Systemic inflammation, nutritional status and survival in patients with cancer. Curr Opin Clin Nutr Metab Care 12(3):223–226
Yamashita H, Katai H (2010) Systemic inflammatory response in gastric cancer. World J Surg 34(10):2399–2400
Fernández J, Clària J, Amorós A, Aguilar F, Castro M, Casulleras M et al (2019) Effects of albumin treatment on systemic and portal hemodynamics and systemic inflammation in patients with decompensated cirrhosis. Gastroenterology 157(1):149–162
Cederholm T, Jensen GL, Correia M, Gonzalez MC, Fukushima R, Higashiguchi T et al (2019) GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community. J Cachexia Sarcopenia Muscle 10(1):207–217
Kamarajah SK, Bundred J, Tan BHL (2019) Body composition assessment and sarcopenia in patients with gastric cancer: a systematic review and meta-analysis. Gastric Cancer 22(1):10–22
Acknowledgements
We thank Shotaro Aso, MD, MPH, PhD (Department of Real World Evidence, Graduate School of Medicine, The University of Tokyo) for his helpful assistance with the statistical analyses.
Author information
Authors and Affiliations
Contributions
Study conception and design: M. Urabe. Acquisition of data: all authors. Analysis and interpretation of data: M. Urabe and Y. Okumura. Drafting of manuscript: all authors. Critical revision: K. Yagi, H. Yamashita, and Y. Seto.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Urabe, M., Okumura, Y., Okamoto, A. et al. Preoperative NUn score serves as a robust predictor of overall and disease-specific survivals following radical surgery for gastric cancer. Langenbecks Arch Surg 409, 126 (2024). https://doi.org/10.1007/s00423-024-03317-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-024-03317-9