Abstract
Purpose
The search for the optimal procedure for creation of a safe gastroesophageal intrathoracic anastomosis with a lower risk of leakage in totally minimally invasive Ivor–Lewis esophagectomy (TMIIL) is ongoing. In the present study, we compared the outcomes of end-to-side (with circular stapler [CS]) and side-to-side (with linear stapler [LS]) techniques for intrathoracic anastomosis during TMIIL performed in 2 European high-volume centers for upper gastrointestinal surgery. A propensity score method was used to compare the CS and LS groups.
Methods
We retrospectively evaluated patients with lower esophageal cancer or Siewert type 1 or 2 esophagogastric junction carcinoma who underwent a planned TMIIL esophagectomy, performed from January 2017 to September 2020. The anastomosis was created by a semi-mechanical technique using a LS in one center and by a mechanical technique using a CS in the other center. General features, operative techniques, pathology data, and short-term outcomes were analyzed. Statistical evaluations were performed on the whole cohort, stratifying the analyses by risk strata factors identified with the propensity scores, and on a subgroup of patients matched by propensity score. The primary endpoint of the study was the rate of anastomotic leakage in the two groups. Secondary endpoints included rates of anastomotic stricture and overall postoperative complications.
Results
Considering the whole population, 256 patients were included; of those, 220 received the anastomosis with a circular stapler (CS group), and 36 received the anastomosis with a linear stapler (LS group). No significant differences by group in terms of sex, age, American Society of Anesthesiologists physical status classification, and type of neoplasm were showed. The rate of anastomotic leakage did not differ in the two groups (9.6% CS vs. 5.6% LS, p = 0.438), as well as the rate of anastomotic stricture in the 3-month follow-up (0.9% CS vs. 2.8% LS, p = 0.367). The rate of chyle leakage and of pulmonary, cardiac, and infective complications was not significantly different in the groups. After propensity score matching, 72 patients were included in the analysis. The 2 obtained propensity score matched groups did not differ for any of the clinical and pathologic variables considered for the analysis, resulting in well-balanced cohorts. The results obtained on the whole population were confirmed in the matched groups.
Conclusions
The results of our study suggest that both techniques for esophagogastric anastomosis during TMIIL are feasible, safe, and effective, with comparable rates of postoperative anastomotic leakage and stricture.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Esophageal resection remains an essential step in the curative management of patients with locally advanced esophageal cancer. Ivor–Lewis esophagectomy is an accepted technique for disease located in the distal esophagus and gastroesophageal junction [1, 2]. Compared with an open approach, totally minimally invasive (laparoscopy and thoracoscopy) Ivor–Lewis (TMIIL) has increased in popularity, resulting in a lower rate of postoperative complications (particularly pulmonary infections), a decreased length of hospital stay, and improved quality of life [3–6]. Nevertheless, outcomes have sometimes been discordant, particularly with respect to the incidence of anastomotic leakage (AL), one of the most severe complications [7].
Even though the causes of AL are multifactorial, the long proficiency gain curve for minimally invasive esophagectomy is a crucial factor in AL development, especially at intrathoracic anastomoses [8]. Indeed, performing an intrathoracic gastroesophageal anastomosis in TMIIL is technically challenging, and no detailed, standardized technique has yet been generally accepted. Various techniques have been developed and are currently used for the construction of the esophagogastric anastomosis. These anastomotic techniques are basically divided into hand-sewn, mechanical, and semi-mechanical, the last two of which involve the use of a stapler. The stapling techniques use either a linear or circular stapler, and a circular stapler can be used either in combination with an anvil inserted via the mouth or the thorax. The stapling techniques have been extensively reported in the literature, in contrast to the hand-sewn anastomosis (less commonly adopted) [9, 10]. A common goal of all techniques is the creation of a safe anastomosis, reducing the risk of leakage and related complications. Nevertheless, the ideal manner in which to construct the anastomosis remains uncertain, given that no decisive evidence exists to recommend one technique over another [9]. Consequently, the choice of technique is based on surgeon preference.
Circular (CS) and linear stapled (LS) are the two most commonly used anastomotic techniques [11, 12]. Major technical difficulties are related to the hand-suturing of the anterior aspect of the anastomosis in LS and the complexity of performing the purse-string suture fixing the anvil in CS [13–16]. Dedicated studies directly comparing the CS and LS techniques are limited and have discordant results. Compared with CS, LS seems to reduce the stricture rate; the AL incidence seems not to differ [17–19].
The aim of the present study was to retrospectively compare outcomes of the LS and CS techniques for patients undergoing TMIIL esophagectomy for esophageal or esophagogastric junction malignancies at 2 high-volume European centers for upper gastrointestinal surgery.
Materials and methods
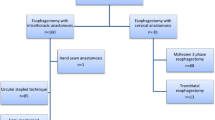
From January 2017 to September 2020, patients with lower esophageal cancer or Siewert type 1 or 2 esophagogastric junction carcinoma who underwent a planned TMIIL esophagectomy at 2 surgical centers—the Amsterdam University Medical Centers (UMC), Amsterdam, and the European Institute of Oncology (IEO), Milan—were retrospectively evaluated. Both institutions are considered high-volume centers, performing more than 20 esophagectomies per year (hybrid, minimally invasive or open, both Ivor–Lewis and McKeown procedures). The staff surgeons in the 2 Centers have an extensive experience in esophageal surgery with more than 500 esophagectomies performed during their working activity. For the group in IEO, TMIIL represent 33% of the total number of total or subtotal esophagectomies performed with an yearly volume of about 50 esophagectomies, while TMIIL is the standard approach in the Amsterdam UMC that boasts about 90 esophagectomies a year. The centers each used a different technique to perform the gastroesophageal intrathoracic anastomosis, with the respective technique being the standard at their center. The IEO group used a linear stapler to create a side-to-side semi-mechanical anastomosis, while the Amsterdam UMC group used a mechanical technique with circular stapler to perform an endo-to-side anastomosis. All operations were performed by senior surgeons experienced in minimally invasive esophagectomy.
Inclusion criteria were lower esophageal cancer or Siewert type 1 or 2 esophagogastric junction carcinoma. Exclusion criteria were conversion to an open approach, if the anastomosis was performed differently than it would have been with the minimally invasive approach, or use of an esophagojejunal or esophagocolic anastomosis or neck anastomoses. Moreover, at the IEO, other exclusion criteria were previous major abdominal or thoracic surgery and bulky tumors.
Data and outcomes for all patients were considered. The data collected included demographic characteristics, comorbidities, preoperative staging, neoadjuvant treatment, intraoperative details, postoperative outcomes and complications, length of hospital stay and mortality, readmission rate, and short-term oncologic outcome.
The primary endpoint of the study was the rate of anastomotic leakages in the two groups.
The diagnosis of AL was based on CT scan and/or upper GI endoscopy which were performed in case of suspicion of a leak, based on clinical symptoms, routine laboratory tests, and/or chest X-ray. Secondary endpoints included anastomotic stricture (AS) within 3 months of surgery, overall complication rates, length of stay, and 90-day all-cause mortality. AS was defined as a narrowing at the level of the esophageal anastomosis, causing clinically significant functional impairment and dysphagia, detected by endoscopy and/or barium esophagram performed on demand only in symptomatic patient, that required endoscopic dilatation. Postoperative complications were graded according to both the Esophagectomy Complications Consensus Group (ECCG) and Clavien–Dindo classifications. The comprehensive complication index was also calculated. Hospital stay was calculated from the date of surgery to the date of discharge. Readmission and mortality were recorded for the first 90 days after surgery. The study was approved by both institutional review boards because no patient-identifying information was used.
Anastomotic techniques and perioperative protocols
Linear anastomoses were performed at the IEO as previously described [20]. Briefly, after a 45-mm linear stapler is used to transect the esophagus above the level of the azygos vein, a corner of that suture is removed. Two full-thickness (adventitia to mucosa) stitches are placed anteriorly and posteriorly in the esophageal wall to prevent esophageal mucosal retraction (technique described by Irino et al. [21]). A small gastrotomy is made on the anterior wall of the gastric tube approximately 5 cm away from the top of the conduit. The esophagogastric side-to-side anastomosis is performed using a 30-mm linear stapler with a medium-thick cartridge. The enterotomies are closed with hand-sewn sutures using both a corner stitch made with monofilament absorbable suture and a running self-gripping barbed suture. Care is taken to accurately include the esophageal mucosa in every pass of the suture. A leak test is performed with methylene blue. An omental wrap is performed (Fig. 1).
Execution of side-to-side linear stapled esophagogastric anastomosis. a, b After transecting the esophagus at the level of the azygos vein and removing a corner of the staple line on the esophageal stump (a), the naso-gastric tube is pushed through this small esophagotomy to accurately identify the opening (b). Placement of two stitches anteriorly and posteriorly in the esophageal wall (b). c Completion of the gastric tube by dividing the bridge between the conduit and the specimen. d Performing a small gastrostomy on the anterior wall of the gastric tube. e Introduction of a 30-mm linear stapler into the esophageal stump and gastric conduit, removing the naso-gastric tube and closure of the stapler. f Closure of the enterotomies by hand-sewn sutures
At the Amsterdam UMC, circular anastomoses were performed. After using a diathermic hook to transect the esophagus, the anvil is secured with a purse-string suture made using the Endo Stitch (Medtronic, Minneapolis, MN, USA). The circular stapler of diameter of 29 mm is introduced into the gastric tube, with the tip of the stapler emerging at the mesenteric side of the gastric tube, after which the two stapler parts are aligned and the stapler is fired. A linear stapler is then used to close the open end of the gastric tube. The anastomosis is oversewn with 2 sutures, and the tip of the gastric tube is fixated to the pleural flap, so that the weight is taken off the circular anastomosis. Finally, an omentoplasty is wrapped around the anastomosis [22] (Fig. 2).
Execution of end-to-side circular stapled esophagogastric anastomosis. a After transecting the esophagus at the level of the azygos vein, performing the purse-string using the Endo Stitch TM. b, c Securing the anvil with the purse-string suture performed. d Introduction the circular stapler (29 mm diameter) in the gastric tube, with the tip of the stapler coming out at the mesenteric side of the gastric tube. The two stapler parts are aligned and the stapler is fired. e Closing the open end of the gastric tube with a linear stapler
With respect to perioperative care, similar ERAS protocols [23] were routinely applied in both centers.
Statistical analysis
Descriptive statistics with frequencies and median values with interquartile ranges are presented to describe baseline tumor characteristics and treatments in the LS and CS cohorts. Other categorical variables are reported as frequencies with percentages, and continuous variables as medians with interquartile range (25th–75th percentiles). Differences between the two cohorts were evaluated using chi-squared tests for categorical variables and Wilcoxon rank tests for continuous variables. To make a comparison between treatment groups, we calculated a propensity score using multivariate logistic models. One-to-one basis matching was based on nearest-neighbor criteria.
Statistical analyses were performed on the whole cohort, stratifying the analyses by risk strata identified with the propensity scores, and for the subgroup of patients matched by propensity score. The first analysis can count on a large sample size that allows a greater statistical power, whereas the second has the advantage of 2 balanced cohorts in terms of confounding factors.
Statistical analyses were performed using the SAS statistical software (version 9.4 for Windows) and R (version 3.4.3). Two-sided p values are also presented.
Results
From January 2017 to September 2020, 256 patients at the two centers underwent TMIIL esophagectomy for lower esophageal or gastroesophageal junction cancer. Of those 256 patients, 220 at Amsterdam UMC received a mechanical anastomosis with a circular stapler (CS group), and 36 at IEO received a semi-mechanical anastomosis with a linear stapler (LS group). After propensity score matching, these numbers were reduced to 36 patients in each group. Data from the prospectively maintained database at both Centers were retrospectively analyzed. Table 1 presents the baseline characteristics of the whole cohort. No significant differences between the groups in terms of sex, age, American Society of Anesthesiologists physical status classification, and neoplasm types were identified. Median body mass index was in the healthy range (23 kg/m2) in the LS group, while in the CS group, it fell into the overweight range (26 kg/m2) (p = 0.002). Different preoperative therapies were used in the two groups. Most patients in the IEO group with adenocarcinoma were treated with chemotherapy (11 chemotherapy vs. 7 chemoradiotherapy); those in the Amsterdam UMC group were mostly treated with chemoradiotherapy (156 chemoradiotherapy vs. 15 chemotherapy). In both groups, all patients with squamous cell carcinoma received chemoradiotherapy, with the exception of 1 psychiatric case in the IEO group and 2 stage I cases in the Amsterdam UMC group.
All prognostic factors were well balanced in the matched subgroup (Table 2).
Table 3 provides an overview of the operative data. Median estimated intraoperative blood loss was 200 mL in the CS group (range: 40–850 mL) and 100 mL in the LS group (range: 50–1000 mL), p = 0.0009. All patients in the whole cohort received extended mediastinal lymphadenectomy, except a minority of patients in the LS group that received a standard mediastinal dissection (p = 0.0001). No intraoperative mortality was observed in either group.
Tables 4 and 5 show postoperative complications and short-term outcomes respectively. Length of hospital stay, 90-day mortality, rate of readmission within 30 days, and postoperative complications were not statistically different between the groups. According to the ECCG classification, 23 cases of AL were recorded in the series, 21 in the CS group (9.6%), and 2 in the LS group (5.6%), without significant statistical heterogeneity (p = 0.438). Of the 21 patients experiencing AL in the CS group, 9 required a wash-and-drain re-intervention after an endoluminal vacuum therapy device had been positioned endoscopically, 11 received only endoscopic treatment (6, with a self-expandable esophageal stent and radiologic positioning of a drain; 5, with the use of an endoluminal vacuum therapy device), and 1 was managed conservatively. Both cases of AL in the LS group were treated endoscopically with a self-expandable esophageal stent after a 1-week course of treatment with an endoluminal vacuum therapy device. Length of hospital stay in cases with leakages was similar (on average, 39 days [CS] vs. 40 days [LS]). The rate of anastomotic stricture (AS) at the 3-month follow-up did not differ significantly (LS: 2.8% [n = 1] vs. CS: 0.9% [n = 2], p = 0.367). All cases of AS were diagnosed and treated with endoscopic dilation. None of those patients had experienced an AL. Chyle leak developed in 26 patients (11.8%) in the CS group and in 5 patients (13.9%) in the LS group (p = 0.786).
Other complications were also not statistically different in the two groups.
Using the comprehensive complication index, median values for complications were 26.2 in the CS group and 27.9 in the LS group (both ranging from 20.9 to 100, p = 0.527, Table 6).
Median hospital stay was 13 days in the LS group (7–64 days) and 10 days in the CS group (6–125 days), p = 0.076. The readmission rate was 10.3% (n = 4) in the IEO group and 14.8% (n = 34) in the Amsterdam UMC group (p = 0.538). In the Amsterdam UMC group, 3 patients died within 30 days of surgery. No statistical difference in the 90-day mortality rate was found (CS, 2.3%; LS, 2.8%).
Results derived on the whole cohort, stratifying the analyses by risk strata factors identified with the propensity scores, were confirmed also by the analysis on the 2 matched subgroups (Table 7).
Discussion
Ivor–Lewis esophagectomy is a complex surgical procedure, with associated high rates of postoperative complications and morbidities. In recent years, TMIIL has been gradually gaining favor among surgeons and was recommended as the preferred approach in several international registry analyses, given that it minimizes surgical trauma, reduces postoperative complications (particularly pulmonary infections and blood loss), and possibly even improves long-term survival [3–5, 24–27]. Nevertheless, AL remains a severe complication associated with esophagectomy, leading to significant morbidity, prolonged hospital stay, considerable use of healthcare resources, and increased risk of mortality [28]. Identification of risk factors for AL is of critical importance for prevention and treatment, as well as for pre- and postoperative optimization. Some of the risk factors are modifiable and, consequently, may guide a patient-tailored management of pre-, peri-, and postoperative strategies. Nevertheless, no overall agreement has been reached on which of them are the most decisive in AL development, leading to the lack of reliable predictive models and tools for a standardized preoperative risk assessment. Occurrence of an anastomotic leak depends on several factors all included in the multidisciplinary perioperative management of these patients, including nutritional surgical and anesthesiological factors. Most of these variables have been standardized in high-volume centers taking care of these patients; the technique for minimally invasive esophagogastric anastomosis has also been standardized within the single high-volume centers even if comparative evidence concerning the effect of the various techniques on the development of AL (or other anastomotic complications) is still scant. A range of options is currently available for intrathoracic anastomosis reconstruction: manual, mechanical, and semi-mechanical. None of those options can be considered a reference “standard.” In order to try to improve the knowledge about the results of different anastomotic techniques for esophagogastric anastomosis, we compared the series of totally minimally invasive Ivor–Lewis performed in 2 high-volume European centers, each of them using a different but standardized clinical pathway, and using a different technique. Standardization of the perioperative management may reduce the influence of nonsurgical factors and differences in anastomotic technique may become more important to explain different results.
In this retrospective 2-center study, the main clinical outcomes after end-to-side CS and side-to-side LS esophagogastric anastomosis during TMIIL were compared, with a particular focus on the rates of AL and AS. Each technique has its own pros and cons. The linear stapler is easy to insert into the esophageal stump and allows for the creation of an enlarged anastomotic caliber. However, the technique requires experience with hand-sewn suturing to complete the anterior anastomotic wall. Furthermore, the need for longer visceral segments to achieve alignment for the anastomosis is a major limitation, making the LS technique poorly adapted for creating an anastomosis at the apex of the thoracic cavity. And in case of the need for a redo anastomosis, LS necessitates a longer esophageal resection.
The CS technique avoids manual suturing, although the construction and tying of the purse-string suture to fix the anvil is technically demanding. Moreover, the caliber of the anastomosis is smaller.
In our trial, the incidence of leakages in LS group (5.6%) was not statistically different from the incidence in the CS group (9.6%, p = 0.438). The lower incidence of anastomotic leaks in the LS group may be explained by the low number of included cases in comparison to the more stable number of leaks in the CS group. An incidence of anastomotic leaks around 10% both for LS and CS is the incidence reported by the authors at IEO center in a group of 50 patients submitted to TMIIL (unpublished results), a percentage that can be considered stable and expected when compared to the literature. Beyond that, it should be considered that patients treated at Amsterdam UMC were treated with chemoradiotherapy whereas patients treated at IEO received chemotherapy. This difference may represent a reason for a higher (though not statistically significant) incidence of anastomotic leaks in CS group [7]. Notwithstanding the unbalanced sample (36 patients at the IEO and 220 patients at Amsterdam UMC), the outcomes accord with those reported in several other studies that compared the two anastomotic techniques (summarized in Table 8). The literature survey indicates an AL incidence ranging from 0 to 15.6% in the LS group and from 1.5 to 15.3% in the CS group, without a statistically significant difference, except in Yanni et al. [31], who reported a reduction of the AL incidence in the LS group (4.1% vs. 15.3%). In contrast, the data for AS were discordant, with the range varying from 0 to 9.1% in LS group and from 9.4 to 31.2% in the CS group, and a significantly higher incidence being reported in the CS group in some studies [17–19]. In our study, the incidence of AS was not significantly different in the two groups (LS, 2.8% vs. CS, 0.9%).
Literature comparing the various surgical techniques for Ivor–Lewis esophagectomy is scarce and reports mostly the outcomes of the open approach. Our study and two recent trials [30, 32] are the only reports dealing with the minimally invasive approach, in which the anastomosis is probably more difficult to perform. Nevertheless, outcomes in our trial are comparable to those reported for open surgery, in contrast with the presumed higher AL incidence found with the mini-invasive approach [33] That observation is probably consistent with the experiences completed before arriving at a single standardized technique for each surgical center [34]. The details for performing this anastomosis are an important determinant of good results, and standardization of the technique is of the utmost importance.
We compared two different techniques that had each been adopted at one center as the reference technique. Our comparison is different from others reported in the literature, where, in single-center studies, the two techniques were used at the surgeon’s discretion without a reference standard technique. Achieving dexterity in the performance of a minimally invasive intrathoracic anastomosis requires a long learning process (as demonstrated by Van Workum et al. [35]). Not uncommonly, surgeons change or modify their initial technique until they identify the most suitable one—that is, the one in which they have reached a certain degree of experience and technical confidence [34]. Becoming familiar with a surgical technique, rather than putative differences in its performance, seems to be a major determinant of the learning curve. Some studies have emphasized the benefit of structured training and mentorship programs for minimally invasive surgery [36]. In our study, the 2 participating centers have reached a high level of proficiency in their respective anastomotic techniques [20, 37], ensuring minimization of learning-associated bias (a major confounding factor in esophagogastric anastomosis studies). As in our study, the multicenter trial by Schröder et al. [30
Limitations
The limitations of the present study are its retrospective, non-randomized character and the different number of patients in the two groups. In part, that difference stems from the fact that, at the IEO, many patients are still treated with a hybrid technique, which is considered elective in the case of bulky tumors or a long operative time in the abdominal phase of the operation. At the Amsterdam UMC, all patients are generally treated with a minimally invasive technique. The sample size is low and this implies low statistical power. We used Fisher exact test and propensity score strata in the whole cohort and in the matched subgroup in order to take into account of unbalances between the two groups and issues due to low frequencies.
Conclusions
Both techniques, LS and CS, for the performance of a minimally invasive esophagogastric anastomosis are safe and effective, producing comparably good clinical results. Details of the surgeries as derived from the surgeons’ experience have to be followed to achieve these results.
Leakages at this anastomotic site do not depend directly on the anastomotic technique, but are determined by many factors such as peri- and intraoperative care, whose influence depends on the experience of the surgical center.
Data availability
The datasets generated during the study are available from the corresponding author on reasonable request.
References
Pennathur A, Zhang J, Chen H, Luketich JD (2010) The “best operation” for esophageal cancer? Ann Thorac Surg 89(6):S2163–S2167
Van Workum F, Berkelmans GH, Klarenbeek BR, Nieuwenhuijzen GAP, Luyer MDP, Rosman C (2017) McKeown or Ivor Lewis totally minimally invasive esophagectomy for cancer of the esophagus and gastroesophageal junction: systematic review and meta-analysis. J Thorac Dis 9(Suppl 8):S826–S833
Biere SS, van Berge Henegouwen MI, Maas KW, Bonavina L, Rosman C, Garcia JR, Gisbertz SS, Klinkenbijl JH, Hollmann MW, de Lange ES, Bonjer HJ, van der Peet DL, Cuesta MA (2012) Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 379:1887–1892
Sihag S, Wright CD, Wain JC, Gaissert HA, Lanuti M, Allan JS, Mathisen DJ, Morse CR (2012) Comparison of perioperative outcomes following open versus minimally invasive Ivor Lewis oesophagectomy at a single, high-volume centre. Eur J Cardiothorac Surg 42(3):430–437
Lv L, Hu W, Ren Y, Wei X (2016) Minimally invasive esophagectomy versus open esophagectomy for esophageal cancer: a meta-analysis. Onco Targets Ther 31(9):6751–6762
van der Sluis PC, Schizas D, Liakakos T, van Hillegersberg R (2020) Minimally invasive esophagectomy. Dig Surg 37(2):93–100
Fabbi M, Hagens ERC, van Berge Henegouwen MI, Gisbertz SS (2021) Anastomotic leakage after esophagectomy for esophageal cancer: definitions, diagnostics, and treatment. Dis Esophagus 34(1):doaa039
Gisbertz SS, Hagens ERC, Ruurda JP, Schneider PM, Tan LJ, Domrachev SA, Hoeppner J, van Berge Henegouwen MI (2018) The evolution of surgical approach for esophageal cancer. Ann N Y Acad Sci 1434(1):149–155
Carr RA, Molena D (2021) Minimally invasive esophagectomy: anastomotic techniques. Ann Esophagus 4:19
Bonavina L, Asti E, Sironi A, Bernardi D, Aiolfi A (2017) Hybrid and total minimally invasive esophagectomy: how I do it. J Thorac Dis 9(Suppl 8):S761–S772
Kamarajah SK, Bundred JR, Singh P, Pasquali S, Griffiths EA (2020) Anastomotic techniques for oesophagectomy for malignancy: systematic review and network meta-analysis. BJS Open 4(4):563–576
Nickel F, Probst P, Studier-Fischer A et al (2021) Minimally invasive versus open abdominothoracic esophagectomy for esophageal carcinoma (MIVATE) - study protocol for a randomized controlled trial DRKS00016773. Trials 22(1):41. Published 2021 Jan 11. https://doi.org/10.1186/s13063-020-04966-z
Misawa K, Hachisuka T, Kuno Y, Mori T, Shinohara M, Miyauchi M (2005) New procedure for purse-string suture in thoracoscopic esophagectomy with intrathoracic anastomosis. Surg Endosc 19(1):40–42
Nguyen NT, Longoria M, Chang K, Lee J, Wilson SE (2006) Thoracolaparoscopic modification of the Ivor Lewis esophagogastrectomy. J Gastrointest Surg 10(3):450–454
Thairu N, Biswas S, Abdulaal Y, Ali H (2007) A new method for intrathoracic anastomosis in laparoscopic esophagectomy. Surg Endosc 21(10):1887–1890
Usui S, Nagai K, Hiranuma S, Takiguchi N, Matsumoto A, Sanada K (2008) Laparoscopy-assisted esophagoenteral anastomosis using endoscopic purse-string suture instrument “Endo-PSI (II)” and circular stapler. Gastric Cancer 11:233–237
Xu QR, Wang KN, Wang WP, Zhang K, Chen LQ (2011) Linear stapled esophagogastrostomy is more effective than hand-sewn or circular stapler in prevention of anastomotic stricture: a comparative clinical study. J Gastrointest Surg 15:915–921
Price TN, Nichols FC, Harmsen WS, Allen MS, Cassivi SD, Wigle DA, Shen KR, Deschamps C (2013) A comprehensive review of anastomotic technique in 432 esophagectomies. Ann Thorac Surg 95(4):1154–60; discussion 1160-1
Wang WP, Gao Q, Wang KN, Shi H, Chen LQ (2013) A prospective randomized controlled trial of semi-mechanical versus hand-sewn or circular stapled esophagogastrostomy for prevention of anastomotic stricture. World J Surg 37(5):1043–1050
Fabbi M, De Pascale S, Ascari F, Petz WL, Fumagalli RU (2021) Side-to-side esophagogastric anastomosis for minimally invasive Ivor-Lewis esophagectomy: operative technique and short-term outcomes. Updates Surg 73(5):1837–1847
Irino T, Tsai JA, Ericson J, Nilsson M, Lundell L, Rouvelas I (2016) Thoracoscopic side-to-side esophagogastrostomy by use of linear stapler-a simplified technique facilitating a minimally invasive Ivor-Lewis operation. Langenbecks Arch Surg 401(3):315–322
Maas KW, Biere SS, Scheepers JJ, Gisbertz SS, Turrado Rodriguez VT, van der Peet DL, Cuesta MA (2012) Minimally invasive intrathoracic anastomosis after Ivor Lewis esophagectomy for cancer: a review of transoral or transthoracic use of staplers. Surg Endosc 26(7):1795–1802
Low DE, Allum W, De Manzoni G, Ferri L, Immanuel A, Kuppusamy M, Law S, Lindblad M, Maynard N, Neal J, Pramesh CS, Scott M, Mark Smithers B, Addor V, Ljungqvist O (2019) Guidelines for perioperative care in esophagectomy: enhanced recovery after surgery (ERAS®) Society Recommendations. World J Surg 43(2):299–330
Low DE, Kuppusamy MK, Alderson D, Cecconello I, Chang AC, Darling G, Davies A, D’Journo XB, Gisbertz SS, Griffin SM, Hardwick R, Hoelscher A, Hofstetter W, Jobe B, Kitagawa Y, Law S, Mariette C, Maynard N, Morse CR, Nafteux P, Pera M, Pramesh CS, Puig S, Reynolds JV, Schroeder W, Smithers M, Wijnhoven BPL (2019) Benchmarking complications associated with esophagectomy. Ann Surg 269(2):291–298
Schmidt HM, Gisbertz SS, Moons J, Rouvelas I, Kauppi J, Brown A, Asti E, Luyer M, Lagarde SM, Berlth F, Philippron A, Bruns C, Hölscher A, Schneider PM, Raptis DA, van Berge Henegouwen MI, Nafteux P, Nilsson M, Räsanen J, Palazzo F, Rosato E, Mercer S, Bonavina L, Nieuwenhuijzen G, Wijnhoven BPL, Schröder W, Pattyn P, Grimminger PP, Gutschow CA (2017) Defining benchmarks for transthoracic esophagectomy: a multicenter analysis of total minimally invasive esophagectomy in low risk patients. Ann Surg 266(5):814–821
Haverkamp L, Seesing MF, Ruurda JP, Boone J, Hillegersberg V, R, (2017) Worldwide trends in surgical techniques in the treatment of esophageal and gastroesophageal junction cancer. Dis Esophagus 30(1):1–7
Straatman J, van der Wielen N, Cuesta MA, Daams F, Roig Garcia J, Bonavina L, Rosman C, van Berge Henegouwen MI, Gisbertz SS, van der Peet DL (2017) Minimally invasive versus open esophageal resection: three-year follow-up of the previously reported randomized controlled trial: the TIME trial. Ann Surg 266(2):232–236
Kassis ES, Kosinski AS, Ross P Jr, Koppes KE, Donahue JM, Daniel VC (2013) Predictors of anastomotic leak after esophagectomy: an analysis of the society of thoracic surgeons general thoracic database. Ann Thorac Surg 96(6):1919–1926
Blackmon SH, Correa AM, Wynn B, Hofstetter WL, Martin LW, Mehran RJ, Rice DC, Swisher SG, Walsh GL, Roth JA, Vaporciyan AA (2007) Propensity-matched analysis of three techniques for intrathoracic esophagogastric anastomosis. Ann Thorac Surg 83(5):1805–1813; discussion 1813
Schröder W, Raptis DA, Schmidt HM, Gisbertz SS, Moons J, Asti E, Luyer MDP, Hölscher AH, Schneider PM, van Berge Henegouwen MI, Nafteux P, Nilsson M, Räsanen J, Palazzo F, Mercer S, Bonavina L, Nieuwenhuijzen GAP, Wijjnhoven BPL, Pattyn P, Grimminger PP, Bruns CJ, Gutschow CA (2019) Anastomotic techniques and associated morbidity in total minimally invasive transthoracic esophagectomy: results from the EsoBenchmark database. Ann Surg 270(5):820–826
Yanni F, Singh P, Tewari N, Parsons SL, Catton JA, Duffy J, Welch NT, Vohra RS (2019) Comparison of outcomes with semi-mechanical and circular stapled intrathoracic esophagogastric anastomosis following esophagectomy. World J Surg 43(10):2483–2489
Zhang H, Wang Z, Zheng Y, Geng Y, Wang F, Chen LQ, Wang Y (2019) Robotic side-to-side and end-to-side stapled esophagogastric anastomosis of ivor lewis esophagectomy for cancer. World J Surg 43(12):3074–3082
Fumagalli U, Baiocchi GL, Celotti A, Parise P, Cossu A, Bonavina L, Bernardi D, de Manzoni G, Weindelmayer J, Verlato G, Santi S, Pallabazzer G, Portolani N, Degiuli M, Reddavid R, de Pascale S (2019) Incidence and treatment of mediastinal leakage after esophagectomy: Insights from the multicenter study on mediastinal leaks. World J Gastroenterol 25(3):356–366
Mungo B, Lidor AO, Stem M, Molena D (2016) Early experience and lessons learned in a new minimally invasive esophagectomy program. Surg Endosc 30(4):1692–1698
van Workum F, Stenstra MHBC, Berkelmans GHK, Slaman AE, van Berge Henegouwen MI, Gisbertz SS, van den Wildenberg FJH, Polat F, Irino T, Nilsson M, Nieuwenhuijzen GAP, Luyer MD, Adang EM, Hannink G, Rovers MM, Rosman C (2019) Learning curve and associated morbidity of minimally invasive esophagectomy: a retrospective multicenter study. Ann Surg 269(1):88–94
Visser E, van Rossum PSN, van Veer H, Al-Naimi K, Chaudry MA, Cuesta MA, Gisbertz SS, Gutschow CA, Hölscher AH, Luyer MDP, Mariette C, Moorthy K, Nieuwenhuijzen GAP, Nilsson M, Räsänen JV, Schneider PM, Schröder W, Cheong E, van Hillegersberg R (2018) A structured training program for minimally invasive esophagectomy for esophageal cancer- a Delphi consensus study in Europe. Dis Esophagus 31(3). https://doi.org/10.1093/dote/dox124
Straatman J, Van der Wielen N, Nieuwenhuijzen GAP, Rosman C, Roig J, Scheepers JJG, Cuesta MA, Luyer MDP, van Berge Henegouwen MI, van Workum F, Gisbertz SS, van der Peet DL (2017) Techniques and short-term outcomes for total minimally invasive Ivor Lewis esophageal resection in distal esophageal and gastroesophageal junction cancers: pooled data from six European centers. Surg Endosc 31(1):119–126
Author information
Authors and Affiliations
Contributions
All the authors listed above contributed substantially to the conception or design of the work and the acquisition, analysis, or interpretation of data for the work; and all the authors contributed to the drafting of the work or revising it critically for important intellectual content and the final approval of the version to be published; and all the authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval
All the procedures described in this study were in accordance with the ethical standards of the internal review board and with the 1964 Helsinki Declaration.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fabbi, M., van Berge Henegouwen, M.I., Fumagalli Romario, U. et al. End-to-side circular stapled versus side-to-side linear stapled intrathoracic esophagogastric anastomosis following minimally invasive Ivor–Lewis esophagectomy: comparison of short-term outcomes. Langenbecks Arch Surg 407, 2681–2692 (2022). https://doi.org/10.1007/s00423-022-02567-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02567-9