Abstract
Purpose
Gastric cancer after pancreaticoduodenectomy was firstly reported in 1995, and the number of reports about this topic has increased in the past years. This review aimed to elucidate the clinicopathological features of this disease.
Methods
Data for 32 cases were obtained using literature search, and three cases in our institution were added.
Results
Twenty cases were reported from Japan, and fifteen cases were from the Western countries (Germany: 1 case, France: 2 cases, USA: 12 cases). In Japanese and the Western cases, the most dominant indication for pancreaticoduodenectomy was distal bile duct cancer and pancreatic ductal adenocarcinoma, respectively. The most frequently applied procedure of pancreaticoduodenectomy was pylorus-preserving pancreatoduodenectomy with pancreaticogastrostomy and pancreaticoduodenectomy with pancreaticojejunostomy, respectively. The median length of time interval from pancreaticoduodenectomy to GC detection tended to be shorter in the Japanese cases (61.5 months vs. 115 months). Of all cases, thirteen (37.1%) patients with gastric cancer showed no abdominal symptoms, and eight were diagnosed at regular gastroscopy. Surgical gastrectomy was performed in 30 patients, and among them, concomitant pancreatectomy was performed in six patients. Four patients received reanastomosis of remnant pancreas using pancreaticojejunostomy. Twenty-two (73.3%) patients had undifferentiated carcinomas, and stage 1, 2, 3, and 4 cancer was identified in 14, six, six, and four patients, respectively. All eight patients who had received routine gastroscopy were T1N0M0 stage 1.
Conclusion
Gastric cancers after pancreaticoduodenectomy including newly reported Japanese cases and our institutional cases were reviewed to make Japanese studies available to a broader scientific audience. Further investigation is necessary to elucidate the most important carcinogens among the various potential local and systemic factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreaticoduodenectomy (PD) is one of the most complex procedures in abdominal surgery. Recently, better management has resulted in decreased postoperative mortality [1], and the survival period after pancreaticoduodenectomy for pancreatic ductal adenocarcinoma (PDAC) and periampullary malignancies has improved due to better neoadjuvant and adjuvant treatments [2,3,4]. Furthermore, pancreaticoduodenectomy has been more frequently performed due to the increasing prevalence of PDAC and expanded adaptation for benign and potentially malignant disease [1]. Consequently, patients have a longer survival time following pancreaticoduodenectomy, which increases the likelihood of these patients to develop a secondary malignancy over the course of their remaining lifetime.
Among the secondary malignancies following pancreaticoduodenectomy, we focused on investigating gastric cancer (GC) [5,6,7]. The number of previous reports on GC following pancreaticoduodenectomy is limited, and it may be due to several reasons such as loss to follow-up after pancreaticoduodenectomy, not appreciating the GC as an independent new malignancy, or unawareness of the patient’s previous history of pancreatic surgery. Further, the lack of universal investigations might be caused by a language barrier. More than half of the previous reports were case reports written in Japanese [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24], and it can be challenging for non-Japanese researchers to fully comprehend these reports. Thus, we conducted an extensive review to elucidate the clinicopathological characteristics of patients with GC after pancreaticoduodenectomy.
Methods
Eligibility criteria and literature search
Observational studies written in English or Japanese were eligible for inclusion. Only full-text articles were eligible, and abstracts for conference or workshop were excluded. A literature search was conducted using these terms: “pancreaticoduodenectomy and gastric cancer,” “pancreaticoduodenectomy and gastric adenocarcinoma,: and “pancreaticoduodenectomy and gastric tumor.” MEDLINE and Igakuchuozasshi database, a database of Japanese articles, were searched. Studies in the reference lists of the retrieved articles were also searched. By reading the articles in detail, cases other than gastric tumor following pancreatic surgery were excluded. Further, the ineligible cases of gastrointestinal stromal tumor (GIST) or gastric metastasis were excluded. The ineligible case of duodenum preserving pancreatectomy was also excluded (Fig. 1).
Data collection and assessment
The following data were extracted from the identified studies: patient characteristics at pancreaticoduodenectomy, patient characteristics at GC treatment, clinicopathological features of GC, surgery for GC, and prognosis. The location of GC was described according to the Japanese classification of gastric carcinoma, and the stomach was anatomically divided into three portions, the upper (U), middle (M), and lower (L). The pathologic tumor stage was determined according to the tumor staging system based on the American Join Committee on Cancer Staging Manual, 8th edition criteria. The type of gastrectomy and reconstruction method were summarized using schematic illustrations. The patients in Japan and those in the Western countries were separately described to investigate the differences in reported cases.
Statistical analysis
All statistical analyses were performed using JMP statistical software version 13 (SAS Institute, Cary, NC).
Results
Literature review and cases in our institution
Seventeen eligible articles were identified from the electronic data bases search, and 32 patients were identified. We also included three patients from our institution. Therefore, the data of 35 patients were included in this review (Fig. 1; Table 1) [8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24].
Patient characteristics at pancreaticoduodenectomy of literature review cohort
Table 1 shows the patient characteristics at pancreaticoduodenectomy. The patient population comprised 23 males and 12 females. The age at PD was described or estimated in 15 patients, and the median age was 66 years, ranging from 48 to 79 years. The indication for pancreaticoduodenectomy was pancreatic ductal adenocarcinoma (PDAC; n = 13; 37.1%), distal bile duct cancer (DBDCa; n = 7; 20.0%), ampullary cancer (n = 6; 17.1%), pancreatitis (n = 3; 8.6%), duodenal cancer (n = 2; 5.7%), intraductal papillary mucinous neoplasm (n = 2; 5.7%), mucinous cystadenoma (n = 1; 2.9%), and gastrointestinal stromal tumor (GIST; n = 1; 2.9%). Twenty-nine (82.9%) of the 35 patients were diagnosed with cancer. Five (14.3%) patients had no malignant tumor, including three (8.6%) patients with pancreatitis. Cancer staging was noted in 11 of the 13 patients with PDAC, including stage 1, 2, and 3 in five, five, and one patient, respectively. The staging was noted in 19 of the 30 patients with cancer. No patients had stage 3 or 4 cancer, except for one patient with stage 3 PDAC. Regarding the surgical procedure, pylorus-preserving pancreatoduodenectomy (PPPD; n = 18; 51.4%), pancreaticoduodenectomy (n = 14, 40.0%), subtotal stomach-preserving pancreaticoduodenectomy (n = 2, 5.7%), and total pancreatectomy (n = 1, 2.9%) were performed. Reconstruction of the pancreas was noted in 34 patients, including pancreaticojejunostomy (PJ) in 16 (47.1%) patients, and pancreaticogastrostomy (PG) in 18 (52.9%). Adjuvant therapy after pancreaticoduodenectomy was noted in 28 patients, including chemoradiotherapy (CRT) in nine patients, and chemotherapy in three. All cases that received adjuvant therapy were reported since 2017.
Differences between the Japanese and Western cases
Table 2 summarizes the differences between the Japanese and Western cases. The most dominant indication for pancreaticoduodenectomy was biliary tract cancer (n = 6; 30.0%) in the Japanese cases, and it was PDAC (n = 10; 66.7%) in the western cases, respectively. The most frequently applied procedure of pancreaticoduodenectomy was PPPD with PG (n = 15; 75.0%) in the Japanese cases, and it was pancreaticoduodenectomy with PJ (n = 11, 73.3%) in the Western cases. The median length of time interval from pancreaticoduodenectomy to gastric cancer detection was 61.5 months and 115 months, respectively. Eight cases of well or moderately differentiated GCs were included in the Japanese cases. On the other hand, all cases had undifferentiated GCs in the Western cases. Eight patients who had received routine gastroscopy were Japanese cases, and the rate of early GC was higher in those. The most frequently applied procedure of gastrectomy was distal gastrectomy (n = 9, 45.0%) and total gastrectomy (n = 5, 33.3%), respectively.
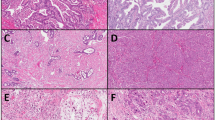
Clinicopathological features of gastric cancer after pancreaticoduodenectomy
Table 3 shows clinicopathological features of GC after pancreaticoduodenectomy. The age at GC detection was not described in 8 (22.9%) patients, and the median age of remaining 27 patients was 68 years, ranging from 49 to 83 years. The time interval between pancreaticoduodenectomy and GC detection was described in 29 (82.9%) patients, and the median interval was 78 months, ranging from 12 to 228 months. Fourteen (40.0%) patients with GC showed no abdominal symptoms, and among them, eight (22.9%) patients were diagnosed as having GC at regular gastroscopy after pancreaticoduodenectomy. The GCs were located at L portion in 19 (54.3%) patients, M portion in eight (22.9%), ML portion in three (8.6%), UM portion in two (5.7%), U portion in two (5.7%), and UML portion in one (2.9%). In 19 patients with GC in the L portion, 12 had tumors at the gastrojejunostomy or duodenojejunostomy site. The tumor differentiation was noted in 30 of the 35 patients, including well, moderately, and undifferentiated carcinomas in three (10.0%), five (16.6%), and 22 (73.3%) patients, respectively. Twenty-two undifferentiated carcinomas comprised eight poorly differentiated carcinomas and 14 signet-ring cell carcinomas. In 33 patients, T stage was noted, and among them, 15 patients were diagnosed as having early gastric cancer with T1 tumor. In 30 patients, GC staging was noted, including stage 1 cancer in 14 patients, stage 2 in six, stage 3 in six, stage 4A in one, and stage 4B in three. All eight patients who had received routine gastroscopy were T1N0M0 stage 1 (Fig. 2). On the other hand, the remaining 22 patients with GC included each six patients with stage 1, 2, or 3 (27.3% each), and four patients were diagnosed at stage 4 (18.2%).
Cancer staging in 30 patients with gastric cancer. No information about staging was available for the remaining 5 cases. In all 8 patients who had received routine gastroscopy after pancreaticodudenectomy (gastroscopy group), cancer stage was T1N0M0 stage 1. In the remaining 22 patients who had not received routine gastroscopy (non-gastroscopy group), cancer staging was stage 1 in 6 patients (27.3%), stage 2 in 6 (27.3%), stage 3 in 6 (27.3%), and stage 4 in 4 (18.2%), respectively
Patient characteristics at gastric cancer treatment
Table 4 shows patient characteristics at GC treatment. Genetic disease was noted in 3 patients, including BRCA2 gene mutation in one (8.3%) patient and Lynch syndrome in two (16.7%). The medical history of malignant tumor was noted in 33 patients, and 31 patients had received the treatment for malignant tumor. Cancer history in first-degree relatives was noted in 13 patients, including GC and breast cancer in one patient, PDAC in one, and GC in one. A Helicobacter pylori test was conducted on 5 patients, with one positive. The serum CEA and CA19-9 levels were measured in ten patients, and one and two patients showed abnormally high levels, respectively.
Surgery for gastric cancer
Table 5 and supplemental Figs. 1–5 summarize the surgical information for GC. Surgical resection was performed in 30 patients, including distal gastrectomy in nine patients, subtotal gastrectomy in four, total gastrectomy in nine, partial gastrectomy in five, proximal gastrectomy in two, and local excision in one. Among five patients without surgical resection, one patient received endoscopic submucosal dissection. Concomitant resection was performed in seven patients, including partial pancreatectomy in four patients, remnant pancreatectomy and splenectomy in two, and enterectomy in two. All six patients with concomitant pancreatectomy (cases 4, 6, 11, 16, 20, 22) had previously received PG at pancreaticoduodenectomy (Tables 1 and 5).
Reconstruction at gastrectomy
The reconstruction at gastrectomy is shown in supplemental figures. Several procedures were applied according to GC location, the extent of gastrectomy, and the type of pancreaticoenterostomy at pancreaticoduodenectomy. Following pancreaticoduodenectomy with PJ, reconstruction of the pancreas was not necessary, irrespective of the extent of gastrectomy (Supplemental Fig. 1). Following pancreaticoduodenectomy with PG and B-I gastrojejunostomy (or duodenojejunostomy), three types of gastrointestinal reconstructions without reanastomosis of the pancreas were performed (Supplemental Fig. 2). Following pancreaticoduodenectomy with PG and B-I gastrojejunostomy, two types of gastrointestinal reconstructions with reanastomosis of the pancreas were performed (Supplemental Fig. 3). Following pancreaticoduodenectomy with PG and B-II gastrojejunostomy, two types of gastrointestinal reconstructions without reanastomosis of the pancreas were performed (Supplemental Fig. 4). Following pancreaticoduodenectomy with PG and B-II gastrojejunostomy, two types of gastrointestinal reconstructions with reanastomosis of the pancreas were performed (Supplemental Fig. 5). All four patients with partial pancreatectomy received reanastomosis of the remnant pancreas using PJ, and none received reanastomosis using PG (Supplemental Fig. 3, 5). Furthermore, the remnant pancreas was always anastomosed to the jejunum apart from the main pathway of food.
Postoperative course and prognosis
Postoperative morbidity was noted in 26 patients, and gastrojejunostomy leakage, gastric outlet obstruction, and pyothorax were found in one patient (Table 5). One patient with gastrojejunostomy leakage died 9 days after gastrectomy due to peritonitis. The length of hospitalization after surgery was noted in 17 of the 30 patients, and the median length was 16 days ranging from 7 to 76 days. Postoperative chemotherapy was performed in five patients, and four of them were in the adjuvant setting. Five of the 27 patients showed the recurrence of GC. Fifteen (42.9%) patients with GC died during follow-up, and the cause of death was noted in seven patients, including GC in five patients.
Three cases from our institution
Case no. 1
A 66-year-old woman with no abdominal symptoms underwent gastroscopy as part of medical checkup, and the ampullary cancer was detected. She underwent pancreaticoduodenectomy with pancreaticogastrostomy. According to the UICC-TNM classification system, the ampullary cancer was classified as stage 0 (TisN0M0), and she did not undergo postoperative adjuvant chemotherapy. Seventeen months later, she underwent gastroscopy as part of medical checkup again, and 20-mm-sized early GC was detected in the lower third of the stomach. She underwent endoscopic submucosal dissection (ESD). The pathological examination revealed that the GC was moderately differentiated tubular adenocarcinoma, and it was confined within the mucosa (T1aN0M0). She was discharged 3 days after the ESD. She showed no sign of recurrence 54 months after the ESD.
Case no. 2
A 70-year-old woman with no abdominal symptom underwent follow-up computed tomography (CT) after cervical cancer treatment, and the pancreas head cancer was detected. She underwent pancreaticoduodenectomy with pancreaticogastrostomy. According to the UICC-TNM classification system, the PDAC was classified as stage 1A (T1N0M0). She underwent 20 cycles of adjuvant chemotherapy with gemcitabine and S1. About 10 years later, she showed melena, and the gastroscopy detected the GC in the lower third of the stomach. The GC was confined to the lower part of the stomach, and she underwent distal gastrectomy without reanastomosis of remnant pancreas. The pathological examination revealed that the GC was moderately differentiated tubular adenocarcinoma and it was classified as stage 1 (T1bN0M0). Her postoperative course was uneventful, and she was discharged 26 days after the gastrectomy. She showed no sign of recurrence 11 months after the gastrectomy.
Case no. 3
A 74-year-old man with a medical history of diabetes mellitus suffered from acute cellulitis, and contrast-enhanced CT accidentally detected the pancreas head tumor. His serum IgG4 level was within the normal range, and FDG-PET showed increased uptake of FDG in the pancreas head tumor. He was suspected to have PDAC, and he underwent pancreaticoduodenectomy with pancreaticogastrostomy. Pathological examination revealed that the pancreas head tumor was not PDAC but autoimmune pancreatitis. Six and a half years later, he showed severe fatigue and his serum hemoglobin was 3.6 g/dL. Gastroscopy revealed the bulky advanced cancer occupying the lower and middle parts of the stomach. The contrast-enhanced CT revealed that the GC invaded around the stomach, and the pancreaticogastrostomy site was also involved (Fig. 3a). He underwent subtotal gastrectomy concomitant with partial resection of the small intestine and transverse colon, and partial pancreatectomy (Fig. 3b). We added ρ anastomosis in Roux-en-Y reconstruction, and the remnant pancreas was anastomosed to a ρ loop. The pathological examination revealed that the GC was poorly differentiated tubular adenocarcinoma and it was classified as stage 4a (T4bN3aM0). His postoperative course was uneventful, and he was discharged 23 days after the gastrectomy. He showed no sign of recurrence 2 months after the gastrectomy.
Discussion
GC after pancreaticoduodenectomy is a fairly rare disease. However, it is estimated to increase in the near future due to several reasons such as decreased post-pancreatectomy mortality, better neo- and adjuvant treatments, increasing prevalence of PDAC, and expanding surgical indications to perform pancreaticoduodenectomy [1,2,3,4,5,6,7,8]. Following the first case reports three decades ago that predominantly originated from Japan, an increasing number of cases has been published in the meantime. Recently, the first institutional analyses from two large US institutions have provided more structured analyses of this phenomenon and enabled initial assessments of its frequency [8, 9]. Pflüger et al. included articles published in German and Japanese language in the review section of their manuscript. However, they did miss relevant articles of the Japanese literature. Therefore, we included a search in the Igakuchuozasshi database, a database of Japanese articles, that allowed us to identify twelve additional articles not previously reported (Table 1). By abstracting their clinicopathological features in this review article, we make them accessible for a broader scientific audience and to readers without Japanese language skills.
The differences between the Japanese and Western cases were also investigated, and several underlying factors were different between the two groups. GC following pancreaticoduodenectomy was reported from fourteen institutions in Japan and on the other hand, it was reported from only four institutions in the Western countries. This might be attributed to the difference whether single cases were regarded as scientific reporting or not. The most dominant indication for pancreaticoduodenectomy was biliary tract cancer in the Japanese cases, and seven cases of non-cancer were also included. In the western cases, PDAC was most dominant, and therefore, Japanese cases had undergone adjuvant therapy less frequently. The median length of time interval from pancreaticoduodenectomy to GC detection tended to be shorter in the Japanese cases, and it might be attributed to the routine gastroscopy. Eight patients who had received routine gastroscopy were all Japanese cases, and the rate of early GC was higher in those. The most frequently applied procedure of pancreaticoduodenectomy was also different, and it was PPPD with PG in the Japanese cases and pancreaticoduodenectomy with PJ in the Western cases. Further, Billroth I reconstruction was applied only in Japanese cases. These many factors were different in the two groups, and it was unclear whether the racial difference itself had influence on the carcinogenesis after pancreaticoduodenectomy. However, 40% of cases had been reported from the Western countries, and GC after pancreaticoduodenectomy may be the common problem for Western and Eastern countries.
Overall, the indication for pancreaticoduodenectomy included five (14.3%) patients with benign or low malignant disease, and most of the cancers were stage 0 to 2. Special attention to GC may be necessary for patients whose long survival time would be expected following pancreaticoduodenectomy. As risk factors of GC following pancreatectoduodenectomy, biliopancreatic reflux, genetic predisposition, adjuvant therapy, and helicobacter pylori infection have been reported [13, 15, 17, 18, 22,23,24]. Among them, biliopancreatic reflux was suspected to be the most important [13, 15, 18, 22,23,24]. Nineteen (54.3%) of the 35 patients had GC at the L portion, and 12 patients had involvement of the gastrojejunostomy (or duodenojejunostomy) site. It is noteworthy that 18 patients had previously received PPPD, and among them, 15 (83.3%) patients received PG. Meanwhile, 16 patients had previously received pylorus-resected pancreaticoduodenectomy, and among them, 13 (81.3%) patients received PJ. Pylorus preservation could theoretically limit biliary reflux into the gastric lumen; however, pancreatic juice from the PG site can cause mucosal damage. The technical variants of PG and PJ, pylorus-preserving, and resected pancreaticoduodenectomy may induce different mechanisms of carcinogenesis.
Genetic predisposition may also contribute to the development of remnant gastric cancer [23, 24]. Three (8.6%) patients had genetic diseases, and another three (8.6%) had a cancer history in first-degree relatives. Another possible contributing factor is adjuvant therapy for primary cancer [25,26,27,28,29]. In this study, no adjuvant therapy had been reported before 2017, and it had been reported in 12 of 19 patients since 2017. It remains unclear whether adjuvant therapy can cause GC following pancreaticoduodenectomy, because it is not used for patients with benign disease. However, neoadjuvant treatment prior to surgical resection of PDAC is a topic of debate and could be seen as recently increasing. As a novel risk factor of GC, some recent reports described the relationship between long-term PPI use and GC development [30,31,32,33]. Marginal ulcer is a relatively common complication after pancreaticoduodenectomy, and it can cause anemia, melena, or peritonitis [34]. To prevent marginal ulcer, antiulcer drugs are usually administered, and PPIs have been routinely administered after pancreaticoduodenectomy in our institution. However, it remains unclear whether PPI contributes to the carcinogenesis of GC after pancreaticoduodenectomy, because no previous report has described this problem. Molecular studies including Helicobacter pylori infection might be likely best suited to elucidate the most important carcinogens among the various potential local and systemic factors [35]. To the best of our knowledge, no dedicated molecular studies have been performed yet to investigate specifically GC after pancreaticoduodenectomy and we think that these are needed to gain better insights into the exact mechanisms of carcinogenesis.
The pathological features of GC following pancreaticoduodenectomy were investigated. Over 70% of GCs were highly malignant undifferentiated carcinomas, and therefore, early detection of GC might be especially important after pancreaticoduodenectomy. Fourteen (40%) patients had no abdominal symptoms, and among them, eight patients who had received regular gastroscopy had early GC with stage 1. However, stomach X-ray at medical checkup and tumor marker elevation could not detect GCs in the early stage among patients without abdominal symptoms. Long-term follow-up and regular gastroscopies might be important for long-term survivors following pancreaticoduodenectomy.
The surgical reconstruction methods after resection have not been reported in a systematic fashion yet, and therefore, we summarized surgical procedures in this review. In patients who had received PG at initial PD, reanastomoses of the remnant pancreas were occasionally necessary, depending on the gastric tumor size and location (Supplemental Figs. 3, 5). The reanastomosis can cause postoperative pancreatic fistula and subsequent serious intraabdominal hemorrhage. Therefore, GC screening may be more important for patients who received PG at pancreaticoduodenectomy, although the influence of reanastomosis on survival remains unclear. In all cases with reanastomosis, the site was jejunum, and it differed depending on the length of blind end jejunum. If the jejunum on the left side of choledochojejunostomy is long enough, the remnant pancreas can be anastomosed to there (Supplemental Fig. 3ab, 5ab). If the length is short, the ρ loop can be a candidate for the reanastomosis site (Supplemental Fig. 5 cd). In our case (case no. 3), the jejunum strictures and stasis at the anastomosis site were of concern. Therefore, we added ρ anastomosis in Roux-en-Y reconstruction, and the remnant pancreas was anastomosed to the ρ loop. It is noteworthy that the remnant pancreas was anastomosed to the jejunum other than the main food passage in all cases.
The present review had several limitations. First, the number of cases included is small, and the molecular and epidemiological investigations including ethnicities are necessary to stimulate further research. However, this review has included the largest number of patients thus far. Secondly, previous reports written in languages other than English or Japanese were not included in this study. We found one report written in German, and it was not cited due to the insufficient understanding of document content. However, this review includes information of Japanese reports, which have previously not been accessible for a broader scientific audience. Thirdly, it cannot be fully excluded that the cases are just coincidental findings of metachronous cancer and that there may not be a causal relationship between the two malignancies. However, there is emerging evidence indicating that GC is a sequel of pancreaticoduodenectomy in certain patients and needs to be appreciated as potential long-term complication of the procedure.
References
Cameron JL, He J (2015) Two thousand consecutive pancreaticoduodenectomies. J Am Coll Surg 220:530–536
Motoi F, Kosuge T, Ueno H et al (2019) Randomized phase II/III trial of neoadjuvant chemotherapy with gemcitabine and S-1 versus upfront surgery for resectable pancreatic cancer (Prep-02/JSAP05). Jpn J Clin Oncol 49:190–194
Uesaka K, Boku N, Fukutom A et al (2016) Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: a phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet 388:248–257
Neoptolemos JP, Palmer DH, Ghaneh P et al (2017) Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): a multicentre, open-label, randomised, phase 3 trial. Lancet 389:1011–1112
Takeno S, Hashimoto T, Maki K et al (2014) Gastric cancer arising from the remnant stomach after distal gastrectomy: a review. World J Gastroenterol 20:13734–13740
Lundegardh G, Adami HO, Helmick (1988) Stomach cancer after partial gastrectomy for benign ulcer disease. N Engl J Med 319:195–200
Tersmette AC, Offerhaus GJ, Tersmette KW et al (1990) Meta-analysis of the risk of gastric stump cancer: detection of high risk patient subsets for stomach cancer after remote partial gastrectomy for benign conditions. Cancer Res 50:6486–6489
Sonoda K, Samdani RT, Ikoma N (2019) Gastric cancer in the remnant stomach after pancreaticoduodenectomy: a case series. J Surg Oncol 120:1137–1141
Pflüger MJ, Felsenstein M, Schmocker R et al (2020) Gastric cancer following pancreaticoduodenectomy: experience from a high-volume center and review of existing literature. Surg Open Sci 2:32–40
Tatsuzawa Y, Osari A, Uno Y et al (1995) A case of early gastric cancer after pylorus-preserving pancreatoduodenectomy. J Jpn Pract Surg Soc 56:2084–2088
Kaneda K, Nomura H, Fujiwara H et al (1996) A case of early gastric cancer after pylorus-preserving pancreatoduodenectomy. Acta Med Kinki Univ 21:263–268
Manabe T, Nishihara K, Kurokawa Y et al (2001) A collision tumor composed of adenocarcinoma and malignant lymphoma in the remnant stomach after pancreatoduodenectomy: report of a case. Surg Today 31:450–453
Ohashi N, Tamaki H, Sanda T et al (2001) Development of carcinoma of the stomach after pylorus-preserving pancreatoduodenectomy (PPPD) for early carcinoma of the papilla of Vater: case report. J Jpn Pancreas Soc 16:42–47
Emoto T, Yoshikawa K, Dousei T et al (2002) A case of early gastric cancer after pylorus-preserving pancreatoduodenectomy. Jpn J Gastroenterol Surg 35:277–281
Mihara Y, Kubota K, Nemoto T et al (2005) Gastric cancer developing in the stomach after pylorus-preserving pancreaticoduodenectomy with pancreaticogastrostomy: case report and review of the literature. J Gastrointest Surg 9:498–502
Tsukahara A, Koyama S, Hatayama S et al (2006) A case of early gastric cancer after pylorus-preserving pancreatoduodenectomy. Operation 60:259–262 (in Japanese)
Furukawa K, Oguma H, Yamamoto M (2007) A case of early gastric cancer revealed 7 years after PPPD. Nihon Gekakei Rengo Gakkaishi 32:44–47
Sunagawa H, Taskahashi I, Nishizaki T (2013) A case of gastric cancer after pylorus-preserving pancreatoduodenectomy with pancreaticogastrostomy. Rinsho To Kenkyu 90:181–184 (in Japanese)
Yamada M, Nakai K, Inoue K et al (2014) A case report of residual gastric cancer 15 years after pancreatoduodenectomy with modified child’s reconstruction. Gan To Kagaku Ryoho 41:2439–2441
Sakaki M, Taniguchi H, Yamano T (2015) A case of early gastric cancer with intraductal papillary mucinous carcinoma (IPMC) recurrence developing at the site of pancreaticogastrostomy (PG) after pancreaticoduodenectomy (PD) for IPMC of the pancreas head. J Kyoto Pref Univ Med 124:265–276
Hiramatsu K, Kato T, Shibata Y et al (2016) Five cases of early gastric cancer after pylorus-preserving pancreatoduodenectomy with pancreaticogastrostomy. Operation 70:1113–1120
Kujiraoka M, Asai K, Watanabe R et al (2019) A case of resection of early gastric cancer developing after pancreaticoduodenectomy with pancreaticogastrostomy. Nihon Gekakei Rengo Gakkaishi 44:209–216
Kassahun WT, Lamesch P, Wittekind C et al (2008) Signet-ring cell carcinoma arising in the gastric stump after duodenopancreatectomy for ductal adenocarcinoma of the pancreas: a case report. Clin Med Oncol 2:109–112
Bouquot M, Dokmak S, Barbier L et al (2017) Gastric stump carcinoma as a long-term complication of pancreaticoduodenectomy: report of two cases and review of the English literature. BMC Gastroenterol 17:117
Tempero MA, Malafa MP, Al-Hawary M et al (2017) Pancreatic adenocarcinoma, version 2.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 15:1028–1061
Oettle H, Post S, Neuhaus P et al (2007) Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA 297:267–277
Hsu CC, Herman JM, Corsini MM et al (2010) Adjuvant chemoradiation for pancreatic adenocarcinoma: the Johns Hopkins Hospital–Mayo Clinic collaborative study. Ann Surg Oncol 17:981–990
Ahsan H, Neugut AI (1998) Radiation therapy for breast cancer and increased risk for esophageal carcinoma. Ann Intern Med 128:114–117
Hauptmann M, Fossa SD, Stovall M et al (2015) Increased stomach cancer risk following radiotherapy for testicular cancer. Br J Cancer 112:44–51
Kuipers EJ (2006) Proton pump inhibitors and gastric neoplasia. Gut 55:1217–1221
Hagiwara T, Mukaisho K, Nakayama T et al (2011) Long-term proton pump inhibitor administration worsens atrophic corpus gastritis and promotes adenocarcinoma development in Mongolian gerbils infected with Helicobacter pylori. Gut 60:624–630
Cheung KS, Chan EW, Wong AYS et al (2018) Long-term proton pump inhibitors and risk of gastric cancer development after treatment for Helicobacter pylori: a population-based study. Gut 67:28–35
Seo SI, Park CH, You SC et al (2021) Association between proton pump inhibitor use and gastric cancer: a population-based cohort study using two different types of nationwide databases in Korea. Gut 70:2066–2075
Suemori K, Kojima T, Mimura T (2021) Investigation of marginal ulcer after pancreatoduodenectomy. Nihon Shokakibyo Gakkai Zasshi 118:61–69
Imai S, Ooki T, Murata-Kamiya N et al (2021) Helicobacter pylori CagA elicits BRCAness to induce genome instability that may underlie bacterial gastric carcinogenesis. Cell Host Microbe 29:941–958
Author information
Authors and Affiliations
Contributions
Study conception and design: Tatsuaki Sumiyoshi. Acquisition of data: Hiroyuki Otsuka. Analysis and interpretation of data: Kenichiro Uemura, Naru Kondo. Drafting of manuscript: Tatsuaki Sumiyoshi, Kenichiro Uemura, Kenjiro Okada, Shingo Seo, Shinya Takahashi. Critical revision of manuscript: Kenichiro Uemura
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethics committee of Hiroshima University and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sumiyoshi, T., Uemura, K., Kondo, N. et al. Clinicopathological features of gastric cancer after pancreaticoduodenectomy: reporting of three institutional cases and review of the global literature. Langenbecks Arch Surg 407, 2259–2271 (2022). https://doi.org/10.1007/s00423-022-02524-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02524-6